Abstract
Background
Maternal healthcare (MHC) in Cameroon reflects the persistent challenges in Sub-Saharan Africa, where high maternal mortality continues despite improved service utilization, stressing inequitable effective coverage (EC). This study applied EC cascade analysis—including service contact, continuity, and input-adjusted coverage—to quantify geographic and socioeconomic disparities, informing equity-focused strategies to dismantle structural barriers in the MHC continuum.
Methods
We combined population and health facility data (2018 Cameroon Demographic and Health Survey and 2015 Emergency Obstetric and Neonatal Care Assessment) to estimate the input-adjusted coverage of antenatal care (ANC) and intra-and postpartum care (IPC). Inequalities were assessed using absolute and relative measures.
Results
The MHC cascade showed significant falls in input-adjusted coverage. For ANC, 86.3% service contact eroded to 25.3% continuity and 14.4% input-adjusted coverage. For IPC, the service continuum dropped from 51.4 to 31.4% input-adjusted coverage, revealing steeper losses compared to ANC (20.0% vs. 10.9%). When accounting for service readiness, relative inequalities intensified (e.g., the wealth-based RII for ANC increased by 122%), while absolute gaps narrowed (SII declined by 25%), indicating a greater loss of coverage among socioeconomically privileged groups (IPC input-adjusted coverage dropped by 20.9% for the highest quintile vs. 11.1% for the lowest quintile). At the same time, marginalized populations experienced compounded exclusion—facing severely limited access to care and substandard service quality at available facilities—highlighting the critical need to improve both access and quality.
Conclusion
Cameroon’s MHC disparities stem from systemic resource and quality gaps. Integrating absolute and relative inequality metrics into policy frameworks can dismantle structural biases, aligning interventions with continuum-of-care strategies to prevent avoidable mortality.
Keywords: Inequality, Service readiness, Input-adjusted coverage, Maternal healthcare, Continuum of care, Effective coverage cascade
Background
Sub-Saharan Africa (SSA) bears a disproportionately high burden of global maternal mortality, accounting for nearly 70% of maternal deaths worldwide in 2020 [1]. This situation reflects broader health inequalities across and within countries, including persistent geographic disparities in service access, with rural areas experiencing significantly lower healthcare coverage compared to urban areas [1–6]. Furthermore, unfavourable socioeconomic conditions persist in shaping care utilization, creating significant obstacles for SSA countries in reaching the Sustainable Development Goal (SDG) 3.1 [7–9], which aims to reduce the global maternal mortality ratio (MMR) to less than 70 per 100,000 live births by 2030. Preventable causes— Obstetric hemorrhage, hypertensive disorders in pregnancy, non-obstetric complications, and pregnancy-related infections—dominate maternal deaths in SSA, underscoring the critical need for quality care [1, 10].
Cameroon serves as a poignant example of the SSA countries ongoing challenges. While incremental progress has been made in maternal healthcare (MHC) coverage, the MMR remains alarmingly high at 406 deaths per 100,000 live births [11]. In response, the Cameroon Health Sector Strategy (HSS) 2020–2030 identifies refocused antenatal care (ANC) and skilled attendance at birth as the main pillars for reducing maternal mortality [12]. However, its reliance on service contact metrics (e.g., achieving 95% skilled birth attendance by 2030) overlooks explicit equity and quality benchmarks.
The WHO Guidelines on MHC highlight the critical role of skilled personnel in ensuring continuity of care through timely, evidence-based interventions across the antenatal, intrapartum, and postpartum periods—essential for reducing maternal mortality [13–15]. However, Cameroon’s fragmented healthcare system faces challenges in operationalizing this continuum, as inequitable distribution of skilled providers, unlicensed private facilities, and variable care quality compound missed opportunities to prevent maternal deaths [12, 16–21]. Effective coverage (EC) metrics, integrating service contact with quality adjustments, offer a powerful framework for measuring and addressing these systemic weaknesses [22–25].
Traditional coverage indicators overlook the dimension of care quality, potentially resulting in an inflated perception of healthcare coverage progress. EC cascades track attrition from service contact to health outcomes, with each stage of the cascade capturing distinct dimension of care quality [26]. Applying the EC cascade framework to assess inequalities in MHC enables a systematic examination of how geographic disparities and socioeconomic barriers affect access to appropriate care, and provides actionable insights for targeting interventions and advancing equitable health outcomes [27].
This study aimed to assess the capacity of the Cameroon health system to provide equitable, quality services across the MHC continuum. Specifically, the analysis involved constructing an EC cascade using available data, with estimates for service contact, continuity of service, and input-adjusted coverage. It further evaluated geographic and socioeconomic disparities across cascade stages, employing both absolute and relative inequality metrics.
Methods
EC cascade framework
The EC cascade framework is a model used to evaluate how populations access healthcare services at different level. This includes service utilization (access/contact), system inputs (e.g., staffing, equipment, and infrastructure), quality of care (services delivered in line with evidence-based standards) and health outcome. The primary objective is to assess EC, defined as the proportion of a population in need of a service that experiences a positive health outcome as a result of receiving it [23].
To address the diverse methods used for estimating EC metrics, the WHO/UNICEF Effective Coverage Think Tank introduced a seven-step cascade, derived from Amouzou et al. [22], to establish a consensus on defining and measuring EC for maternal, newborn, child, and adolescent health and nutrition [23]. The proposed coverage cascade include population in need, service contact coverage (proportion of the population in need who came into contact with qualified staff at a facility), input-adjusted coverage (proportion of the population who came into contact with qualified staff at a facility that was ready), intervention coverage (proportion of the population who received healthcare from qualified staff at a facility that was ready), quality-adjusted coverage (proportion of the population who received healthcare according to quality-of-care standards from qualified staff at a facility that was ready), user adherence-adjusted coverage (proportion of the population who received healthcare according to quality-of-care standards and that adhered to provider instructions), and outcome-adjusted coverage (proportion of the population in need who received healthcare according to quality-of-care standards, adhered to provider instructions, and had the expected health outcome) [22, 23, 27].
In this study, the cascade framework, as developed by Amouzou et al. [22] and Marsh et al. [23], was adapted to incorporate the service continuum stage that follows service contact, with the objective of assessing the completion of MHC across all phases of pregnancy—a critical factor in improving women’s health outcomes and preventing maternal mortality [17, 28, 29]. Service continuum coverage of MHC was defined as the proportion of the women who came into contact with qualified staff in a timely and continuous manner at a facility that was ready. The fourth and final stage of our adapted cascade framework (Fig. 1) was input-adjusted coverage across the MHC continuum, which accounted for service readiness—defined as a health facility’s capacity to deliver specific, effective services.
Fig. 1.
EC cascade for MHC service continuum (adapted from Amouzou et al. [22] and Marsh et al. [23])
Data sources
The 2018 Cameroon Demographic and Health Survey (CDHS) and the 2015 Cameroon Emergency Obstetric and Neonatal Care Assessment (EONCA) were identified as two nationally representative and reliable data sources for constructing the EC cascade for MHC in Cameroon. The CDHS and EONCA provide information on the utilization of MHC services by the population and the availability and quality of these services in health facilities, respectively.
The EONCA data collection was undertaken between 7 and 27 December 2015, and its reference period covered the three months preceding the data collection [30]. The CDHS-2018 data collection was conducted from 16 June 2018 to 19 January 2019, with the reference period for MHC information being the five years preceding the data collection [11]. The sample of the two surveys was designed to yield representative results for the country as a whole, for urban and rural areas separately, and for the 12 study regions, which include the country’s 10 administrative regions and its two capital cities, Yaoundé and Douala.
The main objective of the CDHS, conducted under the auspices of The Demographic and Health Surveys (DHS) Program, was to provide estimates of basic demographic and health indicators, including ANC, delivery care and postnatal care.
The EONCA was a retrospective, cross-sectional survey. Its sample included all public and private hospital-level facilities, as well as 30% of public and private lower-level health facilities (health centers). The selection was based on a master list compiled during the 2011 census by the Ministry of Public Health, updated in 2015 for the survey. All sampled facilities provided both ANC and delivery services, in line with Cameroon’s national reproductive health policies, which mandate the integration of ANC into delivery services at every level of the health system. The primary objective was to assess facilities’ capacity to deliver emergency obstetric and newborn care. Additionally, it evaluated essential maternal health services including ANC, family planning, and postpartum care, focusing on structural characteristics (equipment, infrastructure, drugs, human resources, and guideline compliance) [30].
Data linkage strategy and input-adjusted coverage estimation
We employed an ecological approach to integrate population-level data with facility-level data [24]. The health facilities were stratified into 48 strata according to the following criteria: facility type (hospital or health center), managing authority (public or private) and region of location (12 regions). Facility data was regrouped into domains of MHC items. The selection of input-adjusted coverage items was guided by data availability in the EONCA and aligned with key WHO guidelines, including standards for maternal/newborn care quality, task-shifting recommendations, and priority medicines for women/children [31–34]. Items were considered as binary variables (available = 1 or not available = 0). The scores for facility readiness to deliver appropriate ANC and intra- and postpartum care (IPC) were calculated by assigning equal weight to items within each domain and giving equal importance to each domain. The scores were then linked to indicators of utilization of ANC and IPC services (based on population-level data) in each stratum to generate population-level estimates of the input-adjusted coverage index (IAC). Input-adjusted coverage for each group of women was estimated as the mean of the IAC of women in that group. CDHS sampling weights were considered in all estimations to account for complex sampling design of DHS.
The estimations of service contact coverage indicators for ANC and IPC care were conducted separately. For each woman who received care of service s (ANC or IPC) in a health facility of type i, managed by authority j, located in region k, the IAC was calculated using the following formula [35]:
 |
1 |
 and
and  represent, the scores assessing facility readiness to provide appropriate ANC or IPC, and the indicator of the service continuum, respectively.
represent, the scores assessing facility readiness to provide appropriate ANC or IPC, and the indicator of the service continuum, respectively.
Considering all women with a live birth in the last five years (population in need, P), we calculated two distinct binary indicators for ANC and two for IPC using CDHS data. For ANC, we estimated: (A1) service contact—the proportion of women who, during their last pregnancy, had at least one ANC visit from a skilled health personnel in a health facility; and (A2) service continuum—the proportion of women who had at least four ANC visits from a skilled provider in a health facility and received at least seven essential ANC services: weight measurement, height measurement, blood pressure measurement, urine and blood sample collection, intermittent preventive treatment for malaria, and iron supplementation.
For IPC, we estimated: (B1) service contact—the proportion of women assisted at delivery by a skilled attendant in a health facility; and (B2) service continuum—the proportion of those who were both assisted at delivery by a skilled attendant in a health facility and received a postpartum visit within 48 h of delivery.
Finally, we applied formula (1) to continuum indicators (A2) and (B2) to generate input-adjusted coverage estimates (A3) for ANC and (B3) for IPC, respectively. To quantify uncertainty around these estimates, we computed confidence intervals using the delta method, based on the variance formula for the product of independent variables [36, 37]. Contact and readiness data were treated as independent, given that they were drawn from distinct sampling frames.
The evaluation of facility readiness was performed using EONCA data. For women who attended a facility of type i, managed by authority j, located in region k, the score assessing the facility’s readiness to provide them with appropriate care was calculated using the following formula:
 |
2 |
 is the number of facilities of type i, managed by authority j, located in region k, and
is the number of facilities of type i, managed by authority j, located in region k, and  is the score assessing the availability of MHC service items, which was calculated through the following formula:
is the score assessing the availability of MHC service items, which was calculated through the following formula:
 |
3 |
 represents the number of domains (for service s) and
represents the number of domains (for service s) and  is the mean of the binary variable indicating the availability of items related to each domain, as illustrated in Tables 1 and 2.
is the mean of the binary variable indicating the availability of items related to each domain, as illustrated in Tables 1 and 2.
Table 1.
Domains and items used to estimate scores for facility readiness to provide appropriate ANC
| Domain | Item | Item assessment metthod |
|---|---|---|
| Screening and Diagnostics (ANC service) | Blood pressure monitoring, Blood tests, Urine tests, Ultrasound (provision of service) | Interview with the head of the ANC unit |
| Preventive Interventions (ANC service) | Tetanus toxoid, Iron-folic acid, Intermittent preventive treatment for malaria, Insecticide-Treated Nets, Antiretroviral drugs (provision of service) | Interview with the head of the ANC unit |
| Education and Counseling (ANC service) | Nutrition, Danger signs, Birth preparedness, Postpartum family planning (provision of service) | Interview with the head of the ANC unit |
| Psychosocial Support (ANC service) | Mental health screening (provision of service) | Interview with the head of the ANC unit |
| Diagnostic equipment | At least one unit each of the following : Scales, thermometer, Stethoscope, Blood pressure monitor, Ultrasound scanner | Interview with the head of the ANC unit and observational verification |
| Infrastructure | Electricity, Water, Communication equipment (internet, phone or shortwave radio) | Interview with the head of the ANC unit and observational verification |
| Room | At least one room for antenatal consultation | Interview with the head of the ANC unit |
| Medical supplies and equipment | At least one unit each of the following: bed for antenatal unit, Sterilizer | Interview with the head of the ANC unit and observational verification |
| Essential medicines and commodities | Gentallin/gentamycin/penicillin, Metronidazole, Amoxicillin, Corticosteroid, Magnesium sulfate, Quinine salts, Artemisinin-based combination therapies. (Availability) | Interview with the head of the ANC unit and observational verification |
| Staff |
Primary Healthcare Provider (at least one unit of any of the following: General Practitioner, Midwife, Nurse, or Caregiver), Diagnostic or Laboratory Professional (at least one unit of any of the following: Biologist, Laboratory Technician, Laboratory Engineer) |
Interview with the head of the ANC unit |
| Refocused antenatal consultation | Adherence to guidelines for personalizing care and reducing unnecessary interventions | Interview with the head of the ANC unit and record review |
Table 2.
Domains and items used to estimate scores for facility readiness to provide appropriate IPC
| Domain | Item | Item assessment method |
|---|---|---|
| Obstetrical unit | Provision of obstetrical care services available 7 days a week | Interview with the head of the labor and delivery unit |
| Postnatal unit | Provision of postnatal care services available 7 days a week | Interview with the head of the maternity unit |
| Family planning | Provision of postpartum family planning services | Interview with the head of the labor and delivery unit |
| Anaesthesia services | Administartion of anesthesia | Interview with the head of the labor and delivery unit |
| Diagnostic equipment | At least one unit each of the following: Thermometer, Stethoscope, Blood pressure monitor, Ultrasound scanner | Interview with the head of the labor and delivery unit and observational verification |
| Infrastructure | Permanent source of : Electricity, Water, Communication equipment (internet, phone or shortwave radio) | Interview with the head of the labor and delivery unit and observational verification |
| Room | Labor, Delivery, Delivery suite, Operating room, Laboratory (capable of performing essential diagnostic tests) | Interview with the head of the labor and delivery unit and observational verification |
| Medical supplies and equipment | At least one unit each of the following: bed in the obstetric unit, sterilizer, delivery boxe, Caesarean section boxe | Interview with the head of the labor and delivery unit and observational verification |
| Essential medicines and commodities | Gentallin/gentamycin/penicillin, Metronidazole, Amoxicillin, Magnesium sulfate/diazepam, Synthocinone/oxytocin, Misoprostol, Ergometrine, Quinine salts, artemisinin-based combination therapies, Antiretroviral drugs. (Availability) | Interview with the head of the labor and delivery unit and observational verification |
| Staff |
Primary Healthcare Provider (at least one unit of any of the following: General Practitioner, Midwife, Nurse, or Caregiver), Specialized Medical Professional (at least one unit of any of the following: Obstetrician, Gynecologist, or Surgeon), Diagnostic or Laboratory Professional (at least one unit of any of the following: Biologist, Laboratory Technician, Laboratory Engineer) |
Interview with the head of the labor and delivery unit |
| Emergency obstetric care signals | Parenteral antibiotics, Uterotonics, Parenteral anticonvulsants, Manual removal of the placenta, Assisted vaginal delivery, Caesarean section, Blood transfusion (service provision) | Interview with the head of the labor and delivery unit |
| Active management of the third stage of labor | Adherence to guidelines for Administration of Oxytocin, Umbilical Cord Traction, Uterine Massage, Examination of the Placenta, Prophylactic Uterotonics, and active Observation Monitoring | Interview with the head of the labor and delivery unit and record review |
Inequality analysis
The magnitude of geographic (region and area of residence—capital cities, other urban, and rural) and socioeconomic (level of education and wealth quintile) inequalities was measured using indicators that take into account the estimates of intermediate subgroups between the most and least advantaged categories. For the non-ordered subgroup dimensions (region and area of residence), absolute inequality was measured using the weighted Mean Difference from the overall Mean (MDMw), while relative inequality was measured via the weighted Index of Disparity (IDISw). Taking into account the weight  of each subgroup, the coverage
of each subgroup, the coverage  for each subgroup, the number n of subgroups and the overall mean µ, MDMw and IDISw were calculated as follows:
for each subgroup, the number n of subgroups and the overall mean µ, MDMw and IDISw were calculated as follows:
 |
4 |
 |
5 |
MDMw and IDISw have positive magnitudes, with 0 indicating no inequality and higher values indicating higher levels of inequality [38].
Regarding the ordered subgroup dimensions (level of education and wealth quintile), absolute inequality was measured using the Slope Index of Inequality (SII), while relative inequality was evaluated with the Relative Index of Inequality (RII). SII was ranged from − 1 to 1. When there is no inequality, the SII is equal to 0. Higher SII absolute values reflect greater inequality levels, with positive values indicating a concentration of the indicator among advantaged subgroups and negative values suggesting a concentration among disadvantaged subgroups. In contrast, the RII only takes positive values. An RII value of 1 signifies no inequality, and the degree of inequality increases as the RII diverges further from 1. Values greater than 1 indicate a concentration of the indicator among advantaged subgroups, while values below 1 represent a concentration among disadvantaged subgroups [38].
The relative rates of change in absolute inequality (RCA) and relative inequality (RCR) were calculated to assess changes in the magnitude of inequality across successive stages of the EC cascade.
Results
Characteristics of the study population and health facilities
Table 3 summarizes residential and socioeconomic characteristics of the study population. This study included 6,446 women aged 15–49 years who had at least one live birth in the last five years, with an average age of 28.2 years. The majority of women (53%) resided in rural areas, while 14% lived in capital cities (Yaoundé or Douala), and 33% were located in other urban areas. Approximately two out of five women (41%) had reached secondary education, nearly one-third (31%) had attained primary education, 6% had acquired higher education and about one-fifth (22%) had no formal education. Of these women, 16% belonged to the highest wealth quintile, 17% to the lowest, 20% to the fourth quintile, 23% to the second, and 24% to the middle quintile.
Table 3.
Study population characteristics
| Characteristic | Number | % | |
|---|---|---|---|
| Area of residence | Capital cities | 936 | 14.5 |
| Other urban | 2,103 | 32.6 | |
| Rural | 3,407 | 52.9 | |
| Education | No education | 1,414 | 21.9 |
| Primary | 2,019 | 31.3 | |
| Secondary | 2,642 | 41.0 | |
| Higher | 371 | 5.8 | |
| Wealth Quintile | Lowest | 1,088 | 16.9 |
| Second | 1,466 | 22.7 | |
| Middle | 1,542 | 23.9 | |
| Fourth | 1,306 | 20.3 | |
| Highest | 1,044 | 16.2 | |
| Average age (years) | 6,446 | 28.2 | |
Table 4 shows the characteristics of the 1,636 facilities analyzed. All health facilities included in the study provide both ANC and delivery services. Among them, 266 (16%) were hospitals, 1,370 (84%) were health centers, 1,023 (62%) were public, and 613 (38%) were private. Their distribution among regions varies from 4 to 13%.
Table 4.
Facility characteristics
| Characteristic | Number | % | |
|---|---|---|---|
| Cameroon | 1,636 | 100 | |
| Region | Adamawa | 72 | 4.4 |
| Centre | 200 | 12.2 | |
| Douala | 220 | 13.4 | |
| East | 86 | 5.3 | |
| Far‒North | 143 | 8.7 | |
| Littoral | 97 | 5.9 | |
| North | 107 | 6.5 | |
| North‒West | 132 | 8.1 | |
| West | 193 | 11.8 | |
| South | 78 | 4.8 | |
| South‒West | 128 | 7.8 | |
| Yaoundé | 180 | 11.0 | |
| Type | Hospital | 266 | 16.3 |
| Health center | 1,370 | 83.7 | |
| Managing authority | Public | 1,023 | 62.5 |
| Private | 613 | 37.5 | |
EC cascade for MHC continuum
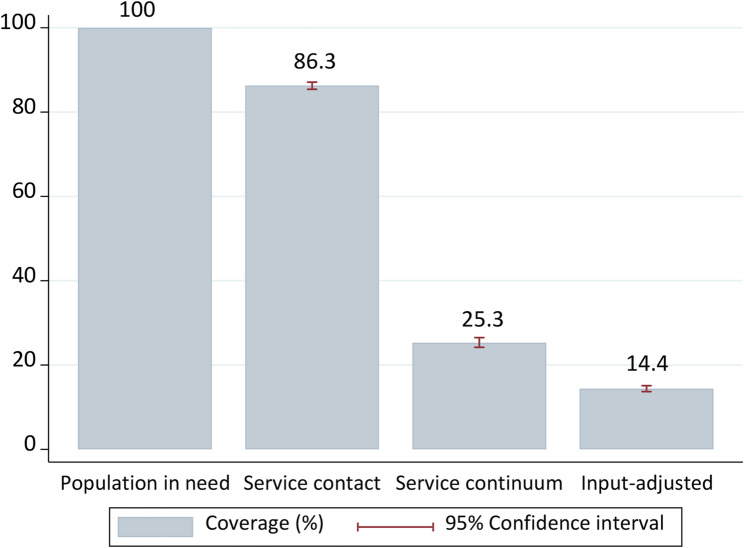
Overall, service contact coverage for ANC was 86.3% (95% CI: 85.4–87.1), indicating that 13.7% of pregnant women lacked initial engagement with the health system. ANC service continuum coverage—measuring access to complete ANC with adequate care content—was markedly lower at 25.3% (95% CI: 24.2–26.5), reflecting a 61.0% loss of opportunity between initial contact and continuity. Input-adjusted coverage, which accounts for facility readiness, dropped further to 14.4% (95% CI: 13.7–15.1), leaving 10.9% of women who accessed continuous ANC unable to receive appropriate care due to facility limitations (Fig. 2).
Fig. 2.
EC cascade for the ANC continuum
For IPC, service contact coverage stood at 68.5% (95% CI: 67.3–69.6), falling 31.5% behind ANC. Service continuum coverage for IPC reached 51.4% (95% CI: 50.2–52.6), but input-adjusted IPC coverage declined to 31.4% (95% CI: 30.6–32.3), representing a 20.0% loss of opportunity for appropriate care—nearly double the attrition observed for ANC (10.9%) (Fig. 3).
Fig. 3.
EC cascade for the IPC continuum
Inequalities in MHC coverage
Service contact coverage
Substantial disparities in ANC and IPC service contact coverage were observed across geographic dimensions (IDISw range: 0.9–8.9) (Tables 5 and 6). For ANC, regional coverage ranged from 70.0% (95% CI: 64.7–75.0) in Adamawa to near-universal levels (99.1%; 95% CI: 95.0–100.0) in the South-West, while IPC coverage varied from 36.9% (Far-North; 95% CI: 34.2–39.7) to 97.6% (South-West; 95% CI: 95.8–99.3). Residence-based inequities were pronounced for ANC (IDISw = 3.1) and even more so for IPC (IDISw = 8.9), with rural areas lagging significantly: ANC coverage in rural areas (78.0%; 95% CI: 76.9–79.7) was 19% points lower than in capital cities (97.3%; 95% CI: 96.0–97.9), while IPC coverage in rural areas (50.2%; 95% CI: 48.5–51.9) was almost half that of capital cities (93.1%; 95% CI: 91.6–94.5).
Table 5.
Inequalities in service contact, service continuum and input-adjusted coverage for ANC
| Service contact (%) | 95%CI | Service continuum (%) | 95%CI | Input-Adjusted (%) | 95%CI | ||
|---|---|---|---|---|---|---|---|
| Cameroon | 86.3 | (85.4-87.1) | 25.3 | (24.2-26.5) | 14.4 | (13.7-15.1) | |
| Region | Adamawa | 70.0 | (64.7-75.0) | 20.7 | (15.6-26.7) | 8.0 | (5.6-10.36) |
| Centre | 88.2 | (85.7-90.4) | 27.5 | (24.2-31.0) | 14.3 | (12.4-16.2) | |
| Douala | 97.6 | (96.1-98.7) | 39.8 | (35.9-43.8) | 31.5 | (28.3-34.7) | |
| East | 82.0 | (78.6-85.1) | 28.3 | (24.3-32.6) | 13.9 | (11.5-16.4) | |
| Far‒North | 77.2 | (74.7-79.5) | 15.2 | (12.9-17.7) | 5.7 | (4.8 - 6.6) | |
| Littoral | 95.0 | (91.0-97.6) | 29.9 | (23.5-37.1) | 19.9 | (15.6-24.1) | |
| North | 70.6 | (67.6-73.5) | 6.3 | (4.6 - 8.3) | 2.3 | (1.7 - 3.0) | |
| North‒West | 98.5 | (96.8-99.5) | 19.0 | (15.2-23.2) | 12.3 | (9.7 −14.9) | |
| West | 98.3 | (97.0-99.1) | 26.6 | (23.4-29.9) | 17.0 | (14.8-19.2) | |
| South | 93.8 | (88.8-97.0) | 35.6 | (27.9-43.8) | 16.1 | (13.1-19.0) | |
| South‒West | 99.1 | (95.0 −100) | 17.8 | (11.0-26.3) | 15.0 | (9.0 −20.9) | |
| Yaoundé | 96.5 | (94.8-97.8) | 45.6 | (41.6-49.7) | 32.9 | (29.8-35.9) | |
| MDMw|RCA | 0.8|NA | 0.7|−12.5 | 0.5|−28.6 | ||||
| IDISw |RCR | 0.9|NA | 2.9|222.2 | 3.5|20.7 | ||||
| Area of residence | Capital cities | 97.3 | (96.0-97.9) | 42.7 | (39.8-45.5) | 32.2 | (30.0-34.4) |
| Other urban | 93.0 | (91.8-94.1) | 26.4 | (24.4-28.5) | 15.5 | (14.2-16.7) | |
| Rural | 78.0 | (76.9-79.7) | 16.9 | (15.5-18.3) | 7.6 | (6.9 - 8.3) | |
| MDMw|RCA | 2.7|NA | 2.4|−11.1 | 2.2|−8.3 | ||||
| IDISw |RCR | 3.1|NA | 9.7|212.9 | 15.1|55.7 | ||||
| Level of education | No education | 66.6 | (64.3-68.8) | 11.7 | (9.9 −13.7) | 4.1 | (3.4 - 4.8) |
| Primary | 87.9 | (86.4-89.3) | 20.6 | (18.7-22.6) | 11.4 | (10.2-12.5) | |
| Secondary | 96.3 | (95.5-97.0) | 32.1 | (30.3-34.0) | 20.9 | (19.7-22.2) | |
| Higher | 99.3 | (97.9-99.8) | 45.3 | (40.3-50.4) | 33.1 | (29.4-36.9) | |
| SII|RCA | 0.5|NA | 0.5|0.0 | 0.4|−20.0 | ||||
| RII|RCR | 1.9|NA | 5.7|200.0 | 12.1|112.3 | ||||
| Wealth quintile | Lowest | 66.7 | (64.2-69.2) | 8.3 | (6.6 −10.3) | 2.7 | (2.1 - 3.4) |
| Second | 82.4 | (80.3-84.3) | 17.4 | (15.3-19.7) | 7.7 | (6.7 - 8.7) | |
| Middle | 89.1 | (87.3-90.7) | 21.0 | (18.7-23.3) | 11.5 | (10.1-12.8) | |
| Fourth | 96.6 | (95.5-97.5) | 34.5 | (31.9-37.2) | 23.3 | (21.5-25.2) | |
| Highest | 98.3 | (97.4-99.0) | 41.8 | (38.9-44.7) | 30.2 | (28.0-32.4) | |
| SII|RCA | 0.4|NA | 0.4|0.0 | 0.3|−25.0 | ||||
| RII|RCR | 1.7|NA | 6.3|270.6 | 14.0|122.2 | ||||
NA Not applicable
Table 6.
Inequalities in service contact, service continuum and input-adjusted coverage for IPC
| Service contact (%) | 95%CI | Service continuum (%) | 95%CI | Input-Adjusted (%) | 95%CI | ||
|---|---|---|---|---|---|---|---|
| Cameroon | 68.5 | (67.3-69.6) | 51.4 | (50.2-52.6) | 31.4 | (19.6-26.4) | |
| Region | Adamawa | 52.5 | (46.9-58.1) | 44.1 | (38.5-49.7) | 23.0 | (19.6-26.4) |
| Centre | 74.1 | (70.9-77.2) | 51.4 | (47.8-55.0) | 28.1 | (25.9-30.2) | |
| Douala | 94.9 | (92.9-96.5) | 66.3 | (62.5-70.0) | 50.2 | (47.2-53.3) | |
| East | 59.5 | (55.3-63.6) | 37.0 | (33.0-41.1) | 21.0 | (18.3-23.7) | |
| Far‒North | 36.9 | (34.2-39.7) | 31.1 | (28.5-33.8) | 15.2 | (13.8-16.5) | |
| Littoral | 95.5 | (91.6-97.9) | 59.3 | (52.1-66.2) | 40.7 | (36.0-45.4) | |
| North | 39.5 | (36.4-42.7) | 28.2 | (25.3-3.11) | 12.9 | (11.5-14.2) | |
| North‒West | 91.2 | (88.0-93.8) | 76.0 | (71.6-80.1) | 46.9 | (43.8-50.0) | |
| West | 93.8 | (91.9-95.5) | 76.4 | (73.2-79.4) | 48.6 | (46.3-50.8) | |
| South | 84.4 | (77.8-89.6) | 72.5 | (64.9-79.3) | 35.7 | (32.5-38.8) | |
| South‒West | 97.6 | (95.8-99.3) | 84.5 | (76.4-90.7) | 59.8 | (54.4-65.3) | |
| Yaoundé | 91.4 | (89.0-93.5) | 66.6 | (62.9-70.2) | 48.9 | (46.0-51.8) | |
| MDMw|RCA | 1.6|NA | 1.3|−18.8 | 1.1|−19.1 | ||||
| IDISw |RCR | 2.3|NA | 2.6|13.0 | 3.4|32.4 | ||||
| Area of residence | Capital cities | 93.1 | (91.6-94.5) | 66.5 | (63.8-69.0) | 49.6 | (47.5-51.7) |
| Other urban | 83.8 | (82.1-85.4) | 63.9 | (61.8-66.0) | 39.6 | (38.2-41.1) | |
| Rural | 50.2 | (48.5-51.9) | 38.3 | (36.7-40.0) | 20.4 | (19.5-21.4) | |
| MDMw|RCA | 6.1|NA | 4.4|−29.9 | 3.7|−15.9 | ||||
| IDISw |RCR | 8.9|NA | 8.6|−3.4 | 11.8|37.2 | ||||
| Level of education | No education | 30.9 | (28.7-33.1) | 22.7 | (20.7 −24.7) | 10.5 | (9.5 - 11.5) |
| Primary | 69.4 | (67.3-71.4) | 53.0 | (50.8-55.2) | 30.6 | (29.2-32.0) | |
| Secondary | 88.5 | (87.2-89.7) | 65.4 | (63.5-67.2) | 42.3 | (41.0-43.7) | |
| Higher | 98.0 | (96.2-99.1) | 77.6 | (73.2-81.6) | 56.6 | (53.3-59.9) | |
| SII|RCA | 0.8|NA | 0.7|−12.5 | (0.5 - 0.9) | 0.6|−14.3 | |||
| RII|RCR | 5.5|NA | 4.2|−23.6 | (2.1 - 6.3) | 6.5|57.7 | |||
| Wealth quintile | Lowest | 27.9 | (25.6-30.4) | 20.0 | (17.9-22.3) | 8.9 | (7.9 - 9.9) |
| Second | 57.6 | (55.0-60.1) | 44.8 | (42.2-47.4) | 24.1 | (22.6-25.6) | |
| Middle | 75.3 | (73.0-77.6) | 57.2 | (54.5-59.8) | 33.3 | (31.5-35.0) | |
| Fourth | 89.6 | (87.8-91.2) | 63.2 | (60.6-65.8) | 41.3 | (39.5-43.2) | |
| Highest | 95.8 | (94.5-96.8) | 74.8 | (72.3-77.3) | 53.9 | (51.9-55.9) | |
| SII|RCA | 0.8|NA | 0.6|−25.0 | 0.5|−16.7 | ||||
| RII|RCR | 4.7|NA | 3.8|−19.1 | 6.0|57.9 | ||||
NA Not applicable
Coverage was largely determined by socioeconomic gradients (RII range: 1.7–5.5) (Tables 5 and 6). ANC access among women with higher education (99.3%; 95% CI: 97.9–99.8) was nearly 33% points higher than among uneducated women (66.6%; 95% CI: 64.3–68.8), mirroring wealth-based disparities (98.3% in the highest vs. 66.7% in the lowest quintile). IPC coverage showed even starker divides (RII > 4.7): the most educated women and the wealthiest quintile exceeded 95%, compared to approximately 30% among uneducated and poorest groups.
Service continuum vs. Contact coverage
There were gaps between service contact and continuum coverage across all groups, with larger gaps for ANC (Figs. 4, 5, 6 and 7). ANC coverage loss reached 81.3% points in the South-West region (from 99.1 to 17.8%); while it was approximately 50% points in the Yaoundé/Adamawa region. The highest IPC coverage loss was in the Littoral region (36.2% points; from 95.5 to 59.3%), followed by Douala (28.6% points; from 94.9 to 66.3%) (Tables 5 and 6).
Fig. 4.
Geographic inequalities in service contact, service continuum and input-adjusted coverage for ANC, according to region (a) and area of residence (b), with weighted mean difference from the mean (MDMw) and weighted index of disparity (IDISw)
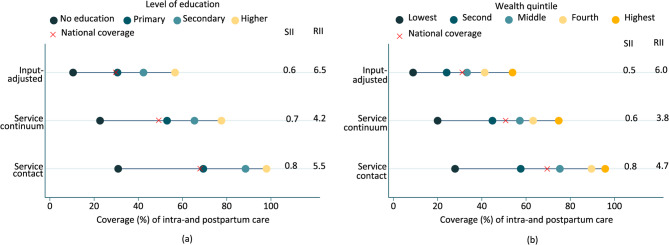
Fig. 5.
Socioeconomic inequalities in service contact, service continuum and input-adjusted coverage for ANC, according to level of education (a) and wealth quintile (b)
Fig. 6.
Geographic inequalities in service contact, service continuum and input-adjusted coverage for intra-and postpartum care, according to region (a) and area of residence (b), with weighted mean difference from the mean (MDMw) and weighted index of disparity (IDISw)
Fig. 7.
Socioeconomic inequalities in service contact, service continuum and input-adjusted coverage for intra-and postpartum care, according to level of education (a) and wealth quintile (b), with slope index of inequality (SII) and relative index of inequality (RII)
Substantial inequalities were observed across the MHC continuum, with geographic (IDISw range: 2.6–9.7) and socioeconomic disparities (RII range: 3.8–6.3) highlighting notable differences in access to care (Tables 5 and 6). ANC disparities intensified significantly (RCR > 200%). Regional disparities were stark, as the Nord region recorded complete ANC continuum coverage for only 6.3% of women (95% CI: 4.6–8.3), seven times lower than in Yaoundé (45.6%; 95% CI: 41.6–49.7). Wealth-driven inequities were pronounced, with ANC coverage among the poorest women (8.3%; 95% CI: 6.6–10.3) lagging fivefold behind their wealthiest counterparts (41.8%; 95% CI: 38.9–44.7). Educational attainment mirrored these patterns, with coverage gaps between women with no formal education and those with higher education aligning closely with wealth- based trends. By residence, rural areas exhibited ANC and IPC coverage that were half those of capital cities.
Input-adjusted coverage
Input-adjusted coverage for both ANC and IPC consistently lagged service continuum metrics across all geographic and socioeconomic groups (Figs. 4, 5, 6 and 7). Relative inequalities surged by > 20% for ANC and > 32% for IPC at the input-adjusted stage, signalling systemic exclusion of northern, rural, less educated, and impoverished women (with IPC coverage < 21%, and extremely low ANC coverage < 10%) (Tables 5 and 6). ANC input-adjusted coverage in northern regions (2.7–5.7%) was at least six times lower than in Yaoundé/Douala (31.5–32.9%), and coverage among the poorest (2.7%; 95% CI: 2.1–3.4) was 11 times lower than among the wealthiest (30.2%; 95% CI: 28.0–32.4). For IPC, input-adjusted coverage in northern regions (12.9–15.2%) was at least three times lower than in the South-West region (59.8%; 95% CI: 54.4–65.3), while coverage in rural areas (20.4%; 95% CI: 19.5–21.4%) was half that of urban centers (39.6–49.6%). Among the poorest and uneducated (8.9–10.5%), IPC coverage was six times lower than among the wealthiest and most educated (53.9–56.6%).
Unlike relative inequalities, absolute inequalities tended to decrease (RCA < 0%), suggesting that input-adjusted losses were more pronounced among advantaged groups (Figs. 4, 5, 6 and 7; Tables 5 and 6). For ANC (wealth-based RCR = 122%; RCA = −25%), coverage declined by 5.6% points in the poorest quintile (from 8.3 to 2.7%) and by 11.6 points in the wealthiest quintile (from 41.8 to 30.2%). Similarly, IPC coverage fell by 11.1 points in the poorest quintile (from 20.0 to 8.9%) versus a 20.9-point decline in the wealthiest (from 74.8 to 53.9%).
Discussion
The steep geographic and socioeconomic disparities observed across Cameroon’s MHC continuum underscore systemic inequities that threaten progress toward reducing maternal mortality. Our analysis reveals a fragmented health system where access to care—and crucially, the likelihood of accessing appropriate care—is heavily stratified by region, residence, education, and wealth. This disproportionately excludes rural, northern —among the country’s poorest—, and socioeconomically marginalized women, mirroring patterns across sub-Saharan Africa where gaps in care quality drive preventable deaths [39–42].
The MHC cascade highlights critical attrition points. While 86.3% of pregnant women initiated ANC, only 25.3% accessed adequate care continuity, and just 14.4% accessed care in facilities with sufficient readiness. For IPC, service contact coverage (68.5%) declined to 51.4% continuity and 31.4% input-adjusted coverage, reflecting a 20.0% loss in care appropriateness—nearly double ANC’s 10.9% loss. This steeper attrition in IPC is alarming, given that 75% of maternal deaths occur during delivery and postpartum [1, 42, 43]. The sharp decline in IPC readiness highlights systemic failures in emergency obstetric infrastructure, especially in rural and northern regions where input-adjusted coverage remains critically low (< 20.4%), exposing more than four in five women to life-threatening complications such as hemorrhage and sepsis.
Geographic disparities were profound. ANC service contact coverage ranged from 70.0% in Adamawa to 99.1% in the South-West, while rural areas lagged 19% points behind urban centers. At the input-adjusted stage, northern regions faced catastrophic gaps: only 2.7–5.7% of women accessed appropriate ANC—six times lower than in Yaoundé/Douala. Similarly, rural IPC input-adjusted coverage was less than half that of capitals (49.6%). These gradients align with evidence linking rural residence to 3–4 times higher maternal mortality risks in sub-Saharan Africa due to shortages of skilled providers and emergency readiness [1, 40, 42, 43].
Socioeconomic status profoundly stratified effective coverage, with disparities intensifying at the input-adjusted stage. The wealthiest quintile exhibited 11-fold higher input-adjusted ANC coverage (30.2% vs. 2.7%) and six-fold higher IPC coverage (53.9% vs. 8.9%) than the poorest. Notably, while absolute inequalities diminished (RCA < 0%), relative inequalities widened markedly (RCR > 20%). This paradox reflects a health system in which both privileged and marginalized groups lose ground to substandard care [44, 45], with privileged populations sustaining greater reductions in coverage of potentially high-quality care - reflecting their unrealized potential due to system-wide readiness gaps [46]. The critically suboptimal input-adjusted coverage (30–57%) among wealthier women despite near-universal service contact (96–99%) demonstrates that quality improvements yield the greatest marginal gains in high-coverage populations. Meanwhile, marginalized groups faced compounded exclusion—marked by severely restricted initial access and the lowest quality of care at the facilities they could reach [47]—underscoring the urgent need to expand both access and quality in tandem.
This study has multiple limitations. The estimation of EC for maternal health services in Cameroon is constrained by scarce, limited facility-level data. While the study utilized nationally representative surveys (CDHS-2018 for population data and EONCA-2015 for facility data), aggregating health facility data at the regional level reduces granularity, potentially masking variations in service availability across individual facilities. Additionally, categorizing facilities broadly as “hospitals” or “health centers” involves averaging across facilities with highly varied capacities. For example, central/referral hospitals in cities typically offer comprehensive obstetric care and handle complex cases, while district hospitals in rural areas may have limited staffing, equipment, or patient volumes. This aggregation may obscure disparities in service quality—particularly for labor and delivery—and could modestly underestimate gaps in care access. To address these limitations, future research should adopt geospatial methods to link facility-level and population-level data, ensuring greater precision [48]. Additionally, using EONCA-2015 alongside CDHS-2018 introduces temporal gaps that may misalign readiness-side and utilization-side trends, potentially impacting the accuracy of assessments [49].
The study infers care quality from structural readiness (e.g., infrastructure, staffing), a common but flawed approach in Low- and Middle-Income Countries (LMICs), as evidence from 4,300 facilities shows no infrastructure threshold reliably predicts care quality [50]. Moreover, DHS prioritize self-reported utilization metrics over clinical process indicators (e.g., uterotonic administration, partograph use), limiting their effectiveness for assessing EC [51], and introducing potential recall bias. These limitations underscore the need to integrate structural metrics with direct observational or clinical process data—aligned with WHO quality standards [32]—by linking population-level surveys with facility data to better approximate EC and reduce reliance on proxies [23].
Conclusion
Cameroon’s MHC disparities reveal systemic failures in equitable resource allocation and care quality. Stark geographic divides exist, with northern regions facing sixfold lower ANC coverage than urban centers, while socioeconomic gradients leave the poorest quintile with sixfold lower IPC access than the wealthiest. Adjusting for service readiness, relative inequalities intensify while absolute inequalities narrow, reflecting greater attrition among privileged groups and persistent extreme deprivation among marginalized populations. To address these challenges, Cameroon should prioritize: (1) enhancing emergency obstetric care infrastructure in rural and underserved areas through strategic investments; (2) standardizing and ensuring the consistent provision of high-quality maternal health services across all tiers of the health system; and (3) expanding financial protection mechanisms to reduce cost-related barriers to accessing care. Integrating absolute and relative inequality metrics into policy frameworks will ensure reforms dismantle structural biases, bridging survival gaps tied to wealth and geography. Aligning these efforts with the full care continuum is critical to curbing preventable deaths and advancing maternal health equity in a region burdened by the world’s highest MMR.
Acknowledgements
We gratefully acknowledge the African Population and Health Research Center (APHRC) for its collaboration through the Countdown 2030 Fellowship Program, which served as the impetus for this study. We also thank the DHS Program and the National Institute of Statistics (Cameroon) for generously providing access to the datasets used in this analysis.
Abbreviations
- 95% CI
95% Confidence interval
- ACT
Artemisinin-based combination therapy
- ANC
Antenatal care
- ARV
Antiretroviral treatment for HIV-infected patients
- CDHS
Cameroon Demographic and Health Survey
- DHS
Demographic and Health Survey
- EC
Effective coverage
- EONCA
Cameroon Emergency Obstetric and Neonatal Care Assessment
- HSS
Health Sector Strategy
- IDISw
Weighted index of disparity
- IPC
Intra-and postpartum care
- LMIC
Low- and Middle-Income Countries
- MDMw
Weighted mean difference from the overall mean
- MHC
Maternal healthcare
- MMR
Maternal mortality ratio
- RII
Relative index of inequality
- RCA
Rate of change in absolute inequality
- RCR
Rate of change in relative inequality
- SDG
Sustainable Development Goal
- SII
Slope index of inequality
- SSA
Sub-Saharan African
- WHO
World Health Organization
Authors’ contributions
MS designed the study, conducted the analysis and drafted the manuscript. AJDB contributed to the conceptualisation of the equalities analysis. ADD, EMS and ABS supervised the work and contributed to the analysis. All authors reviewed and contributed to the manuscript.
Funding
This work was funded by the Countdown to 2030’s BMGF, grant number INV-042414. The study design, data analysis, manuscript drafting, and submission were independent of any funding influence.
Data availability
All data used in this analysis are publicly available upon request from the DHS Program (http://www.dhsprogram.com) and the National Institute of Statistics (https://ins-cameroun.cm/).
Declarations
Ethics approval and consent to participate
Ethical approval was not required for this study because it was based on publicly available data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division., Geneva, World Health Organization; 2023. Available: https://iris.who.int/bitstream/handle/10665/366225/9789240068759-eng.pdf?sequence=1
- 2.Sully EA, Biddlecom A, Darroch JE. Not all inequalities are equal: differences in coverage across the continuum of reproductive health services. BMJ Glob Health. 2019;4(5): e001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanou M, Kishida T, Kamiya Y. The effects of geographical accessibility to health facilities on antenatal care and delivery services utilization in Benin: a cross-sectional study. Reprod Health Déc. 2021;18(1):205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anarwat SG, Salifu M, Akuriba MA. Equity and access to maternal and child health services in Ghana a cross-sectional study. BMC Health Serv Res. 2021;21(1):864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samuel O, Zewotir T, North D. Decomposing the urban–rural inequalities in the utilisation of maternal health care services: evidence from 27 selected countries in sub-Saharan Africa. Reprod Health. 2021;18(1): 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Awoke N, Ababulgu SA, Hanfore LK, Gebeyehu EG, Wake SK. Regional disparities in antenatal care utilization among pregnant women and its determinants in Ethiopia. Front Glob Womens Health 9 Févr. 2024;5:1230975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amwonya D, Kigosa N, Kizza J. Female education and maternal health care utilization: evidence from Uganda. Reprod Health Déc. 2022;19(1):142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ataguba JE, Nwosu CO, Obse AG. Is socioeconomic inequality in antenatal care coverage widening or reducing between- and within-socioeconomic groups? A case of 19 countries in sub-Saharan Africa. SSM. 2023;23:101402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asefa A, Gebremedhin S, Marthias T, Nababan H, Christou A, Semaan A, et al. Wealth-based inequality in the continuum of maternal health service utilisation in 16 sub-Saharan African countries. Int J Equity Health 2 Oct. 2023;22(1):203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Musarandega R, Nyakura M, Machekano R, Pattinson R, Munjanja SP. Causes of maternal mortality in Sub-Saharan africa: A systematic review of studies published from 2015 to 2020. J Glob Health 9 Oct. 2021;11:04048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institut National de la Statistique (INS), and ICF. 2019. Cameroon Demographic and Health Survey 2018. Yaoundé, Cameroon, and Rockville, Maryland, USA: INS and ICF. Available: https://dhsprogram.com/publications/publication-fr360-dhs-final-reports.cfm
- 12.Ministry of Public Health. 2020. Health Sector Strategy 2020–2030. Yaoundé, Cameroon. Available: https://minepat.gov.cm/wp-content/uploads/2022/01/Strategie-Sectorielle-de-la-Sante_Francais.pdf
- 13.De Masi S, Bucagu M, Tunçalp Ö, Peña-Rosas JP, Lawrie T, Oladapo OT, et al. Integrated person-centered health care for all women during pregnancy: implementing World Health Organization recommendations on antenatal care for a positive pregnancy experience. Glob Health Sci Pract. 2017;5(2):197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. WHO recommendations on maternal and newborn care for a positive postnatal experience. Geneva: World Health Organization. 2022. Available: https://iris.who.int/bitstream/handle/10665/352658/9789240045989-eng.pdf?sequence=1 [PubMed]
- 15.World Health Organization. WHO recommendations on maternal health: guidelines approved by the WHO Guidelines Review Committee, second edition. Geneva, World Health Organization. 2025. Available: https://iris.who.int/bitstream/handle/10665/380666/9789240080591-eng.pdf?sequence=1
- 16.Tandi TE, Cho Y, Akam AJC, Afoh CO, Ryu SH, Choi MS, et al. Cameroon public health sector: shortage and inequalities in geographic distribution of health personnel. Int J Equity Health Déc. 2015;14(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384(9940):347–70. [DOI] [PubMed] [Google Scholar]
- 18.Oleribe OE, Momoh J, Uzochukwu BS, Mbofana F, Adebiyi A, Barbera T, et al. Identifying key challenges facing healthcare systems in Africa and potential solutions. IJGM Nov. 2019;12:395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang B, Trawin J, Dzelamunyuy S, Wiens MO, Tagoola A, Businge S, et al. Assessment of facility readiness for pediatric emergency and critical care utilizing a 2-Phase survey conducted in six hospitals in Uganda and cameroon: A quality improvement study. Pediatr Emer Care Févr. 2025;41(2):94–103. [DOI] [PubMed] [Google Scholar]
- 20.Bongajum Yenban A, Foumane P, Moussi C, Vogue N, Banseka H, Nwobegahay J, et al. Strengthening maternal death surveillance systems for Evidence-Based decision making in Sub-Saharan africa: the case of the center region in Cameroon. Int J MCH AIDS 1 Déc. 2021;10(2):258–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bernard YM, Ahmed J, Mostel J, Ba T, Ciceron AC, Busiga M, et al. Clinical outreach training and supportive supervision quality-of-care analysis: impact of readiness factors on health worker competencies in malaria case management in Cameroon, Mali, and Niger. Am J Trop Med Hyg. 2024;110(3):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amouzou A, Leslie HH, Ram M, Fox M, Jiwani SS, Requejo J, et al. Advances in the measurement of coverage for RMNCH and nutrition: from contact to effective coverage. BMJ Glob Health Mai. 2019;4(Suppl 4):e001297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marsh AD, Muzigaba M, Diaz T, Requejo J, Jackson D, Chou D, et al. Effective coverage measurement in maternal, newborn, child, and adolescent health and nutrition: progress, future prospects, and implications for quality health systems. Lancet Global Health Mai. 2020;8(5):e730–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Do M, Micah A, Brondi L, Campbell H, Marchant T, Eisele T, et al. Linking household and facility data for better coverage measures in reproductive, maternal, newborn, and child health care: systematic review. J Global Health Déc. 2016;6(2):020501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karim A, De Savigny D. Effective coverage in health systems: evolution of a concept. Dis 22 Févr. 2023;11(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Exley J, Gupta PA, Schellenberg J, Strong KL, Requejo JH, Moller AB, et al. A rapid systematic review and evidence synthesis of effective coverage measures and cascades for childbirth, newborn and child health in low- and middle-income countries. J Glob Health 15 Janv. 2021;12:04001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khatri RB, Durham J, Karkee R, Assefa Y. High coverage but low quality of maternal and newborn health services in the coverage cascade: who is benefitted and left behind in accessing better quality health services in nepal?? Reprod Health 19 Juill. 2022;19(1):163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–92. [DOI] [PubMed] [Google Scholar]
- 29.Addisu D, Mekie M, Melkie A, Abie H, Dagnew E, Bezie M, et al. Continuum of maternal healthcare services utilization and its associated factors in ethiopia: A systematic review and meta-analysis. Womens Health (Lond Engl) Janv. 2022;18:17455057221091732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ministère de la Santé Publique. 2016. Rapport d’évaluation rapide des besoins en soins obstétricaux et néonatals d’urgence. Yaoundé, Cameroun. Yaoundé, Cameroun. Available: http://cdnss.minsante.cm/
- 31.World Health Organization. Service Availability and Readiness Assessment (SARA), Reference Manual, Version 2.2. Geneva, World Health Organization. 2015. Available: https://iris.who.int/bitstream/handle/10665/149025/WHO_HIS_HSI_2014.5_eng.pdf?sequence=1
- 32.World Health Organization. Standards for improving quality of maternal and newborn care in health facilities. Geneva, World Health Organization. 2016. Available: https://iris.who.int/bitstream/handle/10665/249155/9789241511216-eng.pdf?sequence=1
- 33.World Health Organization. WHO recommendations: optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. Geneva, World Health Organization. 2012. Available: https://iris.who.int/bitstream/handle/10665/77764/9789241504843_eng.pdf?sequence=1 [PubMed]
- 34.World Health Organization. Priority life-saving medicines for women and children. Geneva, World Health Organization., 2012. Available: https://iris.who.int/bitstream/handle/10665/75154/WHO_EMP_MAR_2012.1_eng.pdf?sequence=1
- 35.Shengelia B, Tandon A, Adams OB, Murray CJL. Access, utilization, quality, and effective coverage: an integrated conceptual framework and measurement strategy. Social Sci Med Juill. 2005;61(1):97–109. [DOI] [PubMed] [Google Scholar]
- 36.Sauer SM, Pullum T, Wang W, Mallick L, Leslie HH. Variance Estimation for effective coverage measures: A simulation study. J Glob Health Juin. 2020;10(1):010506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang W, Mallick L, Allen C, Pullum T. Effective coverage of facility delivery in Bangladesh, Haiti, Malawi, Nepal, Senegal, and Tanzania. PLoS One. 2019;14(6):e0217853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schlotheuber A, Hosseinpoor A. Summary measures of health inequality: a review of existing measures and their application. IJERPH. 2022;19(6): 3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kruk ME, Leslie HH, Verguet S, Mbaruku GM, Adanu RMK, Langer A. Quality of basic maternal care functions in health facilities of five African countries: an analysis of national health system surveys. Lancet Glob Health. 2016;4(11):e845-55. [DOI] [PubMed] [Google Scholar]
- 40.Gabrysch S, Nesbitt RC, Schoeps A, Hurt L, Soremekun S, Edmond K, et al. Does facility birth reduce maternal and perinatal mortality in brong ahafo, ghana?? A secondary analysis using data on 119 244 pregnancies from two cluster-randomised controlled trials. Lancet Global Health Août. 2019;7(8):e1074–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leslie HH, Malata A, Ndiaye Y, Kruk ME. Effective coverage of primary care services in eight high-mortality countries. BMJ Glob Health. 2017;2(3): e000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Onambele L, Ortega-Leon W, Guillen-Aguinaga S, Forjaz MJ, Yoseph A, Guillen-Aguinaga L et al. oct. Maternal Mortality in Africa: Regional Trends (2000–2017). Int J Environ Res Public Health. 2022;19(20):13146. [DOI] [PMC free article] [PubMed]
- 43.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health Juin. 2014;2(6):e323–33. [DOI] [PubMed] [Google Scholar]
- 44.Kumah E. The informal healthcare providers and universal health coverage in low and middle-income countries. Global Health 27 Avr. 2022;18(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hirose A, Yisa IO, Aminu A, Afolabi N, Olasunmbo M, Oluka G, et al. Technical quality of delivery care in private- and public-sector health facilities in Enugu and Lagos states, Nigeria. Health Policy Plan. 2018;33(5):666–74. [DOI] [PubMed] [Google Scholar]
- 46.Azevedo MJ. The State of Health System(s) in Africa: Challenges and Opportunities. In: Historical Perspectives on the State of Health and Health Systems in Africa, Volume II. Cham: Springer International Publishing; 2017. pp. 1–73. Available: https://link.springer.com/10.1007/978-3-319-32564-4_1
- 47.Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Global Health 1 Nov. 2018;6(11):e1196–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yoo Ehye, Palermo T, Maluka S. Geostatistical linkage of National demographic and health survey data: a case study of Tanzania. Popul Health Metrics Déc. 2021;19(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carter ED, Ndhlovu M, Eisele TP, Nkhama E, Katz J, Munos M. Evaluation of methods for linking household and health care provider data to estimate effective coverage of management of child illness: results of a pilot study in Southern province, Zambia. J Global Health Juin. 2018;8(1):010607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leslie HH, Sun Z, Kruk ME. Association between infrastructure and observed quality of care in 4 healthcare services: a cross-sectional study of 4,300 facilities in 8 countries. PLoS Med. 2017;14(12): e1002464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Exley J, Marchant T. Inequalities in effective coverage measures: are we asking too much of the data? BMJ Glob Health. 2022;7(5): e009200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this analysis are publicly available upon request from the DHS Program (http://www.dhsprogram.com) and the National Institute of Statistics (https://ins-cameroun.cm/).