Abstract
Introduction
Menstrual inequity refers to the systematic and avoidable differences experienced by women and people who menstruate, based on having a menstrual cycle and menstruating. Given the paucity of prior research examining the impact of menstrual inequity on health, a scoping review was conducted to explore and map out the menstrual inequities and their association with health outcomes in women and people who menstruate within the published academic literature.
Methodology
Two searches were conducted in May 2022 and March 2024 in PubMed and Scopus. Academic literature published until December 2023 was included. Following the screening process, 74 articles published between 1990 and 2023 were included in the review. Results were then synthesised through narrative analysis and organised into nine categories.
Results
A range of both physical and emotional health outcomes were documented to be associated with menstrual inequity. Urinary tract infection, reproductive tract infection, and other genital discomforts (e.g. itching) were linked to certain menstrual discomforts (e.g. dysmenorrhea) as well as a lack of access to menstrual products, menstrual management facilities and/or menstrual information. The emotional health outcomes, especially anxiety, distress and depression, were salient and were shown to be related to menstrual stigma, the lack of menstrual information and the limited access to menstrual-related healthcare.
Conclusions
The majority of the included studies were focused on menstrual management, being one of the most addressed themes concerning menstruation, and the health outcomes were mainly reproductive tract infection and emotional/mental health. Expanding the range of health outcomes studied will strengthen research and inform policy. Further research is needed to better understand the complex association between menstrual inequities and other potential health outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12978-025-02103-0.
Keywords: Menstrual inequity, Menstruation, Social determinants of health, Health outcomes, Emotional health, Reproductive tract infections, Scoping review
Plain Language summary
Menstruation and the menstrual cycle are connected to the overall health of women and other people who menstruate. Menstrual inequity refers to the unfair situations and barriers that women and people who menstruate face because they menstruate. These include not having access to proper menstrual healthcare, menstrual education and knowledge, menstrual products, lacking services and facilities for menstrual management, experiencing menstrual stigma and discrimination, and the ability to fully participate in social, community, political and economic spheres. All these challenges can have an impact on their overall health. This study had the objective to explore these menstrual inequities and their association with health outcomes in women and people who menstruate in the published academic literature. We included information from 74 articles published until December 2023. The findings showed that menstrual inequity is linked to various health issues. For example, physical healthproblems, like urinary or reproductive tract infections, were often linked to difficulties managing menstruation. Moreover, emotional health issues like anxiety, distress, and depression were connected to experiences of menstrual stigma and discrimination, and having limited access to menstrual healthcare and education. This review also found that more research is needed about the relationship between menstrual inequity and health outcomes to fully understand how menstrual inequity affects women and people who menstruate. By doing so, researchers can provide better information to guide policies and improve health of women and people who menstruate.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12978-025-02103-0.
Resumen
Introducción
La inequidad menstrual se refiere a las diferencias sistemáticas y evitables que experimentan las mujeres y las personas que menstrúan, basadas en el hecho de tener un ciclo menstrual y menstruar. Dada la escasez de investigaciones previas que examinen el impacto de la inequidad menstrual en la salud, se llevó a cabo una revisión de alcance para explorar y mapear las inequidades menstruales y su asociación con los resultados de salud en mujeres y personas que menstrúan dentro de la literatura académica publicada.
Metodología
Se realizaron dos búsquedas en mayo de 2022 y marzo de 2024 en PubMed y Scopus. Se incluyó la literatura académica publicada hasta diciembre de 2023. Tras el proceso de cribado, se incluyeron en la revisión 74 artículos publicados entre 1990 y 2023. Los resultados se sintetizaron mediante un análisis narrativo y se organizaron en nueve categorías.
Resultados
Se documentaron una serie de resultados en salud, tanto físicos como emocionales, asociados a la inequidad menstrual. Las infecciones del tracto urinario, las infecciones del tracto reproductivo y otras molestias genitales (p. ej., picor) se relacionaron con ciertas molestias menstruales (p. ej., dismenorrea), así como con la falta de acceso a productos menstruales, instalaciones para la gestión menstrual y/o información menstrual. Los resultados de salud emocional, especialmente la ansiedad, la angustia y la depresión, se destacaron y se demostró que estaban relacionados con el estigma menstrual, la falta de información menstrual y el acceso limitado a la asistencia sanitaria relacionada con la menstruación.
Conclusiones
La mayoría de los estudios incluidos se centraron en el manejo menstrual, siendo uno de los temas más abordados en relación con la menstruación, y los resultados en salud principalmente reportados fueron las infecciones del tracto reproductivo y la salud emocional/mental. Ampliar la variedad de resultados en salud fortalecerá la investigación y orientará las potenciales políticas. Es necesario realizar investigaciones para comprender mejor la compleja relación entre las inequidades menstruales y otros posibles resultados en salud.
Palabras Clave: Inequidad menstrual, Menstruación, Determinantes Sociales de la Salud, Resultados en Salud, Salud emocional, Infecciones del Sistema Genital, Revisión de Alcance
Introduction
Menstruation, the menstrual cycle and how they are related to the overall health of women and people who menstruate (PWM) is a widely under-prioritized topic in both the academic, social and political field [1, 2]. This corresponds to a well-documented gender bias within health that continues to persist, manifesting itself, among other things, as an underrepresentation of women in health-related studies, misdiagnosis of women’s symptoms, the trivialization of women’s complaints, and discrimination in the awarding of research grants towards female researchers and research on women’s health [3]. This disregard of health conditions that disproportionately affect women is rooted in the all-encompassing tendency for society, its institutions, discourses and norms, to be centred around (white, cis-gendered, heterosexual, able-bodied) men and their needs, values and priorities, consequently prioritizing the male experience and marginalizing any other experience - such as menstruation [4, 5].
We understand menstrual inequities (MI) as a concept grounded in health equity and social inequities frameworks. Medina-Perucha et al., 2023 define MI as “the systematic and avoidable differences in the access to menstrual healthcare, education and knowledge, products, services and facilities for menstrual management, menstrual related experiences of stigma and discrimination, and social, community, political and economic participation based on having a menstrual cycle and menstruating” [6]. This umbrella term encompasses fundamental dimensions of MI, such as menstrual poverty (the struggle to afford menstrual products) [7] and menstrual management [8], menstrual healthcare, experiences of stigma and discrimination, and social, community, political and economic participation. These dimensions often intersect and overlap, maintaining and reinforcing health inequities for women and PWM. Framing these dimensions within the broader concept of MI allows for attending to how such inequities are a structural issue, rather than an individual one. Table 1 illustrates a conceptualisation of the relations between these concepts.
Table 1.
Relationship between menstrual inequity (MI) and its components
| Concept | Definition | Relationship with menstrual inequity |
|---|---|---|
| Access to menstrual healthcare | The access to timely diagnosis, treatment and care for menstrual cycle-related discomforts and disorders, including access to appropriate health services and resources, pain relief, and strategies for self-care [9]. | Menstrual inequity occurs when healthcare systems do not recognise and prioritise menstrual health. This can result in delayed, inaccurate diagnoses, unnecessary medicalisation, dismissal of symptoms, among other issues. Menstrual inequities do not, however, exist in isolation and also intersect with other types of (health) inequities such as race, class, gender etc. Moreover, there are barriers (e.g., economic, geographic) that limit the access to specialised menstrual healthcare for some women and PWM. |
| Access to menstrual products and menstrual poverty | The ability to obtain safe, effective, and affordable menstrual materials (e.g., cups, pads, tampons). Limited access to these products is known as “menstrual poverty”. We understand and classify menstrual poverty in three types: (1) not being able to afford menstrual products, (2) not being able to afford preferred products, and (3) having to prioritize menstrual products over other products or activities [1]. | Menstrual poverty is a material expression of menstrual inequity. Menstrual poverty not only highlights inequities related to menstruation and the menstrual cycle, but also reveals other inequities such as financial hardship and poverty. |
| Menstrual related experiences of stigma and discrimination | Menstrual stigma and discrimination are the result of complex social notions manifesting as negative attitudes towards menstruation. Menstrual discrimination refers to marginalization, oppression, harassment or even microaggressions directed at individuals because they menstruate and have a menstrual cycle [10, 11]. | Menstrual stigma and discrimination are both an expression of and contributing factors to menstrual inequities. Menstrual stigma and discrimination have a wide range of negative consequences for women and PWM’s health, sexuality, wellbeing and social status. It furthermore upholds social and institutional barriers limiting access to resources, information, healthcare and supportive environments perpetuating social exclusion. |
| Access to menstrual management | The access to clean menstrual management is defined as access to materials to absorb and collect blood, that can be changed in privacy as often as necessary for the duration of the menstruation, soap and water for washing the body as required and having access to facilities to dispose of used menstrual management materials [12]. Other definitions also specify that menstrual management facilities are clean spaces, where water is available and include a bin and can be locked [1]. Many definitions are based on the use of ‘menstrual hygiene management (MHM)’ although we choose not to use the term ‘hygiene’ because of the connotations associating menstruation with a lack of cleanliness. | The lack of access to menstrual management reflects menstrual inequity, as insufficient possibilities to manage menstruation with dignity, which can affect health and social participation. Barriers that limit access to menstrual management are expressions of systems that reproduce a variety of inequities not limited to menstrual inequity (e.g., gender, class, territoriality). These structural inequities shape the material and social conditions that hinder safe and dignified menstrual management for women and PWM. |
| Access to menstrual education and knowledge | The access to accurate, timely, age-appropriate information about the menstrual cycle, menstruation, and changes experienced throughout the life-course, as well as related self-care and hygiene practices [9]. | A lack of access to menstrual education and knowledge directly contributes to menstrual inequity, as it limits (self-)knowledge about the body and menstruation-related processes. In some contexts, menstrual education has been provided incompletely or predominantly with a biomedical focus, leaving out important information on self-care and socio-cultural aspects of menstruating. This prevents a comprehensive understanding of the menstrual cycle. |
| Access to social, community, political, and economic participation | Being able to participate in all spheres of life refers to being able to decide whether and how to participate in the civil, cultural, economic, social, and political spheres, during all phases of the menstrual cycle, free from menstrual-related exclusion, restriction, discrimination, and/or violence [9]. | The access to social, community, political and economic participation are closely linked to other dimensions of menstrual inequity, such as access to adequate menstrual management, freedom from menstrual stigma and discrimination, and acquisition of menstrual education and information, among others. When women and PWM face barriers through lack of access to resources and education, or the presence of stigma and discrimination, their full participation cannot be realised. |
The concept of MI serves to draw attention towards how androcentric social structures (which prioritise cis male experiences and perspectives) systematically stigmatise menstruation [13]. Several frameworks have been applied within research to investigate systemic menstrual-related disparities, such as the menstrual justice framework [14] or the human rights framework [15]. Both approaches emphasize how political and economic structures are shaped by different axes of domination generating disadvantages, oppression and violations of the fundamental rights of women and PWM [14, 16, 17]. They do not, however, directly engage with how these systematic inequities affect the health of women and PWM.
The urgency of examining health outcomes linked to MI is alternatively underscored by the social determinants of health (SDH) framework. This framework highlights how the circumstances in which people are born, grow, work, and live significantly impact their health [18]. SDH thus include (but is not limited to) economic policies and systems, development agendas, cultural norms, social policies and political systems [18, 19]. SDH plays an important role in producing and upholding health inequities and have been argued to be even more determining of an individual’s health than healthcare or lifestyle choices [18, 20]. Reducing (menstrual) inequities thus requires systemic changes to the SDH, addressing social, economic, and environmental conditions.
Previous research on the health outcomes posed by MI have demonstrated the risk of bacterial infections [21], barriers in the access to adequate diagnosis (and treatment) of menstrual health-related conditions (e.g. endometriosis) [22], a negative impact on mental health [2], and misinformation regarding the menstrual cycle generating subsequent negative health outcomes such as psychological stress [23]. Menstrual experiences like endometriosis, menstruations perceived to be irregular, and menstruations characterized by heavy bleeding or pain, have been demonstrated to be associated with lower quality of life and wellbeing and higher rates of mental health diagnoses [2]. In a similar manner, the experience of menstrual poverty has been shown to be associated with depressive symptoms [24], anxiety, and reproductive and urinary tract infections [25]. Additionally, Holmes et al. (2021) have demonstrated how the normalisation of certain menstrual health issues, such as dysmenorrhea, further prevents women and PWM to seek and receive proper healthcare treatment [23]. Much of this investigation focuses on geographical contexts in the Global South1, but is mainly developed, conducted, and funded by researchers and institutions in the Global North1. The formulation of research questions, the definition of research subjects, and the theoretical frameworks in menstrual studies are thus often permeated by Western cultural notions, reinforcing predominant global power structures [26–28]. Despite largely being studied in the Global South it has been demonstrated that MI transcend geographical, cultural and socioeconomic status, and therefore are equally relevant in the Global North1 [6, 23, 29].
While previous literature reviews have been looking into how menstrual management, menstrual poverty and menstrual health literacy affect the (menstrual) health of women and PWM [21, 23, 30–32], little inquiry has so far been carried out to explore how MI, as an umbrella term, may impact the health of women and PWM [6]. The aim of this scoping review is to explore and map the components of MI and their association with health outcomes in women and PWM, as reported inthe published academic literature.
Methods
A scoping review of academic literature was carried out to identify original research articles on health outcomes and their association with MI. This study followed the PRISMA guidelines (see Additional file 1) [33] and was registered in Open Science Framework (10.17605/OSF.IO/ZU73X).
Conceptual framework
This study adopts a critical feminist perspective, recognizing that systemic and structural patriarchal powers in society have an impact on health [34–36]. This approach implies using a social equity lens to conduct research that promotes collective freedom, justice, and equity [37]. Moreover, the SDH framework [38] was used to guide the identification of determinants implied in health outcomes related to menstrual experiences and health. This theoretical framework, in conjunction with the feminist perspective of the review, served as the guiding principle throughout the review process, particularly in the inductive identification of themes within the results. While the results will be presented descriptively for the purpose of facilitating comprehensibility, the structure of the analysis was informed by these frameworks.
The research has furthermore incorporated the practice of reflexivity, which included a critical examination of current approaches to MI in the literature [39]. Considering this, the research team conducted the study based on the following definitions:
Menstrual inequity: the systematic and avoidable differences in the access to menstrual healthcare, education and knowledge, products, services and facilities for menstrual management, menstrual related experiences of stigma and discrimination, and social, community, political and economic participation based on having a menstrual cycle and menstruating [6].
Health outcomes: any physical, psychological or emotional health-related symptom or condition. This is aligned with the WHO’s concept of health, defined as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [40]. This broad definition was necessary to reflect the wide variety of health implications related to the menstrual cycle and MI, including not only physical but mental and emotional health outcomes. We define emotional health based on a definition on emotional well-being as “an umbrella term for psychological concepts such as life satisfaction, life purpose, and positive emotions” [41].
Social determinants of health: the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life (e.g. economic policies and systems). The SDH have an important influence on health inequities [42, 43].
Given that SDH may influence menstrual experiences and related health outcomes [44], it is important to consider how MI are associated with health outcomes. This review is based on the perspective that health is a social issue and that social inequities determine health outcomes, which are distributed unequally across populations [7, 45]. Although the focus of the review is on inequities, the SDH framework is used to first understand how social inequities arise in relation to menstruation and menstrual health.
Searches
The search was conducted in two databases: PubMed and Scopus. The search was performed in May 2022 and updated in March 2024. This second search was conducted to include recently published articles. The search strategy included the following terms: “menstrual health and hygiene”, “menstrual hygiene management”, “menstrual management”, “menstrual health”, “menstrual poverty”, “period poverty”, “menstrual equit*”, “menstrual inequit*”, “menstrual product*”, “menstrual hygiene product*”, “menstrual education”, and “menstrual knowledge” (see Additional file 2). The search was conducted by GPD and LMP.
Study inclusion and exclusion criteria
Studies were eligible if they were [1] original research articles of qualitative, quantitative and mixed-methods methodologies [2], published until December 2023 [3], in English or Spanish [4], considered at least one health outcome associated with one menstrual inequity dimension (e.g., menstrual poverty, menstrual education, etc.), and focused on [5] women and PWM. No restrictions for age or geographical areas were applied.
Reasons for exclusion were: [1] not focused on menstruation-related SDH [2], publications not including primary data and certain study designs (protocols, evaluations, intervention/pilot studies, conference papers, guidelines, case studies, theoretical framework or questionnaire development studies, editorials, commentaries, viewpoints, systematic literature reviews or meta-analyses, and other review designs) [3], not include any mention or exploration of a relation between one menstrual inequity dimension (e.g., menstrual poverty, menstrual education, etc.) and health outcomes [4], unavailable full-text, and [5] studies not published in English or Spanish. Studies focusing solely on menstrual experiences without a reference to health consequences were not included. This allowed us to map a broad range of evidence, including descriptive studies, while staying aligned with the aim.
Screening process
A total of 4,009 articles were included in the screening process. The screening process consisted of three phases: Phase (I) Title and abstract screening, after deleting duplicates (n = 2,863); Phase (II) Full-text screening (n = 465); Phase (III) Review of full-text screening (n = 96). The screening process was conducted between May and December 2022, and between March and April 2024 (once the search was updated). At the end 74 articles were included in the review. GPD and LMP performed the whole screening process; AGE performed the full-text screening and the review of full-text screening; ASH and ABH collaborated in the full-text screening of some studies. In all screening phases, some articles were triangulated by the members of the research team. The researchers met regularly to discuss and triangulate the screening process and to resolve any disagreements in the inclusion and exclusion of articles. When consensus was not reached, a third reviewer was introduced to make the final decision. This collaborative and reflective approach ensured consistency and transparency in decision-making, in line with good practice recommended for exploratory reviews. The Rayyan software [46] was used to facilitate the screening process. See Fig. 1 for more details on the screening process.
Fig. 1.
Flow-chart of study screening process. *Several studies were excluded for multiple reasons, so the sum of these is not equivalent to the total of excluded articles
Data extraction
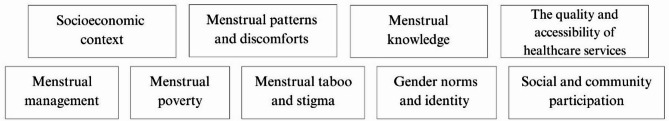
Data of the 74 articles were extracted and included in an Excel sheet by AGE, GPD, ASH, ABH, and LMP (February-October 2023), and by AGE, GPD, and ABH (April-May 2024). Data extraction included publication and methodological characteristics (authors, title, year of publication, geographical and period context, objective, methods, study population characteristics, sample, area of study), relevant findings (health outcomes, SDH and the association between health outcomes and SDH), and quality evaluations (see Table 2). The studies were classified according to different categories, which were constructed based on the definitions of MI and the SDH framework. These categories comprised: [1] socioeconomic context [2], menstrual patterns and discomforts [3], menstrual knowledge [4], the quality and accessibility of healthcare services [5], menstrual management [6], menstrual poverty [7], menstrual taboo and stigma [8], gender norms and identity, and [9] social and community participation (see Fig. 2). 22 articles were excluded at the data extraction stage, as they did not focus on health outcomes, or they did not include associations between health outcomes and menstruation-related SDH. The results were summarised according to the categories.
Table 2.
Main characteristics of included studies (n = 74)
| Reference | Country of data collection | Methodology and design | Study population | Age of participants | Sample size | Area of study | Health outcome(s) | Quality score* |
|---|---|---|---|---|---|---|---|---|
| Camas-Castillo et al., 2023 | Brazil (Campinas, São Paulo) | Quantitative (cross-sectional) | Young adult and adult women | 18-49y | n = 415 | Menstrual management | Psychological quality of life | 17/22 |
| Ssemata et al., 2023 | Uganda (Wakiso and Kalungu districts) | Qualitative (in-depth interviews, focus group discussions) | Adolescents and young adult students (girls and boys) | 15-24y | n = 274 (in-depth interviews), n = 600 (26 focus groups) | The quality and accessibility of healthcare services, Menstrual taboo and stigma | Shame, fear, feeling uncomfortable | 18/20 |
| Marí-Klose et al., 2023 | Spain (Barcelona) | Quantitative (cross-sectional) | Young adult and adult women | 15-34y | n = 647 | Menstrual poverty | Poor mental health | 22/22 |
| Schmitt et al., 2023 | United States (all territories) | Qualitative (in-depth interviews) | Young adult women | 18-25y | n = 25 | Menstrual poverty | Feeling vulnerable, anxiety | 17/20 |
| Borg et al., 2023 | Uganda (Mukono District) | Quantitative (cross-sectional) | Young adult and adult women | 18-45y | n = 499 | Menstrual management | Urogenital symptoms | 22/22 |
| Babbar et al., 2023 | India (not specified) | Qualitative (secondary analysis of qualitative data from an online survey) | Young adult and adult women | 18-49y | n = 140 | Menstrual poverty | Concern | 15/20 |
| Getahun et al., 2023 | Ethiopia (Dilla) | Qualitative (in-depth interviews) | Young adult women | Mean age 21.55y (± SD = 1.191) | n = 20 | The quality and accessibility of healthcare services | Fears of become addicted to menstrual pain medication, concern | 16/20 |
| Mohammed et al., 2023 | United States and United Kingdom (not specified) | Qualitative (critical approach to transcribed data) | Adolescent girls | 13-19y | n = 15 | The quality and accessibility of healthcare services | Uncertainty | 17/20 |
| Boden et al., 2023 | United States (St. Louis, Missouri) | Qualitative (content analysis) | Adult women | 19-65y | n = 32 | Menstrual management, Menstrual poverty, Menstrual taboo and stigma, Social and community participation | Discomfort, anxiety, embarrassment, fatigue, moodiness | 19/20 |
| ElBanna et al., 2023 | United States (St. Louis, Missouri) | Qualitative (semi-structured interviews) | Adult women | 18-50y | n = 15 | Menstrual management | Pain, embarrassment, feelings of dehumanization, (di)stress | 18/20 |
| Choudhary et al., 2023 | India (New Delhi) | Qualitative (interviews) | Young adult and adult women | 18-40y | n = 20 | Menstrual management, Menstrual taboo and stigma | Stress, frustration, anger, embarrassment, humiliation, shame, worry and concern. | 11/20 |
| Betsu et al., 2023 | Ethiopia (rural Tigray) | Qualitative (interviews, focus groups) | Adolescent girls | 13-18y | n = 79 | Menstrual taboo and stigma, Social and community participation | Menstrual anxiety, self-confidence, feeling uncomfortable | 14/20 |
| Varshney & Kimport, 2023 | United States (not specified) | Qualitative (narrative analysis) | Adolescents, young adult and adult women | 9-39y | n = 32 | The quality and accessibility of healthcare services, Social and community participation | Emotional anxiety, anxiety of feeling alone | 12/20 |
| Chan et al., 2023 | United States (all territories) | Qualitative (in-depth interviews) | Young adult and adult women | 21-50y | n = 32 | The quality and accessibility of healthcare services | Health consequences being on the wrong medication, medical trauma | 18/20 |
| Sadique et al., 2023 | Pakistan (Sindh province) | Qualitative (interviews, discussion groups) | Adolescents and adult women | Not specified | Not specified | Menstrual management, Menstrual taboo and stigma | Feeling uncomfortable, rashes, itching, vaginal infections, urinary tract infections, embarrassment, discomfort, shyness, afraid being teased by men | 13/20 |
| Hennegan et al., 2022 | Uganda (Mukono District) | Quantitative (cross-sectional) | Young adult and adult women | 18-45y | n = 600 | Menstrual management, Social and community participation | Urinary tract infections, discomfort | 22/22 |
| Winter et al., 2022 | Kenya (Mathare informal settlement, Nairobi) | Qualitative (in-depth interviews) | Young adult and adult women | 18-55y | n = 55 | Menstrual management, Menstrual taboo and stigma | Embarrassment, concern, shame, fears of harassment, fears of contracting infections, frustration | 18/20 |
| Adib-Rad et al., 2022 | Iran (not specified) | Quantitative (cross-sectional) | Young adult women | 18-20y | n = 340 | Socioeconomic context | Psychological distress | 17/22 |
| Cherenack & Sikkema, 2022 | Tanzania (not specified) | Quantitative (cross-sectional) | Adolescents and young adult women | 13-21y | n = 701 | Menstrual patterns and discomforts, Menstrual knowledge | Reproductive tract infections | 21/22 |
| Alshdaifat et al., 2022 | Jordan (all territories) | Quantitative (cross-sectional) | Young adult women | Mean age 21.6y (± SD = 2.2) | n = 594 | Menstrual patterns and discomforts | Stress | 17/22 |
| Mariappen et al., 2022 | Malaysia (Klang Valley) | Quantitative (cross-sectional) | Adolescent girls | 13-18y | n = 1,050 | Menstrual patterns and discomforts, Menstrual management | Quality of life | 16/22 |
| Buitrago-García et al., 2022 | Burkina Faso (Kossi Province) | Qualitative** (photo-elicitation) | Adolescents and young adult women | 12-28y | n = 56 (focus groups), n = 30 individual interviews | Menstrual management, Menstrual taboo and stigma | Discomfort, concern, shame, feeling unsafe, fear, humiliation. | 15/20 |
| Deriba et al., 2022 | Ethiopia (North Shewa Zone) | Qualitative** (in-depths interviews) | Adolescent girls | 13-19y | n = 12 | Menstrual knowledge, Menstrual management | Concern, fear | 16/20 |
| Ní Chéileachair et al., 2022 | Ireland (all provinces and Northern Ireland) | Qualitative (semi-structured interviews) | Adult women | ≥ 18y | n = 21 | Social and community participation | Feeling guilty, fears of discrimination | 19/20 |
| Boyers et al., 2022 | United Kingdom (England) | Qualitative (in-depth interviews, focus group discussions) | Adult women | ≥ 18y | n = 32 | Menstrual taboo and stigma | Shame, anxiety | 18/20 |
| Daniels et al., 2022 | Cambodia (2 rural provinces) | Mixed-methods (quantitative: cross-sectional; qualitative: structured interviews, focus group discussions) | Adolescent girls | ≥ 14y | n = 75 (structured interviews), n = 55 (focus group) | Menstrual knowledge, Menstrual management, Menstrual taboo and stigma, Social and community participation | Fear, shyness, discomfort, social anxiety | 18/20 |
| Swe et al., 2022 | Myanmar (Magway Region) | Mixed-methods (quantitative: cross-sectional; qualitative: structured interviews, focus group discussions) | Adolescent girls | 11-16y | n = 421 (quantitative study); n = 10 interviews, n = 10 focus groups (qualitative study) | Menstrual taboo and stigma | Shyness, embarrassment, fear, distress | 16/20 |
| McGregor & Unsworth, 2022 | Australia (urban areas, not specified) | Qualitative (semi-structured interviews) | Young adult and adult women | 16-70y | n = 6 | Menstrual management, Menstrual taboo and stigma | Confidence issues, concerns, embarrassment, awkwardness, frustration, comfortability | 15/20 |
| Schmitt et al., 2022 | United States (Chicago, Los Angeles, and New York City) | Qualitative (in-depth interviews) | Adolescent girls | 15-19y | n = 12 | Menstrual knowledge | Distress | 17/20 |
| Ames & Yon, 2022 | Peru (Huancavelica, Lima, Loreto, and Ucayli regions) | Qualitative (in-depth interviews) | Adolescent girls | 10-17y | n = 277 | Menstrual taboo and stigma | Fear of being ridiculed, discomfort, shame | 14/20 |
| Asumah et al., 2022 | Ghana (West Gonja, Savannah Region) | Qualitative (exploratory study) | Adolescent girls | 13-19y | n = 18 | Menstrual management | Discomfort and illness | 9/20 |
| Wilbur et al., 2022 | Vanuatu (Torba and Sanma Provinces) | Mixed-methods (quantitative: case-control; qualitative: in-depth interviews, focus group discussions, Photovoice) | Adolescents, young adult and adult menstruators | 10-45y | n = 164 (menstruators with disabilities), n = 169 (menstruators without disabilities) | Menstrual management, Menstrual taboo and stigma | Pain, fear, shame | 18/20 |
| Gouvernet et al., 2022 | France (not specified) | Quantitative (cross-sectional) | Adult women | 18-50y | n = 890 | Menstrual poverty | Depression and anxiety | 22/22 |
| Sommer et al., 2022 | United States (not specified) | Quantitative (cohort) | Adult women | > 18y | n = 1,496 | Menstrual poverty, Menstrual taboo and stigma | Stress | 19/22 |
| Shah et al., 2022 | Gambia (rural Kiang districts) | Mixed-methods (two cross-sectional surveys; focus group discussions, in-depth interviews, menstrual diaries, and school WASH facility observations) | Adolescents and young adult women | 11-25y (quantitative study); mean age 15.7–17.5 (qualitative study) | n = 561 (quantitative study); n = 155 (qualitative study) | Menstrual taboo and stigma, Social and community participation | Embarrassment, shame, urinary tract infection symptoms |
22/22 (quantitative) 19/20 (qualitative) |
| Trant et al., 2022 | United States (not specified) | Qualitative** (semi-structured interviews) | Adolescents and young adult women | 13-24y | n = 10 | Menstrual knowledge, Menstrual taboo and stigma | Feeling overwhelmed and scared with menstruation, fear, worry, shame. | 15/20 |
| Sharma et al., 2022 | India (Punjab) | Quantitative (cross-sectional) | Adolescents and young adult women | 15-25y | n = 2673 | Menstrual patterns and discomforts | Stress | 20/22 |
| Fernández-Martínez et al., 2022 | Spain (Andalusia region) | Qualitative (focus group discussions) | Young adult women | Mean age 22.72y (± SD = 3,46) | n = 33 | The quality and accessibility of healthcare services | Fear of medication side-effects, fear of developing dependence and tolerance of pain medication, fear of downplaying the severity of pain | 18/20 |
| Tanton et al., 2021 | Uganda (Entebbe sub-district) | Quantitative (cohort) | Adolescents and young adult women | 12-20y | n = 232 | Socioeconomic context, Menstrual knowledge, Menstrual taboo and stigma | Anxiety | 16/22 |
| Lane et al., 2021 | United States (New York City) | Qualitative (in-depth interviews) | NB/trans, young adult, adult population | 17-32y | n = 10 | Gender norms and identity | Anxiety, unsafety | 17/20 |
| Bali et al., 2021 | India (urban slum of Madhya Pradesh) | Quantitative (cross-sectional) | Adolescents and young adult women | 10-19y | n = 393 | Menstrual management | Anaemia | 18/22 |
| Gruer et al., 2021 | United States (New York City) | Qualitative (in-depth interviews) | Homeless adult women | 18-62y | n = 22 | Menstrual poverty | Shame, humiliation, experiences of sexual harassment | 18/20 |
| Wilbur et al., 2021 | Nepal (Kavrepalanchok district) | Qualitative (in-depth interviews, observation, PhotoVoice and ranking) | Adolescents and young people with disability | 15-24y | n = 20 | Menstrual knowledge, Menstrual management | Feeling uncomfortable, stress, worry, humiliation, concern | 18/20 |
| Cardoso et al., 2021 | United States (not specified) | Quantitative (cross-sectional) | Young adult women | 18-24y | n = 471 | Menstrual poverty | Depression | 20/22 |
| Nabwera et al., 2021 | The Gambia (rural Kiang districts) | Quantitative (cross-sectional) | Adolescents and young adult women | 15-21y | n = 358 | Menstrual patterns and discomforts, Menstrual management | Depression, urinary tract infections, reproductive tract infections | 21/22 |
| Briggs, 2021 | United Kingdom (Stoke-on-Trent) | Qualitative (in-depth interviews, focus group discussions) | Adolescent girls | ≥ 16y | Not specified | Menstrual poverty, Menstrual taboo and stigma | Worry, anxiety, unhappiness, embarrassment | 10/20 |
| Li et al., 2020 | Australia (Melbourne) | Qualitative (in-depth semi-structured interviews) | Adolescent girls | Mean age 14.8y, range 12–18 | n = 30 | Menstrual patterns and discomforts, Menstrual taboo and stigma, Social and community participation | Embarrassment, distress, frustration, self-consciousness, school stress. | 19/20 |
| Kim & Choi, 2020 | South Korea (Seoul and Incheon) | Quantitative (cross-sectional) | Young adult and adult women | Mean age 21y, range 17–32 | n = 383 | Menstrual management | Genitourinary infections | 22/22 |
| Hennegan & Sol, 2020 | Bangladesh (Northern Bangladesh) | Quantitative (cross-sectional data from a cluster randomised controlled trial) | Adolescent girls | Mean age 11.84y, range 10–16 | n = 1,359 | Menstrual patterns and discomforts, Menstrual management, Menstrual taboo and stigma, Gender norms and identity | Confidence to manage menstruation | 20/22 |
| Frank, 2020 | United States (Midwest, not specified) | Qualitative (virtual ethnographic approach) | NB/trans, young adult population | Mean age 22y, range 18–29 | n = 19 | The quality and accessibility of healthcare services | Dysphoric feelings, feeling unsafe | 16/20 |
| Ademas et al., 2020 | Ethiopia (Dessie City) | Quantitative (cross-sectional) | Adolescents, young adult and adult women | 16-49y | n = 602 | Menstrual management | Reproductive tract infections | 20/22 |
| Borjigen et al., 2019 | China (Changsha city) | Quantitative (cross-sectional) | Adolescent girls | 11-14y | n = 1,349 | Menstrual patterns and discomforts, Menstrual knowledge, Menstrual management | Psychological stress | 15/22 |
| Gundi & Subramanyam, 2019 | India (Nashik district) | Mixed-methods (qualitative: semi-structured interviews, focus group discussions; quantitative: cross-sectional survey) | Adolescents (girls and boys) | 13-19y | n = 1,421 (quantitative study); n = 56 (qualitative study) | Menstrual management, Menstrual taboo and stigma | Menstrual illnesses (itching, dryness, excess discharge), feeling lonely, feeling uncomfortable |
17/22 (quantitative) 18/20 (qualitative) |
| Muralidharan, 2019 | India (RG Nagar, Dharavi, central Mumbai) | Qualitative (focus group discussions, in-depth interviews) | Adolescents and young adult women | 15-24y | n = 26 | Menstrual patterns and discomforts, Menstrual knowledge, The quality and accessibility of healthcare services, Menstrual management, Menstrual taboo and stigma, Social and community participation | Stress, concern, discomfort, embarrassment, security, comfort, genital discomfort, uncomfortable | 15/20 |
| Torondel et al., 2018 | India (Odisha) | Quantitative (cross-sectional) | Young adult and adult women | 18-45y | n = 588 | Menstrual management | Reproductive tract infections | 21/22 |
| Lahme et al., 2018 | Zambia (Mongu District, Western Province) | Qualitative (focus group discussions) | Adolescents and young adult women | 13-20y | n = 51 | Menstrual knowledge, Menstrual poverty, Menstrual taboo and stigma | Humiliation, (di)stress | 16/20 |
| Amatya et al., 2018 | Nepal (Far-Western) | Qualitative** (interviews, focus group discussion, observation) | Adolescents and young adult women | 10-19y | n = 7 | Social and community participation | Psychological problems (loneliness, lack of interest, sleep difficulties, etc.), general problems (headache, diarrhea, etc.), environmental problems (snake bite, insect bite). These are problems related to Chhaupadi | 15/22 |
| Van Leeuwen & Torondel, 2018 | Greece (Ritsona) | Qualitative (semi-structured interviews, focus group discussions) | Young adult and adult women | 18-50y | n = 30 | Menstrual management, Menstrual poverty | Genital discomforts (itching), heavy bleeding, irregular periods, shame, concerns, anxiety, social exclusion | 16/20 |
| Girod et al., 2017 | Kenya (Nairobi) | Qualitative (focus group discussions) | Girl students (not specified) | Not specified, scholar age | 6–11 girls for each of 6 focus groups | Menstrual knowledge, Menstrual taboo and stigma, Gender norms and identity | Fear of urogenital tract infections, gonorrhoea, infertility, fear and anxiety of being raped and harassed, stress | 15/20 |
| Mathiyalagen et al., 2017 | India (Puducherry) | Quantitative (cross-sectional) | Adolescent girls | 12-18y | n = 242 | Menstrual management | Itching and pustules over genitalia | 13/22 |
| Schmitt et al., 2017 | Myanmar (Rakhine State) and Lebanon (Tripoli, Beirut and the Bekaa Valley) | Qualitative (focus group discussions) | Displaced (in humanitarian settings) adolescents, young adult and adult women | 14-49y | n = 39 (participatory mapping); n = 117 (women aged 19-49y), n = 39 (girls aged 14-18y) | Menstrual knowledge, Menstrual management | Genital discomforts, anxiety, feeling uncomfortable, feeling unsafe | 15/20 |
| Hennegan et al., 2017 | Uganda (Kamuli district) | Qualitative (semi-structured interviews) | Adolescent girls | 12-17y | n = 27 | Menstrual knowledge, Menstrual management, Menstrual taboo and stigma, Social and community participation | Genital discomfort (itching, irritation, abnormal discharge, burning sensation), fear, anxiety, stress, abdominal pain, embarrassment, feel confident | 17/20 |
| Hennegan et al., 2016 | Uganda (Kamuli district) | Quantitative (cross-sectional) | Adolescents and young adult women | 10-19y | n = 435 | Menstrual management | Genital discomfort (skin irritation/rashes in pelvic area, itching or burning sensation, white or green discharge, concerns about odour), fear of soiling, menstrual pain, embarrassment, shame, insecurity, difficulties to concentrate in school | 17/22 |
| Mishra et al., 2016 | India (West Bengal) | Quantitative (cross-sectional) | Adolescents and young adult women | 10-19y | n = 715 (325 rural and 390 urban areas) | Menstrual management | Gynaecological problems (burning sensation during urination, increased frequency of urination, difficulty in controlling urine, leakage of urine and itching around genitalia) | 16/22 |
| Malhotra et al., 2016 | India (Uttar Pradesh) | Quantitative (cross-sectional) | Adolescents and young adult women | 10-19y | n = 1,800 | Socioeconomic context | Attitudes or feelings of impurity during menstruation | 16/22 |
| Anand et al., 2015 | India (28 states and 6 union territories, not specified) | Quantitative (cross-sectional) | Adolescents and young adult women | 15-49y | n = 577,758 | Menstrual management | Reproductive tract infections, vaginal discharge | 17/22 |
| Ranabhat et al., 2015 | Nepal (Kailali and Bardiya districts) | Quantitative (cross-sectional) | Adolescents and young adult women | 15-49y | n = 672 | Menstrual management, Social and community participation | Reproductive health problems (reproductive tract infections, burning micturition, abnormal discharge, itching in genitalia, pain and foul-smelling menstruation) | 20/22 |
| Das et al., 2015 | India (Odisha) | Quantitative (case-control) | Young adult and adult women | 18-45y | n = 486 (228 symptomatic cases and 258 asymptomatic controls) | Menstrual management | Inflammation, reproductive tract infections, urinary tract infections, genital discomforts (e.g. vaginal discharge). | 20/22 |
| Parker et al., 2014 | Uganda (Katakwi district) | Qualitative (interviews, focus group discussions) | Adolescents and young adult women | 9-20y | n = 765 (focus groups); n = 17 (interviews) | Menstrual management, Menstrual taboo and stigma | Shame, embarrassment | 17/20 |
| Crichton et al., 2013 | Kenya (Nairobi) | Qualitative (in-depth interviews, focus group discussions) | Adolescents and adult women | 12-17y, adult women not specified | n = 87 (girls) and n = 69 (women) | Menstrual management, Menstrual poverty, Menstrual taboo and stigma, Social and community participation | Discomfort, genital discomforts (e.g. dampness, itching, irritation, rashes), concern, anxiety, embarrassment, fear of being stigmatized, low mood, emotional distress, physical discomfort | 18/20 |
| Yamamoto et al., 2009 | Japan (Fukoka) | Quantitative (cross-sectional) | Young adult women | 18-25y | n = 221 | Menstrual patterns and discomforts | Stress | 19/22 |
| Chen & Chen, 2005 | Taiwan (Tainan County) | Quantitative (cross-sectional) | Adolescents and young adult women | 15-20y | n = 198 | Socioeconomic context | Menstrual distress | 14/22 |
| Khanna et al., 2005 | India (Rajasthan) | Mixed-methods (qualitative: focus group discussion, interviews; quantitative: survey) | Adolescents and young adult women | 13-19y | n = 730 | Menstrual management, Menstrual taboo and stigma, Social and community participation | Reproductive tract infections, embarrassment, social exclusion | 13/22 |
| Warner & Bancroft, 1990 | United Kingdom (not specified) | Quantitative (cross-sectional) | Not specified, assumed adult women | Not specified | n = 5,457 | Menstrual patterns and discomforts | Premenstrual syndrome, stress | 11/22 |
*: quality score was assessed using the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields [14]. 22 items were scored for quantitative studies and 20 for qualitative studies. **: Buitrago-García et al., 2022, Deriba et al., 2022, Trant et al., 2022 and Amatya et al., 2018 used a mixed-methods design, although the cross-sectional analyses were not included for this review. Other studies’ methods may only reflect the techniques that were analysed for this review
Fig. 2.
Categories of menstrual inequities that guided the analysis
Study quality assessment
The Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields [47] was used to assess the quality of the included studies. Quantitative and qualitative studies were assessed separately, following the guide’s checklists. Mixed-methods studies were evaluated using both quantitative and qualitative checklists, if both quantitative and qualitative data were extracted. Each item was scored as follows (yes: 2; partially: 1; no: 0; not applicable) and calculated over the maximum number of points (22 for quantitative studies and 20 for qualitative studies). Table 2 displays the final score for each article.
Data synthesis and narrative analysis
The data from the 74 included articles were synthesised and organised into the identified categories. AGE, GPD, ABH, and LMP conducted the synthesis and narrative analysis; ASH and CJA collaborated in the narrative analysis. Narrative analysis is suitable to investigate the similarities and differences of findings of different studies, as well as to explore patterns in the data [48, 49]. Data are collected and presented using a textual approach to ‘tell the story’ of the findings from included studies [50], which in our study were grouped into the previously mentioned categories. The analysis process included reviewing, integrating and summarising the data extracted from articles in each category. This process was triangulated by all researchers in regular meetings, by reading the synthesis and narrative analysis of each category, making comments and resolving any doubts or disagreements between the researchers. The final analysis was unified by AGE and GPD.
Results
Study and sample characteristics
A total of 74 articles were included (see Table 2). 51 (69%) were published between 2023 − 2020 [51–101], 16 (22%) between 2019 − 2015 [102–118], three (4%) between 2014 − 2010 [119, 120], three (4%) between 2009 − 2005 [121–123], and lastly one (1%) in 1990 [124]. 35 (47%) used qualitative methods [52–57, 59, 65, 67, 68, 71, 73–75, 78, 82, 84, 87, 88, 91, 92, 95, 96, 98–101, 104, 111, 113, 115, 116, 118–120]; 30 (41%) quantitative methods [51, 60–64, 77, 78, 81, 83, 85, 86, 89, 90, 93, 94, 97, 102, 105–110, 112, 117, 121, 122, 124], and nine (12%) were mixed-methods studies [66, 69, 70, 76, 79, 80, 103, 114, 123]. Most studies included girls and women from menarche to before menopause. Other studies focused on non-binary and trans individuals [84, 95], refugees [115, 118], people with disabilities [71, 76, 88], and people experiencing homelessness [87, 100].
Articles were classified in nine categories (one article could be classified in more than one category). Six (8%) articles were included in the “socioeconomic context” category [60, 62, 81, 83, 107, 122]; 9 (12%) on “menstrual patterns and discomforts” category [61, 62, 64, 90, 92, 102, 111, 121, 124]; 13 (18%) on ”menstrual knowledge” category [61, 66, 69, 72, 76, 80, 83, 102, 104, 111, 113, 116, 118]; eight (11%) on “the quality and accessibility of healthcare services” category [52, 55, 56, 82, 95, 98, 99, 111]; 36 (49%) on “menstrual management” category [51, 53, 57–59, 64–66, 69, 71, 75, 76, 85, 86, 88, 90, 93, 94, 97, 100–102, 104–106, 108–112, 115, 117–120, 123]; 12 (16%) on ”menstrual poverty” category [63, 74, 77, 78, 87, 89, 91, 96, 100, 113, 115, 120]; 26 (35%) on ”menstrual taboo and stigma” category [52–54, 57, 59, 65, 68–71, 73, 78–80, 83, 91, 92, 94, 100, 103, 104, 111, 116, 119, 120, 123]; four (5%) on ”gender norms and identity” category [84, 94, 95, 116]; and 15 (20%) on “social and community participation” category [54, 55, 58, 67, 69, 79, 92, 100, 104, 109, 111, 113, 114, 120, 123].
20 (27%) studies were conducted in Sub-Saharan Africa [52, 54, 58, 59, 61, 65, 66, 75, 79, 83, 85, 90, 97, 98, 104, 105, 113, 116, 119]; 18 (24%) in South Asia [53, 57, 81, 86, 88, 94, 96, 103, 106–112, 114, 117, 123]; 12 (16%) in North America (all of them in the United States (US)) [55, 56, 72, 74, 78, 80, 84, 87, 89, 95, 100, 101]; 10 (14%) in the East Asia–Pacific Region [64, 69–71, 76, 92, 93, 102, 121, 122]; eight (11%) in Europe [63, 67, 68, 77, 82, 91, 115, 124]; two (3%) in North Africa–Middle East Region [60, 62]; and two (3%) in Latin America–Caribbean Region [51, 73]. Two studies (3%) were carried out across different regions [99, 118].
More than half of the studies were conducted in the Global South (48 studies, 65%), while 26 were carried out in the Global North (35%). The affiliations of the first, corresponding and last authors were from institutions in the Global North in 44 publications (59%) [53, 55, 56, 59, 61, 63, 65, 67–69, 71, 72, 74, 76–80, 82–85, 87–95, 99–101, 104, 105, 109, 115, 116, 118, 119, 121, 122, 124], in 20 (42%) cases by institutions in the Global South [51, 57, 60, 62, 66, 73, 81, 86, 96–98, 102, 103, 106–108, 111, 113, 117, 123], and in 10 (38%) cases institutions from both The Global South and Global North [52, 54, 58, 64, 70, 75, 110, 112, 114, 120]. Of the studies conducted in the Global South, 27 (56%) were affiliated with at least one institution in the Global North [52–54, 58, 59, 61, 65, 69, 70, 75, 76, 79, 83, 85, 88, 90, 94, 104, 105, 109, 110, 112, 114, 116, 118, 120], whereas none of the studies conducted in the Global North were affiliated with an institution in the Global South. The three countries that were mostly affiliated with the studies were the US (21 studies, 28%) [53–56, 59, 61, 65, 69, 72, 78, 80, 84, 87, 89, 94, 95, 100, 101, 114, 116], England (17 studies, 23%) [52, 68, 75, 76, 79, 83, 88, 90, 91, 104, 105, 110, 112, 115, 118–120] and India (12 studies, 16%) [81, 86, 96, 103, 106–108, 110–112, 117, 123]. Of the funding institutions, 36 (49%) were located in the Global North [52–56, 58, 59, 61, 65, 68–70, 72, 74, 76, 78–80, 83–85, 87–90, 92, 94, 104, 105, 107, 110, 112, 116, 118, 120, 121], eight (11%) in the Global South [51, 66, 73, 81, 97, 98, 102, 106], and only one (1%) study was funded by institutions in both the Global North and Global South [109]. 15 (20%) publications declared not having received any financial support [57, 60, 63, 64, 67, 77, 86, 91, 96, 99, 103, 111, 113, 114, 117] and in 14 (20%) cases it was not possible to determine whether there had been any funding for the study [62, 71, 75, 82, 93, 95, 100, 101, 108, 115, 119, 122–124]. The funding institutions were mainly placed in the US (16 studies, 21%) [53–55, 58, 59, 61, 69, 72, 78, 85, 87–89, 94, 116], England (12 studies, 16%) [52, 68, 79, 83, 84, 90, 104, 105, 110, 112, 118, 120] and Australia (4 studies, 5%) [70, 76, 85, 92]. 17 studies (23%) were financed by public institutions, organizations or foundations [51, 55, 65, 66, 68, 76, 79, 81, 90, 92, 97, 98, 102, 104–106, 120], 10 (14%) by private ones [56, 58, 61, 69, 72, 80, 84, 87, 88, 107], while four studies (5%) received funding from both private and public institutions [74, 78, 85, 116]. 24 studies (50%) conducted in the Global South were funded by institutions in the Global North [52–54, 58, 59, 61, 65, 69, 70, 76, 79, 83, 85, 88, 90, 94, 104, 105, 109, 110, 112, 116, 118, 120], while none of the studies in the Global North were funded by institutions in the Global South. See Table 3 for further details.
Table 3.
Main characteristics of authorship, affiliations and funding of included studies (n = 74)
| 1st author, year of publication | Data collection country | Affiliation (1st author) | Affiliation (Corresponding author) | Affiliation (last author) | Affiliation Country | Funding | Funding country |
|---|---|---|---|---|---|---|---|
| Camas-Castillo et al., 2023 | Brazil (Campinas, São Paulo) | Public university | Public university | Public university | Brazil | A public institution and a public foundation | Brazil |
| Ssemata et al., 2023 | Uganda | Public university research institute. | Public university research institute. | Public university | Uganda & Engand | Three public institutions and an independent foundation | United Kingdom |
| Marí-Klose et al., 2023 | Spain (Barcelona) | Public university | Public university | Public university | Spain | The author(s) reported no funding | - |
| Schmitt et al., 2023 | United States | Private university | Private university | Private university | United States | Two private foundations and a public institution | United States |
| Borg et al., 2023 | Uganda (Mukono District) | Private non-university research institute | Private non-university research institute | Private non-university research institute | Australia |
Private foundation. One of the authors is furthermore financed by a public institution and a private foundation |
United states & Australia |
| Babbar et al., 2023 | India | Private university | Private university | Private university | India | The author(s) reported no funding | - |
| Getahun et al., 2023 | Ethiopia | Public university | Public university | Public university | Ethiopia | Public university | Ethiopia |
| Mohammed et al., 2023 | United States, United Kingdom | Public university | Public university | Public University | Canada | The author(s) reported no funding | - |
| Boden et al., 2023 | United States | Private university | Private university | Private university | United States | This information could not be found | - |
| ElBanna et al., 2023 | United States | Non-profit healthcare organisation | Non-profit healthcare organisation | Private university | United States | This information could not be found | - |
| Choudhary et al., 2023 | India (New Delhi) | Public university | Public university | Public university | United States | Independent federal agency | United States |
| Betsu et al., 2023 | Ethiopia (rural Tigray) | Public university | Public university | Private university | Ethiopia & United States | Not-for-profit organization | United States |
| Varshney et al., 2023 | Not specified | Private university | Private university | Public university | United States | Public university | United States |
| Chan et al., 2023 | United States | Private university | Private university | Private university | United States | Funded in part by the Center for Reproductive Health Research in the Southeast (RISE) through support from an anonymous foundation | United States |
| Sadique et al., 2023 | Pakistan | Public university | Public university | Unspecified | Pakistan | The author(s) reported no funding. | - |
| Hennegan et al., 2022 | Uganda | Private non-university research institute | Private non-university research institute | Public university | Australia & Uganda | Two private foundations | United States & Sweden |
| Winter et al., 2022 | Kenya (Mathare informal settlement, Nairobi) | Private university | Private university | Private university | United States | The first author is funded by a non-profit organization | United States |
| Adib-Rad et al., 2022 | Iran | Public university | Public university | Public university | Iran | The author(s) reported no funding. | - |
| Cherenack & Sikkema 2022 | Tanzania | Private university | Private university | Private university | United States | Private university | United States |
| Alshdaifat et al., 2022 | Jordan | Public university | Public university | Private university | Jordan | This information could not be found | - |
| Mariappen et al., 2022 | Malaysia | Public university | Public university | Public university affiliated hopistal | Malaysia & Australia | The author(s) reported no funding. | - |
| Buitrago-García et al., 2022 | Burkina Faso | Public university hospital | Public university hospital | Private university | Germany & United States | Public institution | Germany |
| Deriba et al., 2022 | Ethiopia | Public university | Public university | Public university | Ethiopia | Public university | Ethiopia |
| Ní Chéileachair et al., 2022 | Ireland | Public university | Public university | Public university | Ireland | The author(s) reported no funding | - |
| Boyers et al., 2022 | United Kingdom (England) | Public university | Public university | Public university | England | Public institution | United Kingdom |
| Daniels et al., 2022 | Cambodia (2 rural provinces) | Private university | Private university | Private university | United States | Private Christian organisation | United States |
| Swe et al., 2022 | Myanmar (Magway Region) | Private non-university research institute | Private non-university research institute | Private non-university research institute | Myanmar & Australia | Two public institutions and two non-governmental organizations | Australia |
| McGregor & Unsworth, 2022 | Australia | Non-profit organisation | Public university | Public university | Australia | This information could not be found | - |
| Schmitt et al., 2022 | United States | Private university | Private university | Private university | United States | Two private foundations | United States |
| Ames & Yon, 2022 | Peru | Private university | Private university | Private university | Peru | Inter-governmental organisation |
Peru (UNICEF, Peru office) |
| Asumah et al., 2022 | Ghana | Public university | Public university | Private university hospital | Ghana & United Kingdom | This information could not be found | - |
| Wilbur et al., 2022 | Vanuatu | Public university | Public university | Public university | England | Public institution | Australia |
| Gouvernet et al., 2022 | France | Public university | Public university | Public university | France | The author(s) reported no funding | - |
| Sommer et al., 2022 | United States | Private university | Private university | Public university | United States | Private foundation, public institution and a public university | United States |
| Shah et al., 2022 | Gambia | Public university | Public university | Public university | England | Public institution | United Kingdom |
| Trant et al., 2022 | United States | Private university | Private university | Private university | United States | Private company | Italy |
| Sharma et al., 2022 | India (Punjab) | Public university | Public university | Public university | India | Public institution | India |
| Fernández-Martínez et al., 2022 | Spain | Public university | Public university | Public university | Spain | This information could not be found | - |
| Tanton et al., 2021 | Uganda | Public university | Public university | Public university | England | Three public institutions and an independent charitable organization | United Kingdom |
| Lane et al., 2021 | United States | Private university | Private university | Private university | United States | Private foundation | United Kingdom |
| Bali et al., 2021 | India | Public university | Public university | Public university | India | The author(s) reported no funding | - |
| Gruer et al., 2021 | United States (New York City) | Private university | Private university | Private university | United States | Two private foundations | United States |
| Wilbur et al., 2021 | Nepal | Public university | Public university | Public university | England | Private foundation | United States |
| Cardoso et al., 2021 | United States | Private university | Public university | Public university | United States | Non-profit organization | United States |
| Nabwera et al., 2021 | Gambia | Public university | Public university | Public university | England | Public institution | United Kingdom |
| Briggs, 2021 | United Kingdom | Public university | Public university | Public university | England | The author(s) reported no funding | - |
| Li et al., 2020 | Australia | Public university affiliated hospital | Public university affiliated hospital | Public university affiliated hospital | Australia | Two authors are funded by a public university, one author is funded by a public institution | Australia |
| Kim & Choi, 2020 | South Korea | Public university | Private university | Private university | South Korea | This information could not be found | - |
| Hennegan & Sol, 2020 | Bangladesh | Private university | Private university | Public university | United States & Netherlands | One public institution and a non-governmental organization. One author is furthermore funded by two private foundations | Sweden, United States, The Netherlands |
| Frank, 2020 | United States | Public university | Public university | Public university | United States | This information could not be found | - |
| Ademas et al., 2020 | Ethiopia (Dessie City) | Public university | Public university | Public university | Ethiopia | Public university | Ethiopoia |
| Borjigen et al., 2019 | China (Changsha city) | Public university | Public university hospital | Public university hospital | China | Two public institutions and a public university | China |
| Gundi & Subramanyam, 2019 | India (Nashik district) | Public university | Public university | Public university | India | The author(s) reported no funding | - |
| Muralidharan et al., 2019 | India (RG Nagar, Dharavi, central Mumbai) | Non-governmental organization | Non-governmental organization | Non-governmental organization | India | The author(s) reported no funding | - |
| Torondel et al., 2018 | India (Odisha) | Public university | Private university hospital | Private university hospital | India & England | A public institution and an inter-governmental organization | United Kingdom & Switzerland |
| Lahme et al., 2018 | Zambia (Mongu District, Western Province) | Unspecified | Unspecified | Public university | Zambia & South Africa | The author(s) reported no funding | - |
| Amatya et al., 2018 | Nepal (Far-Western) | Public university | Public university | Public university | Nepal & United States | The author(s) reported no funding | - |
| Van Leeuwen & Torondel, 2018 | Greece (Ritsona) | Public university | Public university | Public university | England | This information could not be found | - |
| Girod et al., 2017 | Kenya (Nairobi) | Private university | Private university | Private university | United States | A private university, a private foundation and a public institution | United States |
| Mathiyalagen et al., 2017 | India | Public university affiliated research institute | Public university affiliated research institute | Public university affiliated research institute | India | The author(s) reported no funding | - |
| Schmitt et al., 2017 | Myanmar (Rakhine State) and Lebanon (Tripoli, Beirut and the Bekaa Valley) | Private university | Private university | Private university | England | A non-profit organization, one independent charitable organization and a public institution | United Kingdom |
| Hennegan et al., 2017 | Uganda | Public university | Public university | Public university | England | Public institution | United Kingdom |
| Hennegan et al., 2016 | Uganda (Kamuli discrict) | Public university | Public university | Public university | England | Public institution | United Kingdom |
| Mishra et al., 2016 | India (West Bengal) | Public university | Public university | Public university | India | Public institution | India |
| Malhotra et al., 2016 | India (Uttar Pradesh) | Inter-governmental organisation | Inter-governmental organisation | Inter-governmental organisation | India | Private company | - |
| Anand et al., 2015 | India | Public university | Public university | Public university | India | This information could not be found | - |
| Ranabhat et al., 2015 | Nepal | Private university | Private university | Public organisation | South Korea | A non-governmental organization and a public institution | Nepal & South Korea |
| Das et al., 2015 | India (Odisha) | Private university | Public university | Public university | India & England | A public institution and an inter-governmental organization | United Kingdom |
| Parker et al., 2014 | Uganda | Public university | Public university | Non-governmental organisation | England | This information could not be found | - |
| Crichton et al., 2013 | Kenya (Nairobi) | Public university | Public university | Non-governmental organisation | England & Kenya | Public institution | United Kingdom |
| Yamamoto et al., 2009 | Japan | Public university | Public university | Private university | Japan | Independent institution | Japan |
| Chen & Chen, 2005 | Taiwan | Private university | Private university | Private university | Taiwan | This information could not be found | - |
| Khanna et al., 2005 | India (Rajasthan) | Public university | Public university | Public university | India | This information could not be found | - |
| Warner & Bancroft, 1990 | United Kingdom | Public university | Public university | Public university | Scotland | This information could not be found | - |
Moreover, quotes illustrating some qualitative findings are presented in Table 4. The definition of terms and concepts used in included articles are available in Table 5. The relevant terms and concepts are indicated in italics throughout the Results section.
Table 4.
Quotes for qualitative studies classified by categories
| Categories | References | Quotes |
|---|---|---|
| Menstrual patterns and discomforts | Li et al., 2020 | “I have trouble sleeping when I’m on my period, ‘cause that’s just constantly there and constantly waking me up, so I have to go off to the toilet again” |
| Muralidharan, 2019 | “I think everyone is worried about their periods. But I think that those who do not get their periods at all are the most stressed… People are quick to misinterpret why a girl is not menstruating… they think she is pregnant” | |
| Menstrual knowledge | Deriba et al., 2022 | “I will never forget what I experienced during my first menses; while sitting and learning in class, I noticed that blood flowed from my organ. I was terrified, confused, and fell from the bench to the ground, where my friends carried me out of the class while other students teased me and older girls told me that it was normal even if I did not believe them” |
| Trant et al., 2022 |
“I was in the bathroom doing my business and I saw blood and I was scared.” She said, “I was crying because I didn’t know if I was dying or not” “I guess I was just nervous because I didn’t know like what it was going to do like if it was going to like bleed through my pants or anything, and I was asking my friends about it, and they weren’t that experienced either, so they were kind of telling me false information making me more scared, so” |
|
| Lahme et al., 2018 | ”I was scared and terrified as I did not know what was happening to me” | |
| Schmitt et al., 2022 | “I told my auntie that there was something wrong, I explained…my severe stomach-ache and the blood on the sheets and she asked me the question: ‘Didn’t nobody ever talk to you about your period?’ And my response was ‘no, I didn’t know what that was’… I was only in third grade at the time…” | |
| The quality and the accessibility to healthcare services | Ssemata et al., 2023 | “The nurse is always rude and tough on the girls. Even when you experience severe cramps and need medical attention, the nurse will always say you are pretending and in the end, you struggle with your pain and are not helped” |
| Getahun et al., 2023 | “When I wanted to go and consult my friends, they always told me that if I use treatment, I might become addicted, so I gave up going. I mean, I live in a rural area where there is no medical treatment, so I did not go” | |
| Mohammed et al., 2023 | “I went to the doctor and I said […] ‘I’m in agony’ so the doctors recommended that I go onto birth control […], so that I wasn’t going through agony all the time, but they still just condensed that down to being just heavy periods so it was never like a label’. They just sort of shoved me off, so I didn’t come back to the doctors” | |
| Chan et al., 2023 | “It’s a woman’s issue which already gets tossed aside and it’s a mental health issue which also gets tossed aside. It’s just- it’s a double whammy of bad luck and they just don’t want to take it seriously for whatever reason.… They just wanna think it’s either brain issue or it’s a reproductive system issue and they can’t seem to connect that it’s- they’re both. They’re tied into each other. And that the body is making the brain feel this way.” | |
| Fernández-Martínez et al., 2021 | “I think they won’t consider it important, if they ask me about my cycle, my pain, if I’m not in extreme pain they’ll ask me why I want an analysis or cytology test” | |
| Frank, 2020 | “You know even when you go to the doctors now it’s, like, the first thing they ask you is when was the first day of your last period always. And I’m always like, “Why do you need to know?” [..] Like, one time I didn’t take a shit for like two weeks I was just severely constipated and I went to the doctors and they were like, “Oh you’re PMS-ing,” and I’m like, “Okay, like, that doesn’t make me feel better. Can you just like give me something to, like, get this waste out of my body?” | |
| Muralidharan, 2019 | “I like lady doctors. I can talk to them openly about my body and not be embarrassed. I can talk about my chest area or my genitals and not be embarrassed. They can understand what the problem is because they are women, too.” | |
| Menstrual management – Use of menstrual products for menstrual management | Sadique et al., 2023 | “I used homemade pads but because of the flood all our houses got destroyed, and we didn’t have anything left. We were living beside the road, all clothes were soaked and floated away. I was forced to use leaves, which was very uncomfortable, and I even got rashes and itching on my vaginal and anal area. It’s after that I had a vaginal infection” |
| Daniels et al., 2022 | “The pads turn over for [the] sticker isn’t good. The pads are thin and short, [and there is] too much blood. Accidents happen especially when sleeping and playing” | |
| Wilbur et al., 2021 | “When I sit in the wheelchair the pads may fold or something like that might happen which makes me feel uneasy […]. It becomes very uncomfortable to sit. Unlike my sisters who keep moving around, I have to sit in a place continuously. I get angry then and it gets difficult” | |
| Van Leeuwen & Torondel, 2018 | “When I use cloth, when you walk you have a problem in the groin and it is very moist and you have problems and itching” | |
| Parker et al., 2014 | “We are embarrassed to transport rags to and from school. We have no bags to put them in” | |
| Menstrual management – Menstrual care and management practices | Asumah et al., 2022 | “When it enters the vagina, you would feel some unusual pain. I just use water to wash my vagina” |
| Menstrual management – Menstrual care and management spaces | ElBanna et al., 2023 |
“I was in an alley. I was by a dumpster.… I had soiled my clothes, and uh I was changing, and I see this person walking down… I was trying to hurry up before they got close to me, and it was a guy, and he kept trying to come close and thank God I did have a knife. You know, and once he saw that knife, he kinda went about his business but it made me think if I didn’t have that knife, what would a happened, you know. I remember him calling me, ‘Oh you bloody mess’” “I feel miserable. I don’t even feel like a person anymore, I just feel like I’m existing and I just keep trying to improve my life and trying to find a job and trying to find this and trying to find that and it’s just when you get your period, it’s hot outside and you’re dirty and you can’t take care of yourself, it’s dehumanizing you know” |
| Choudhary et al., 2023 |
“I feel bad. We have to think and plan even for bathing and drinking…It’s not a good feeling. I feel bad, at least during periods. In such a water situation, you can’t work freely” “When water is not there, dishes are not washed and when someone visits and asks me why I am not cleaning them, I feel ashamed. How will I clean the dishes when water is not there!” |
|
| Sadique et al., 2023 | “I use old clothes on my period. I have no access to a washroom; therefore I use flood water to clean the vagina and wash the menstrual clothes. I don’t have the place to make it dry due to rainy weather. I have to use the wet one again and again. I experience urinary tract infection and itching” | |
| Winter et al., 2022 | “There are gaps in the door. Sometimes you will find I am standing here and somebody is in the toilet. You feel like he or she is seeing what I am doing inside there” | |
| Buitrago-García et al., 2022 |
“You already feel disgusting on your period and you come into a toilet that is again dirty, you feel even more disgusted” “I’m on my period at school, I’m not safe to change, there is no kettle to put water in (…) and it is often dirty” “It’s a little hard to manage (your period) in the bathroom, you’re not safe there because someone can open the door at any time” |
|
| Deriba et al., 2022 | “Because the school property and the latrine area are unclean and there is no water, the toilet is always dirty and unpleasant, making it unsafe to use or change modes” | |
| Daniels et al., 2022 | “At school, I feel shy, lack clean water, toilet, soap, and sanitary pad during menstruation” | |
| Van Leeuwen & Torondel, 2018 |
“In the tent, if it’s very cold and you have your period, you’re going to feel bad and it’s not comfortable. If it’s hot, you are not going to feel comfortable” “There was a girl of 16 years who lived behind my tent. She was going to the toilet to change her pad. Just when she arrived, there were a lot of young men and she dropped her pad in front of them. She came back crying. I asked her what happened, and she told me the story. For many days, she did not leave her tent” |
|
| Crichton et al., 2013 |
“If you go to the toilet and see it on the floor or the toilet basin, it is not good. It messes your day when you see it. It is a private thing and not for all to see” “It is a problem because these houses are single rooms and the whole family is there including the father. It becomes hard for them to go and change [sanitary products] and then they also don’t have toilet facilities…Maybe they will wait until night when their family are asleep]” |
|
| Menstrual poverty | Schmitt et al., 2023 | “Sometimes I would have to buy the way cheaper brand of pads that were no good at all and didn’t really work for me and I was always messing up my clothes. And I didn’t feel good at all, and it was uncomfortable…” |
| Gruer et al., 2021 | “The humiliation is that you have to keep going back to them and asking them, and when you’re asking for, because they have police and security, so it’s not private. So you’re asking for it in front of NYPD and DHS security, and most of those are male staff” | |
| Briggs, 2021 |
“They’re asking friends to bring them in for them. If you ask the girls, that’s what they’ll say, that they do bring sanitary products in for their friends as well, which is also very demeaning isn’t it? Having to ask your friend to bring in sanitary products for you?” “Yeah, it does affect you mentally. I think when it’s affecting your everyday life and you can’t do what you want, it does bring you down” |
|
| Menstrual taboo and stigma | Ssemata et al., 2023 |
“Witches use menstrual blood to cast spells on a person and one way to get this blood is from the menstrual materials. My mum told me never to dispose my pads at school or anywhere” “Some girls say they hate menstruation because it makes them feel uncomfortable sitting with boys at school especially those with the heavy flow because they are worried about bloodstains on their skirts. Some girls are really shy, they fear and will never ask a colleague for help during their menstrual periods, so they suffer in silence” |
| Betsu et al., 2023 | “Even though I am physically present in class during menstruation, I don’t follow things well and I don’t understand it [the education] well because I’m only thinking about my period, not about the class. So it affects my education. We are really afraid to stand up and do classroom activities [such as writing on the board] because we worry about being soaked with menstrual blood” | |
| Sadique et al., 2023 |
“The hygiene (menstruation kit) in our area is distributed by male social workers and as it is strictly prohibited to hide it from others, especially men and now they are distributing it. It’s quite an embarrassing situation and we are afraid of being teased by men during distribution. But I had nothing to manage my periods, so I sent my little daughter to take it” “It is convenient for the woman if menstrual products should be distributed with other items so we wouldn’t feel awkward or embarrassed. The items should be packed separately and then put in a box, so food items or other necessities have hygienic space between them. We would not feel any embarrassment if menstrual kits should be distributed privately by female workers because in our culture it is prohibited to talk to the man about menstruation” “When a heavy flood occurred, we were all wet from head to toe and it was my second day of period and in our culture it is prohibited to take a bath or wash your body during menstruation. My clothes became wet and the scrap of cloth that I used as pad for period blood leaked and stained my kamiz (shirt). I was embarrassed that I covered it with my dupatta (shawl)” |
|
| Boyers et al., 2022 | “Don’t want it leaking into your pants and then it’s on show. The embarrassment of walking round constantly checking yourself all the time” | |
| Daniels et al., 2022 |
“[I feel] shy at them [boys] because [of] blood stain during menstruation. However, I am not shy if there is no blood stain” “[I] tell teachers and ask them to go home. It helps me not to feel scared” “Teachers are not helpful because they are busy to teach and [have] no spare time” “Teachers are not helpful because students don’t tell teachers, and they [girls] feel shy.” |
|
| Swe et al., 2022 | “At first, I dare not buy. Now I buy it from a shop outside the school. Last year, I brought a pad in my school bag. But I thought it can send me to hell, and so I don’t bring it this year. I also worry that boys may see it if I keeps it in the pouch beside my bag” | |
| Ames & Yon, 2022 | “We were in physical education class. We were running, and [a girl] sat down because she was in pain. And then, she asked the teacher for permission to go to the bathroom, and when she stood up, she was all stained. My classmates began to make fun of her (…). She felt ashamed and crouched” | |
| Li et al., 2020 | “A lot of boys notice how constantly I go to the toilet for that little bit of my period… it also gets them to look at you in a different way… I don’t think anybody takes it– unless you’re on it– nobody takes it seriously as you do. And I feel like people need to take it a little bit more seriously” | |
| Muralidharan, 2019 | “I don’t want to make a mountain of a molehill, so I think to myself, let the pain continue. I just sit quietly. Crying will not make the pain go away, telling my mother will not make the pain go away. I just have to go through it” | |
| Lahme et al., 2018 | “The boys… will be laughing… wherever you pass, they will be… mocking and talking about you (being)… careless and dirty. Therefore… we are affected psychologically and become stressed and always live in fear leading to low self-esteem, hence our school performances go down. Some even stop coming to school” | |
| Parker et al., 2014 | “In the village we were able to wash and hang the rags anywhere without shame, in the camp that is very difficult” | |
| Crichton et al., 2013 | “If you don’t have pads, and maybe that day there is water shortage, you will definitely start smelling and if your parent or the people living with you smell that bad odor, they will complain and you will feel embarrassed to say you are the cause” | |
| Gender norms and identity | Frank, 2020 | “For me, that week or so of bleeding is when my gender dysphoria is at its peak. It is a continual reminder of body parts that are alien to me. It’s a reminder of all the barriers in front of me as I try to medically transition. I panic about being outed as trans whenever I get sup- plies at the drugstore. And not only that, but I am forced to directly interact with a part of my body that horrifies me — multiple times throughout the day” |
| Amatya et al., 2018 | “I don’t like to stay at the shed. There is a constant fear of the animals, snakes, and scorpions. We hear about women being raped and abused while staying in the shed” | |
| Social and community participation | Varshney & Kimport, 2023 | “This is so scary for women and you feel like you’re the only one in the world going through this […] There wasn’t anything out there about this when I was experiencing it [primary dysmenorrhea]” |
| Ní Chéileachair et al., 2022 | “You don’t want people in the workplace treated differently. If you say a period is a problem, then they won’t hire you” | |
| Li et al., 2020 | “I couldn’t leave my house, I couldn’t do anything… I didn’t really have an output to make [the menstrual pain] better. I have some mental health problems as well and I find that sport really helps… when I’m not doing sport and then I’m on my period as well, I struggle with that because I don’t have anything to put me in a positive frame of mind about it” | |
| Muralidharan, 2019 |
“When we grow up, our parents tell us to stay away from boys. Things really change after we start menstruating—we are not allowed to go out much; we are expected to stay at home; we are not allowed to spend much time with friends. Parents want to know where we are at all times” “I tolerate the pain. What else can I do? If I stay home from school, they mark me absent… this is not a good enough reason to take leave…. I get very stressed. Because I have bad cramps, I have to go to the toilet repeatedly. And the teacher in school doesn’t let you go to the toilet in the middle of class, and this is very difficult for us girls who need to go to the toilet when we have our periods. This really stresses me out” |
|
| Hennegan et al., 2017 | That sometimes, this begins when the teacher has entered in class. You need to finish the lesson, if you go out you will not get what the teacher has told, it will keep on burning until the teacher goes out | |
| Crichton et al., 2013 | “When she [mother] is under pressure it is not easy for her to listen to you. She can easily start abusing you instead.… I worry who to tell because there are some mothers who when told about periods don’t care and you are forced to go and tell someone else about it to assist you [with sanitary pads]” |
Table 5.
Table of specific terms and definitions from selected articles
| Reference | Terms and definitions |
|---|---|
| Camas-Castillo et al., 2023 |
Adequate conditions to perform menstrual hygiene outside the home: Having a private place for hygiene, soap, clean water, and disposable bins. Psychological quality of life: Measures self-image, negative thoughts, positive attitudes, self-esteem, mentality, learning ability, memory concentration, religion, and mental status. |
| Marí-Klose et al., 2023 |
Period poverty: Not being able to afford menstrual products. Poor mental health: No definition. |
| Borg et al., 2023 |
Improvised materials, clean and not reused: Those that were used only once (that is, where participants had reported that they did not wash and reuse any materials) or were cleaned appropriately, were grouped as ‘improvised materials clean or not reused’. Unclean reused materials: Any reused materials (commercially produced or improvised) that were not cleaned appropriately. |
| Boden et al., 2023 |
Homelessness: The authors critique the definition of homelessness presented by The United States Department of Housing and Urban Development: “as individuals or families living without stable or adequate housing”. They argue that this definition is too narrow and overlooks hidden forms of homelessness such as “doubling-up” (e.g. shared living arrangements). The authors rely on the study’s participants’ self-identification to validate their unique and varied experiences with homelessness. Menstrual hygiene management (MHM): Obtaining menstrual products, changing products, and controlling associated pain and increased hygiene needs (e.g. bathing and washing clothing more frequently). The authors highlight how MHM requires access to clean absorbents (e.g. tampons, pads), soap, clean water, and shelter to clean and change products safely and privately. Poor MHM then occurs when any of these needs are unmet. |
| Choudhary et al., 2023 | Dignity: The felt experience and signal to the self that one has worth and value. |
| Varshney & Kimport, 2023 | Primary dysmenorrhea: Painful menstruation in the absence of pelvic pathology. |
| Chan et al., 2023 | Premenstrual dysphoric disorder: Cyclical recurrence of distressing or impairing affective symptoms, which must appear 3–4 days before menstrual bleeding. |
| Hennegan et al., 2022 | Unmet menstrual needs: The extent to which women have access to resources and environments to care for their body which supports their preferences, comfort, privacy and safety during their last period. |
| Cherenack & Sikkema et al., 2022 |
Menstrual symptoms: Physical and psychological experiences associated with the pre-menstrual and menstrual phase, such as bloating, cramps, fatigue, and irritability Menstrual deficits: Difficulties getting menstrual supplies, a lack of education and social support, and difficulties getting money for absorbent materials or difficulties finding someone to get help or talk to about menstruation. |
| Alshdaifat et al., 2022 |
Perceived stress: The degree to which situations in a person’s life are perceived as stressful because it taps into unpredictable and uncontrollable situations in one’s life. Dysmenorrhea: Chronic pain spasmodic in nature that occurs right before or during menstruation. |
| Mariappen et al., 2022 |
Quality of life: No definition. Heavy menstrual bleeding: No definition. Dysmenorrhoea: Recurrent cramping abdominal pain associated with nausea. Amenorrhea: No definition. Oligomenorrhea: No definition. Physical and psychosocial health: No definition. |
| Daniels et al., 2022 |
Menstrual knowledge: As examples of menstrual knowledge the authors mention knowing to shower and clean with soap, use pads to prevent staining, change pads multiple times per day, dietary knowledge and the correct way to wear disposable pads, such as knowing how to properly position pads or keep them in place. Reliable menstrual products: Whether menstrual products were reliable were not defined, however the authors defined unreliable products as products with poor adhesive, inappropriate sizing, limited absorbent capacity, and failure to prevent odours. |
| McGregor & Unsworth, 2022 | Visual impairments: Having an eye condition that caused low vision or blindness. |
| Gouvernet et al., 2022 |
Menstrual poverty: The authors asked participants to indicate whether they encountered difficulties in acquiring menstrual protection during lockdown. Depression: No definition. Anxiety: No definition. |
| Sommer et al., 2022 |
Income loss: Having experienced a personal loss of income in the past month as a result of the coronavirus. Increased stress: Assessed by asking the participants whether they agreed with the following statement: “Compared to before the pandemic, getting my sanitary product is more stressful”. |
| Sharma et al., 2022 |
Amenorrhea: The absence of bleeding phase for two/three months continuously. Stress: No definition. |
| Tanton et al., 2021 | Anxiety: Operationalised as ‘anxiety about next menstrual period’ and defined according to participants stating that they agreed or strongly agreed with the following statement: “I feel anxious about having my next period”. |
| Bali et al., 2021 | Menstrual hygiene management: Adolescent girls using a clean menstrual management material to absorb or collect blood that can be changed in privacy as often as necessary for the duration of the menstruation period, using soap and water for washing the body as required, and having access to facilities to dispose of used menstrual management material. |
| Cardoso et al., 2021 |
Period poverty: Not being able to afford menstrual products. Depression: No definition. |
| Nabwera et al., 2021 |
Heavy menstrual bleeding (HMB): No definition. Depression: No definition. |
| Li et al., 2020 |
Heavy menstrual bleeding (HMB): No definition. Dysmenorrhea: No definition. |
| Hennegan & Sol, 2020 |
Confidence to manage menstruation: Girls’ level of assurance in undertaking tasks associated with managing menstrual bleeding, including collecting, washing, drying and changing menstrual materials. Gender norms: Attitudes towards gender equity and gender norms covered topics such as discrimination, social image, dominance and female education. |
| Frank, 2020 |
Gender dysphoria: No definition. Anxiety: No definition. |
| Borjigen et al., 2019 |
Psychological stress: No definition. Dysmenorrhea: No definition. Menstrual restrictions: No cold drinks, no strenuous exercise such as running and no bathing during menstruation. |
| Gundi & Subramanyam, 2019 |
Menstrual illness: Extreme pain during menstruation, itching near the genitalia, foul smell near the groyne, excess white discharge, periods multiple times in a month, periods missed or general weakness. Severe/moderate/mild taboos: Whether participants were told to follow religious restrictions, keep menstruation a secret from males in the family, sit away from the rest of the family, not touching or talking to boys during menstruation. Menstrual complaints: No clear definition, but examples of itching, dryness, excess white discharge are mentioned. |
| Muralidharan, 2019 |
Stress: No definition. Irregular menstruation: A period that occurred much earlier than expected or twice in a month, a period that was delayed by a couple of months or the absence of periods for ≥ months. |
| Torondel et al., 2018 |
Menstrual hygiene management practices: The type of absorbent material used, the frequency it is changed, associated body washing, the methods of washing, drying and storing reusable pads as well as other contextual factors, such as the location of menstruation-related changing and washing practices. Frequency of menstrual product change: The authors divide the frequency of menstrual product change into “more frequent” which is defined as 2 changes or more per day, or “less frequent”, defined as changing once per day. |
| Lahme et al., 2018 | Lozi tradition: An initiation process that girls are required to conform to at the beginning of menarche. It includes various rituals, one entailing being kept in isolation from family and friends for between 3 weeks and 6 months. |
| Amatya et al., 2018 | Chhaupadi: A tradition in far-western Nepal that entails a menstrual exile and is characterised by the “untouchability” of menstruating women and girls. It is forbidden for them to touch other people and certain objects, and they are required to live away from the community, typically in a livestock shed, during menstruation. |
| Van Leeuwen & Torondel, 2018 |
Heavy bleeding: No definition. Irregular periods: No definition. |
| Girod et al., 2017 | Menstrual management: Access to toilets, water, disposal, ablution spaces, and pads are mentioned as part of menstrual management. Furtherrmore, WASH facilities were observed to be adequate for menstrual management by assessing cleanliness, function, lighting, and privacy. |
| Mathiyalagen et al., 2017 | Satisfactory menstrual hygiene practices: Washing genitalia more than twice a day during menstruation. |
| Hennegan et al., 2017 |
Anxiety: No definition. Stress: No definition. |
| Hennegan et al., 2016 | Adequate privacy: Whether privacy for changing menstrual absorbents were adequate were understood by asking participants if they worried about being observed when washing their menstrual absorbents. When they answered “no”, privacy was considered adequate. |
| Mishra et al., 2016 |
Menstrual hygiene practices: Use of absorbent materials, cleaning and drying practices if the product was reused, frequency of change of menstrual products and cleaning practices of genitals during menstruation. Practices such as use of sanitary pads, use of detergent for cleaning of clothes/rags if reused, regular cleaning of genitals and use of pipe water for cleaning genitals were considered by the authors to be more hygienic than the use of clothes/rags, washing clothes/rags only by water for reuse, irregular cleaning of genitals and use of pond water for cleaning of genitals, respectively. Gynaecological problems: Any burning sensation during urination, increased frequency of urination, difficulty in controlling urine, leakage of urine and itching around genitalia. |
| Malhotra et al., 2016 | Attitudes or feelings of impurity during menstruation: The authors do not provide a clear definition but mention that attitudes about menstruation are measured in questions related to girs’ feelings of impurity, isolation, depression, and irritation. |
| Ranabhat et al., 2015 |
Reproductive health problems: Assessed based on the comprehensive cervical cancer control manual 2006 from WHO, and guidelines for the management of sexually transmitted infections 2003 from WHO, especially with focus on reproductive tract infection. The participants were asked whether they experienced a burning sensation during urination, severe pain and/or foul-smelling discharge during menstruation etc. Chhaupadi: Traditional practice in Nepal where menstruating women are imposed certain restrictions, such as restrictions to consume milk products; restricted access to public water sources; not being allowed to touch men, children, cattle, living plants, or fruit bearing trees; and having to live outside the home such as in an animal shed. |
| Yamamoto et al., 2009 |
Premenstrual symptoms: A constellation of physical, emotional, and behavioural symptoms which occur premenstrually and remit after the onset of bleeding. Physical symptoms included abdominal pain, headache, nausea, skin disorders, abdominal bloating, painful breast, and swelling of extremities. Emotional symptoms included irritability, anger, depression, and tension. Behavioural symptoms included increased food intake, decreased food intake, hypersomnia, lethargy, and marked lack of energy. Stress: The accumulation of somatic, psychological, and behavioural changes occurring in a person as a result of exposure to psychosocial stress. Heavy menstrual flow: No definition. Irregular menstrual cycle: Amenorrhea (menses occurring less often than every three months), long cycles (≥ 39 days) for two consecutive periods or more, short cycles (≤ 24 days) for two consecutive periods or more, and menstrual cycles too irregular to determine the cycle length. |
| Chen & Chen, 2005 | Menstrual distress: Symptoms of pain, water retention, autonomic reactions, mental distress, impaired concentration, behaviour change, and arousal. |
| Khanna et al., 2005 | Safe menstrual practices: The use of either readymade sanitary napkins or new cloths. |
| Warner & Bancroft, 1990 |
Stress: No definition. Premenstrual syndrome: No definition. Natural menstrual cycle: A menstrual cycle unmodified by oral contraceptives and uninterrupted by pregnancy. |
* It should be noted that not all the articles included in the scoping review are represented in Table 5. The table highlights terms and definitions from selected articles where the authors’ definitions were necessary to understand the review's findings.
Socioeconomic context
A study among adolescent and young adult women in India links living in a deprived district (OR = 0.29, ± 95% CI 0.23) and living in a middle economic status household (OR = 0.61, ± 95% CI 0.42) with attitudes or feelings of impurity during menstruation (Table 5) [107]. Anxiety (Table 5) about menstruation is associated with participants not living with their mother (aOR = 1.91, 95% CI 1.01–3.60) in adolescent and young adult women in Uganda [83]. Another study conducted in Iran states that one predictor for Global Severity Index (understood as equivalent to psychological distress by the authors) is mother’s education. It was also found that the severity of dysmenorrhea is associated with mother’s education (p = 0.037) in young adult women [60]. A study in Taiwan shows positive correlations between menstrual distress (Table 5) and age (b = 0.205, p < 0.001), as well as mother’s occupation (b = 0.179, p < 0.001) in adolescents and young adult women [122].
Menstrual patterns and discomforts
In Gambia, heavy menstrual bleeding (HMB) (Table 5) in adolescents and young adult women is associated with increased prevalence of depression (Table 5) (aPR = 1.4, 95% CI 1.0–1.9) and reproductive tract infections (RTIs) (aPR = 1.4, 95% CI 1.1–1.8) [90]. Similarly, a study in Malaysia report that adolescent girls with HMB, dysmenorrhea, or amenorrhea/oligomenorrhea have lower quality of life (Table 5) (70.23 ± 13.53, p = 0.001), compared to those who do not have these menstrual patterns (76.36 ± 14.93, p = 0.001). Concretely, physical health (74.10 ± 16.83 vs. 79.00 ± 15.86, p < 0.001) and psychosocial health (68.05 ± 14.27 vs. 73.21 ± 13.09, p = 0.001) (Table 5) are lower among those with HMB, dysmenorrhea, or amenorrhea/oligomenorrhea, compared to those without these menstrual patterns [64]. Amenorrhea (Table 5) is likewise shown to be associated with stress (Table 5) in adolescents and young adult women in India (OR = 1.24, 95% CI 1.06–1.44) [81]. In an Australian qualitative study, adolescents link HMB and dysmenorrhea with poorer emotional health (e.g. anxiety, worry) [92]. In another qualitative study, adolescents and young women in India report that the presence of irregular menstruations (Table 5) are associated with feelings of fear and stress (Table 5), as this might be related to premarital sex and potentially being pregnant [111]. In Japan, young adult women with premenstrual symptoms, HMB, and irregular menstrual cycles (Table 5) show higher scores of stress (Table 5). The same study shows that stress score, HMB, and menstrual pain are significant predictors for premenstrual symptoms (Table 5) (aORstress score=1.03, 95% CI 1.01–1.06; aORheavy menstrual flow=2.34, 95% CI 1.11–4.91; aORmenstrual pain=3.43, 95% CI 1.52–7.72), whereas higher stress scores (aORstress score=1.03, 95% CI 1.01–1.05) and lower body mass index (BMI) (aORBMI=0.86, 95% CI 0.77–0.97) are related to experience irregular menstrual cycles (Table 5) [121].
Dysmenorrhea (Table 5) is associated with higher psychological stress (Table 5) in adolescent girls in China, compared to those without dysmenorrhea (x̄ and SD dysmenorrhea: 21.38 ± 4.94, x̄ and SD no dysmenorrhea: 20.27 ± 4.81, p = 0.000) (102). Similar results are provided by a study in Jordan, where higher stress (Table 5) scores are correlated with the presence of dysmenorrhea (Table 5) in young adult women (rpb = 0.185, ≤ 0.001) (62). A family history of dysmenorrhea (Table 5) (OR = 2.33, 95% CI 1.43–4.15) is a predictor of the Global Severity Index (understood as equivalent to psychological distress by the authors) in young adult women in Iran (60). Besides, adolescents and young adult women from a study in Gambia report an increased prevalence of urinary tract infections (UTIs) symptoms with extreme pain during menstruation (aPR = 1.3, 95% CI 1.2–1.4) (90).
In the United Kingdom (UK), women experiencing long natural menstrual cycles (Table 5) are more likely to experience premenstrual syndrome (Table 5), and among younger women who have never given birth, those who previously used oral contraception report more PMS (premenstrual syndrome) (current users, 37%; never users; 39%, ex-users 50%; p = 0.0003). PMS is shown to be less frequent among women who recently discontinued using oral contraception. In the same study, an association between PMS and stress (Table 5) is observed (x2 = 23.3, p = 0.019) [124]. In a study in Tanzania, menstrual symptoms (e.g. irritability, cramps) (Table 5) are associated with RTIs (aOR = 1.69, 95% CI 1.21–2.36) among adolescents and young adult women [61].
Longer time since menarche (> 1 year) is associated with higher level of confidence to manage menstruation (Table 5) at home, compared to less than one year since menarche (aOR = 1.39, 95% CI 1.39–1.78) among adolescent girls in Bangladesh [94]. Another study among adolescents in China, state a correlation between higher psychological stress (Table 5) regarding menstruation and reaching menarche at a lower age (< 13 years) (x̄ and SD menarche < 13y: 20.97 ± 4.93; x̄ and SD menarche ≥ 13y: 19.92 ± 4.83, p = 0.019) (102).
Menstrual knowledge
Several studies report that misinformation about menstruation affects emotional health (e.g. fear, anxiety) at menarche [69, 72, 80, 88, 113, 118] and before menarche [66, 111]. A qualitative study in the US reveals that late and limited menstrual education from parents or at school poses consequences on mental health [80]. Similarly, another qualitative study states that adolescent girls in Cambodia with menstrual knowledge (Table 5) at the onset of menarche feel more confident about menstruation [69]. In contrast, adolescents in Uganda with lower menstrual biology knowledge are less likely to report anxiety (Table 5) about their next menstrual period (aOR = 0.44, 95% CI 0.23–0.84), compared to those with greater knowledge [83]. Similarly, another study from China states that psychological stress (Table 5) increases with menstrual knowledge in adolescent girls (b = 0.324, 95% CI 0.114–0.534) [102].
A qualitative study shows that the disparities between information provided by family and peers, compared to the information received in an educational intervention is a source of stress (Table 5) for adolescent girls in Uganda [104]. Concretely, some girls are told by their families to restrict activities during menstruation, while in the educational intervention they are recommended the contrary [104]. In a qualitative study in Kenya, girls express fear about getting infections due to poor menstrual management (Table 5), as they believe that urine splattering onto the vulva can cause UTIs, gonorrhoea, or infertility [116]. A study in Tanzania, finds that the risk of RTIs is higher among adolescents and young adult women with menstrual deficits (including the lack of menstrual education) (Table 5) (aOR = 1.91, 95% CI 1.24–2.95) [61].
The quality and accessibility of healthcare services
The (lack of) attention in healthcare systems and professionals for menstrual-related consultations results in emotional impacts (e.g. frustration, isolation) in participants of several qualitative studies [55, 56, 82, 99]. For example, the dismissal of symptoms, misdiagnosis, and other negative experiences may lead to “medical trauma” (not defined by the authors) and mistrust of doctors among young and adult women [56]. In the same study, participants elucidated the adverse health effects resulting from the administration of inappropriate medications due to the inability to obtain an accurate diagnosis (e.g. for premenstrual dysphoric disorder (Table 5)) [56]. Based on adolescents and young women narratives in India, the medical treatment is only undertaken in cases where menstrual discomfort and pain disrupt daily routines [111]. Additionally, adolescent and young girls in Uganda fear unfriendly attitudes from teachers and school nurses when they need menstrual consultations [52]. In a similar manner, menstrual healthcare services are often avoided by trans and non-binary menstruators in the US because of feeling uncomfortable and having negative encounters with healthcare providers [95].
Participants from a qualitative study in India experience barriers to healthcare access (e.g. distance from healthcare facilities and associated travel costs) which affect their emotional health (e.g. being uncomfortable, self-conscious). Furthermore, they prefer talking to women doctors to avoid embarrassment [111]. Other barriers to healthcare access are identified in Ethiopia, where young adult women avoid healthcare services because of fears of becoming addict to menstrual pain medication. These fears are especially salient in rural areas, where healthcare facilities are not generally accessible [98]. Participants with primary dysmenorrhea from a study with self-published narratives online in the US, report feeling isolated due to the lack of access to insurance for possible therapies. Moreover, according to their narratives, other extra-medical factors such as “finances, politics, education, and logistics” (not specified) complicate relief from primary dysmenorrhea [55].
Menstrual management
Use of menstrual products for menstrual management
Poor menstrual hygiene management practices (Table 5) are associated with higher prevalence of lower RTIs in young and adult women in India. Concretely, those diagnosed with Candida infection are more likely to use reusable cloths (aPRR = 1.54, 95% CI 1.2–2.0) [112]. Another study with adolescents and young adult women in India reveals that not using sanitary pads is associated with RTIs (aOR = 1.04, 95% CI 1.021–1.071) and vaginal discharge (aOR = 1.30, 95% CI 1.266–1.341) [108]. Similarly, reusable cloths are associated with inflammation (OR = 2.03, 95% CI 1.4–2.9), RTIs (aOR = 2.3, 95% CI 1.5–3.4) or having either bacterial vaginosis (BV) or UTIs (aOR = 2.8, 95% CI 1.7–4.5) in young and adult women in India [110]. A study from Uganda states that using clean/not reused materials (aPR = 1.33, 95% CI: 1.04–1.71) or unclean reused materials (Table 5) (aPR = 1.84, 95% CI: 1.46–3.42) is related to higher prevalence of self-reported urogenital symptoms, compared to using disposable pads only among young and adult women [85].
Women in a Greek refugee settlement participating in a qualitative study link having genital discomforts (e.g. itching) to using cloths made by themselves [115]. Similarly, participants from a qualitative study in Pakistan explain their sensations of genital discomforts (e.g. rashes) by the use of leaves or cloths for collecting menstrual blood that have already been used by other women [57]. Besides, participants from two different qualitative studies in Cambodia and Uganda reveal that using sanitary pads for a prolonged time increases genital discomforts [69, 104]. Moreover, adolescent girls from a qualitative study in Cambodia express that having reliable menstrual products (Table 5) available reduces emotional health impacts (e.g. shyness) about staining [69]. In a similar manner, based on the narratives of a few adolescent girls in Uganda, those whose parents regularly provide disposable pads and pain relievers express lower levels of anxiety (Table 5) [104]. Some women living in slums in India express feeling more secure using branded sanitary pads, while others preferred cloths because of greater comfort and less genital discomfort [111].
A study with adolescent girls in Bangladesh finds that using sanitary pads poses higher odds of reporting confidence to manage menstruation at home (Table 5) (aOR = 3.41, 95% CI 1.64–7.07) and at school (aOR = 2.41, 95% CI 1.54–3.87), compared to using old cloths. Girls who always/often access menstrual products at school have higher odds of confidence to manage menstruation (Table 5) at school (aOR = 4.71, 95% CI 2.11–10.49), compared to those that only occasionally have access [94]. However, in another study in Uganda, having access to sanitary pads at school was associated with an increased prevalence of UTIs (aPR = 1.4, 95% CI 1.2–1.5) [58]. Using unclean menstrual absorbents is associated with increased concerns about odour among adolescent and young adult women [105], and the absence of menstrual materials is linked to staying at home due to emotional and physical impacts (e.g. abdominal pain) in adolescent girls [104].
Psychological stress increases with a higher frequency of sanitary pads changes in adolescent girls in China (b = 0.855, 95% CI 0.243–1.468). However, the results from this study do not exhibit a clear relation between these variables [102]. Another study finds that changing menstrual products only once per day is associated with RTIs (aOR = 8.99, 95% CI 4.51–17.92) [97]. Moreover, the transportation and changing of menstrual products to school generate emotional health impacts (e.g. embarrassment) on women from a qualitative study in Uganda [119]. In a study in India, young and adult women changing menstrual products less frequently (Table 5) are more likely to have BV. Higher frequencies of menstrual products change (Table 5) are shown to be protective against infection in women with BV (aPRR = 0.56, 95% CI 0.4–0.75) [112].
The emotional impacts of menstrual management are expressed by people with disabilities in several qualitative studies [71, 76, 88]. People with mobility impairments express feeling uncomfortable regarding specific types or wrong positioning (not specified) of menstrual products [88]. Moreover, people with visual impairments explain experiencing emotional repercussions (e.g. worry) because of their difficulties with seeing potential blood stains and disposing of menstrual products discreetly [88]. A study from Australia describes how some women with visual impairments (Table 5) order menstrual products online or ask family/friends to buy them, to avoid embarrassment. However, a few participants mention feeling confident about asking supermarket staff members for assistance [71]. Participants from two studies in Vanuatu and Nepal, express feeling ashamed of relying on others to manage their menstruation [76, 88].
Menstrual care and management practices
Gynaecological problems (Table 5) are shown to be less prevalent if menstrual hygiene practices are better (Table 5) in adolescent girls in India. Those with higher levels of education (b = 0.23), age (b = 0.12), mother’s level of education (b = 0.17), father’s level of education (b = 0.28), and a monthly household income (b = 0.14), have better menstrual hygiene practices (Table 4) and less prevalence of gynaecological problems (Table 5) (b=-0.13) [106]. Moreover, unsatisfactory menstrual hygiene management (Table 5) is associated with itching in genitalia (x2 = 6.909, p = 0.009) and pustules over genitalia (x2 = 7.871, p = 0.005) in adolescent girls in India [117]. Another study among adolescent girls in urban slums in India found that poor menstrual hygiene management (Table 5) is associated with anaemia (aOR = 2.66, 95% CI 1.1–5.7) [86]. A study from India shows that the odds of RTIs increase when adolescents and young women do not engage in safe menstrual practices (Table 5) (OR = 3.07, p = 0.0000) [123]. Besides, psychological stress is demonstrated to increase when engaging in menstrual restrictions (e.g. not bathing while menstruating) (Table 5) in China (b = 0.073, 95% CI 0.032–0.114) [102]. In another study, quality of life (Table 5) is correlated with taking oral contraceptive pills for menstrual problems (Table 5) among adolescent girls (b = 7.976, 95% CI 2.691–13.260) [64].
Not washing hands with soap before touching the genital area (aOR = 3.94, 95% CI 1.49–10.45) and washing the genital area only once per day during menstruation (aOR = 5.76, 95% CI 2.07–16.05) is associated with RTIs in Ethiopia [97]. Bathing or vaginal washing only with water during menstruation is associated with genital discomforts (e.g., vaginal discharge) (OR = 2.4, 95% CI 1.01–5.7) among young and adult women in India [110]. Vaginal douching during menstruation poses a higher odds for genitourinary infections (OR = 4.93, 95% CI 1.29–18.84), and using a bidet during menstruation shows a positive association with genitourinary infections (p = 0.015) in young and adult women in South Korea [93]. Whereas, adolescent girls from a qualitative study in Ghana associate the use of soap to was the vagina with discomfort and illness [75].
Drying reusable menstrual products inside the home and keeping cloths hidden is shown to be associated with having Candida infections, compared to drying them in the sun/open space (aPRR = 1.78, 95% CI 1.34–2.38), or keeping them stored within cupboards (aPRR = 1.96, 95% CI 1.49–2.57) [112]. Similarly, one qualitative study states that participants in refugee settlements in Myanmar and Lebanon experience genital discomforts related to hiding and wearing damp cloths [118]. However, adolescent and young women in Uganda express feelings of shame associated with drying cloths outside [119]. Women from a qualitative study in Pakistan suggest that the lack of access to washrooms, clean water to clean the vagina and wash the menstrual cloths, and not having a place to dry menstrual products could be related to UTIs and itching [57]. In contrast, drying menstrual products inside the home or hiding them is associated with less white/green discharge and feeling less ashamed in a study from Uganda (OR = 0.44, 95% CI 0.21–0.91) [105].
Menstrual care and management spaces
The lack of access to inadequate facilities for changing menstrual products has an impact on the emotional health of the participants in several studies [51, 57, 58, 65, 66, 100, 101]. Young and adult women without adequate conditions to perform menstrual hygiene outside their homes (Table 5) are at higher risk to report lower psychological quality of life (Table 5) (OR = 1.01, 95%CI 1.00–1.02) in Brazil [51]. Two qualitative studies reveal that using shared public toilets or inadequate sanitation facilities (Table 5) is linked to fear of victimisation, harassment, and crime [59, 101]. Long waiting times and distances in community toilets are a concern for young and adult women because they link it to heavy bleeding, irregular periods (Table 5) and infections [115]. Based on women’s narratives in a study from Kenya, the condition of the bathroom structure (e.g. lack of privacy, lack of gender separation, inadequate access to water) has an impact on women’s emotional health (e.g. shame). Women are also concerned and anxious about the lack of gender segregated bathrooms [115, 118], as the absence of gender-segregated bathrooms is associated with shame and social exclusion [115]. Given the lack of privacy, most women express their preference to manage menstruation at home [59]. Also, changing menstrual products inside shelters/home is reported to be extremely discomforting because of the lack of privacy in other qualitative studies [57, 118, 120]. In one study, adolescents and adult women prefer public toilets, despite considering them inadequate [57].
In India, changing pads indoors (aOR = 0.56, 95% CI 0.3–0.9) decreases the likelihood to have BV [110]. In fact, UTI symptoms are shown to decrease when there is privacy in school toilets (aPR = 0.6, 95% CI 0.5–0.7) in Gambia [90]. Contrarily, adequate privacy (Table 5) for washing absorbents is associated with shame (aOR = 3.18 95% CI 1.54–6.57), insecurity (aOR = 2.16 95% CI 1.09–4.28), and difficulties to concentrate in school in Uganda (aOR = 3.03 95% CI 1.54–5.99) [105]. Lacking places to manage menstruation was related to adolescent girls feeling concerned, and sometimes leads them to skip school in Ethiopia [66]. Similarly, young and adult women with unmet menstrual needs (Table 5) are more likely to report work absenteeism and discomfort in a study in Uganda (aPR = 1.45, 95% CI 1.17–1.79) [58].
Using unclean latrines is associated with having RTIs among adolescent, young and adult women in Ethiopia (aOR = 4.20, 95% CI 2.00–8.80) [97]. Similarly, socioeconomically deprived girls experience menstrual illnesses (Table 5) due to unclean toilets in India [103]. Using dirty, shared latrines is also linked to feeling unsafe and uncomfortable, as well as to fear of kidnapping when using them at night among girls and women in refugee settlements [118]. Cleanliness at home (aOR = 2.64, 95% CI 2.04–3.42) and the presence of a bin (aOR = 1.57, 95% CI 1.01–2.44) are associated with confidence to manage menstruation among adolescent girls [94]. In the same study, the confidence to manage menstruation increases when participants feel comfortable using the toilet at school (aOR = 2.06, 95% CI 1.55–2.72) and when there is a light in the sanitation facility (aOR = 2.83, 95% CI 1.51–5.32) in Bangladesh [94]. One qualitative study in Burkina-Faso report that schoolgirls feel discomfort due to the unclean toilets, and are concerned about the availability of clean water, preferring menstrual management at home for more privacy [65]. Similar findings are reported in other studies [66, 69].
Women whose water source is outside the home are more likely to have RTIs (OR = 1.46 95% CI 1.0–2.2) [110], and more likely to have reproductive health problems (Table 5) if water is lacking during menstruation (aOR = 2.78, 95% CI 1.32–5.88) [109]. Similarly, reproductive health problems (Table 5) are associated with having no access to water during menstruation (OR = 2.78, 95% CI 1.32–5.88) in Nepal [109]. Women in India participating in a qualitative study express that the persistent lack of water in households generates emotional impacts (e.g. anger, stress) related to a perceived loss of dignity (Table 5) for not being “clean” during menstruation [53]. In a study in Gambia, girls attending schools with a water source that is only functional two-four per week (aPR = 1.4, 95% CI 1.3–1.6) have an increased prevalence of UTIs. An increase of RTIs is found when the duration to collect water at home is less than 30 min (aPR = 1.2, 95% CI 1.0–1.5), and a decrease of RTI symptoms when soap to wash hands is available in the school toilets (aPR = 0.6, 95% CI 0.5–0.8) [90].
Menstrual poverty
Period poverty (Table 5) is associated with moderate (aOR = 1.83, 95% CI 0.99–3.38) and severe depression (Table 5) (aOR = 2.34, 95% CI 1.09–4.99) among college women in the US. These associations remain significant considering the variable “previous mental health diagnosis” [89]. Period poverty is furthermore associated with poor mental health (Table 5) (aOR = 1.85, 95% CI 1.12–3.05) among young and adult women in Spain [63]. Menstrual poverty is also affecting the emotional health (e.g. fear, low mood, shame) of women in several contexts in the Global North and South [87, 91, 100, 115, 120]. Based on young women’s narratives from the UK, their social relationships are affected when asking for menstrual products, or when asking for a loan to be able to purchase them. Also, not being able to afford pain medication affect how women relate to others while in pain [91]. In two studies from the US, participants who experience homelessness (Table 5) report emotional impacts of menstrual poverty [87, 100]. Concretely, in one of the studies, women express shame, humiliation, and in some cases (sexual) harassment, when accessing menstrual products in shelters [87]. Other qualitative research highlights the genital discomforts (e.g. dampness, itching) experienced by adolescents in Kenya and Zambia when they struggle to access menstrual products and when using rags due to financial constraints [113, 120].
Additionally, menstrual poverty (Table 5) was associated with depression (Table 5) (aOR = 2.27, 95% CI 1.43 − 3.17) and anxiety (Table 5) (aOR = 1.89, 95% CI 1.18 − 3.03) in adult women during the COVID-19 lockdown in France [77]. In a study from the US, income loss (Table 5) during the COVID-19 pandemic was associated with higher odds of not being able to afford menstrual products (aOR = 3.64, 95% CI 2.14–6.19), and of experiencing increased stress (Table 5) when acquiring menstrual products (aOR = 2.2, 95% CI 1.66–2.77) in adult women. Moreover, higher odds of stress when acquiring menstrual products is related to lower educational attainment (aOR = 1.74, 95% CI 1.12–2.71) [78]. Qualitative studies also highlight the impact of menstrual poverty on emotional health during the COVID-19 pandemic [74, 96]. The emotional health of young women in the US is shown to be affected when lacking sufficient menstrual products and therefore having to rely on makeshift menstrual products due to shortages, whereas anxiety is lessened when buying menstrual products in bulk. On the other hand, many participants indicate complications in their daily routines. For instance, a few women in this study experience anxiety when using poor quality menstrual products in the workplace. In the same study, women reveal the emotional impacts (e.g. feeling vulnerable) of possible leaks caused by low quality and cheap menstrual products. Some of them shower more frequently to avoid feelings of dirtiness and fear of emitting bad odours [74]. In a study from India, one participant mentioned being concerned about requesting a male to purchase menstrual products during the lockdown [96].
Menstrual taboo and stigma
Many studies show how adolescent, young and adult women [54, 71, 73, 78, 80, 100, 111, 116, 119, 120] and PWM [76] are emotionally affected (e.g. fear, discomfort) if their menstrual status is revealed - especially to men [53, 65, 70, 123]. Based on one qualitative study, the onset of menstruation introduces gender inequities (not defined by authors) that impact the emotional health and safety of girls at school. Based on the narratives of participants of several qualitative studies, the teasing, bullying, judgement, aggression and lack of understanding by men pose an emotional impact on adolescent girls at school (e.g. stress, shame) [52, 69, 73, 92, 104], sometimes resulting in them avoiding social settings [70]. In a study in Pakistan, participants feel embarrassed to receive hygienic kits from male workers [57]. A quantitative study from Uganda shows that girls either being teased during their menstruation (aOR = 2.89, 95% CI 1.28– 6.54), or being worried about being teased during their periods pose higher odds of anxiety (aOR = 2.27, 95% CI 1.21–4.27) [83].
Other studies suggest an internalization of menstrual stigma. In Uganda, participants expressing anxiety about getting their menstruation is associated with believing it is not healthy to run, dance or cycle during menstruation (aOR = 1.83, 95% CI 0.95–3.50), and with beliefs of uncleanliness when a girl is on her period (aOR = 1.97, 95% CI 1.04–3.73) [83]. Participants from another study in Uganda report fear of being bewitched when disposing menstrual products [52].
Research amongst adolescents and young women reveal that the secrecy around menstruation results in feelings of embarrassment and shame in Gambia [79]. Likewise, a few women living in slums in India reveal feeling uncomfortable washing menstrual cloths because they perceive menstrual blood as dirty [111]. Anxiety, embarrassment and stigma is also related to fear of leakage and body odour because of infrequent change of menstrual products in Pakistan [57], the UK [68], and Kenya [120]. Women acknowledge feeling self-conscious when menstruating in public spaces, which amplifies emotional health impacts (e.g. worry) during menstruation in the UK [91]. A participant from a study in Australia expresses how menstrual taboo increased the sense of self-consciousness among adolescents with HMB and dysmenorrhea (Table 5) [92].
In India, few adolescent girls feel comfortable discussing their menstruation with school teachers. Boys seem more comfortable asking questions to a schoolteacher regarding menstruation, compared to girls (IRR = 2.38 95% CI: 1.80–3.15). Moreover, being comfortable asking questions to schoolteachers is associated with menstrual knowledge (IRR = 1.41 95% CI 1.06–1.88), and positive beliefs about menstruation (PR = 1.72 95% CI 1.19–2.49). In the same study, girls from low socioeconomic urban settings prefer to keep their menstrual complaints (Table 5) hidden, or to use home-based remedies. Feeling unable to communicate menstrual-related complaints seem to create fear, stress and body-shame amongst the girls. Higher stress about menstrual staining is present in the participants who are communicated severe menstrual taboos (Table 5) (IRR = 1.31 95% CI 1.10–1.57), compared to those who are communicated mild or no taboos (Table 5). Additionally, newly married adolescent girls share how they feel uncomfortable discussing anything related to menstruation with their husbands, which leave them feeling lonely during their menstruation [103]. Adolescents who are comfortable discussing menstruation experience higher confidence to manage menstruation at home (aOR = 2.13, 95% CI 1.61–2.82) [94]. Interestingly and contradictorily, the same study finds that discussing menstruation with a parent or guardian in the past three months is associated with lower odds of confidence to manage menstruation at home (aOR = 0.60, 95% CI 0.47–0.77), whereas having discussed it with friends in the past three months is associated with increased odds of confidence to manage menstruation at school (aOR = 1.59, 95% CI 1.21–2.09) [94]. Additionally, a qualitative study from India finds that young adults are uncomfortable discussing menstruation with their mothers [111].
Gender norms and identity
The gender norms tied to women and how they affect menstrual experiences are explored in some articles. Adolescent girls with internalised gender norms (e.g. agreeing values favouring males over females) (Table 5) predict lower confidence to manage menstruation at school (aOR = 0.96, 95% CI 0.93–0.98) and at home (aOR = 0.95, 95% CI 0.92–0.97) in Bangladesh [94]. Adolescents from a qualitative study in informal settlements in Kenya express fear of being raped and harassed from males; a fear that becomes especially triggered during menarche. Some participants disclose that they have been raped and feel unsafe in their communities [116].
Based on trans and non-binary menstrual experiences in the US, the social links of menstruation to womanhood and the gendering of menstrual products can be related to gender dysphoria (Table 5) [95]. Moreover, public toilets are considered unsafe [84] and become a source of anxiety (Table 5) [95]. A few younger trans and non-binary participants using menstrual products fear harassment if they are heard using menstrual products in bathrooms aimed for men, with some waiting to use menstrual products until they are alone [84]. Using men’s bathrooms when menstruating is considered unsafe by one participant when menstruating [95] but are still preferred due to their gender affirming nature [84, 95]. Moreover, trans and non-binary participants express feeling self-conscious using gender-segregated toilets, as they consider their bodies are being policed to ensure their gender matches with the bathroom [84].
Social and community participation
Adolescent and young girls from two studies in India reveal the emotional impacts of menstruation (e.g., stress, tension, embarrassment) due to the sociocultural implications of their communities (e.g. menstruation linked to marriage, supervised interactions) [111], and the exclusion from social activities and spaces during menstruation [123]. Another study from Nepal shows that reproductive health problems (Table 5) are associated with practising Chhaupadi (Table 5), a tradition that requires that women and girls live away from the community during menstruation (aOR = 14.6, 95% CI 6.99–30.5) [109]. In another qualitative study from Nepal, participants report mental and emotional health implications (e.g. boredom, unhappiness) when staying at a shed during Chhaupadi (Table 5) [114]. In a study from Zambia, adolescent girls report experiencing the Lozi tradition (a ritual at the onset of menarche) (Table 5) as traumatic [113].
Based on adolescent girls’ narratives in Australia, the lack of support systems at school (e.g. available medication for menstrual pain, understanding from teachers) is linked to suffering from school stress (not defined by authors) [92]. Similarly, girls from a study in Kenya report emotional health impacts (e.g. emotional distress) in school environments [120]. Moreover, self-confidence is sometimes lost during menstruation because of paying attention to menstrual blood during class [54]. This fear becomes a barrier to both concentration and participating in games [104]. In a study from Gambia, missing school during the most recent menstrual period was associated with having at least one UTIs symptom (aOR = 1.71, 95% CI 1.16–2.52) or RTIs (aOR = 1.99, 95% CI 1.34–2.94) [79]. A study in Uganda shows that young and adult women who think that women should avoid working during menstruation (aPR = 1.94, 95%CI 1.50–2.51) and should stay at home during menstruation (aPR = 1.49, 95%CI 1.02–2.18) are more likely to miss work and report discomfort [58]. Moreover, based on adult women narratives in Ireland, fears of discrimination and feelings of guilt for not remaining productive while experiencing menstrual pain are reported [67].
In a qualitative study from the US, women experiencing homelessness (Table 5) describe not socialising with friends due to fatigue and embarrassment of inadequate menstrual hygiene (Table 5) [100]. Adolescent girls from a study in Cambodia express feeling more comfortable socialising with females during menstruation, because they consider them mutually caring in contrast to males [69]. Moreover, some adolescent girls in a qualitative study in Kenya report concerns about the lack of support from their mothers [120]. Based on adolescent girls narratives’ in Australia, social and day-to-day activities during menstruation are affected due to HMB and dysmenorrhea, and often result in fatigue, low mood and feelings of isolation [92]. One participant of another qualitative study fears primary dysmenorrhea (Table 5) due to the lack of discourse and the sense that others cannot understand their pain, contributing to a sense of isolation and anxiety of feeling alone [55].
Discussion
This scoping review encompasses data from 74 original research articles that examine the relationship between MI and health outcomes in women and PWM from diverse age groups, geographical locations, and sociocultural contexts, among other characteristics. Emotional and mental health along with genitourinary tract infections were the most researched and reported health outcomes related to MI among the included studies. The preponderance of research findings indicating that mental and emotional health is one of the most frequently reported outcomes in relation to MI highlights the necessity for research that does not reduce women’s and PWM’s experiences to an emotional vulnerability inherent to the menstrual cycle. A narrow focus on biological factors alone may contribute to the perpetuation of gender stereotypes that obscure the structural factors that shape these experiences, thereby reinforcing the stigma surrounding the processes women and PWM experience. Besides, it is important to consider that MI may not be exclusively associated with the aforementioned health outcomes, but that they could also be linked to a broader range of health-related outcomes. It is important to notice that the androcentrism [125], and the hegemonic biomedical approach within academic research [36, 126, 127] have significantly hindered the development of comprehensive studies on MI from a SDH framework.
The field of menstrual research employs a multitude of terminological approaches that are not standardised. For example, the terms “menstrual hygiene” and “menstrual management” are at times used as synonyms, despite the fact that the term “hygiene” carry connotations that may be perceived as stigmatising [128]. As illustrated in Table 5, several studies included in this review showed differences in the use and understanding of menstrual research-related concepts. Given the increase of menstrual research in recent years, it is crucial that future research prioritise the refinement of conceptual frameworks and terminology employed in this field. One area that needs further attention is the conceptualisation of menstrual health [9]. In addition, this review identified deficiencies in the quality of several included articles. These included studies that failed to conceptualise menstrual health and its emotional or mental aspects. This may stem from the limited availability of validated instruments in menstrual research which can affect the way data are collected and interpreted. Addressing these gaps is fundamental for improving the quality of menstrual research and ensuring that menstrual health is comprehensively understood and effectively addressed.
One of the most notable findings from this review is the significant similarities in the relationship between MI and health outcomes across different sociocultural and geographical contexts. Although this review identifies countries where studies have been conducted, it does not provide a detailed analysis of the specific cultures within each of these countries. Moreover, it is important to challenge the culturalist perspective– the attribution of menstrual beliefs and practices solely pertaining to certain cultural, social or geographic contexts [129]. On the contrary, this continuous finding demonstrate that social conceptions of menstruation and menstrual practices cut across such contexts. A culturalist perspective may oversimplify complex phenomena by neglecting broader structural factors, which could in turn reinforce stereotypes and ethnocentric narratives. Furthermore, research that does not incorporate a critical examination of coloniality2 may be problematic, as it has the potential to misinterpret and decontextualise the findings [130]. As this scoping review demonstrates, 56% of the included studies conducted in the Global South were affiliated with at least one institution in the Global North, whereas none of the studies conducted in the Global North were affiliated with an institution in the Global South. The preponderance of institutions from the Global North studying menstruation in the Global South raises important concerns about the balance of power and agency within academic research. This means that research institutions from the Global North define the research agenda, control the funding and interpret the results. This can potentially result in imposing specific cultural worldviews and values that may not fully reflect the specific nuances of each context, inflicting a culturalist and even discriminatory perspective. The predominance of Western institutions and epistemologies in menstrual research exemplifies an epistemic injustice (systemic discrimination relating to the creation of knowledge), as the knowledge and lived experiences of women and menstruating people in the Global South are often reframed through other interpretative frameworks, limiting the reflection of diverse realities. Research initiatives led by Global North institutions may prioritise the interests of international funders. Consequently, certain studies may present Global South communities primarily through a lens of vulnerability, rather than acknowledging their agency. Even well-meaning research may inadvertently repeat power imbalances—for example, by not including local voices, keeping control of knowledge in the hands of Global North institutions, or not involving communities in deciding what to study and how to interpret it. Recognizing these imbalances is crucial for advancing a truly research agenda within menstrual research. Future research -and research teams- should critically reflect upon their positionality, promote equitable research collaborations (e.g., research led by Global South institutions and researchers), and ensure the presence of Global South epistemologies in research.
Although the majority of the findings from the included studies pertain to what could be considered “negative” experiences associated with menstruation, a few articles do highlight some more “positive” aspects, such as feelings of confidence or comfort when discussing menstruation. The paucity of research on “positive” menstrual experiences can be attributed to the negative and stigmatising connotations that menstruation entails [131] and that menstruation is often perceived as a burden rather than a health indicator [132]. This may result in the omission of positive menstrual experiences reported by some women and PWM, overlooking how SDH—such as education, social support systems, and others—can also foster positive experiences. Adopting a salutogenic perspective [133] in menstrual research and policies, which emphasises the factors that promote health and well-being, would enable the exploration of how different SDH can generate health and well-being during menstruation. Several findings on the relationship between menstrual patterns, discomforts and health outcomes are reported in this review [60–62, 64, 81, 90, 92, 94, 102, 111, 121, 124]. Some studies have reported that HMB is associated with psychological impacts (e.g. higher stress, depression), diminished quality of life, and an increased risk of RTIs. In addition, dysmenorrhoea is associated with poorer emotional/mental health (e.g. stress, worry), a reduction in quality of life, and UTI symptoms. Moreover, these relationships can be exacerbated by structural determinants of health (e.g. socioeconomic status) and other determinants like limited access to healthcare, limited access to menstrual products, social stigma surrounding menstruation, and inadequate social support [134, 135]. These findings underscore the importance of addressing MI in the broader context of SDH. They also highlight the need for comprehensive approaches that enhance both physical and emotional/mental health outcomes, while tackling the underlying structural inequities shaping menstrual experiences. Future studies should address the intersections of different dimensions of MI (e.g. menstrual patterns and access to menstrual healthcare) to better inform effective policies and interventions.
Education is a pivotal SDH, as it enables individuals to both make informed choices and reduce health inequities. Prior research has indicated that the provision of educational resources to the population can lead to enhanced health literacy, which is linked to better health outcomes [136]. Data from this review suggest that the lack of menstrual knowledge before menarche has impact on emotional/mental health [66, 111], findings that are consistent with previous evidence [23, 44, 137]. Interestingly, two studies [83, 102] in our review indicate the opposite relationship: adolescent girls with more menstrual knowledge experience higher levels of anxiety/stress. This finding raises an important question regarding the role of information, as it may suggest that excessive information, contradictory messages, or inappropriate methods and formats for conveying information could contribute to a more overwhelming experience and a detrimental impact. As other research has pointed out, menstrual education should be integrated into the school curriculum before menarche and consider the diversity of menstrual experiences of women and PWM students [45, 138]. Menstrual education should be adapted to the context and needs of individuals and should extend beyond the adolescent/school population to include the adult population, and also men and people who do not menstruate [139].
Access to healthcare is determined by several factors, all of which have an impact on health equity: socioeconomic status, education, health literacy, the availability of healthcare professionals and facilities, geographic location, government regulations and healthcare funding [140]. It is worth empathising that the structure and access to healthcare systems differs across countries (e.g. in the services offered, the cost of healthcare to users, etc.). This has an inevitable impact on increasing health inequities, through the differential access to health care systems depending on factors such as gender, race, ethnicity, administrative status, or social class of individuals and communities [141–143]. In this review, the inadequate access to healthcare and assistance for menstrual-related conditions (e.g. primary dysmenorrhea) among women and PWM is described as having an impact in emotional health [55, 56, 82, 99]. Other articles have also identified this issue amongst women living with endometriosis, which is linked to a long process of diagnosis that exacerbates discomfort and contribute to anxiety or depression [144, 145]. Many of these conditions lack specific treatments, in part because of androcentrism in health sciences [125], leading to the reliance on painkillers and hormonal contraceptives [45, 146, 147]. However, it is important to highlight the pathologisation of some menstrual experiences guided by a hegemonic biomedical approach [36, 126, 127], leading to an over-medicalisation of some women and PWM. Both the dismissal from healthcare providers– downplaying the severity of symptoms– and the scarcity of solutions offered may foster the avoidance of healthcare facilities [56, 148]. It is also important to emphasise the lack of training for healthcare professionals beyond the hegemonic biomedical model, which also has an impact on their ability to respond to these menstrual needs. In order to improve both menstrual health and the emotional/mental health of women and PWM, it is essential that healthcare services become more sensitive, accessible and depathologising.
More than half of the included studies are focused on menstrual management, revealing that this is one of the most addressed themes concerning menstruation. Consistent with the findings presented in this review, numerous studies have shown that inadequate menstrual management practices (e.g. using unclean menstrual products, prolonged use of menstrual products, inadequate access to sanitation facilities, etc.) are associated with an increased prevalence of RTIs [108]. In addition, the lack of adequate spaces for menstrual management can have a significant emotional impact on women and PWM. Although menstrual management studies approach a wide variety of aspects (access, type and frequency of change of menstrual products, or access and status of menstrual management facilities) in relation to health outcomes (e.g. RTIs), some of them largely fail to address the deeper structural factors that underlie these relationships. These structural determinants may include socioeconomic status and political instability and violence in some contexts (e.g. studies centred in menstrual management in refugee settlements). Furthermore, poverty and economic instability do not only restrict access to menstrual products but also exacerbate other health disparities. Similarly, political instability can hinder the development of sustainable menstrual management facilities, disproportionately affecting vulnerable populations by limiting their access to the essential resources for safe and healthy menstrual management [149].
Some studies have highlighted the impact of menstrual poverty on mental health (e.g. depression) [63, 77, 78, 89]. In addition, the impact of menstrual poverty on emotional health has been recognised, particularly during the COVID-19 pandemic. It is important to mention that menstrual poverty encompasses not only the access to menstrual products, but also broader issues like economic challenges and social vulnerability [150]. It is imperative that efforts to address menstrual poverty extend beyond merely providing access to menstrual products, taking into account the underlying socioeconomic vulnerabilities that significantly affect emotional health [150]. For instance, the decrease in emotional and mental well-being is often linked to inadequate living conditions and housing insecurity. Furthermore, it is crucial to acknowledge that menstrual poverty is a gendered issue, with women and PWM bearing a disproportionate burden due to systemic gender inequities, which in turn intensify their experiences of poverty [151].
Menstrual taboo and stigma, and their impact on emotional health, are widely reported in several studies [53, 54, 65, 70, 71, 73, 76, 78, 80, 100, 111, 116, 119, 120, 123]. Menstrual-related stigma is found across different regions and reveal outcomes such as fear of leakage or body odour, embarrassment to talk about menstruation with male teachers or peers, and fear of being teased or harassed due to menstruation. It is essential to recognise that menstrual taboos and stigma are rooted and maintained by gender inequities [34, 152, 153], and deepened in intersecting inequities based on race, social class and other SDH. Menstruation has generally been socially constructed as an invisible experience, which contributes to maintaining the silence, stigma and discrimination against women and PWM, and disregarding the consequent health impacts [10, 154].
On the other hand, this review’s findings also emphasize the health impacts on social and community participation [54, 55, 58, 67, 69, 92, 100, 104, 109, 111, 113, 114, 120, 123]. The role of cultural and societal values (e.g. Chhaupadi), a structural social determinant, is key in the results of this review, as it appears to have an impact on RTI prevalence and emotional health. This is consistent with previous research that has pointed out that marginalization and social exclusion have an influence on health. For instance, individuals experiencing marginalization often lack the resources needed to engage in community health, which in turn may exacerbate health disparities [155]. Fostering community engagement to build awareness and provide support systems that can improve health outcomes and strengthen social cohesion, thereby preventing social exclusion due to menstruation.
Limitations
Some limitations can be acknowledged from this study. Only two databases (Scopus and PubMed) were used to perform the searches, thus potentially leaving out important and relevant research. However, it is important to note that these two databases are the most widely used in the academic community. Another limitation is that review follows a scoping review methodology rather than a systematic review, which may also have resulted in the omission of some relevant studies. However, the selection of a scoping review is well-suited to the exploratory nature of this subject, as it permits greater flexibility in mapping and synthesising the emerging results. The integration in the review of both qualitative and quantitative studies, with diversity of samples (e.g. in ages, context) may limit the overall generalisability of the review. Nevertheless, the combination of methodologies permits the acquisition of a more comprehensive range of perspectives and evidence of the phenomenon of study. Lastly, the quality of some included articles is relatively weak, which may have an impact on the results presented. Given the relative novelty of the topic, the number of available studies is limited. It is therefore necessary to include these articles to provide an initial overview of the research field. Furthermore, the studies included in this review explicitly linked dimensions of MI with health outcomes. This has led to the exclusion of relevant and critical research in the menstrual field that did not address health outcomes. This underscores the necessity for future research that incorporates the assessment of health impacts.
Implications for research and policy
This scoping review underscores gaps in research on various aspects of MI and the impact on health outcomes. As discussed above, much of the existing literature primarily focuses on menstrual management. Other aspects that impact MI (e.g. menstrual education) are important to study with the lens of SDH and its relationship with outcomes in health. While there is a need for further research on the relationships between MI and emotional/mental health and RTIs, our review also suggests that more research is needed to investigate the relationship between MI and other potential health outcomes. Moreover, future research should delve deeper into the role of SDH, such as socioeconomic status, racism, administrative status, or gender identity, which can all shape MI and intersect with the relationship with health outcomes. It is therefore necessary that future research, policy and practice are approached from an intersectional perspective. In this sense, it is crucial to examine culturalist practices and the impact of coloniality on knowledge production, practice and policy. Furthermore, it is essential for future studies to directly address the health impacts of MI, as this relationship sometimes is not the primary focus of many studies. Indeed, it would be valuable for future research to explore the intersections and interactions among different dimensions of MI and how they can influence health outcomes. Deepening the scope of inquiry will provide a more comprehensive understanding of how menstruation-related inequities influence health. Additionally, future research should assess the effectiveness of interventions aimed at reducing MI and improving health outcomes, as evaluating such interventions can offer evidence-based insights for policymakers and practitioners seeking to address this issue. Future policies should be guided by research and consider the specific contextual factors of the populations they aim to serve. These policies should take a multifaceted approach, addressing various dimensions of MI rather than focusing on a single aspect (e.g. menstrual management). Policies must also integrate menstrual health needs into national health and gender equity agendas, ensuring that healthcare resources are distributed equitably to meet the diverse needs of women and PWM.
Conclusions
This scoping review presents an overview of the evidence available concerning the relationship between MI and health outcomes, based on a SDH framework. Many studies were concentrated on the menstrual management area and health outcomes like RTIs and emotional/mental health. It is imperative to pursue studies that more comprehensively elucidate the relationship between MI and health outcomes, as well as to investigate all potential determinants of MI through an intersectional perspective. Furthermore, this review proposes the challenge of setting aside culturalist views in menstrual research. Besides, it would be beneficial to map out a more exhaustive range of potential health outcomes (beyond emotional/mental health and RTIs) that may be associated with MI. Longitudinal studies could provide insights into the long-term health impacts of menstrual inequity. In addition, future studies should focus on better conceptualising the terminology and instruments used for assessing menstrual health and inequities, to improve the quality of menstrual research production. This research also contributes to our understanding of the impact of MI on the health of women and PWM. It is therefore vital that this relationship is translated into policymaking and healthcare professional practices. Current and future research in the field of menstruation should inform the development of evidence-based policies and community actions. In this sense, policies and community actions need to be implemented at different levels and can be carried out not only in school settings or the healthcare system but also at the community level. Furthermore, future research would benefit from adopting participatory designs and equitable collaborations, particularly when conducting research from the Global North in the Global South.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- HMB
Heavy menstrual bleeding
- MI
Menstrual inequities
- PMS
Premenstrual syndrome
- PWM
People who menstruate
- RTIs
Reproductive tract infections
- SDH
Social determinants of health
- UK
United Kingdom
- US
United States
- UTIs
Urinary tract infections
Author contributions
A.G.E.: Conceptualization, Investigation, Formal analysis, Writing– original draft; G.P.D.: Conceptualization, Investigation, Formal analysis, Writing– original draft; A.B.H.: Conceptualization, Investigation, Formal analysis, Writing– original draft; A.S.H.: Conceptualization, Investigation, Formal analysis, Writing– review & editing; C.J.A.: Conceptualization, Methodology, Formal analysis, Writing– review & editing; L.M.P.: Conceptualization, Methodology, Investigation, Formal analysis, Funding acquisition, Project administration, Supervision, Writing– original draft.
Funding
The project received a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain), awarded on the call for the creation of Health Outcomes-Oriented Cooperative Research Networks (RICORS), with reference RD21/0016/0029 (Network for Research on Chronicity, Primary Care, and Health Promotion (RICAPPS)), co-funded with European Union– Next Generation EU funds. The funders had no role in the development of the study and this manuscript.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Institut de Recerca en Atenció Primària Jordi Gol i Gurina (IDIAPJGol) (Research Institute in Primary Health Jordi Gol i Gurina). Ethical approvals were obtained on 2nd of June 2022 (REF. 19/178-P). All activities included in the study were carried out according to existing guidance in ethics as indicated in the Universal Declaration on Bioethics and Human Rights adopted by UNESCO (19/10/2005); the Council of Europe Convention for the Protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine (1997) and its additional protocol on biomedical research (2005); the Helsinki Declaration (2013) and relevant EU laws (European Parliament and Council Directive 2001/20/EC); the Spanish Law on Biomedical Research (14/2007) and the LOPD (Spanish Law on Personal Data Protection) (3/2018).
Consent for publication
Not applicable.
Competing interests
The authors declare having recently received funds from DIM Protect to support the team’s research on equity and menstrual health in Spain. DIM Protect was not involved in the conceptualization or development of this study. The authors declare no other conflict of interest.
Footnotes
The Global South is a term that refers to countries that historically have been colonised and exploited by colonial powers and which are largely (though not all) located on the southern hemisphere. These countries, mainly in Africa, Latin America, Asia, and Oceania, have been (and continue to be) subjected to economic extraction, cultural oppression and political domination by the colonisers. The Global North refers to countries that have been the main colonial powers, especially Europe and The United States of America. The terms ‘Global South’ and ‘Global North’ do not only describe economic and developmental disparities and injustices, but also reflect the historical and continuing impact of colonialism on global power dynamics.
Coloniality refers to forms of domination and control that emerged with colonialism and continue to persist even after the independence of colonies. In contrast to colonialism (which refers to the direct occupation of territories), coloniality is a broader and more enduring phenomenon that implies the continuation of the structures of power, knowledge and economic relations imposed during colonialism [156].
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Andrea García-Egea and Georgina Pujolar-Díaz joint first authorship.
References
- 1.Holst AS, Jacques-Aviñó C, Berenguera A, Pinzón-Sanabria D, Valls-Llobet C, Munrós-Feliu J et al. Experiences of menstrual inequity and menstrual health among women and people who menstruate in the Barcelona area (Spain): a qualitative study. Reprod Health. 2022;1–16. [DOI] [PMC free article] [PubMed]
- 2.Sharp GC, De Menarche GL. Menstruation, menopause and mental health (4 M): a consortium facilitating interdisciplinary research at the intersection of menstrual and mental health. Front Glob Women’s Heal. 2023;4:1258973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirin AA. Gender disparity in the funding of diseases by the U.S. National institutes of health. J Women’s Heal. 2021;30(7):956–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey AH, LaFrance M, Dovidio JF. Is man the measure of all things?? A social cognitive account of androcentrism. Personal Soc Psychol Rev. 2019;23(4):307–31. [DOI] [PubMed] [Google Scholar]
- 5.Lara-Vargas EJ. Los Viejos caminos y Las nuevas posibilidades: Marcas androcéntricas y epistemologías Feministas En Las representaciones sociales de La menstruación. Rev Estud Contemp Del Sur Glob. 2022;3(9).
- 6.Medina-Perucha L, López-Jiménez T, Jacques-Aviñó C, Holst AS, Valls-Llobet C, Munrós-Feliu J et al. Menstruation and social inequities in spain: a cross-sectional online survey-based study. Int J Equity Health. 2023;22(1):92. [DOI] [PMC free article] [PubMed]
- 7.Rossouw L, Ross H. Understanding period poverty: Socio-Economic inequalities in menstrual hygiene management in eight Low- and Middle-Income countries. Int J Environ Res Public Health. 2021;18(5). [DOI] [PMC free article] [PubMed]
- 8.Sommer M, Hirsch JS, Nathanson C, Parker RG. Comfortably, safely, and without shame: defining menstrual hygiene management as a public health issue. Am J Public Health. 2015;105(7):1302–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hennegan J, Winkler IT, Bobel C, Keiser D, Hampton J, Larsson G et al. Menstrual health: a definition for policy, practice, and research. 10.1080/2641039720211911618 2021;29(1):1911618. [DOI] [PMC free article] [PubMed]
- 10.Johnston-Robledo I, Chrisler JC. The menstrual mark: menstruation as social stigma. Palgrave Handb Crit Menstruation Stud. 2020;181–99. [PubMed]
- 11.Johnson ME. Asking the Menstruation Question to Achieve Menstrual Justice. 2021.
- 12.FIGO Ethics And Professionalism Guideline 082. Menstrual Hygiene Management| Figo [Internet]. [cited 2025 Jul 11]. Available from: https://www.figo.org/figo-ethics-and-professionalism-guideline-082-menstrual-hygiene-management
- 13.Young IM. Menstrual Meditations. In: On female body experience: Throwing like a girl and other essays. 2005. pp. 97–122.
- 14.Johnson M. Menstrual justice. UC Davis Law Rev. 2019;53: 1-79.
- 15.Winkler IT. Human rights shine a light on unmet menstrual health needs and menstruation at the margins. Obstet Gynecol. 2019;133(2):235–7. [DOI] [PubMed] [Google Scholar]
- 16.Manorama S, Desai R, Menstrual Justice. A missing element in india’s health policies. Palgrave Handb Crit Menstruation Stud. 2020;511–27. [PubMed]
- 17.Shahida. It became a cycle I was not able to break towards menstrual justice: addressing human rights violation at Indian workplaces. Int J Hum Rights Healthc. 2024;ahead-of-print(ahead-of-print)
- 18.Marmot M. The health gap: Doctors and the social determinants of health Doctors and the social determinants of health on JSTOR. Scand J Public Health. 2017;45(7):686–93. [DOI] [PubMed] [Google Scholar]
- 19.Wilkinson R, Marmot M. Introduction. In: Social Determinants of Health - The Solid Facts. 2nd ed. 2003. pp. 7–9.
- 20.World Health Organitzation. Operational framework for monitoring the social determinants of health equity. 2024.
- 21.Sumpter C, Torondel B. A systematic review of the health and social effects of menstrual hygiene management. PLoS ONE. 2013;8(4). [DOI] [PMC free article] [PubMed]
- 22.Ellis K, Wood R. A decade to wait: update on the average delay to diagnosis for endometriosis in Aotearoa new Zealand. Aust New Zeal J Obstet Gynaecol. 2024; 64(5): 524-529. [DOI] [PMC free article] [PubMed]
- 23.Holmes K, Curry C, Sherry, Ferfolja T, Parry K, Smith C, et al. Adolescent menstrual health literacy in low, middle and High-Income countries: a narrative review. Int J Environ Res Public Health. 2021;18(5):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muhaidat N, Karmi J, Al, Karam AM, Abushaikha F, Alshrouf MA. Period poverty, reuse needs, and depressive symptoms among refugee menstruators in jordan’s camps: a cross-sectional study. BMC Womens Health. 2024;24(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hennegan JM. Menstrual hygiene management and human rights: the case for an evidence-based approach. Women’s Reprod Heal. 2017;4(3):212–31. [Google Scholar]
- 26.Bobel C. The Managed Body. 2019.
- 27.McCarthy A, Lahiri-Dutt K. Bleeding in public?? Rethinking narratives of menstrual management from delhi’s slums. Palgrave Handb Crit Menstruation Stud. 2020;15–30. [PubMed]
- 28.Risling Baldy C. mini-k’iwh’e:n (For that Purpose—I consider Things): (Re)writing and (Re)righting Indigenous Menstrual Practices to Intervene on Contemporary Menstrual Discourse and the Politics of Taboo. Cult Stud ↔ Crit Methodol. 2017;17(1):21–9. [Google Scholar]
- 29.Medina-Perucha L, Jacques-Aviñó C. Salud, equidad y justicia menstrual: de Los Saberes colectivos a La legislación menstrual En España. Gac Sanit. 2024;38:102356. [DOI] [PubMed] [Google Scholar]
- 30.Ciccia D, Doyle AK, Ng CHM, Armour M. Indigenous peoples’ experience and Understanding of menstrual and gynecological health in australia, Canada and new zealand: A scoping review. Int J Environ Res Public Health. 2023;20(13):6321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hennegan J, Shannon AK, Rubli J, Schwab KJ, Melendez-Torres GJ. Women’s and girls’ experiences of menstruation in low- and middle-income countries: A systematic review and qualitative metasynthesis. PLoS Med. 2019;16(5). [DOI] [PMC free article] [PubMed]
- 32.Orsini GD, Tarabay J, Hardy-Johnson PL, Barker SL, Greenway FT. The homeless period: a qualitative evidence synthesis. Women Health. 2024;64(3):250–60. [DOI] [PubMed] [Google Scholar]
- 33.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 34.Bobel C. New blood: third-wave feminism and the politics of menstruation. 2010;238.
- 35.Blázquez Graf N, Flores Palacios F, Ríos Everardo M. Investigación Feminista. Epistemología, metodología y representaciones sociales. 2010.
- 36.Blázquez Rodríguez M, Bolaños Gallardo E. Aportes a Una antropología feminista de La salud: El estudio Del Ciclo menstrual. Salud Colect. 2017;13(2):253. [DOI] [PubMed] [Google Scholar]
- 37.García-Egea A, Holst AS, Jacques-Aviñó C, Martínez-Bueno C, Berenguera A, Vicente-Hernández MM et al. Perspectives on menstrual policymaking and community-based actions in Catalonia (Spain): a qualitative study. Reprod Health. 2024;21(1): 1. [DOI] [PMC free article] [PubMed]
- 38.Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). World Health Organization Geneva. Geneva, Switzerland; 2010.
- 39.Jootun MD, Marland G, Glenn R. Reflexivity: promoting rigour in qualitative research. 2013. [DOI] [PubMed]
- 40.World Health Organization. Constitution of the World Health Organization [Internet]. 2024 [cited 2024 Jun 17]. Available from: https://www.who.int/about/governance/constitution
- 41.Feller SC, Castillo EG, Greenberg JM, Abascal P, Mdiv RVH, Wells KB et al. Emotional Well-Being and Public Health: Proposal for a Model National Initiative. 10.1177/0033354918754540 2018;133(2):136–41. [DOI] [PMC free article] [PubMed]
- 42.World Health Organization. Social determinants of health [Internet]. Health topics. 2024 [cited 2024 Jun 17]. Available from: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
- 43.World Health Organization. Health inequities and their causes. The World Health Organization [Internet]. 2018. Available from: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes
- 44.Medina-Perucha L, López-Jiménez T, Jacques-Aviñó C, Holst AS, Valls-Llobet C, Munrós-Feliu J, et al. Menstruation and social inequities in spain: a cross-sectional online survey-based study. Int J Equity Health. 2023;22(1):1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holst AS, Jacques-Aviñó C, Berenguera A, Pinzón-Sanabria D, Valls-Llobet C, Munrós-Feliu J, et al. Experiences of menstrual inequity and menstrual health among women and people who menstruate in the Barcelona area (Spain): a qualitative study. Reprod Heal 2022 191. 2022;19(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1). [DOI] [PMC free article] [PubMed]
- 47.Kmet LM, Lee RC, Cook LS. Standard Quality Assessment Criteria for Evaluating Primary Research Papers From a Variety of Fields. 2004. Edmonton: Alberta Heritage Foundation for Medical Research. 2004.
- 48.Ryan R, Cochrane Consumers and Communication Review Group. Cochrane Consumers and Communication Review Group: data synthesis and analysis. 2013.
- 49.Riessman CK. Narrative methods for the human sciences. Sage; 2008.
- 50.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M et al. uidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme. London; 2006.
- 51.Camas-Castillo MA, Gallardo-Alvarado N, Yánez-Sánchez P, Makuch MY, Osis MJD, Bahamondes L. Menstrual health: inequities in a cohort of menstruating people in the Brazilian southeastern region. Int J Gynecol Obstet. 2023;164(3):1160–6. [DOI] [PubMed] [Google Scholar]
- 52.Ssemata AS, Ndekezi D, Kansiime C, Bakanoma R, Tanton C, Nelson KA, et al. Understanding the social and physical menstrual health environment of secondary schools in uganda: A qualitative methods study. PLOS Glob Public Heal. 2023;3(11):e0002665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Choudhary N, SturtzSreetharan C, Trainer S, Brewis A, Wutich A, Clancy K et al. Managing menstruation with dignity: worries, stress and mental health in two water-scarce urban communities in India. Glob Public Health. 2023;18(1). [DOI] [PubMed]
- 54.Betsu BD, Wall LL, Medhanyie AA, Gebrehiwet TG. Menstruation is a fearful thing: A qualitative exploration of menstrual experiences and sources of information about menstruation. Among Adolesc Schoolgirls. 2023;15: 881-892. [DOI] [PMC free article] [PubMed]
- 55.Varshney J, Kimport K. Patients’ perspectives on clinical responses to primary dysmenorrhea: a qualitative analysis of online narratives. Women’s Reprod Heal. 2023;10(2):252–63. [Google Scholar]
- 56.Chan K, Rubtsova AA, Clark CJ. Exploring diagnosis and treatment of premenstrual dysphoric disorder in the U.S. Healthcare system: a qualitative investigation. BMC Womens Health. 2023;23(1):272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sadique S, Ali I, Ali S. Managing menstruation during natural disasters: menstruation hygiene management during super floods in Sindh Province of Pakistan. J Biosoc Sci. 2024; 56 (3): 480-492.. [DOI] [PubMed]
- 58.Hennegan J, Bukenya JN, Makumbi FE, Nakamya P, Exum NG, Schwab KJ, et al. Menstrual health challenges in the workplace and consequences for women’s work and wellbeing: a cross-sectional survey in mukono, Uganda. PLOS Glob Public Heal. 2022;2(7):e0000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Winter SC, Sommer M, Obara LM, Nair D. There is no place to dispose them. What would you have me do?’’: A qualitative study of menstruation in the unique physical and social environment in informal settlements in nairobi, Kenya. Heal Place. 2022;78(November):102932. [DOI] [PubMed] [Google Scholar]
- 60.Adib-Rad H, Kheirkhah F, Faramarzi M, Omidvar S, Basirat Z, Haji Ahmadi M. Primary dysmenorrhea associated with psychological distressin medical sciences students in the North of iran:a Cross-Sectional study. Int J Fertil Steril. 2022;16(3):224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cherenack EM, Sikkema KJ. Puberty- and menstruation-related stressors are associated with depression, anxiety, and reproductive tract infection symptoms among adolescent girls in Tanzania. Int J Behav Med. 2022;29(2):160–74. [DOI] [PubMed] [Google Scholar]
- 62.Alshdaifat E, Absy N, Sindiani A, Alosta N, Hijazi H, Amarin Z, et al. Premenstrual syndrome and its association with perceived stress: the experience of medical students in Jordan. Int J Womens Health. 2022;14:777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Marí-Klose M, Julià A, Escapa S, Gallo P. Period poverty and mental health in a representative sample of young women in barcelona, Spain. BMC Womens Health. 2023;23(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mariappen U, Chew KT, Zainuddin AA, Mahdy ZA, Abdul Ghani NA, Grover S. Quality of life of adolescents with menstrual problems in Klang valley, malaysia: a school population-based cross-sectional study. BMJ Open. 2022;12(1):e051896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Buitrago-García T, Sawadogo NH, Souares A, Koulidiati JL, Sié A, Bärnighausen T et al. Female-friendly toilets in schools in Burkina faso: A mixed-methods study using photo-elicitation. J Glob Health. 2022;12. [DOI] [PMC free article] [PubMed]
- 66.Deriba BS, Garedew G, Gemeda D, Geleta TA, Jemal K, Bala ET et al. Safe menstrual hygiene management practice and associated factors among female adolescent students at high schools in central ethiopia: A mixed-method study. Front Public Heal. 2022;10. [DOI] [PMC free article] [PubMed]
- 67.Ní Chéileachair F, McGuire BE, Durand H. Coping with dysmenorrhea: a qualitative analysis of period pain management among students who menstruate. BMC Womens Health. 2022;22(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Boyers M, Garikipati S, Biggane A, Douglas E, Hawkes N, Kiely C et al. Period poverty: the perceptions and experiences of impoverished women living in an inner-city area of Northwest England. PLoS ONE. 2022;17(7). [DOI] [PMC free article] [PubMed]
- 69.Daniels G, MacLeod M, Cantwell RE, Keene D, Humprhies D. Navigating fear, shyness, and discomfort during menstruation in Cambodia. PLOS Glob Public Heal. 2022;2(6):e0000405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Swe ZY, Mon NO, Than KK, Azzopardi PS, Kennedy EC, Davis J et al. Adolescent girls’ experiences of menstruation and schooling in monastic schools in Magway region, myanmar: a mixed-methods exploration. Front Reprod Heal. 2022;4. [DOI] [PMC free article] [PubMed]
- 71.McGregor FA, Unsworth CA. Menstrual hygiene management strategies used by women who are blind or have low vision. Scand J Occup Ther. 2022;29(7):598–610. [DOI] [PubMed] [Google Scholar]
- 72.Schmitt ML, Gruer C, Hagstrom C, Ekua Adenu-Mensah N, Nowara A, Keeley K, et al. It always gets pushed aside: qualitative perspectives on puberty and menstruation education in U.S.A. Schools. Front Reprod Heal. 2022;4:1018217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ames P, Yon C. Experiences of menstruation and schooling among female adolescents in peru: contributions from an ecological and gender perspective. Cogent Educ. 2022;9(1).
- 74.Schmitt ML, Dimond K, Maroko AR, Phillips-Howard PA, Gruer C, Berry A, et al. I stretch them out as long as possible: U.S. Women’s experiences of menstrual product insecurity during the COVID-19 pandemic. BMC Womens Health. 2023;23(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Asumah MN, Abubakari A, Aninanya GA, Salisu WJ. Perceived factors influencing menstrual hygiene management among adolescent girls: a qualitative study in the West Gonja municipality of the Savannah region, Ghana. Pan Afr Med J. 2022;41: 146. [DOI] [PMC free article] [PubMed]
- 76.Wilbur J, Morrison C, Iakavai J, Shem J, Poilapa R, Bambery L, et al. The weather is not good: exploring the menstrual health experiences of menstruators with and without disabilities in Vanuatu. Lancet Reg Heal - West Pac. 2022;18:100325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gouvernet B, Sebbe F, Chapillon P, Rezrazi A, Brisson J. Period poverty and mental health in times of Covid-19 in France. Health Care Women Int. 2022;44(5):657–69. [DOI] [PubMed] [Google Scholar]
- 78.Sommer M, Phillips-Howard PA, Gruer C, Schmitt ML, Nguyen A-MM, Berry A, et al. Menstrual product insecurity resulting from COVID-19–Related income loss, united states, 2020. Am J Public Health. 2022;112(4):675–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shah V, Nabwera H, Sonko B, Bajo F, Faal F, Saidykhan M, et al. Effects of menstrual health and hygiene on school absenteeism and drop-out among adolescent girls in rural Gambia. Int J Environ Res Public Health. 2022;19(6):1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Trant AA, Vash-Margita A, Camenga D, Braverman P, Wagner D, Espinal M, et al. Menstrual health and hygiene among adolescents in the united States. J Pediatr Adolesc Gynecol. 2022;35(3):277–87. [DOI] [PubMed] [Google Scholar]
- 81.Sharma P, Kaur M, Kumar S, Khetarpal P. A cross-sectional study on prevalence of menstrual problems, lifestyle, mental health, and PCOS awareness among rural and urban population of punjab, India. J Psychosom Obstet Gynecol. 2022;43(3):349–58. [DOI] [PubMed] [Google Scholar]
- 82.Fernández-Martínez E, Pérez-Corrales J, Palacios-Ceña D, Abreu-Sánchez A, Iglesias-López MT, Carrasco-Garrido P, et al. Pain management and coping strategies for primary dysmenorrhea: a qualitative study among female nursing students. Nurs Open. 2022;9(1):637–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tanton C, Nakuya K, Kansiime C, Hytti L, Torondel B, Francis SC, et al. Menstrual characteristics, menstrual anxiety and school attendance among adolescents in uganda: a longitudinal study. BMC Womens Health. 2021;21(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lane B, Perez-Brumer A, Parker R, Sprong A, Sommer M. Improving menstrual equity in the USA: perspectives from trans and non-binary people assigned female at birth and health care providers. Cult Heal Sex. 2022;24(10):1408–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Borg SA, Bukenya JN, Kibira SPS, Nakamya P, Makumbi FE, Exum NG, et al. The association between menstrual hygiene, workplace sanitation practices and self-reported urogenital symptoms in a cross-sectional survey of women working in Mukono district, Uganda. PLoS ONE. 2023;18(7 July):1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bali S, Sembiah S, Jain A, Alok Y, Burman J, Parida D. Is there any relationship between poor menstrual hygiene management and Anemia? - A quantitative study among adolescent girls of the urban slum of Madhya Pradesh. Indian J Community Med. 2021;46(3):550–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gruer C, Hopper K, Smith RC, Kelly E, Maroko A, Sommer M. Seeking menstrual products: a qualitative exploration of the unmet menstrual needs of individuals experiencing homelessness in new York City. Reprod Health. 2021;18(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wilbur J, Kayastha S, Mahon T, Torondel B, Hameed S, Sigdel A et al. Qualitative study exploring the barriers to menstrual hygiene management faced by adolescents and young people with a disability, and their carers in the Kavrepalanchok district, Nepal. BMC Public Health. 2021;21(1): 476. [DOI] [PMC free article] [PubMed]
- 89.Cardoso LF, Scolese AM, Hamidaddin A, Gupta J. Period poverty and mental health implications among college-aged women in the united States. BMC Womens Health. 2021;21(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nabwera HM, Shah V, Neville R, Sosseh F, Saidykhan M, Faal F et al. Menstrual hygiene management practices and associated health outcomes among school-going adolescents in rural Gambia. PLoS ONE. 2021;16(2). [DOI] [PMC free article] [PubMed]
- 91.Briggs A. Period poverty in stoke-on-trent, UK: new insights into gendered poverty and the lived experiences of austerity. J Poverty Soc Justice. 2021;29(1):85–102. [Google Scholar]
- 92.Li AD, Bellis EK, Girling JE, Jayasinghe YL, Grover SR, Marino JL, et al. Unmet needs and experiences of adolescent girls with heavy menstrual bleeding and dysmenorrhea: A qualitative study. J Pediatr Adolesc Gynecol. 2020;33(3):278–84. [DOI] [PubMed] [Google Scholar]
- 93.Kim KM, Choi JS. Female university students’ menstrual-hygiene management and factors associated with genitourinary-tract infections in Korea. Women Heal. 2020;60(5):559–69. [DOI] [PubMed] [Google Scholar]
- 94.Hennegan J, Sol L. Confidence to manage menstruation at home and at school: findings from a cross-sectional survey of schoolgirls in rural Bangladesh. Cult Health Sex. 2020;22(2):146–65. [DOI] [PubMed] [Google Scholar]
- 95.Frank SE. Queering menstruation: trans and non-binary identity and body politics. Sociol Inq. 2020;90(2):371–404. [Google Scholar]
- 96.Babbar K, Swathysree SS, Nanduri K. Navigating through menstrual health experiences of educated urban individuals who menstruate during the COVID-19 lockdown: a study from India. Cult Heal Sex. 2023;0(0):1–12. [DOI] [PubMed] [Google Scholar]
- 97.Ademas A, Adane M, Sisay T, Kloos H, Eneyew B, Keleb A, et al. Does menstrual hygiene management and water, sanitation, and hygiene predict reproductive tract infections among reproductive women in urban areas in ethiopia?? PLoS ONE. 2020;15(8 August 2020):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Getahun SB, Berhe S, Mekonnen B, Melaku G. Reasons for not seeking healthcare among students with dysmenorrhea: a qualitative study. Int J Womens Health. 2023;15:1733–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mohammed SS, Gagnon MM, Cummings JA. You’re not alone: how adolescents share dysmenorrhea experiences through vlogs. Qual Health Res. 2023; 34 (6): 540-551. [DOI] [PMC free article] [PubMed]
- 100.Boden L, Wolski A, Rubin AS, Oliveira LP, Tyminski QP. Exploring the barriers and facilitators to menstrual hygiene management for women experiencing homelessness. J Occup Sci. 2023;30(2):235–50. [Google Scholar]
- 101.ElBanna B, Dell NA, Klier M. Menstrual hygiene management among homeless women with mental illness in st. Louis metropolitan area: A qualitative st.dy. Women’s Reprod Heal. 2023;10(3):385–401. [Google Scholar]
- 102.Borjigen A, Huang C, Liu M, Lu J, Peng H, Sapkota C, et al. Status and factors of menstrual knowledge, attitudes, behaviors and their correlation with psychological stress in adolescent girls. J Pediatr Adolesc Gynecol. 2019;32(6):584–9. [DOI] [PubMed] [Google Scholar]
- 103.Gundi M, Subramanyam MA. Menstrual health communication among Indian adolescents: a mixed-methods study. PLoS ONE. 2019;14(10):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hennegan J, Dolan C, Steinfield L, Montgomery P. A qualitative understanding of the effects of reusable sanitary pads and puberty education: implications for future research and practice. Reprod Health. 2017;14(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hennegan J, Dolan C, Wu M, Scott L, Montgomery P. Measuring the prevalence and impact of poor menstrual hygiene management: A quantitative survey of schoolgirls in rural Uganda. BMJ Open 2016;6(12). [DOI] [PMC free article] [PubMed]
- 106.Mishra SK, Dasgupta D, Ray S. A study on the relationship of Sociocultural characteristics, menstrual hygiene practices and gynaecological problems among adolescent girls in Eastern India. Int J Adolesc Med Health. 2016;29(5). [DOI] [PubMed]
- 107.Malhotra A, Coli S, Coates S, Mosquera-Vasquez M. Factors associated with knowledge, attitudes, and hygiene practices during menstruation among adolescent girls in Uttar Pradesh. Waterlines. 2016;35(3):277–305. [Google Scholar]
- 108.Anand E, Singh J, Unisa S. Menstrual hygiene practices and its association with reproductive tract infections and abnormal vaginal discharge among women in India. Sex Reprod Healthc. 2015;6(4):249–54. [DOI] [PubMed] [Google Scholar]
- 109.Ranabhat C, Kim C-B, Choi EH, Aryal A, Park MB, Doh YA. Chhaupadi culture and reproductive health of women in Nepal. Asia-Pacific J Public Heal. 2015;27(7):785–95. [DOI] [PubMed] [Google Scholar]
- 110.Das P, Baker KK, Dutta A, Swain T, Sahoo S, Das BS, et al. Menstrual hygiene practices, WASH access and the risk of urogenital infection in women from odisha, India. PLoS ONE. 2015;10(6):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Muralidharan A. Constrained choices?? Menstrual health and hygiene needs among adolescents in Mumbai slums. Indian J Gend Stud. 2019;26(1–2):12–39. [Google Scholar]
- 112.Torondel B, Sinha S, Mohanty JR, Swain T, Sahoo P, Panda B, et al. Association between unhygienic menstrual management practices and prevalence. BMC Infect Dis. 2018;18(1):473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lahme AM, Stern R, Cooper D. Factors impacting on menstrual hygiene and their implications for health promotion. Glob Health Promot. 2018;25(1):54–62. [DOI] [PubMed] [Google Scholar]
- 114.Amatya P, Ghimire S, Callahan KE, Baral BK, Poudel KC. Practice and lived experience of menstrual exiles (Chhaupadi) among adolescent girls in far-western Nepal. PLoS ONE. 2018;13(12):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.van Leeuwen C, Torondel B. Exploring menstrual practices and potential acceptability of reusable menstrual underwear among a middle Eastern population living in a refugee setting. Int J Womens Health. 2018;10:349–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Girod C, Ellis A, Andes KL, Freeman MC, Caruso BA. Physical, social, and political inequities constraining girls’ menstrual management at schools in informal settlements of nairobi, Kenya. J Urban Heal. 2017;94(6):835–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mathiyalagen P, Peramasamy B, Vasudevan K, Basu M, Cherian J, Sundar B. A descriptive cross-sectional study on menstrual hygiene and perceived reproductive morbidity among adolescent girls in a union territory, India. J Fam Med Prim Care. 2017;6(2):360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Schmitt ML, Clatworthy D, Ratnayake R, Klaesener-Metzner N, Roesch E, Wheeler E, et al. Understanding the menstrual hygiene management challenges facing displaced girls and women: findings from qualitative assessments in Myanmar and Lebanon. Confl Health. 2017;11(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Parker AH, Smith JA, Verdemato T, Cooke J, Webster J, Carter RC. Menstrual management: a neglected aspect of hygiene interventions. Disaster Prev Manag Int J. 2014;23(4):437–54. [Google Scholar]
- 120.Crichton J, Okal J, Kabiru CW, Zulu EM. Emotional and psychosocial aspects of menstrual poverty in resource-poor settings: a qualitative study of the experiences of adolescent girls in an informal settlement in Nairobi. Health Care Women Int. 2013;34(10):891–916. [DOI] [PubMed] [Google Scholar]
- 121.Yamamoto K, Okazaki A, Sakamoto Y, Funatsu M. The relationship between premenstrual symptoms, menstrual pain, irregular menstrual cycles, and psychosocial stress among Japanese college students. J Physiol Anthropol. 2009;28(3):129–36. [DOI] [PubMed] [Google Scholar]
- 122.Chen HM, Chen CH. Related factors and consequences of menstrual distress in adolescent girls with dysmenorrhea. Kaohsiung J Med Sci. 2005;21(3):121–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Khanna A, Goyal RS, Bhawsar R. Menstrual practices and reproductive problems: a study of adolescent girls in Rajasthan. J Health Manag. 2005;7(1):91–107. [Google Scholar]
- 124.Warner P, Bancroft J. Factors related to Self-reporting of the Pre-menstrual syndrome. Br J Psychiatry. 1990;157(2):249–60. [DOI] [PubMed] [Google Scholar]
- 125.Valls Llobet C. Mujeres invisibles para la medicina. 2021.
- 126.Rodríguez MB. La biomedicalización de Las Vidas de Las mujeres: Una revisión de sus dimensiones desde Las publicaciones En Español. Rev Int Sociol. 2021;79(2):e182–182. [Google Scholar]
- 127.Menéndez EL. Modelo médico hegemónico y Atención primaria. Segundas Jorn Atención Primaria La Salud. 1988;451–64.
- 128.Thomson J, Amery F, Channon M, Puri M. What’s missing in MHM? Moving beyond hygiene in menstrual hygiene management. Sex Reprod Health Matters. 2019;27(1):12–5. [DOI] [PMC free article] [PubMed]
- 129.Sánchez Parga J. El culturalismo: atrofia o Devastación de lo social. Perfiles Latinoam. 2006;13(27):193–225. [Google Scholar]
- 130.Adebisi YA. Decolonizing epidemiological research: a critical perspective. Avicenna J Med. 2023;13(2):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gottlieb A. Menstrual taboos: moving beyond the curse. Palgrave Handb Crit Menstruation Stud. 2020;143–62. [PubMed]
- 132.Medina-Perucha L, Jacques-Aviñó C, Holst AS, Valls-Llobet C, Pinzón-Sanabria D, García-Egea A, et al. Systemic powers, institutionalized thinking and situated knowledge: a qualitative exploration on the meanings of ‘menstruation’ and ‘menstrual health’ in Spain. Sex Roles. 2024;90(3):376–91. [Google Scholar]
- 133.Antonovsky A. Health, stress and coping. San Francisco. 1979.
- 134.Kwak Y, Kim Y, Baek KA. Prevalence of irregular menstruation according to socioeconomic status: a population-based nationwide cross-sectional study. PLoS ONE. 2019;14(3):e0214071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Medina-Perucha L, López-Jiménez T, Pujolar-Díaz G, Martínez-Bueno C, Munrós-Feliu J, Valls-Llobet C et al. Menstrual characteristics and associations with sociodemographic factors and self-rated health in spain: a cross-sectional study. BMC Womens Health. 2024;24(1): 88. [DOI] [PMC free article] [PubMed]
- 136.Nutbeam D, Lloyd JE. Understanding and responding to health literacy as a social determinant of health. Annu Rev Public Heal. 2021;42:159–73. [DOI] [PubMed] [Google Scholar]
- 137.Sommer M. Where the education system and women’s bodies collide: the social and health impact of girls’ experiences of menstruation and schooling in Tanzania. J Adolesc. 2010;33(4):521–9. [DOI] [PubMed] [Google Scholar]
- 138.García-Egea A, López-Jiménez T, Jacques-Aviñó C, Morero Beltrán AM, Pi Sánchez A, Martínez-Bueno C et al. Menstrual experiences and acceptability of a menstrual equity intervention among adolescents in Catalonia (Spain). Gac Sanit. 2024;38. [DOI] [PubMed]
- 139.Erchull MJ. You will find out when the time is right: boys, men, and menstruation. Palgrave Handb Crit Menstruation Stud. 2020;395–407. [PubMed]
- 140.Tzenios N. The determinants of access to healthcare: a review of individual, structural, and systemic factors. J Humanit Appl Sci Res. 2019;2(1):1–14. [Google Scholar]
- 141.Martínez A, Smith K, Llop-Gironés A, Vergara Duarte M, Benach J. La mercantilización de La sanidad: El Caso de Catalunya. Cuad Relac Laborales. 2016;34(2):335–55. [Google Scholar]
- 142.Manuel JI. Racial/Ethnic and gender disparities in health care use and access. Health Serv Res. 2018;53(3):1407–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yearby R. Racial disparities in health status and access to healthcare: the continuation of inequality in the united States due to structural racism. Am J Econ Sociol. 2018;77(3–4):1113–52. [Google Scholar]
- 144.Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, et al. The social and psychological impact of endometriosis on women’s lives: a critical narrative review. Hum Reprod Update. 2013;19(6):625–39. [DOI] [PubMed] [Google Scholar]
- 145.Young K, Fisher J, Kirkman M. Do mad people get Endo or does Endo make you mad? Clinicians’ discursive constructions of medicine and women with Endometriosis. Fem Psychol. 2019;29(3):337–56. [Google Scholar]
- 146.Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21(6):762–78. [DOI] [PubMed] [Google Scholar]
- 147.Modzelewski S, Oracz A, Żukow X, Iłendo K, Śledzikowka Z, Waszkiewicz N. Premenstrual syndrome: new insights into etiology and review of treatment methods. Front Psychiatry. 2024;15:1363875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Requadt E, Nahlik AJ, Jacobsen A, Ross WT. Patient experiences of endometriosis diagnosis: a mixed methods approach. BJOG Int J Obstet Gynaecol. 2024;131(7):941–51. [DOI] [PubMed] [Google Scholar]
- 149.Kemigisha E, Rai M, Mlahagwa W, Nyakato VN, Ivanova O. A qualitative study exploring menstruation experiences and practices among adolescent girls living in the Nakivale refugee settlement, Uganda. Int J Environ Res Public Health. 2020;17(18):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Haneman VJ, Menstrual, Capitalism. Period poverty, and the role of the B corporation. Columbia J Gend Law. 2021;41(1):133–45. [Google Scholar]
- 151.Babbar K, Martin J, Ruiz J, Ahmad Parray A, Sommer M. Menstrual health is a public health and human rights issue. Lancet Public Heal. 2022;7:e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Alhelou N, Kavattur PS, Rountree L, Winkler IT. We like things tangible:’ A critical analysis of menstrual hygiene and health policy-making in india, kenya, Senegal and the united States. Glob Public Health. 2022;17(11):2690–703. [DOI] [PubMed] [Google Scholar]
- 153.Guilló-Arakistain M. Challenging menstrual normativity: nonessentialist body politics and feminist epistemologies of health. Palgrave Handb Crit Menstruation Stud. 2020;869–83. [PubMed]
- 154.Wood JM. (In)Visible bleeding: the menstrual concealment imperative. Palgrave Handb Crit Menstruation Stud. 2020;319–36. [PubMed]
- 155.Campbell* C, Cornish F, Mclean C. Social capital, participation and the perpetuation of health inequalities: Obstacles to African-Caribbean participation in partnerships to improve mental health. Ethn Health. 2004;9(4):305–27. [DOI] [PubMed]
- 156.Quijano A. Colonialidad Del poder, Eurocentrismo y América Latina. In: Lander E, editor. comp. L colonialidad Del saber: Eurocentrismo y ciencias sociales. P latinoamericanas, editor. CLACSO;; 2000. p. 246.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.