Abstract
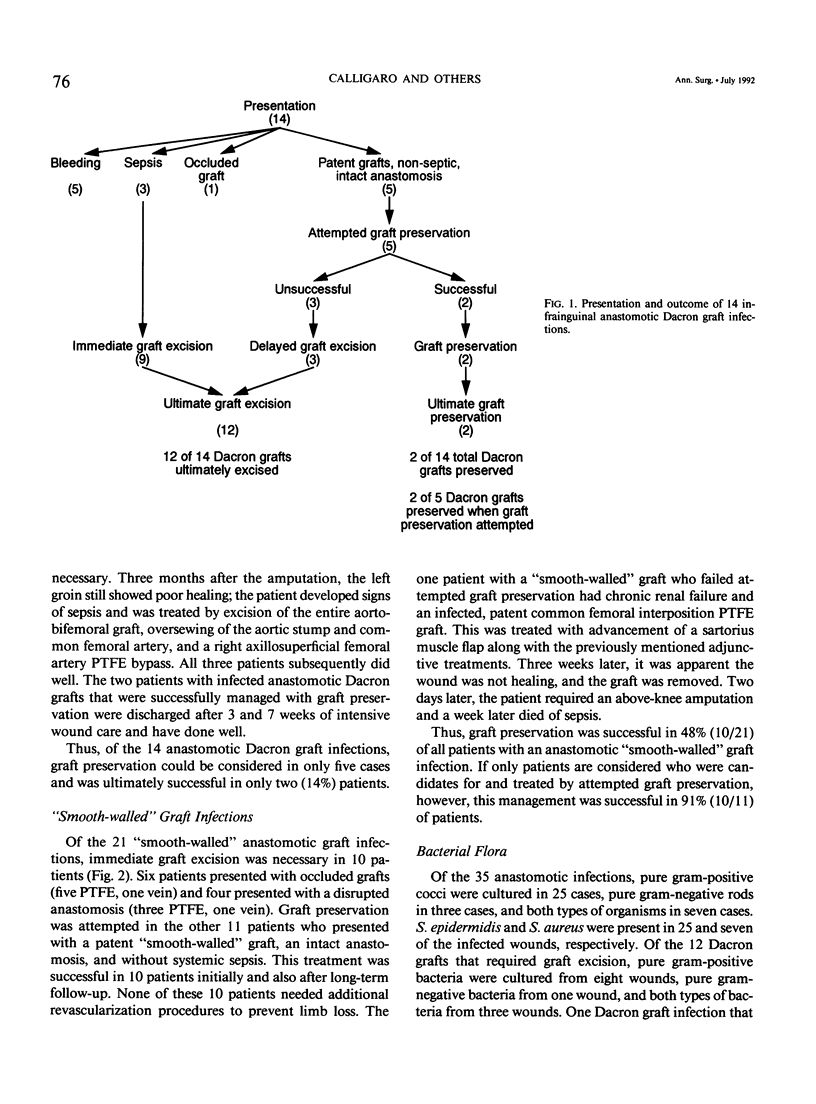
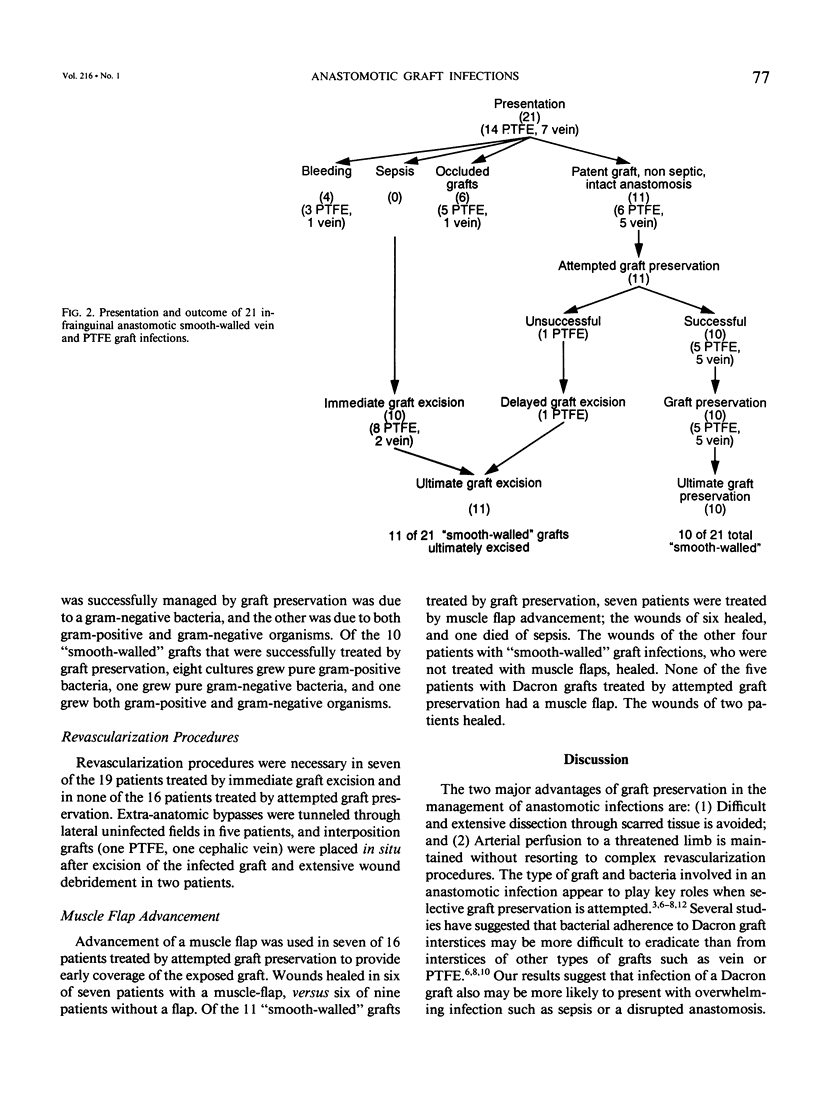
The purpose of this study was to determine whether the type of graft material and bacteria involved in an infrainguinal arterial anastomotic infection can be used as guidelines for graft preservation. Between 1972 and 1990, the authors treated 35 anastomotic infections involving a common femoral or distal artery. The graft material was Dacron in 14 patients, polytetrafluoroethylene (PTFE) in 14, and vein in 7. Of the 14 Dacron grafts, immediate graft excision was required for overwhelming infection in eight patients (bleeding in five, sepsis in three) and for an occluded graft in one patient. Three of five patients failed attempted graft preservation because of nonhealing wounds. Thus, 12 of the 14 Dacron grafts ultimately required graft excision. Of the 21 "smooth-walled" vein and PTFE grafts, 10 required immediate graft excision for occluded grafts (five PTFE, one vein) or bleeding (three PTFE, one vein). Ten of the remaining 11 (91%) patients with patent "smooth-walled" grafts, intact anastomoses, and absence of sepsis managed by graft preservation healed their wounds and maintained distal arterial perfusion. Wound cultures grew pure gram-positive cocci in 17 of 21 "smooth-walled" graft infections versus 8 of 14 Dacron graft infections. In the absence of systemic sepsis, graft preservation is the treatment of choice for gram-positive infections involving an intact anastomosis of patent PTFE and vein grafts. Regardless of the bacterial cause, the authors recommend that any infrainguinal anastomotic infection of a Dacron graft be treated by immediate excision of all infected graft material.
Full text
PDF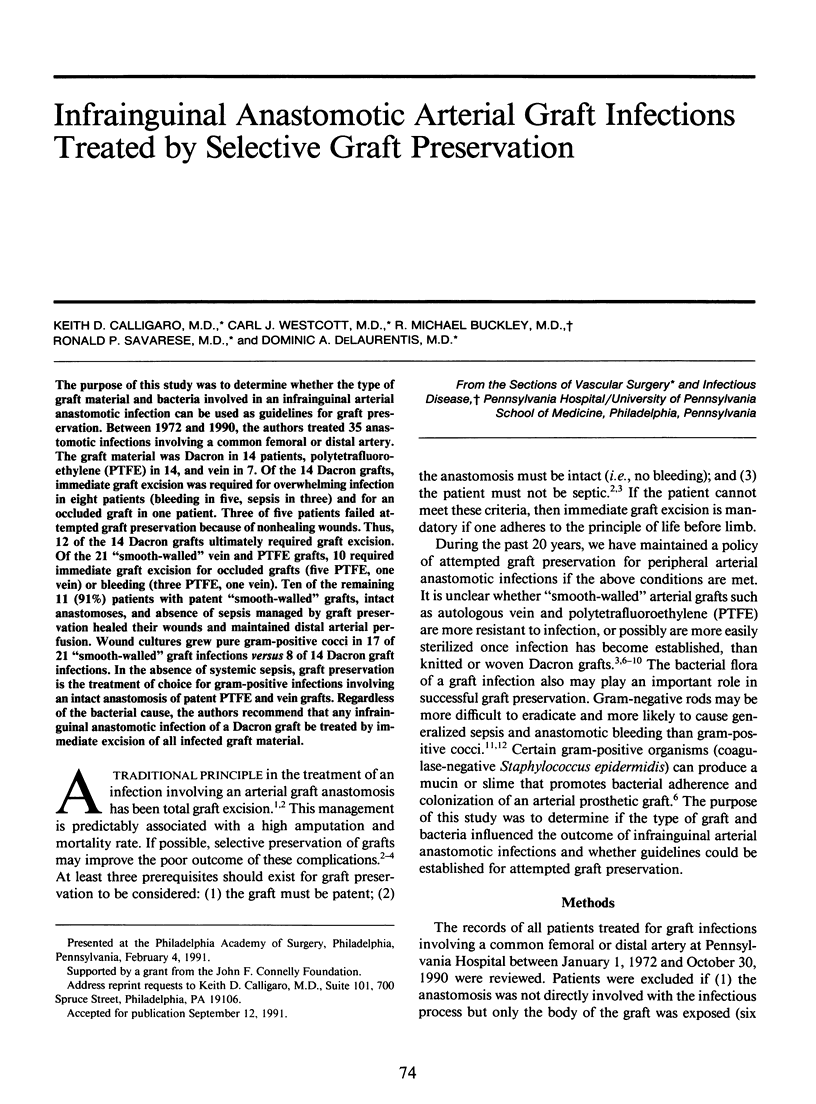


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bunt T. J. Synthetic vascular graft infections. I. Graft infections. Surgery. 1983 Jun;93(6):733–746. [PubMed] [Google Scholar]
- Calligaro K. D., Ascer E., Veith F. J., Gupta S. K., Wengerter K. R., Franco C. D., Bakal C. W., Sprayregen S. Unsuspected inflow disease in candidates for axillofemoral bypass operations: a prospective study. J Vasc Surg. 1990 Jun;11(6):832–837. [PubMed] [Google Scholar]
- Calligaro K. D., Veith F. J. Diagnosis and management of infected prosthetic aortic grafts. Surgery. 1991 Nov;110(5):805–813. [PubMed] [Google Scholar]
- Calligaro K. D., Veith F. J., Gupta S. K., Ascer E., Dietzek A. M., Franco C. D., Wengerter K. R. A modified method for management of prosthetic graft infections involving an anastomosis to the common femoral artery. J Vasc Surg. 1990 Apr;11(4):485–492. [PubMed] [Google Scholar]
- Ehrenfeld W. K., Wilbur B. G., Olcott C. N., Stoney R. J. Autogenous tissue reconstruction in the management of infected prosthetic grafts. Surgery. 1979 Jan;85(1):82–92. [PubMed] [Google Scholar]
- Ghosn P. B., Rabbat A. G., Trudel J. Why remove an infected aortofemoral graft? Can J Surg. 1983 Jul;26(4):330–331. [PubMed] [Google Scholar]
- Jarrett F., Darling R. C., Mundth E. D., Austen W. G. The management of infected arterial aneurysms. J Cardiovasc Surg (Torino) 1977 Jul-Aug;18(4):361–366. [PubMed] [Google Scholar]
- Knott L. H., Crawford F. A., Jr, Grogan J. B. Comparison of autogenous vein, dacron and Gore-Tex in infected wounds. J Surg Res. 1978 Apr;24(4):288–293. doi: 10.1016/0022-4804(78)90094-x. [DOI] [PubMed] [Google Scholar]
- Kwaan J. H., Connolly J. E. Successful management of prosthetic graft infection with continuous povidone-iodine irrigation. Arch Surg. 1981 May;116(5):716–720. doi: 10.1001/archsurg.1981.01380170188033. [DOI] [PubMed] [Google Scholar]
- Malone J. M., Lalka S. G., McIntyre K. E., Bernhard V. M., Pabst T. S. The necessity for long-term antibiotic therapy with positive arterial wall cultures. J Vasc Surg. 1988 Sep;8(3):262–267. [PubMed] [Google Scholar]
- Mixter R. C., Turnipseed W. D., Smith D. J., Jr, Acher C. W., Rao V. K., Dibbell D. G. Rotational muscle flaps: a new technique for covering infected vascular grafts. J Vasc Surg. 1989 Mar;9(3):472–478. doi: 10.1067/mva.1989.vs0090472. [DOI] [PubMed] [Google Scholar]
- Moore W. S., Malone J. M., Keown K. Prosthetic arterial graft material. Influence on neointimal healing and bacteremic infectibility. Arch Surg. 1980 Nov;115(11):1379–1383. doi: 10.1001/archsurg.1980.01380110111017. [DOI] [PubMed] [Google Scholar]
- Ouriel K., Geary K. J., Green R. M., DeWeese J. A. Fate of the exposed saphenous vein graft. Am J Surg. 1990 Aug;160(2):148–150. doi: 10.1016/s0002-9610(05)80295-8. [DOI] [PubMed] [Google Scholar]
- Schmitt D. D., Bandyk D. F., Pequet A. J., Towne J. B. Bacterial adherence to vascular prostheses. A determinant of graft infectivity. J Vasc Surg. 1986 May;3(5):732–740. [PubMed] [Google Scholar]
- Seabrook G. R., Schmitt D. D., Bandyk D. F., Edmiston C. E., Krepel C. J., Towne J. B. Anastomotic femoral pseudoaneurysm: an investigation of occult infection as an etiologic factor. J Vasc Surg. 1990 May;11(5):629–634. doi: 10.1067/mva.1990.19708. [DOI] [PubMed] [Google Scholar]
- Stone K. S., Walshaw R., Sugiyama G. T., Dean R. E., Dunstan R. W. Polytetrafluoroethylene versus autogenous vein grafts for vascular reconstruction in contaminated wounds. Am J Surg. 1984 May;147(5):692–695. doi: 10.1016/0002-9610(84)90144-2. [DOI] [PubMed] [Google Scholar]
- Szilagyi D. E., Smith R. F., Elliott J. P., Vrandecic M. P. Infection in arterial reconstruction with synthetic grafts. Ann Surg. 1972 Sep;176(3):321–333. doi: 10.1097/00000658-197209000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellis V. A., Kohlberg W. I., Bhat D. J., Driscoll B., Veith F. J. Expanded polytetrafluoroethylene graft fistula for chronic hemodialysis. Ann Surg. 1979 Jan;189(1):101–105. doi: 10.1097/00000658-197901000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt P. A., Pairolero P. C., Hollier L. H., Fowl R. J., Cherry K. J., Bernatz P. E. The occluded renal artery: durability of revascularization. J Vasc Surg. 1985 Jan;2(1):125–132. doi: 10.1067/mva.1985.avs0020125. [DOI] [PubMed] [Google Scholar]


