Abstract
Introduction
Diuretics are widely used in Japan for the treatment of hypertension and heart failure. Electrolyte disturbance is a common adverse reaction to diuretics and may be life-threatening. Previous studies have shown that diuretic-induced electrolyte disturbance is more common in women. Electrolyte balance is regulated by the kidneys, and renal function tends to decline with advancing age.
Objective
The aim of this study was to identify patients at high risk of adverse reactions to diuretics, considering the effects of sex, renal function, and age on susceptibility to diuretic-induced electrolyte disturbance.
Methods
Claims data for 67,135 patients on diuretics in Japan were sourced from DeSC Healthcare, Inc. The data covered the period from April 2020 to March 2021.
Results
Analysis of patient numbers using the chi-squared test showed that hyperkalemia was more common in men than in women (326 vs. 271; p = 0.003) and that hypokalemia was more common in women than in men (413 vs. 285; p < 0.001). Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for women considering age and renal function (estimated glomerular filtration rate [eGFR]). In elderly patients aged ≥ 75 years, the odds of developing hypokalemia in women compared to men were 1.47 (95% CI 1.13–1.91) for eGFR 60–30 mL/min/1.73 m2 and 2.05 (95% CI 1.08–4.10) for eGFR < 30 mL/min/1.73 m2.
Conclusion
Among women aged ≥ 75 years, those in lower eGFR groups (60–30 and < 30) had higher odds of hypokalemia compared to men. These data highlight the importance of monitoring for adverse reactions to diuretics, particularly hypokalemia, in elderly women with low eGFR.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40264-025-01564-3.
Key Points
| A retrospective analysis of claims and health check-up data from 67,135 diuretic users in Japan identified patients at high risk of electrolyte disturbances based on sex, age, and renal function. |
| Among women aged ≥ 75 years, the odds of developing hypokalemia were significantly higher than in men, specifically in patients with eGFR 60–30 and < 30 mL/min/1.73 m2. |
| Elderly women with reduced eGFR are at increased risk of hypokalemia and should be carefully monitored in clinical practice. |
Introduction
In Japan, the three leading causes of death are cancer, heart disease, and old age, and 80.9% of cases of heart disease are attributable to heart failure [1]. Heart failure occurs when the ability of the heart to pump blood is weakened and leads to symptoms that include shortness of breath, fatigue, and edema. Diuretics are widely used to relieve symptoms caused by congestion in patients with heart failure [2]. Treatment of hypertension reduces the incidence of heart failure and improves the prognosis [3–6]. In general, the antihypertensive drugs used first-line are selected from the calcium channel blockers, angiotensin receptor blockers, angiotensin-converting enzyme inhibitors, and diuretics [7]. Thiazide diuretics are particularly effective in preventing heart failure [5, 8, 9]. Therefore, these drugs are widely used in clinical practice. Diuretics are widely used not only in Japan but also globally for the treatment of heart failure and hypertension. According to the European Society of Cardiology (ESC) and the American Heart Association (AHA), diuretics are recommended for symptom relief in all types of heart failure and as adjunct therapy in hypertension management [10, 11].
The main action of diuretics is correction of excess fluid retention. Loop and thiazide diuretics act on the renal tubules to inhibit reabsorption of sodium, thereby reducing reabsorption of water and increasing urine volume. Electrolyte disturbance is a life-threatening adverse reaction to diuretics and typically includes an excess or deficiency of potassium or sodium. These abnormalities are generally diagnosed based on blood test results and patient symptoms. These conditions cannot be accurately diagnosed without laboratory tests, and may present with a variety of subjective symptoms. Hyponatremia can manifest as weakness, nausea, seizures and coma [12], while hypokalemia may cause leg cramps, weakness, and arrhythmias [13]. The package inserts for thiazide diuretics refers to these symptoms as “clinically significant adverse reactions.”
Electrolyte levels are regulated by the kidneys, and electrolyte disturbance is more likely to occur in the presence of decreased renal function. Typically, renal function tends to decrease as part of the age-related decline in physiological function [14]. In a super-aging society like Japan, it is essential to take renal function into consideration when prescribing diuretics. Moreover, potassium levels are strongly associated with mortality, exhibiting a U-shaped relationship in which both hypokalemia and hyperkalemia are linked to increased risk of death. This relationship is further influenced by the presence of comorbidities such as heart failure, diabetes mellitus, and chronic kidney disease [15–17]. However, it is unclear to what extent renal function is actually considered in drug treatment. The estimated glomerular filtration rate (eGFR) is widely used to evaluate renal function in the clinical setting [18]. Japanese employers are required to refer their employees for an annual health checkup, which includes laboratory tests of kidney function, such as eGFR, as needed. Health checkup data are recorded in a cloud system linked to the My Number (individual identification number) and provided to medical institutions with the employee’s consent. The government expects healthcare workers to use these health checkup data to provide the best possible medical care for the population of Japan.
In addition to renal function and age, the sex of the patient needs to be considered when assessing the risk of adverse reactions to pharmacotherapy. Several reports have shown that the incidence of adverse reactions is higher in women [19, 20]. We have previously reported that data comparing the dosage, adverse reactions and pharmacokinetics of drugs according to sex are available for only 4.5% (76/1679) of all Japanese package inserts of prescription drugs [21]. Furthermore, it is clear that hospitalization for adverse drug reactions is more common in women than in men [22–24]. Women taking diuretics—particularly thiazide diuretics—have also been found to be at greater risk of hospitalization as a result of hyponatremia than their men counterparts [25–27]. These data suggest that information regarding sex differences is necessary for safe implementation of pharmacotherapy. Older age and reduced renal function have also been shown to increase the risk of electrolyte disturbance [28]. However, it is unclear which of sex, age, and renal function is more likely to cause electrolyte disturbance in day-to-day medical care. The aim of this study was to identify patients at high risk for diuretic-induced electrolyte disturbance and to obtain information on its prevention and early detection.
Materials and Methods
Data Source
Patient information was extracted from health insurance claims data and medical checkup data held in the DeSC database (DeSC Healthcare, Inc., Japan, Tokyo), which include claims data from the Health Insurance Association, National Health Insurance, and the Advanced Elderly Medical Service System in Japan. The claims data include basic information such as date of birth, sex, disease information with the International Classification of Diseases 10th revision (ICD-10) code, and drug information with the Anatomical Therapeutic Chemical classification. The medical checkup data were referenced to eGFR data linked to the patient ID in the claims data.
Study Design and Population
The study had a retrospective cohort design and included patients who had been prescribed oral diuretics between April 2020 and March 2021 and had eGFR data available. In view of the different formula used to calculate renal function and the fact eGFR cannot be calculated for individuals under 20 years of age, data for individuals in this age group were excluded. eGFR was calculated using the JSN eGFRcr equation, which is commonly used in clinical practice in Japan. This equation incorporates serum creatinine, age, and sex [18].
Hypernatremia is defined as a serum sodium concentration greater than 145 mmol/L, whereas hyponatremia is defined as a serum sodium concentration less than 136 mmol/L [29, 30]. Similarly, hyperkalemia is defined as a serum potassium concentration greater than 5.0 or 5.5 mmol/L, whereas hypokalemia is defined as a serum potassium concentration less than 3.5 mmol/L [31, 32]. Patients with a diagnosis of electrolyte disturbances, including imbalances in potassium and sodium, were selected using the ICD-10 codes shown in Table 1. Patients who had been taking diuretics within the 14 days before diagnosis of an electrolyte disturbances were defined as having a diuretic-induced adverse reaction. Only the first electrolyte disturbance that occurred during the study period was included in the analysis. When multiple electrolyte disturbances were diagnosed on the same day, each was counted. The analysis included combination products containing diuretics. Regarding diuretics, single drugs and combination drugs were selected from among the drugs classified as “diuretics” in the “drugs and related comorbidities” section of the “Japan standard commodity classification.” [Electronic Supplementary Material (ESM) file1].
Table 1.
ICD-10 codes for electrolyte disturbances
| ICD-10 code | Electrolyte disturbances |
|---|---|
| E87.0 | Hyperosmolality and hypernatremia |
| E87.1 | Hypo-osmolality and hyponatremia |
| E87.5 | Hyperkalemia |
| E87.6 | Hypokalemia |
ICD-10, International Classification of Diseases 10th revision
Patient Characteristics
Data for the types of diuretics prescribed, age, and eGFR were analyzed according to sex and age group (20 to < 65 years, 65 to < 75 years, or ≥ 75 years) at the start of the study period. These age groups are consistent with those defined by the Japanese “Act on Assurance of Medical Care for Elderly People.” Renal function was classified as normal (eGFR > 60 mL/min/1.73 m2), mildly impaired (eGFR 60–30 mL/min/1.73 m2), or severely impaired (eGFR < 30 mL/min/1.73 m2).
Data Analysis
Odds ratios (ORs) and 95% confidence intervals (95% CI) were calculated for the likelihood of diuretic-induced electrolyte disturbances according to sex. The statistical analysis was performed using Stata/MP 17 for Windows (Stata Corp. LLC, College Station, TX, USA). The p-values were calculated using the chi-squared test and considered statistically significant at p < 0.05.
Results
Patient Characteristics
A total of 67,135 patients (men, n = 32,548; women, n = 34,587) were prescribed diuretics during the study period (Table 2). Risk factors for adverse reactions to diuretics were sought in these patients. Classification according to age and eGFR showed that the number of patients with renal impairment increased with advancing age. Furthermore, the number of patients in the high-risk group with significantly reduced renal function (eGFR < 30 mL/min/1.73 m2) was about one-tenth that of the other groups.
Table 2.
Patient characteristics
| Total | Men (%) | Women (%) | p-value | |
|---|---|---|---|---|
| Patients, n | 67,135 | 32,548 (48.5) | 34,587 (51.5) | – |
| Age (years) | ||||
| 20 to < 65 | 10,461 | 5822 (55.7) | 4639 (44.3) | <0.001 |
| 65 to < 75 | 26,429 | 13,243 (50.1) | 13,186 (49.9) | <0.001 |
| ≥ 75 | 30,245 | 13,483 (44.6) | 16,762 (55.4) | <0.001 |
| eGFR (mL/min/1.73 m2) | ||||
| > 60 | 35,053 | 16,858 (48.1) | 18,195 (51.9) | 0.035 |
| 60–30 | 29,052 | 14,196 (48.9) | 14,856 (51.1) | 0.083 |
| < 30 | 3030 | 1494 (49.3) | 1536 (50.7) | 0.352 |
Data are shown as number and percentage of the total. Bold font indicates statistically significant differences between men and women (p < 0.05). The p-values were calculated using the chi-squared test. eGFR, estimated glomerular filtration rate
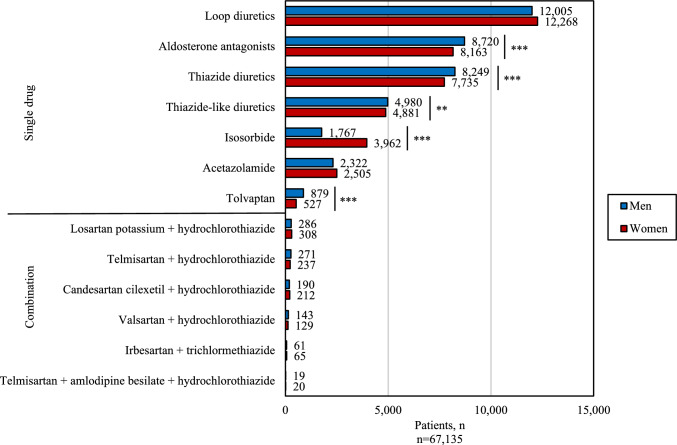
Sex Differences in the Number of Patients Prescribed Diuretics According to Pharmacological Class
The numbers of diuretics prescribed for men and women were compared according to pharmacological class (Fig. 1). Aldosterone antagonists, thiazide diuretics, thiazide-like diuretics, and tolvaptan were prescribed more frequently in men, while isosorbide was prescribed more frequently in women. Combination products containing a calcium channel blocker to lower blood pressure were prescribed less frequently.
Fig. 1.
Numbers of patients for whom diuretics were prescribed according to patient sex and pharmacological class. *p < 0.05, **p < 0.01, ***p < 0.001 (chi-squared test)
Sex Differences in Electrolyte Disturbances
The number of persons having ICD-10 codes indicating electrolyte disturbances (Table 1) were compared according to sex using the chi-squared test (Table 3). Hyperkalemia was significantly more common in men and hypokalemia was significantly more common in women. The denominators for each item were the number of men and number of women who developed electrolyte disturbances while on diuretic therapy.
Table 3.
Electrolyte disturbances in patients on diuretic therapy according to sex
| Total | Men (%) | Women (%) | p-value | |
|---|---|---|---|---|
| Patients, n | 67,135 | 32,548 | 34,587 | – |
| Electrolyte disturbances | 1494 (2.23) | 700 (2.15) | 794 (2.30) | 0.203 |
| Hyperosmolality and hypernatremia | 23 (0.03) | 14 (0.04) | 9 (0.03) | 0.234 |
| Hypo-osmolality and hyponatremia | 222 (0.33) | 95 (0.29) | 127 (0.37) | 0.089 |
| Hyperkalemia | 597 (0.89) | 326 (1.00) | 271 (0.78) | 0.003 |
| Hypokalemia | 698 (1.04) | 285 (0.88) | 413 (1.19) | <0.001 |
(%) indicates the incidence rate calculated using the number of men, the number of women, and the total number of patients, as the denominator. Bold font indicates statistically significant differences between men and women (p < 0.05). The p-values were calculated using the chi-squared test
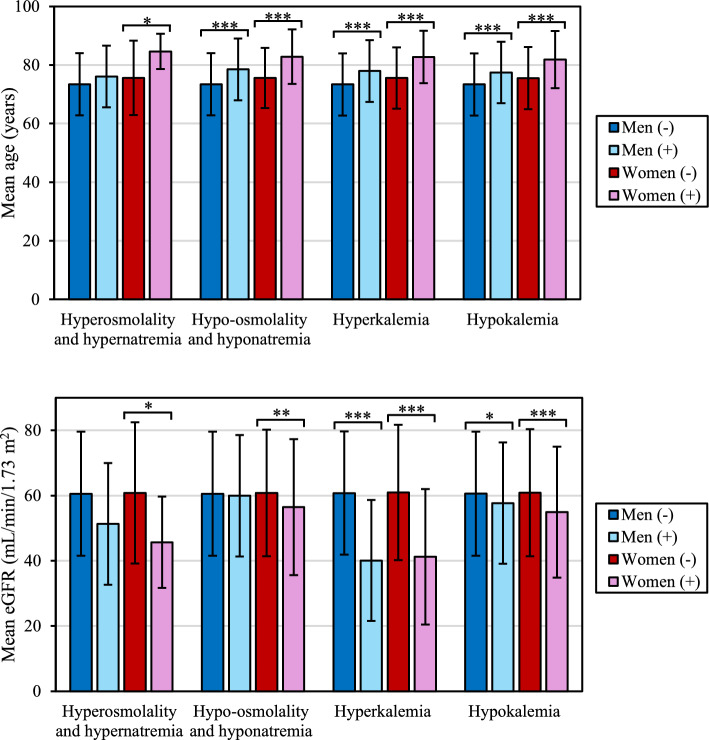
Mean Age and Renal Function in Patients with Electrolyte Disturbances According to Sex
Figure 2 shows that patients who developed electrolyte disturbances were older and had poorer renal function than those who did not regardless of sex, which is consistent with the general view. Women who were older and had impaired renal function were more likely to develop electrolyte disturbances. Patients who developed hyperkalemia had a much lower eGFR than those who did not independent of sex.
Fig. 2.
Mean (a) age and (b) eGFR in patients without (–) and with (+) diuretic-induced electrolyte disturbances according to sex *p < 0.05; **p < 0.01; ***p < 0.001; – no significant difference (chi-squared test) eGFR estimated glomerular filtration rate.
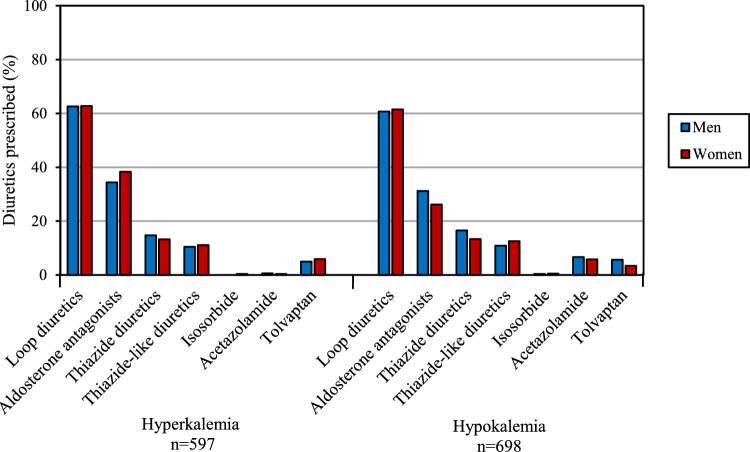
Diuretic Prescription Rate by Pharmacological Class According to Whether Patients Developed Hyperkalemia or Hypokalemia
Figure 3 shows the percentage of patients with hyperkalemia and hypokalemia prescribed diuretics by pharmacological class. Loop diuretics were prescribed for 62.6% of men and 62.7% of women with hyperkalemia and for 60.7% of men and 61.5% of women with hypokalemia.
Fig. 3.
Percentage of diuretics prescribed by pharmacological class in patients who developed hyperkalemia or hypokalemia according to sex. Data for patients taking multiple diuretics are considered as individual cases for each diuretic
Hyperkalemia and hypokalemia were rarely seen in patients taking isosorbide, which is consistent with the frequency of adverse reactions described in the package insert [33]. Similarly, hyperkalemia was also infrequently observed in patients taking acetazolamide.
Sex Differences in Patients with Hyperkalemia and Hypokalemia Based on Age and Renal Function
Comparison of renal function and age according to sex in patients who developed hyperkalemia and hypokalemia showed significant differences in several parameters (Table 4). The denominators for each item were the number of men, the number of women, and the total patient population. As shown in Table 3, data for hyperosmolality and hypernatremia and for hypo-osmolality and hyponatremia were omitted because the numbers of patients with these diagnoses were small and testing was difficult. ORs greater than 1 indicate a higher incidence of electrolyte disturbance in women. Some items were significant in non-elderly subjects and may reflect the small sample size and variability. In patients aged ≥ 75 years, the odds of developing hypokalemia in women compared to men were significantly higher in the eGFR 60–30 (OR 1.47, 95% CI 1.13–1.91) and < 30 mL/min/1.73 m2 (OR 2.05, 95% CI 1.08–4.10) groups. No significant difference was observed in the > 60 mL/min/1.73 m2 group.
Table 4.
Sex differences in age and renal function in patients with hyperkalemia and hypokalemia
| Age (years) | eGFR (mL/min/1.73 m2) | Total (%) | Men (%) | Women (%) | OR (95% CI) | p-value | |
|---|---|---|---|---|---|---|---|
| Total patient population | 20 to < 65 | > 60 | 8182 | 4370 | 3812 | – | |
| 60–30 | 2035 | 1263 | 772 | – | |||
| < 30 | 244 | 189 | 55 | – | |||
| 65 to < 75 | > 60 | 15,974 | 7552 | 8422 | – | ||
| 60–30 | 9809 | 5273 | 4536 | – | |||
| <30 | 646 | 418 | 228 | – | |||
| ≥ 75 | > 60 | 10,897 | 4936 | 5961 | – | ||
| 60–30 | 17,208 | 7660 | 9548 | – | |||
| < 30 | 2140 | 887 | 1253 | – | |||
| Total | 67,135 | 32,548 | 34,587 | ||||
| Hyperkalemia | 20 to < 65 | > 60 | 15 (0.18) | 6 (0.14) | 9 (0.24) | 1.72 (0.54, 5.86) | 0.297 |
| 60–30 | 8 (0.39) | 8 (0.63) | 0 (0) | 0.027 | |||
| < 30 | 19 (7.79) | 17 (8.99) | 2 (3.64) | 0.38 (0.04, 1.71) | 0.192 | ||
| 65 to < 75 | > 60 | 45 (0.28) | 23 (0.30) | 22 (0.26) | 0.86 (0.45, 1.61) | 0.606 | |
| 60–30 | 63 (0.64) | 43 (0.82) | 20 (0.44) | 0.54 (0.30, 0.94) | 0.021 | ||
| < 30 | 43 (6.66) | 33 (7.89) | 10 (4.39) | 0.53 (0.23, 1.13) | 0.087 | ||
| ≥ 75 | > 60 | 53 (0.49) | 30 (0.61) | 23 (0.39) | 0.64 (0.35, 1.13) | 0.097 | |
| 60–30 | 214 (1.24) | 105 (1.37) | 109 (1.14) | 0.84 (0.63, 1.11) | 0.178 | ||
| < 30 | 137 (6.40) | 61 (6.88) | 76 (6.07) | 0.89 (0.62, 1.29) | 0.450 | ||
| Total | 597 (0.89) | 326 (1.00) | 271 (0.78) | ||||
| Hypokalemia | 20 to < 65 | > 60 | 38 (0.46) | 26 (0.59) | 12 (0.31) | 0.53 (0.24, 1.09) | 0.063 |
| 60–30 | 18 (0.88) | 9 (0.71) | 9 (1.17) | 1.63 (0.57, 4.66) | 0.289 | ||
| < 30 | 1 (0.41) | 1 (0.53) | 0 (0) | 0.589 | |||
| 65 to < 75 | > 60 | 91 (0.57) | 46 (0.61) | 45 (0.53) | 0.88 (0.57, 1.35) | 0.531 | |
| 60–30 | 61 (0.62) | 27 (0.51) | 34 (0.75) | 1.46 (0.85, 2.52) | 0.136 | ||
| < 30 | 8 (1.24) | 5 (1.20) | 3 (1.32) | 1.05 (0.16, 5.48) | 0.896 | ||
| ≥ 75 | > 60 | 165 (1.51) | 64 (1.30) | 101 (1.69) | 1.31 (0.94, 1.82) | 0.091 | |
| 60–30 | 262 (1.52) | 93 (1.21) | 169 (1.77) | 1.47 (1.13, 1.91) | 0.003 | ||
| < 30 | 54 (2.52) | 14 (1.58) | 40 (3.19) | 2.05 (1.08, 4.10) | 0.019 | ||
| Total | 698 (1.04) | 285 (0.88) | 413 (1.19) | ||||
(%) indicates the incidence rate calculated using “Total patient population” as the denominator. Bold font indicates statistically significant differences between men and women (p < 0.05). The p-values were calculated using the chi-squared test
CI confidence interval, eGFR estimated glomerular filtration rate, OR odds ratio
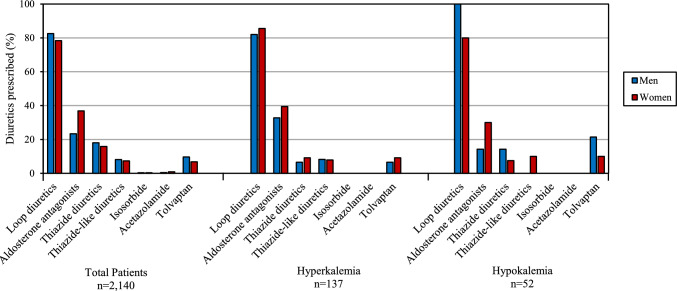
Hyperkalemia and Hypokalemia in Patients Aged ≥ 75 Years with an eGFR of < 30 mL/min/1.73 m2
The association between sex differences in adverse reactions and pharmacological effects was investigated in patients aged ≥ 75 years who had an eGFR < 30 mL/min/1.73 m2. Diuretics prescribed immediately before the onset of electrolyte disturbances were analyzed in 137 patients with hyperkalemia and 52 with hypokalemia (Fig. 4). Two patients with hypokalemia for whom only combination diuretics had been prescribed were excluded. In patients aged ≥ 75 years with an eGFR of < 30 mL/min/1.73 m2, loop diuretics were prescribed to 82.0% of men and in 85.5% of women with hyperkalemia and in 100% of men (all 14 patients) and in 80% of women with hypokalemia. Furthermore, aldosterone antagonists were prescribed for 23.3% of men and for 36.9% of women in the total patient population. However, the rate of prescription of aldosterone antagonists for hyperkalemia was 32.8% for men and 39.5% for women.
Fig. 4.
Percentages of diuretics prescribed by pharmacological class in the total study population and in patients aged ≥ 75 years with an eGFR of < 30 mL/min/1.73 m2 who developed hyperkalemia or hypokalemia by sex. eGFR estimated glomerular filtration rate
Discussion
It is known that there are sex differences in the rates of incidence of adverse reactions to diuretics, but the sex-specific effects of these drugs on patients’ physiological function have not been clarified. This is the first study to identify sex differences in the frequency of diuretic-associated electrolyte disturbances based on age and renal function using Japanese medical claims and health checkup data. The study included 67,135 patients who were taking diuretics and had eGFR data available. The largest proportion of patients prescribed diuretics were aged ≥75 years, followed by patients aged 65–74 years and non-elderly patients (Table 2). This finding probably reflects the fact that cardiac disease and hypertension are common in elderly patients and that use of diuretics is common in this age group. The chi-squared tests showed statistically significant differences in age distribution between men and women in all categories. However, the clinical relevance of this difference may be limited due to the large sample size, which can result in significant p-values even for small absolute differences.
We found that aldosterone antagonists, thiazide diuretics, thiazide-like diuretics, and tolvaptan were prescribed more frequently in men (Fig. 1). According to a 2022 national survey, the percentage of people with systolic (highest) blood pressure of 140 mmHg or higher was 28.9% for men and 21.1% for women [34]. Therefore, it is possible that men are more susceptible to hypertension and therefore may have been using more diuretics. On the other hand, isosorbide, which is primarily used to treat Ménière’s disease, was prescribed more frequently in women. This finding probably reflects the high prevalence of Ménière’s disease among women in Japan [35]. In Japan, isosorbide is primarily prescribed for inner ear disorders such as Ménière’s disease and is classified under “diuretics” according to the Japanese standard commodity classification system. This differs from international classifications, such as in Europe, where isosorbide mononitrate and dinitrate are used as vasodilators for cardiovascular indications.
In our study, more patients were diagnosed with electrolyte disturbances as a result of potassium disturbances than because of sodium disturbances (Table 3). Further studies are needed to determine if there is a difference in the frequency of diagnosis of sodium and potassium disturbances in everyday clinical practice. Hyperosmolality and hypernatremia tended to be more common in men, while hypo-osmolality and hyponatremia tended to be more common in women, although the numbers were small, and these results were not significant. Furthermore, hyperkalemia was more common in men and hypokalemia was more common in women. Another study found that diuretic-induced hyponatremia and hypokalemia were common adverse events leading to hospitalization in women [23]. However, our study is the first to suggest that hyperkalemia may be more common in men.
Electrolyte disturbances are more likely to occur in the elderly (Fig. 2a), probably because physiological functions tend to deteriorate with advancing age. Potassium excretion is decreased in patients with renal disease, and in this study, the eGFR was much lower in patients who developed hyperkalemia than in those who did not independent of sex.
Loop diuretics are inherently likely to cause hypokalemia. However, when the data for patients who developed hyperkalemia and those who developed hypokalemia were compared (Fig. 3), the percentage of loop diuretics prescribed was similar in both groups. Analysis of the number and type of concomitant medications showed that 8717 of the 10,315 patients in this study who were prescribed two or more diuretics were prescribed loop diuretics. We found that loop diuretics were particularly likely to be prescribed with other types of diuretics. Therefore, the proportion of loop diuretics prescribed may have been similar for hyperkalemia and hypokalemia. However, although a loop diuretic may be prescribed to treat hyperkalemia [36], in this study, the first electrolyte disturbance that occurred during the period was analyzed for the drug that had been prescribed immediately prior to occurrence of the disturbance. Therefore, it is unlikely that loop diuretics prescribed for treatment of hyperkalemia are reflected in our results.
We found that hyperkalemia was more common in men than in women (Table 3). However, as shown in Fig. 3, there was no significant sex difference in the percentage of prescriptions. This finding suggests that hyperkalemia in men may be attributable to factors that are independent of diuretic classification. For example, chronic kidney disease is more likely to cause hyperkalemia as a result of reduced renal function, and previous studies have shown that chronic kidney disease is worse in men [37].
The ORs, 95% CIs, and p-values were analyzed for hyperkalemia and hypokalemia by age and eGFR category (Table 4). In general, as renal function declines, patients are more likely to develop hyperkalemia because potassium excretion is reduced as a result of a decreased glomerular filtration rate. Among patients aged ≥75 years, the odds of hypokalemia in women compared to men were significantly higher in the eGFR 60–30 and <30 mL/min/1.73 m2 groups. These findings suggest that particular caution is needed regarding diuretic-associated hypokalemia in elderly women with reduced renal function.
Figure 1 shows that 24,273 (36.2%) of the 67,135 patients in this study were taking loop diuretics, while Fig. 3 shows that approximately 60% of men and women who developed hyperkalemia or hypokalemia had been prescribed these drugs. These results indicate that loop diuretics are prescribed more frequently in patients with hyperkalemia and hypokalemia. Figure 4 shows that the proportion of loop diuretics prescribed increased to about 80% in patients aged ≥ 75 years with an eGFR of < 30 mL/min/1.73 m2. However, when compared with the total patient population, the percentage was similar indicating that the proportion of patients prescribed loop diuretics did not change with development of hyperkalemia or hypokalemia in those aged ≥ 75 years with an eGFR of < 30 mL/min/1.73 m2. Loop diuretics are less likely to cause hyperkalemia because of their mechanism of action, whereas aldosterone antagonists are less likely to cause hypokalemia. Nevertheless, agents with different mechanisms of action were prescribed for each potassium abnormality. This could reflect the fact that elderly patients often take multiple medications concomitantly, some of which may affect potassium balance. Furthermore, electrolyte disturbance is more likely to occur in elderly patients with impaired renal function. In addition, regardless of the type of diuretic, adverse reactions may be more likely to occur because of sex differences in pharmacokinetics. Several studies have reported that the organization and expression of renal transporters differ between male and female rats [38]. These differences, particularly in the regulation of sodium reabsorption along the nephron, may contribute to sex-specific susceptibility to the development of electrolyte disturbances.
This study had some limitations. First, we defined an electrolyte disturbance as an adverse reaction if the patient had taken a diuretic within the 14 days before diagnosis, considering the possibility that the patient took their remaining medication as well as the time needed for the medication to be eliminated from the body. However, this definition may not necessarily apply to all patients. We excluded intravenous diuretics, which are commonly used in hospitalized patients, in an effort to mimic the general population of diuretic users. Therefore, the possibility that information for patients with poor health status was overlooked cannot be excluded. The eGFR is calculated using the serum creatinine level, age, and sex and is defined as a laboratory indicator. The diagnostic criteria for chronic kidney disease include a decrease in eGFR, with diabetes mellitus as a risk factor [39]. Sex differences in the incidence of these diseases may influence the incidence of adverse reactions. In addition, we did not include comorbidities such as diabetes mellitus, heart failure, or chronic kidney disease in our analysis due to the difficulty in establishing a clear temporal relationship between their diagnosis and the occurrence of electrolyte disturbances. These comorbid conditions may independently contribute to the development of electrolyte disturbances regardless of diuretic use. Future research should aim to incorporate comorbidity profiles using data sources that allow for more temporally aligned diagnostic information. Furthermore, patients aged younger than 20 years were excluded because eGFR is a measure of renal function in patients aged older than 20 years. Electrolyte disturbances were identified based on diagnosis codes (ICD-10) in claims data (Table 1). As such, we could not assess the severity of these conditions at the time of diagnosis. This limits the clinical interpretability of our findings, especially in distinguishing between mild and life-threatening cases. Because the health checkup data from which the eGFR values were obtained are generally recorded once a year, it is possible that the most recent electrolyte disturbance was not linked to the eGFR value. It is possible that other concomitant medications besides diuretics may have been involved in renal function and electrolyte regulation. In this study, subgroup analyses, such as those based on specific diuretic classes or patient populations, including methods like propensity score matching, could not be conducted because the dataset included only patients who were prescribed diuretics. No untreated comparison group was available, limiting our ability to adjust for baseline characteristics between groups. Future studies incorporating both treated and untreated populations would enable more robust comparative analyses.
The observed sex differences in adverse event rates may also be partly attributable to the underrepresentation of women in randomized controlled trials, leading to limited generalizability of trial findings to female patients. Addressing this gap in future clinical research is crucial to ensure evidence-based pharmacotherapy across sexes.
In summary, the findings of this study suggest that it is important to be aware of hypokalemia as an adverse reaction when diuretics are used in elderly women with a low eGFR. Regular renal function tests and monitoring for early signs of electrolyte disturbances are necessary in these patients.
Conclusion
In this claims-based study of over 67,000 diuretic users in Japan, sex differences were observed in the incidence of electrolyte disturbances. Hypokalemia was more frequently diagnosed in women, especially among those aged ≥ 75 years. In this age group, the odds of hypokalemia were significantly higher than in men in the eGFR 60–30 and < 30 mL/min/1.73 m2 categories. These findings underscore the need for close monitoring of electrolyte levels in elderly women with reduced renal function. Further research should investigate the role of diuretic combinations and comorbid conditions in contributing to sex-specific differences.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This work was supported by the JST SPRING, Grant Number JPMJSP2123. The Funding source had no role in the study design, in the collection, analysis, or interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Declarations
Funding
This work was supported by Keio University and JST SPRING, Grant Number JPMJSP2123.
Conflicts of Interest
The authors declare no conflicts of interest.
Ethics Approval
The study protocol was approved by the research ethics committee of the Faculty of Pharmacy, Keio University (approval number: 230118-6).
Informed Consent
Informed consent was not required for this study, which analyzed anonymous claims data.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data Material, and Code availability
The dataset analyzed in this study was obtained under license from DeSC Healthcare, Inc. Due to licensing restrictions, these data are not publicly available. Access to the dataset requires a formal purchase agreement with DeSC Healthcare, Inc.Link https://desc-hc.co.jp/. Contact https://desc-hc.co.jp/contact.
Authors’ Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Narumi Maida, Shingo Kondo, and Katsunori Yamaura. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- 1.Vital, Health and Social Statistics Office. 2023 Summary of Vital Statistics (Fixed Number). Ministry of Health, Labour and Welfare. 2024. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei23/. Accessed 1 Oct 2024.
- 2.The Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group. JCS/JHFS 2025 Guideline on Diagnosis and Treatment of Heart Failure. Japanese Circulation Society/Japanese Heart Failure Society. 2025; 10.1253/circj.CJ-25-0002
- 3.Kostis JB, Davis BR, Cutler J, Grimm RH Jr, Berge KG, Cohen JD, et al. Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. JAMA. 1997. 10.1001/jama.1997.03550030052033. [PubMed] [Google Scholar]
- 4.Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008. 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 5.Sciarretta S, Palano F, Tocci G, Baldini R, Volpe M. Antihypertensive treatment and development of heart failure in hypertension: a Bayesian network meta-analysis of studies in patients with hypertension and high cardiovascular risk. Arch Intern Med. 2011. 10.1001/archinternmed.2010.427. [DOI] [PubMed] [Google Scholar]
- 6.Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015. 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019. 10.1038/s41440-019-0284-9. [DOI] [PubMed] [Google Scholar]
- 8.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002; 10.1001/jama.288.23.2981 [DOI] [PubMed]
- 9.Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial Collaborative Research Group. Diuretic versus alpha-blocker as first-step antihypertensive therapy: final results from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension. 2003; 10.1161/01.HYP.0000086521.95630.5A [DOI] [PubMed]
- 10.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021. 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 11.Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018. 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022. 10.1001/jama.2022.11176. [DOI] [PubMed] [Google Scholar]
- 13.Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. Hypokalemia: a clinical update. Endocr Connect. 2018. 10.1530/EC-18-0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Denic A, Glassock RJ, Rule AD. Structural and functional changes with the aging kidney. Adv Chronic Kidney Dis. 2016. 10.1053/j.ackd.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collins AJ, Pitt B, Reaven N, Funk S, McGaughey K, Wilson D, et al. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017. 10.1159/000479802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aldahl M, Jensen AC, Davidsen L, Eriksen MA, Møller Hansen S, Nielsen BJ, et al. Associations of serum potassium levels with mortality in chronic heart failure patients. Eur Heart J. 2017. 10.1093/eurheartj/ehx460. [DOI] [PubMed] [Google Scholar]
- 17.Núñez J, Bayés-Genís A, Zannad F, Rossignol P, Núñez E, Bodí V, et al. Long-term potassium monitoring and dynamics in heart failure and risk of mortality. Circulation. 2018. 10.1161/CIRCULATIONAHA.117.030576. [DOI] [PubMed] [Google Scholar]
- 18.Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009. 10.1053/j.ajkd.2008.12.034. [DOI] [PubMed] [Google Scholar]
- 19.Rademaker M. Do women have more adverse drug reactions? Am J Clin Dermatol. 2001. 10.2165/00128071-200102060-00001. [DOI] [PubMed] [Google Scholar]
- 20.Zopf Y, Rabe C, Neubert A, Gassmann KG, Rascher W, Hahn EG, et al. Women encounter ADRs more often than do men. Eur J Clin Pharmacol. 2008. 10.1007/s00228-008-0494-6. [DOI] [PubMed] [Google Scholar]
- 21.Maida N, Kondo S, Ogawa M, Hayashi N, Iwata H, Kobayashi N, et al. Lack of information on gender differences in the package inserts of prescription drugs in Japan. Drug Discov Ther. 2024. 10.5582/ddt.2023.01093. [DOI] [PubMed] [Google Scholar]
- 22.Hendriksen LC, van der Linden PD, Lagro-Janssen ALM, van den Bemt PMLA, Siiskonen SJ, Teichert M, et al. Sex differences associated with adverse drug reactions resulting in hospital admissions. Biol Sex Differ. 2021. 10.1186/s13293-021-00377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rodenburg EM, Stricker BH, Visser LE. Sex-related differences in hospital admissions attributed to adverse drug reactions in the Netherlands. Br J Clin Pharmacol. 2011. 10.1111/j.1365-2125.2010.03811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hofer-Dueckelmann C, Prinz E, Beindl W, Szymanski J, Fellhofer G, Pichler M, et al. Adverse drug reactions (ADRs) associated with hospital admissions—elderly female patients are at highest risk. Int J Clin Pharmacol Ther. 2011. 10.5414/cp201514. [DOI] [PubMed] [Google Scholar]
- 25.Sharabi Y, Illan R, Kamari Y, Cohen H, Nadler M, Messerli FH, et al. Diuretic induced hyponatraemia in elderly hypertensive women. J Hum Hypertens. 2002. 10.1038/sj.jhh.1001458. [DOI] [PubMed] [Google Scholar]
- 26.Hendriksen LC, van der Linden PD, Herings RMC, Stricker BH, Visser LE. Women on diuretics have a higher risk of hospital admission because of hyponatremia than men. Pharmacoepidemiol Drug Saf. 2023. 10.1002/pds.5592. [DOI] [PubMed] [Google Scholar]
- 27.Hendriksen LC, Mouissie MS, Herings RMC, van der Linden PD, Visser LE. Women have a higher risk of hospital admission associated with hyponatremia than men while using diuretics. Front Pharmacol. 2024. 10.3389/fphar.2024.1409271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schlanger LE, Bailey JL, Sands JM. Electrolytes in the aging. Adv Chronic Kidney Dis. 2010. 10.1053/j.ackd.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000. 10.1056/NEJM200005253422107. [DOI] [PubMed] [Google Scholar]
- 30.Adrogué HJ, Madias NE. Hypernatremia. N Engl J Med. 2000. 10.1056/NEJM200005183422006.10824078 [Google Scholar]
- 31.Palmer BF, Carrero JJ, Clegg DJ, Colbert GB, Emmett M, Fishbane S, et al. Clinical management of Hyperkalemia. Mayo Clin Proc. 2021. 10.1016/j.mayocp.2020.06.014. [DOI] [PubMed] [Google Scholar]
- 32.Gennari FJ. Hypokalemia. N Engl J Med. 1998. 10.1056/NEJM199808133390707. [DOI] [PubMed] [Google Scholar]
- 33.Kowa Company, Ltd. ISOBIDE SYRUP 70% package insert. https://medical.kowa.co.jp/product/item-7.html. Accessed 1 Oct 2024.
- 34.Health Service Bureau, Helth Service Division. 2022 National Health and Nutrition Survey, Ministry of Health, Labour and Welfare. 2024. https://www.mhlw.go.jp/stf/newpage_42694.html. Accessed 1 Oct 2024.
- 35.Shojaku H, Watanabe Y, Yagi T, Takahashi M, Takeda T, Ikezono T, et al. Peripheral Vestibular Disorder Research Committee of Japan. Changes in the characteristics of definite Meniere’s disease over time in Japan: a long-term survey by the Peripheral Vestibular Disorder Research Committee of Japan, formerly the Meniere’s Disease Research Committee of Japan. Acta Otolaryngol. 2009. 10.1080/00016480802112587. [DOI] [PubMed] [Google Scholar]
- 36.Lindner G, Burdmann EA, Clase CM, Hemmelgarn BR, Herzog CA, Małyszko J, et al. Acute hyperkalemia in the emergency department: a summary from a Kidney Disease: improving Global Outcomes conference. Eur J Emerg Med. 2020. 10.1097/MEJ.0000000000000691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eriksen BO, Ingebretsen OC. The progression of chronic kidney disease: a 10-year population-based study of the effects of gender and age. Kidney Int. 2006. 10.1038/sj.ki.5000058. [DOI] [PubMed] [Google Scholar]
- 38.McDonough AA, Harris AN, Xiong LI, Layton AT. Sex differences in renal transporters: assessment and functional consequences. Nat Rev Nephrol. 2024. 10.1038/s41581-023-00757-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol. 2017. 10.2215/CJN.11491116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.