Abstract
Articular cartilage lesions of the knee are common and can lead to persistent symptoms of pain, swelling, and limitations in activity for many active individuals. In the middle-aged patient, cartilage repair options have been shown to have greater failure rates. Total or unicompartmental knee arthroplasty also can be considered but may be undesirable for active patients because of the morbidity of the procedure as well as postoperative activity limitations. Focalplasty is a minimally invasive technique to treat focal chondral and osteochondral lesions of the knee with 3-dimensional−printed porous titanium implants that allow for bony ingrowth and immediate weight-bearing. This technical note demonstrates implantation technique for both the tibial and femoral implants for application in focal tibiofemoral disease.
Technique Video
Focal articular cartilage lesions of the knee can be painful and debilitating, affecting sports participation in younger patients and work for older patients.1,2 Untreated lesions can progress to osteoarthritis.3 The gold standard treatment for large symptomatic focal lesions in younger patients is either osteochondral autograft transplantation surgery, osteochondral allograft transplantation, or matrix-associated autologous chondrocyte implantation. These therapies can be quite successful but are associated with considerable cost and rehabilitation.2,4, 5, 6, 7 Alternatively, either unicompartmental or total knee arthroplasty are treatment options. The complication profile, high risk for future revision, and functional limitations make these options suboptimal for young and middle-aged patients without widespread cartilage involvement.7, 8, 9 This leaves a considerable treatment gap for those patients too old for biologic cartilage restoration and too young or active for arthroplasty.
Resurfacing of the femoral condyle and tibial plateau with metallic inlay implants is not an entirely new concept. HemiCAP/UniCAP, Episealer, and BioPoly RS Knee are all implants that have been introduced over roughly the last 20 years. Midterm survivorship for these implants has been favorable.10, 11, 12, 13 We present a surgical technique for a 3-dimensional−printed porous titanium implant that encourages bony ingrowth for the treatment of focal cartilage lesion of the knee (Video 1).14,15 The implant is a 3D-printed titanium alloy baseplate that features 0.225-mm thick individual beams that make up the porous, lattice-like architecture. This creates a 65% porous structure that is similar to trabecular bone. This design reduces stress shielding and supports the baseplate integrity for biological osseointegration. A titanium nitride coating enhances surface durability and biocompatibility, offering improved wear and corrosion resistance. The tibial-bearing surface features a vitamin E, highly cross-linked molecular weight polyethylene.
Surgical Technique
Patient Evaluation, Imaging, and Indications
Patients are evaluated with history and physical examination, with priority on patients having single-compartment (medial or lateral) symptoms, best described by asking a patient to point with one finger where their pain is the most. Weight-bearing radiographs are obtained to ensure absence of high-grade joint space narrowing, in which patients may be better served with a traditional unicompartmental or total knee arthroplasty. Mild varus and valgus malalignment is acceptable. Magnetic resonance imaging (MRI) scans are scrutinized with attention toward the articular cartilage of the weight-bearing portions of the femoral condyle and tibial plateau. Concomitant pathology of the meniscus and ligaments are assessed as well with the goal to have at least 50% intact meniscus. Indications for knee focalplasty (bipolar resurfacing) includes middle-aged patients with focal chondral defects of the tibiofemoral compartment who are otherwise not suitable candidates for traditional arthroplasty or cartilage repair and transplantation options. Advantages include relatively rapid recovery, minimally invasive nature, and potential for long-term integration.
Arthroscopic Evaluation
The patient is positioned supine with a lateral post and heel bump to support the knee in 90° of flexion. We begin with standard diagnostic arthroscopy to identify concomitant intra-articular pathology and confirm the cartilage defect identified on preoperative MRI scan. Concomitant meniscus pathology is treated to maintain at least 50% remaining meniscus to prevent excessive point loading of the implant or opposing surface (Fig. 1).
Fig 1.
Intraoperative views of the left knee of a patient in the supine position, viewing the medial compartment with a 30° arthroscope (Arthrex, Naples, FL) from the anterolateral portal. Superior, inferior, femoral condyle, and tibial plateau are labeled to orient the reader. The authors frequently indicate focalplasty to treat cartilage pathology of the medial femoral condyle encountered at the time of acute meniscus root tear repair. The authors’ preferred technique is a transtibial pullout technique with a meniscus centralization stitch (Arthrex). (A) Focal cartilage lesion on the medial femoral condyle indicated by the multiple arrows. (B) Drill sleeve in place for meniscal centralization anchor and arrows denoting focal tibial cartilage lesion. (C) Arthroscopic probe assessing meniscal stability, arrow demonstrating meniscal centralization stitch. (D) Transtibial pull-out posterior meniscal root repair with luggage tagged high tensile strength suture indicated by arrow.
Mini-Open Medial or Lateral Parapatellar Arthrotomy
After arthroscopic evaluation, a roughly 5-cm longitudinal skin incision is made along the medial or lateral border of the patellar tendon and a parapatellar arthrotomy is performed. Excision of the fat pad with bovie electrocautery aids in visualization. If the tibial defect will be treated, the periosteum and soft tissues of the proximal medial or lateral tibia are elevated, taking care to preserve the superficial medial collateral ligament, iliotibial band insertion at the Gerdy tubercle, and the lateral collateral ligament. Deep Z-retractors are placed on either side of the femoral condyle with care to protect the cruciate ligaments. The knee is flexed beyond 90° with external rotation (medial side) or internal rotation (lateral side) to expose the plateau. The anterior horn of the meniscus may be detached if needed and can be re-attached at the conclusion of the case using suture anchors.
Tibial Preparation
The tibial guide (OvertureTi, Irvine, CA) is placed to size the defect and oriented in the proper rotation, and the guide pin is drilled (Video 1). Tibial implants are available in various circular sizes to adequately resurface the defect. Next, the cannulated scoring tool is used to create a clean cut on the edge of articular cartilage down to the subchondral bone. The power reamer is used first, then followed by the secondary hand reamer until the high side (with laser mark) of the reamer is recessed 0.5 to 1 mm to the adjacent cartilage surface. The pin is removed, and the trial is inserted and confirmed.
Femoral Preparation
The femoral condyles are then exposed with Z-retractors and the defect is sized with the appropriate guide (OvertureTi). Femoral implants are available in both circular and oval/oblong shapes. Drill pin is placed and the articular cartilage is scored. Again, primary power and secondary hand reamers are used to slightly recess the implant to 0.5 to 1 mm below the articular surface. Oblong implants are prepared using 2 overlapping reamers in a “snowman” configuration as determined by the drill guide. The femoral trial is placed and stability confirmed.
Final Implantation
At this point all trials are removed, the femoral and tibial peg holes are drilled, and the defect is irrigated. A pea-sized amount of Simplex bone cement (Stryker, Kalamazoo, MI) is placed in the central peg defect only, leaving the majority of the implant contacting cancellous bone for ingrowth. The final implants are placed by hand in-line with the original angle of reaming, and gently impacted to fully seat the implants (OvertureTi). Particular attention should be paid to make sure the trial and final implant heights are slightly recessed compared with surrounding cartilage to help prevent early wear. This can be done by using a freer elevator to gently palpate a slight step-off of the cartilage to the final implant (Fig 2). Standard closure is performed according to the surgeon’s preference.
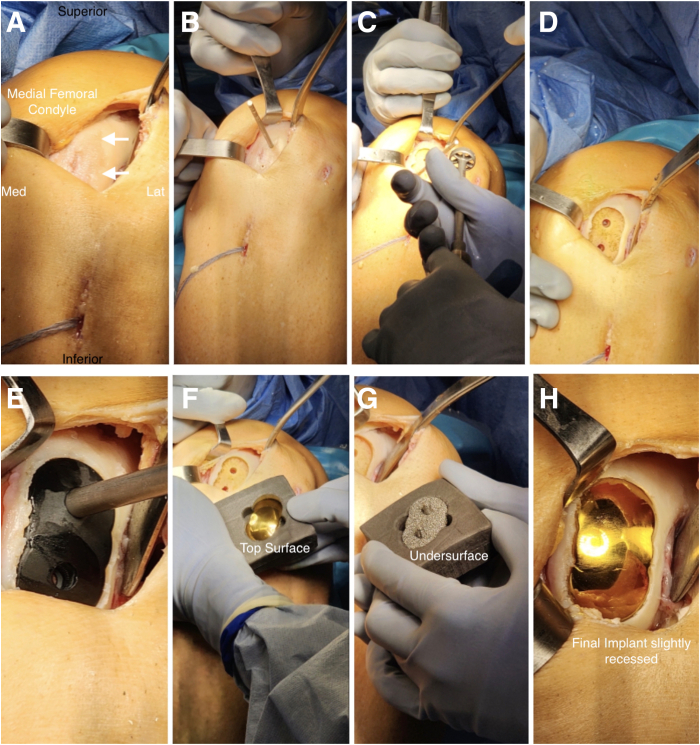
Fig 2.
Clinical photographs of a left medial femoral condyle focalplasty of a patient in the supine position with the left knee flexed at 90°. Superior, inferior, medial, and lateral are labeled for orientation. (A) Medial parapatellar arthrotomy with medial femoral condyle cartilage lesion exposed highlighted by arrows. Transtibial pull-out posterior meniscal root sutures in place inferiorly. (B) Superior femoral pin in place. (C) The lesion has primarily been reamed and the secondary, hand reamer, is being loaded. (D) Final oblong defect has been created after superior, inferior, and central reaming. (E) Femoral oblong trial is in place to confirm fit and depth. (F) Top view of final femoral oblong component bearing surface. (G) Final femoral oblong component backside is seen with 3-dimensional−printed porous coating and 2 barbed pegs. (H) Final implant in position after cementing; note the slight recession compared with surrounding cartilage.
Postoperative Management
Postoperative protocol is dictated by the presence of concomitant procedures. If focalplasty was performed alone, patients are able to immediately weight bear as tolerated. If meniscal repair is performed, patients are limited to touchdown weight-bearing for 4 to 6 weeks and placed in a hinged knee brace. Range of motion for physical therapy is allowed with 0 to 90° for 6 weeks. Patients are transitioned to weight-bearing and range of motion as tolerated after 6 weeks. Impact activities are avoided for 4 to 6 months after surgery.
Discussion
Focalplasty is a surgical option for active patients with focal cartilage lesions. Compared with arthroplasty and biologic resurfacing, it offers certain advantages and risks (Table 1). Namely, it is considerably less expensive and more available than biologic options.2,4, 5, 6 Also, it has a much more tolerable risk profile than knee arthroplasty.7, 8, 9 Although it is not designed to replace either procedure, it fills the treatment gap for patients who are unideal candidates for either.
Table 1.
Advantages and Risks of Focalplasty
Advantages
|
Technical considerations for focalplasty may be especially helpful for early career surgeons or first-time users (Table 2). Although slightly nuanced, the technique is fairly straightforward, and the authors believe the learning curve to be short. Although the implant features a porous trabecular architecture, immediate mechanical stability is increased by cement stabilization of a small central peg until bony ingrowth occurs on the porous backside of the implant. Careful patient selection for focal resurfacing metallic implants involves a thorough clinical assessment, correlating symptoms with isolated full-thickness chondral defects typically in younger, active individuals with preserved joint space and alignment. Imaging, especially MRI and weight-bearing radiographs—is essential to confirm lesion size, depth, and to rule out diffuse arthropathy or malalignment, which are contraindications for this joint-preserving approach.
Table 2.
Pearls and Pitfalls of Focalplasty
Pearls
|
Focalplasty is a minimally invasive technique to treat focal chondral and osteochondral lesions of the knee with 3-dimensional−printed porous titanium implants. The trabecular architectural design mimics cancellous bone to promote biological integration. The surgical technique should be comfortable and reproducible for surgeons who routinely operate on the knee. Modern implant design allows for theoretical stable long-term fixation.14, 15, 16 In addition, because focalplasty is bone preserving, it could theoretically be revised to a total knee arthroplasty with primary components with disease progression. Long-term follow-up studies are needed for outcomes and survivorship.
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: T.W. reports equipment, drugs, or supplies were provided by Overture Orthopaedics and equity or stocks with Overture Orthopaedics. All other authors (J.V., C.C.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
Video demonstration of a tibial and femoral focalplasty technique on a sawbones followed by a medial femoral condyle focalplasty on a middle-aged patient. All knees are left. Surgery is performed with the patient under general anesthesia while lying supine on an operating room table with a lateral post. All arthroscopic images are taken with a 30° arthroscope in the anterolateral portal.
References
- 1.Steinwachs M.R., Engebretsen L., Brophy R.H. Scientific evidence base for cartilage injury and repair in the athlete. Cartilage. 2012;3(1 suppl):11S–17S. doi: 10.1177/1947603511415841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dean R.S., Hinckel B.B., Omari A., Hutchinson I., Gomoll A.H. In: Knee arthroscopy and knee preservation surgery. Sherman S.L., Chahla J., Rodeo S.A., LaPrade R., editors. Springer International Publishing; Cham: 2023. Treatment of focal cartilage defects of the knee: Classic and new procedures; pp. 1–18. [Google Scholar]
- 3.Ghouri A., Muzumdar S., Barr A.J., et al. The relationship between meniscal pathologies, cartilage loss, joint replacement and pain in knee osteoarthritis: A systematic review. Osteoarthritis Cartilage. 2022;30:1287–1327. doi: 10.1016/j.joca.2022.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Pareek A., Reardon P.J., Macalena J.A., et al. Osteochondral autograft transfer versus microfracture in the knee: A meta-analysis of prospective comparative studies at midterm. Arthroscopy. 2016;32:2118–2130. doi: 10.1016/j.arthro.2016.05.038. [DOI] [PubMed] [Google Scholar]
- 5.Wang T., Gao S.L., McCauley J.C., Densley S.M., Bugbee W.D. Outcomes after osteochondral allograft transplantation of the medial femoral condyle in patients with varus and nonvarus alignment. Am J Sports Med. 2024;52:3013–3020. doi: 10.1177/03635465241273947. [DOI] [PubMed] [Google Scholar]
- 6.Ebert J.R., Klinken S., Fallon M., Wood D.J., Janes G.C. Clinical and radiological outcomes at ≥10-year follow-up after matrix-induced autologous chondrocyte implantation in the patellofemoral joint. Am J Sports Med. 2024;52:2532–2540. doi: 10.1177/03635465241262337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Everhart J.S., Campbell A.B., Abouljoud M.M., Kirven J.C., Flanigan D.C. Cost-efficacy of knee cartilage defect treatments in the United States. Am J Sports Med. 2020;48:242–251. doi: 10.1177/0363546519834557. [DOI] [PubMed] [Google Scholar]
- 8.Walker-Santiago R., Tegethoff J.D., Ralston W.M., Keeney J.A. revision total knee arthroplasty in young patients: Higher early reoperation and rerevision. J Arthroplasty. 2021;36:653–656. doi: 10.1016/j.arth.2020.08.052. [DOI] [PubMed] [Google Scholar]
- 9.Hernandez N.M., Wu C.J., Hinton Z.W., Ryan S.P., Bolognesi M.P., Seyler T.M. Primary total knee arthroplasty in patients aged 45 years or younger: 162 total knee arthroplasties with a mean follow-up duration of 7 years. Arthroplast Today. 2022;18:163–167. doi: 10.1016/j.artd.2022.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ayers D.C., Yousef M., Yang W., Zheng H. Age-related differences in pain, function, and quality of life following primary total knee arthroplasty: Results from a FORCE-TJR (Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement) cohort. J Arthroplasty. 2023;38(7 suppl 2):S169–S176. doi: 10.1016/j.arth.2023.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Fuchs A., Eberbach H., Izadpanah K., Bode G., Südkamp N.P., Feucht M.J. Focal metallic inlay resurfacing prosthesis for the treatment of localized cartilage defects of the femoral condyles: A systematic review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2018;26:2722–2732. doi: 10.1007/s00167-017-4714-4. [DOI] [PubMed] [Google Scholar]
- 12.Ryd L., Flodström K., Manley M.T. Patient-specific implants for focal cartilage lesions in the knee: Implant survivorship analysis up to seven years post-implantation. Surg Technol Int. 2020;38:379–386. [PubMed] [Google Scholar]
- 13.Spalding T., Damasena I. Next generation cartilage repair and the pre-arthroplasty patient. Pre-arthroplasty artificial implants part B: Metallic. Oper Tech Sports Med. 2022;30(4) [Google Scholar]
- 14.Megaloikonomos P.D., Becher C., Van der Stok J., O'Donnell T. Femoral condyle resurfacing using an inlay metal implant: Low revision rate of 266 patients in a 5-10 years follow-up. Arch Orthop Trauma Surg. 2023;143:1243–1251. doi: 10.1007/s00402-021-04251-x. [DOI] [PubMed] [Google Scholar]
- 15.McGilvray K.C., Easley J., Seim H.B., et al. Bony ingrowth potential of 3D-printed porous titanium alloy: A direct comparison of interbody cage materials in an in vivo ovine lumbar fusion model. Spine J. 2018;18(7):1250–1260. doi: 10.1016/j.spinee.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kovács Á.É., Csernátony Z., Csámer L., et al. Comparative analysis of bone ingrowth in 3D-printed titanium lattice structures with different patterns. Materials (Basel) 2023;16:3861. doi: 10.3390/ma16103861. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video demonstration of a tibial and femoral focalplasty technique on a sawbones followed by a medial femoral condyle focalplasty on a middle-aged patient. All knees are left. Surgery is performed with the patient under general anesthesia while lying supine on an operating room table with a lateral post. All arthroscopic images are taken with a 30° arthroscope in the anterolateral portal.