Abstract
Three cases of atypical ectopic pregnancies requiring surgical evaluation are presented. The first case represents an undiagnosed heterotopic pregnancy who initially presented with a 1st trimester spontaneous abortion and subsequently a ruptured ectopic pregnancy. The second case represents an omental ectopic pregnancy vs an extruded tubal ectopic pregnancy following a salpingectomy requiring omentectomy and appendectomy. The third case showcases a chronic cornual ectopic pregnancy incidentally found during a robotic myomectomy. These cases highlight uncommon presentations of atypical ectopic pregnancies, diagnostic challenges, and surgical treatment.
Keywords: Heterotopic pregnancies, Interstitial ectopic pregnancies, Laparoscopy, Omental ectopic pregnancies
INTRODUCTION
Ectopic pregnancies account for 2% of all pregnancies.1 These are potentially life-threatening conditions that can have a variety of clinical presentations and remains a leading cause of maternal morbidity and mortality. Three cases of atypical ectopic pregnancies requiring surgical management are presented.
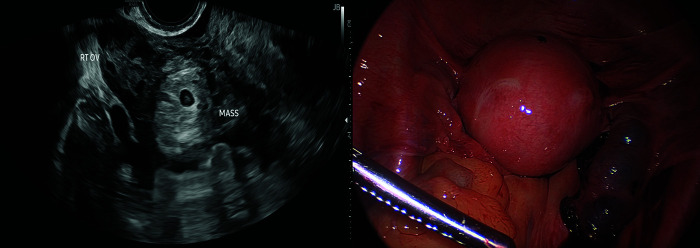
Patient #1 is a 38-year-old G8P2 with recent 6-week confirmed intrauterine pregnancy who presented with pelvic pain and abnormal uterine bleeding (AUB). The patient reported passing of fetal tissue with AUB during the past week. On admission, pelvic ultrasound showed a new complex adnexal mass with a fetal pole and surrounding fluid and no gestational sac within the endometrium. β-hCG rose to 4,589 mIU/mL from 2,900 mIU/mL from 10 days prior. She underwent laparoscopic right salpingectomy for a ruptured fallopian tube ectopic pregnancy. Pathology confirmed chorionic villi. This was a heterotopic pregnancy following a spontaneous abortion (SAB) (Figure 1).
Figure 1.
Pelvic US demonstrating a right gestational sac with fetal pole in the right adnexa.
Laparoscopy is consistent with ruptured right fallopian tube ectopic pregnancy.
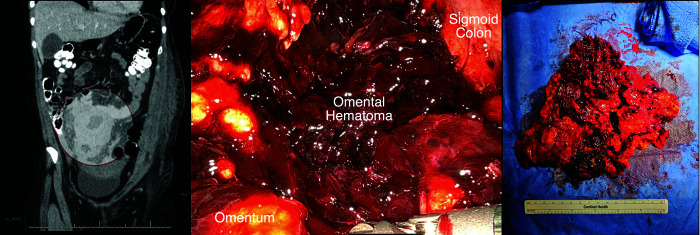
Patient #2 is a 35-year-old G1P0 presenting for symptomatic anemia (Hgb 6.8 g/dL) postoperative day 2 after a right salpingectomy and ovarian cystectomy for ruptured ectopic pregnancy and endometriomas from another gynecologist. Initial pelvic ultrasound demonstrated a right adnexal gestation measuring 2.3 cm without fetal cardiac activity, large complex free fluid, and a 5-cm right hemorrhagic ovarian cyst with a β-hCG level of 20,368 mIU/mL. After surgery, patient was discharged home. Pathology revealed endometriosis of the right fallopian tube without evidence of chorionic villi. She represented to the hospital for symptomatic anemia and recommended by her gynecologist after review of pathology without chorionic villus. On admission, CT abdomen/pelvis demonstrated intraabdominal hematomas measuring 6.9 and 5.1 cm. β-hCG level decreased to 6,807 mIU/mL. The patient underwent robotic evacuation of hemoperitoneum, omentectomy, and appendectomy. Intraoperatively, there were large omental hematomas with active arterial bleeding and diffuse inflammation of the pelvis and fibrotic mildly-dilated appendix. A total of 1,000 mL of hemoperitoneum was evacuated. Pathology demonstrated chorionic villi in the omental hematoma, suggesting either a missed-diagnosed omental ectopic or an extruded tubal ectopic with persistent bleeding (Figure 2). β-hCG levels were trended outpatient weekly until negative.
Figure 2.
CT A/P demonstrating a 6.9- and 5.1-cm hematoma.
A large omental hematoma with diffuse inflammatory reaction and active arterial bleeding. Subsequent omentectomy was confirmatory for chorionic villus.
Patient #3 is a 37-year-old G1P1 who underwent a robotic-assisted myomectomy for AUB-leiomyoma. A negative preoperative pregnancy test was followed by intraoperative discovery of necrotic and hemorrhagic tissue in the left cornua. Pathology confirmed chorionic villi consistent with a chronic cornual ectopic pregnancy (Figure 3).
Figure 3.

A left chronic cornual ectopic pregnancy appearing hemorrhagic and necrotic soft tissue incidentally discovered during myomectomy.
The rarity of heterotopic and nontubal ectopic pregnancies contributes to diagnostic challenges, often resulting in delayed treatment and increased morbidity and mortality.2,3 Heterotopic pregnancies occur in 1/30,000 spontaneous pregnancies and SAB can occur in 26% of heterotopic pregnancies.2,4 Patient #1’s case is unique as the initial evaluation occurred directly after an SAB in the setting of a new complex adnexal mass. In contrast, heterotopic pregnancies are more commonly diagnosed in the presence of both an intra-uterine and extrauterine pregnancies.
Interstitial and abdominal ectopic pregnancies account for 2% and 1% of ectopic cases, respectively.3 Interstitial pregnancies are always nonviable and often have negative or low β-hCG levels as a result of impaired trophoblastic implantation, nonviable trophoblastic tissue, and chronic degneration.3,5 Chronic unruptured interstitial pregnancy is a rare form. A thorough abdominopelvic survey is necessary during surgical evaluation as endometriosis may obstruct fallopian tubes masquerading as a potential ectopic pregnancy or be concealed in another intra-abdominal sites such as the omentum. Early detection and high index of suspicion is crucial in improving treatment timing and decreasing morbidity and mortality.
Footnotes
Disclosure: none.
Conflict of interests: none.
Funding sources: none.
Contributor Information
Bruce Lee, Center for Gynecologic Oncology, Herbert Wertheim College of Medicine, Florida International University, Miramar, Florida, USA. (Drs. Lee and Salom).
Emery M. Salom, Center for Gynecologic Oncology, Herbert Wertheim College of Medicine, Florida International University, Miramar, Florida, USA. (Drs. Lee and Salom).
Alexa Marie Del Mazo, College of Osteopathic Medicine, NOVA Southeastern University, Davie, Florida, USA. (Dr. Del Mazo).
References:
- 1.Tubal Ectopic Pregnancy. ACOG Practice Bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists. Washington, DC: American College of Obstetricians and Gynecologists. [Google Scholar]
- 2.Maleki A, Khalid N, Rajesh Patel C, El-Mahdi E. The rising incidence of heterotopic pregnancy: current perspectives and associations with in-vitro fertilization. Eur J Obstet Gynecol Reprod Biol. 2021;266:138–144. [DOI] [PubMed] [Google Scholar]
- 3.Sokalska A, Rambhatla A, Dudley C, Bhagavath B. Nontubal ectopic pregnancies: overview of diagnosis and treatment. Fertil Steril. 2023;120(3 Pt 2):553–562. [DOI] [PubMed] [Google Scholar]
- 4.Talbot K, Simpson R, Price N, Jackson SR. Heterotopic pregnancy. J Obstet Gynaecol. 2011;31(1):7–12. [DOI] [PubMed] [Google Scholar]
- 5.Yang C, Huang D, Zhang S. Chronic cornual ectopic pregnancy presenting as large cornual mass after in vitro fertilization-embryo transfer: a case report. Laparosc Endosc Robot Surg. 2019;2(4):99–101. [Google Scholar]