Abstract
Aerosolized delivery of virulent or hypervirulent Mycobacterium tuberculosis requires careful consideration of methodology and safety. To maximize safety, we installed a nose-only aerosol apparatus that can reproducibly deliver a low dose (<100 CFU per mouse) of M. tuberculosis in a carefully designed biohazard facility.
Delivery of a low-dose inoculum by inhalation is arguably the most physiologically natural method for infecting experimental animals with Mycobacterium tuberculosis. Aerosol infection has been shown to allow for a more rapid lung pathology, shorter survival time, and higher rate of bacterial growth in mice than intravenous infection of greater numbers of bacilli (9). After immunization with Mycobacterium bovis (bacillus Calmette-Guérin), mice are more susceptible to aerosol infection than to intravenous infection with 625 times the aerosol dosage (10). Given that natural M. tuberculosis infection is the result of bacterial inhalation and that the inoculum deposition may have an influence on the course of infection (8), it is important to utilize models that approximate the course of natural infection by depositing only a few bacteria in the upper airways (11).
Aerosol delivery of M. tuberculosis has been used in other studies, and an aerosol study laboratory with the ability to infect mice by use of a Henderson aerosol apparatus (5) has been described previously (6). However, there is no published information on the experimental setup used in these infection procedures or on the design of a modern facility for murine studies that would include vaccination or protection experimentation. Furthermore, aerosol infection procedures are likely to vary depending on the experimental setup, and there is no published information available on how to control variables to deliver a standard dose of M. tuberculosis. Hypervirulent M. tuberculosis strains may occur naturally (14), and it is possible that an added occupational hazard exists when drug-resistant M. tuberculosis strains are used. In some cases, mutagenesis studies may also have the potential to create hypervirulent M. tuberculosis. For these reasons, we calibrated a nose-only aerosol apparatus from the U.S. Army Medical and Research Institute for Infectious Diseases (USAMRIID) (similar to that used previously [2]) in a specially designed biohazard level-3 (BSL-3) facility. This was achieved through consultation with the safety committees of USAMRIID, the Howard Hughes Medical Institute (HHMI), and the Albert Einstein College of Medicine (AECOM). The nose-only apparatus selected minimizes the localization of bacteria outside the respiratory tree, and this apparatus is enclosed within an airtight glove box for a maximum amount of BSL-3 safety.
(The data in this paper are from a thesis submitted by J. Reid Schwebach in partial fulfillment of the requirements for the degree of doctor of philosophy from the Sue Golding Graduate Division of Medical Sciences, Albert Einstein College of Medicine, Yeshiva University, Bronx, N.Y.)
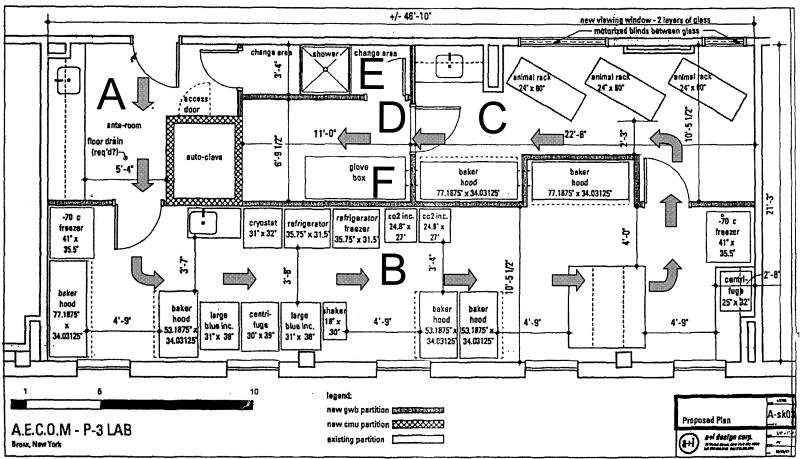
Consultation with the USAMRIID, HHMI, and AECOM safety committees allowed for unanimous approval (all parties having equal say) of the facility construction plans. The facility was designed with concern for airflow and the use of dangerous (aerosolized) M. tuberculosis (Fig. 1). Airflow is routed from the least dangerous to the most dangerous rooms, and the aerosol cabinet was placed in the room with the greatest negative pressure (pressures are approximately −0.0066 in. at 74.6°C in the anteroom, −0.0116 in. at 72.2°C in the change room, −0.142 in. at 71.1°C in the equipment room, −0.0209 in. at 71.9°C in the animal room, and −0.250 in. at 75.2°C in the glove box room). This pressure configuration is monitored remotely by AECOM engineering during the day (adjustments are made with temperature changes) and by an alarm system at all times. The design of the biohazard facility allows for multiple researchers to conduct in vitro experiments in type II biosafety cabinets while work is carried out in another portion (Fig. 1). The routing of airflow should direct any aerosolized M. tuberculosis into the most hazardous room. A shower room (Fig. 1) is available for use after immediate evacuation from the aerosol room (evacuation is necessary should a loss of glove box pressure go beneath −0.25 in.). In the event of a leak, workers are required to shower for 3 min in their full-body Kappler 100% polyolefin Tyvek suits (Fisher Scientific, Springfield, N.J.) and model 3M 9210 N95 particulate respirators (Fisher Scientific). Workers in the AECOM-HHMI BSL-3 facility always wear respirators and full-body Tyvek suits. This apparel is donned and removed in the anteroom.
FIG. 1.
Facility floorplan. The BSL-3 facility contains an anteroom (A), a work area complete with multiple biosafety cabinets (B), an animal room (C), and an aerosol room (D). An autoclave joins the aerosol room with the anteroom (D), and a shower room (E) is available for emergency exit. Dimensions of the facility and appliances are indicated in feet. Airflow is indicated by arrows. The aerosol cabinet is also indicated (F).
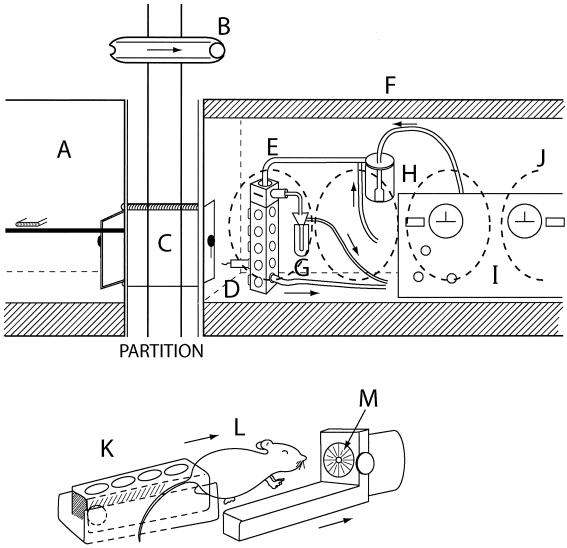
The USAMRIID aerosol apparatus utilizes a Collison nebulizer (7) to create a vapor containing aerosolized mycobacteria. This vapor mixes with dry secondary air traveling at a flow rate of 4.3 to 4.7 liters/min for a combined airflow rate of 11.8 to 12.2 liters/min. The vapor is drawn through the exposure chamber (Fig. 2D), where mice (≤15) are placed in restraining stanchions (Fig. 2K to M) that securely position the animals for nose-only aerosol exposure. After the vapor leaves the exposure chamber, the air is injected into liquid for collection of residual mycobacteria in an all-glass impinger (AGI) (Fig. 2G) (3). The AGI can be used to collect a sample of the air during the exposure to verify the number of bacteria administered. An extensive, approved, and descriptive protocol for the use of this particular aerosol apparatus has been published previously (12). This entire apparatus is safely contained within an Isogard class III glove box (Baker Company, Sanford, Maine) (Fig. 2F) connected to a Sterilgard II, class II, type A/3B hood (Baker Company) (Fig. 2A) in the adjoining room. Sterilization of the glove box is done with paraformaldehyde gas for 8 h. The paraformaldehyde is then neutralized by use of a KMNO4 filter attached to the glove box. This decontamination is to be conducted every 6 months. Settling plates were used for sampling during some experimentation. Exposure of 7H10 agar (Difco, Detroit, Mich.) plates located on all interior corners of the hood floor, for the entire duration of 1 day of experimentation (including four infections, washes, and animal manipulations), did not yield any CFU. This result indicates that little or no deposition of bacteria occurred on the bottom of the hood during the aerosol procedure.
FIG. 2.
Facility and aerosol apparatus photographs. The aerosol cabinet (F) is joined to a biohazard cabinet in the animal room (A) via a sealed, interconnecting passageway (C) that connects the two cabinets between the two rooms. Glove openings in the glove box are shown as dotted lines (J). Airflow in the rooms is indicated above the doorways (ball is pushed by air movement) (B). The control panel of the aerosol apparatus is shown (I), and the nebulizer is illustrated (H). The animal chamber is shown (E), and an AGI (G) and an animal stanchion containing a mouse (D) are illustrated. Mice (L) are contained in stanchions (K and M) that connect to the animal chamber. The nose of each mouse rests inside an aperture of the stanchion (M), allowing for nose-only aerosol exposure. The airflow direction within the aerosol apparatus is indicated by arrows.
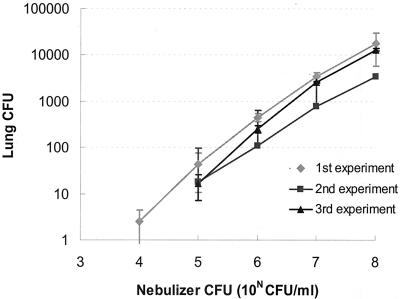
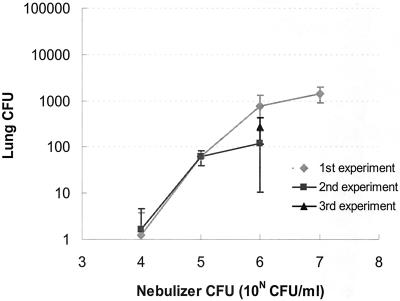
For initial testing of the aerosol apparatus, we used Mycobacterium smegmatis, a BSL-1 pathogen. Delivery of low-dose M. tuberculosis is hindered by the tendency of mycobacteria to aggregate, which necessitates the use of a detergent to prevent clumping (15). We therefore optimized conditions for aerosolization by using Tween 80 (Sigma, St. Louis, Mo.)-grown M. tuberculosis and the antifoaming agent Antifoam-A (Sigma), which prevents frothing. For infection of mice with M. smegmatis strain mc2 155, M. smegmatis cells were grown in liquid 7H9 medium containing 0.05% Tween 80 (7H9-T medium) to an absorbance of approximately 0.8 at 600 nm. Previous experimentation had shown that a mycobacterial culture with an absorbance of 1.0 at 595 nm contained 2 × 108 to 5 × 108 mycobacteria per ml (data not shown). Mice were exposed to aerosolized mycobacteria that had been suspended in phosphate-buffered saline containing 0.05% Tween 80 detergent and 0.4% Antifoam-A. For the initial dilution of mycobacteria, the amount of bacteria to add to the nebulizer was determined with Guyton's formula: breathing volume (in milliliters) = [2.1 × animal weight (in grams) e+0.75] · [(CFU/liter of aerosol) × (animal breathing rate)] = CFU/mouse (4). The preliminary results gave us a basis for designing the experiments in this work. The AGIs could be used to generate a standard curve, which can be used to determine the number of bacilli the mice inhaled. However, we found AGI sampling to be less precise and more susceptible to contamination than the plating of CFU from sentinel animals in determining the M. tuberculosis CFU delivered to the lungs (data not shown). For each dosage, three BALB/c mice (Charles River Laboratories, Wilmington, Mass.) were placed in stanchions, attached to the animal exposure chamber, and exposed to aerosolized mycobacteria for 10 min, followed by a 5-min air wash, before removal of the mice from the apparatus. The animals were sacrificed at 3 h postinfection, and the numbers of CFU in their lungs were determined by plating stomached lung samples as described previously (12a) on 7H10 agar (Difco) and counting colonies 3 to 4 weeks later. The relationship between the number of bacteria in the nebulizer after an animal's exposure was proportional to the number of CFU in the lungs (Fig. 3). Similar results were obtained for M. tuberculosis Erdman (Fig. 4) that had been thawed from frozen stocks. These stocks were prepared from an animal-passaged Erdman strain (designated EF2) and grown until the absorbance of the culture was 0.4 at 595 nm; a spectrophotometer was used to assess the turbidity of a formalin (Biochemical Sciences, Swedesboro, N.J.)-fixed culture sample. Formalin fixation was performed as described previously (13). Aliquots of the culture were then frozen in 10% glycerol (Sigma). It was necessary to change the nebulizer suspension after every group exposure to prevent the M. tuberculosis CFU delivered from being drastically reduced (>3-fold; with a concentration of 106 M. tuberculosis CFU/ml in the nebulizer) during later aerosolizations (data not shown). Repetition of the experimentation on different days, including preparation of new bacterial dilutions, gave very similar numbers of CFU (Fig. 3 and 4). We sacrificed two animals and plated samples from them for each group exposed to aerosolized M. tuberculosis during ongoing experimentation, and this is a reliable method of confirming the number of M. tuberculosis CFU delivered between groups (data not shown).
FIG. 3.
Delivery of M. smegmatis to mice. Total CFU in the lung versus CFU per milliliter in the nebulizer as a result of the aerosolization procedure is shown. Each value represents the average for three animals. Error bars show the standard deviations of the means.
FIG. 4.
Delivery of M. tuberculosis Erdman to mice. Total CFU in the lung versus CFU per milliliter in the nebulizer as a result of the aerosolization procedure is shown. Each value represents the average for three animals. Error bars show the standard deviations of the means.
All workers undergo training by experienced coworkers, followed by proficiency testing in the safe handling of M. tuberculosis. The examination includes a mock electroporation of M. tuberculosis in the BSL-3 facility and colony plating of M. tuberculosis from a mock-infected mouse. Any mistakes in an exam (bringing contaminated material to the outside of a containment cabinet or neglecting to completely wipe any object with Vesphine IIse [Steris Corp., Calgon Vestal Division, St. Louis, Mo.] before removing it from the biosafety cabinet) constitute failure of that exam. An additional safeguard is that a newly trained worker must work with a more experienced worker three times before participating in a new procedure on his own. All workers are tested for reactivity to purified protein derivative by the AECOM environmental health department every 6 months. Purified protein derivative conversions would be reported to the AECOM safety committee, which has oversight of the procedures conducted in the AECOM-HHMI BSL-3 facility, as does HHMI. The elements comprising this type of training and the safety rationale for this level of concern have been discussed previously (1), and we encourage other facilities to utilize this degree of precaution.
Acknowledgments
J. Reid Schwebach and B. Chen contributed equally to this work.
We give special thanks to Robert Hawley and Louise Pitts of HHMI, USAMRIID, the AECOM safety committee, the AECOM department of environmental safety, AECOM engineering, and Emmett Barkley of HHMI for their consultation services in the design, construction, and maintenance of this facility and in its protocol construction.
W.R.J. is supported by HHMI. A.C. is supported by NIH grants AI33142, AI33774, and HL59842. A.G. has been an Aaron Diamond Young Investigator Awardee, and this work was supported in part by a grant from the Aaron Diamond Foundation. This work was also supported in part by NIH grant 1K08AI01691 (A.G.). A.C. is also supported by a Burroughs-Wellcome Fund Scholar Award in Experimental Therapeutics. J.R.S. was supported by an NIH training grant in HIV, AIDS, and Opportunistic Infections (grant 5T32AI07501).
REFERENCES
- 1.Barkley, E. 1994. Safety in the tuberculosis laboratory, p. 73-84. In B. R. Bloom (ed.), Tuberculosis: pathogenesis, protection, and control. ASM Press, Washington, D.C.
- 2.Converse, P. J., A. M. Dannenberg, Jr., J. E. Estep, K. Sugisaki, Y. Abe, B. H. Schofield, and M. L. Pitt. 1996. Cavitary tuberculosis produced in rabbits by aerosolized virulent tubercle bacilli. Infect. Immun. 64:4776-4787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cown, W. B., T. W. Kethley, and E. L. Fincher. 1957. The critical-orifice liquid impinger as a sampler for bacterial aerosols. Appl. Microbiol. 5:119-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guyton, A. C. 1947. Measurement of the respiratory volumes of laboratory animals. Am. J. Physiol. 150:70-77. [DOI] [PubMed] [Google Scholar]
- 5.Loudon, R. G., L. R. Bumgarner, J. Lacy, and G. K. Coffman. 1969. Aerial transmission of mycobacteria. Am. Rev. Respir. Dis. 100:165-171. [DOI] [PubMed] [Google Scholar]
- 6.Loudon, R. G., R. A. Frantz, Jr., and C. A. LeMaistre. 1969. Laboratory for the study of mycobacterial aerosols. Am. Rev. Respir. Dis. 100:160-164. [DOI] [PubMed] [Google Scholar]
- 7.May, K. R. 1973. The Collison nebulizer: description, performance and applications. J. Aerosol Sci. 4:235-243. [Google Scholar]
- 8.McKinney, J. D., W. R. Jacobs, and B. R. Bloom. 1998. Persisting problems in tuberculosis, p. 51-146. In R. M. Krause (ed.), Emerging infections. Academic Press, San Diego, Calif.
- 9.North, R. J. 1995. Mycobacterium tuberculosis is strikingly more virulent for mice when given via the respiratory than via the intravenous route. J. Infect. Dis. 172:1550-1553. [DOI] [PubMed] [Google Scholar]
- 10.North, R. J., R. LaCourse, and L. Ryan. 1999. Vaccinated mice remain more susceptible to Mycobacterium tuberculosis infection initiated via the respiratory route than via the intravenous route. Infect. Immun. 67:2010-2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Orme, I. M., and F. M. Collins. 1994. Mouse model of tuberculosis, p. 113-134. In B. R. Bloom (ed.), Tuberculosis: pathogenesis, protection and control. ASM Press, Washington, D.C.
- 12.Schwebach, J. R. 2002. Ph.D. thesis. Albert Einstein College of Medicine, Bronx, N.Y.
- 12a.Schwebach, J. R., A. Casadevall, R. Schneerson, Z. Dai, X. Wang, J. B. Robbins, and A. Glatman-Freedman. 2001. Expression of a Mycobacterium tuberculosis arabinomannan antigen in vitro and in vivo. Infect. Immun. 69:5671-5678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwebach, J. R., W. R. Jacobs, and A. Casadevall. 2001. Sterilization of Mycobacterium tuberculosis Erdman samples by antimicrobial fixation in a bio-safety level 3 laboratory. J. Clin. Microbiol. 39:769-771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valway, S. E., M. P. C. Sanchez, T. F. Shinnick, I. M. Orme, T. Agerton, D. Hoy, J. S. Jones, H. Westemoreland, and I. M. Onorato. 1998. An outbreak involving extensive transmission of a virulent strain of Mycobacterium tuberculosis. N. Engl. J. Med. 338:633-639. [DOI] [PubMed] [Google Scholar]
- 15.Wayne, L. G. 1994. Cultivation of Mycobacterium tuberculosis for research purposes, p. 73-84. In B. R. Bloom (ed.), Tuberculosis: pathogenesis, protection, and control. ASM Press, Washington, D.C.