Abstract
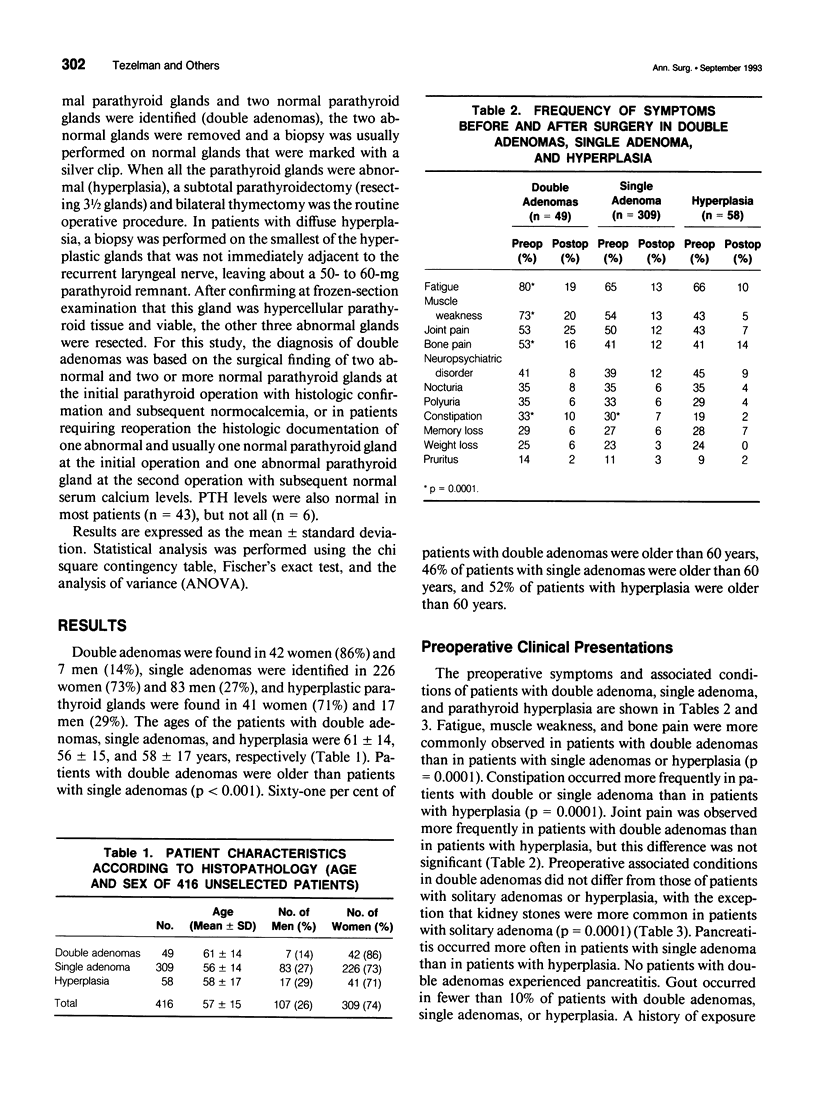
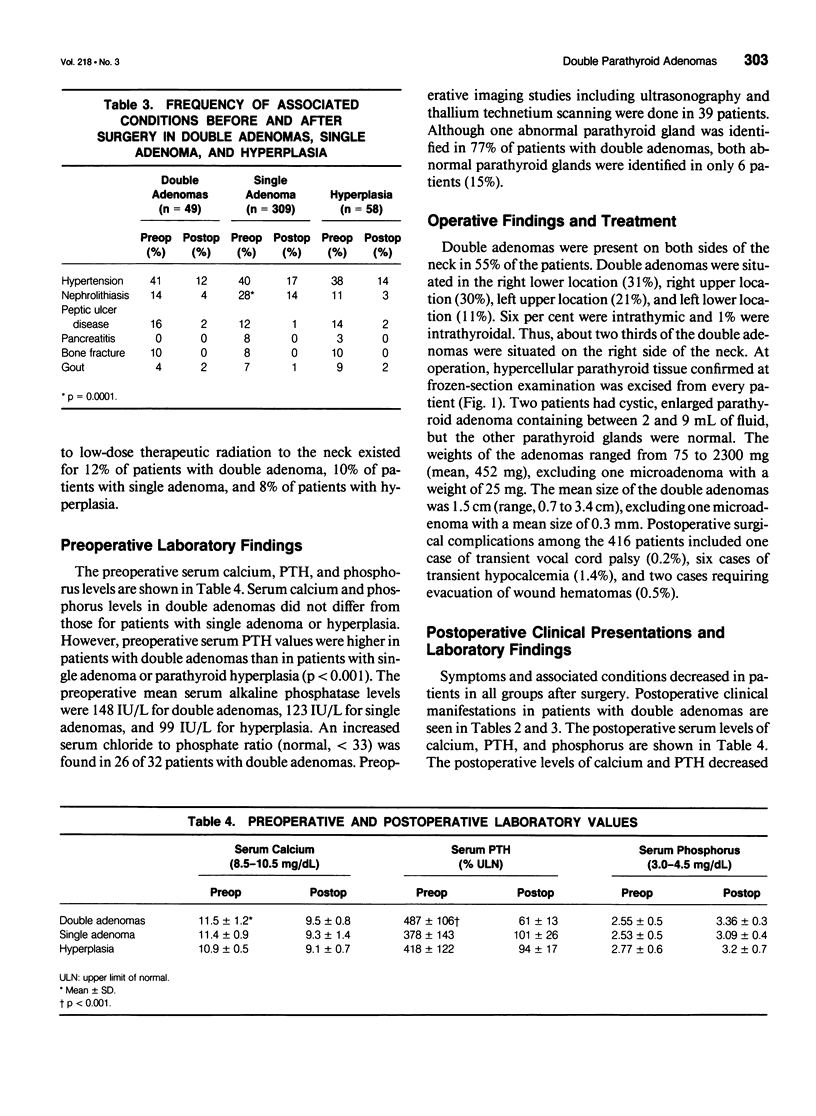
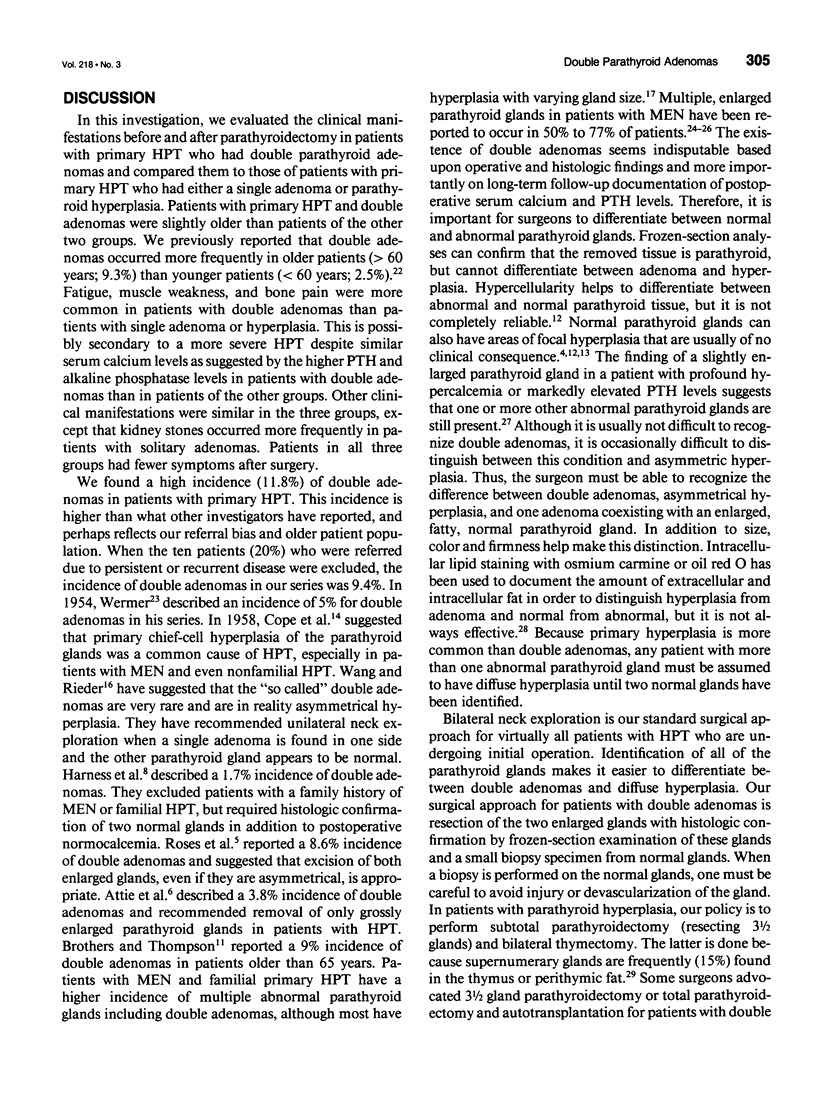
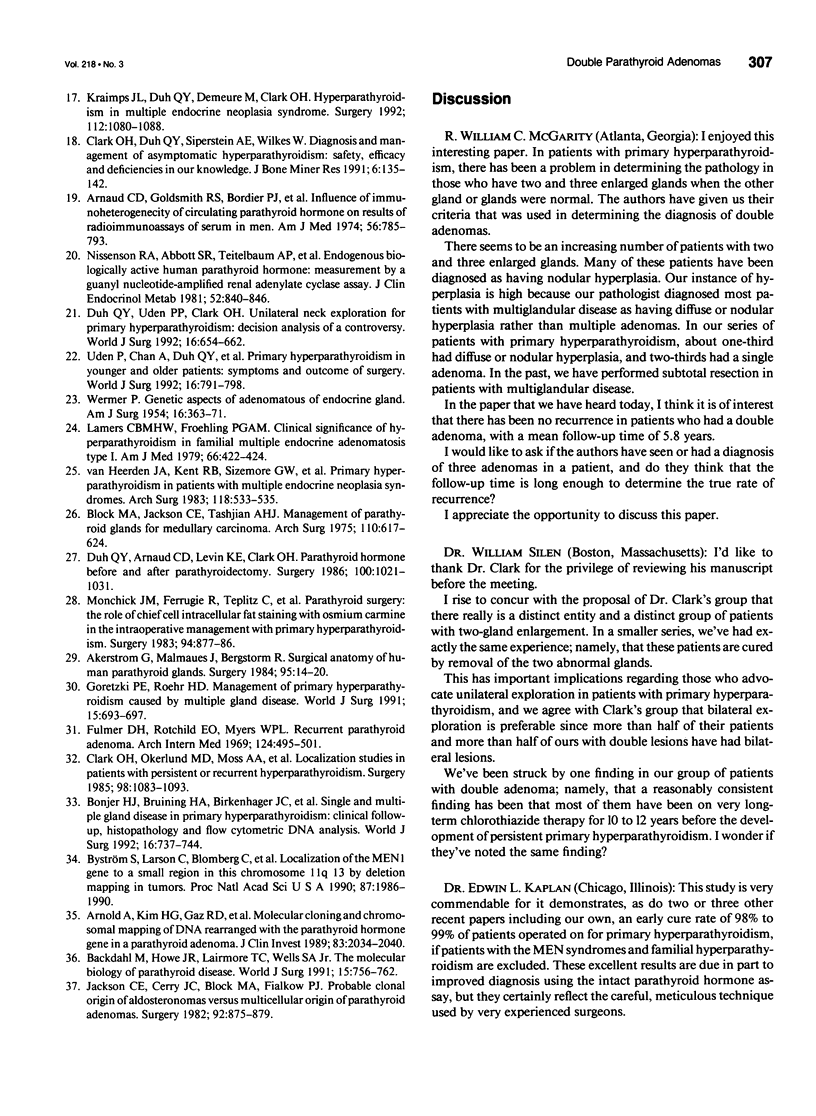
OBJECTIVE: There is considerable debate about whether double parathyroid adenomas are a discrete entity or represent hyperplasia with parathyroid glands of varying sizes. This distinction is important because it impacts on the extent of parathyroid resection and the success of the parathyroid operation. SUMMARY BACKGROUND DATA: Double parathyroid adenomas have been reported to occur in 1.7% to 9% of patients with primary hyperparathyroidism (HPT). It is important for surgeons to differentiate between double adenoma and hyperplasia with glands of varying sizes using gross examination during the initial procedure because microscopic findings of a small biopsy specimen at frozen-section examination may not be diagnostic. METHODS: From 1982 to 1992, 416 unselected patients (309 women and 107 men) with primary HPT without familial HPT or multiple endocrine neoplasia (MEN) were treated by one surgeon at the University of California at San Francisco. Double adenoma occurred in 49 patients, solitary adenoma in 309 patients, and hyperplasia in 58 patients. The authors analyzed the clinical manifestations, the preoperative and postoperative serum levels of calcium, phosphate, and parathyroid hormone (PTH), and the success rate and outcome after parathyroidectomy and compared their results in 49 patients with double adenomas to the results for patients with solitary adenomas or hyperplasia. RESULTS: Ten of the patients with double adenomas (20.4%) were referred for persistent HPT after removal of one abnormal parathyroid gland. The ages of the patients with double adenoma, single adenoma, and hyperplasia were 61 +/- 14, 56 +/- 15, and 58 +/- 7 years, respectively. Fatigue, muscle weakness, and bone pain were common in patients with double adenomas, whereas nephrolithiasis occurred more frequently in patients with solitary adenoma (p = 0.0001). Serum calcium and PTH levels (per cent of upper limit of normal) fell from 11.5 +/- 1.2 mg/dL and 487% to 9.5 +/- 0.8 mg/dL and 61% for patients with double adenomas; from 11.9 +/- 0.9 mg/dL and 378% to 9.3 +/- 1.4 mg/dL and 101% for patients with single adenoma; and from 10.9 +/- 0.5 mg/dL and 418% to 9.1 +/- 0.7 mg/dL and 94% for patients with hyperplasia, respectively. There was no recurrence in the patients with double adenomas with a mean follow-up time of 5.8 years. CONCLUSIONS: Double adenomas are a discrete entity and occur more often in older patients. Patients with double adenomas can be successfully treated by removal of the two abnormal glands.
Full text
PDF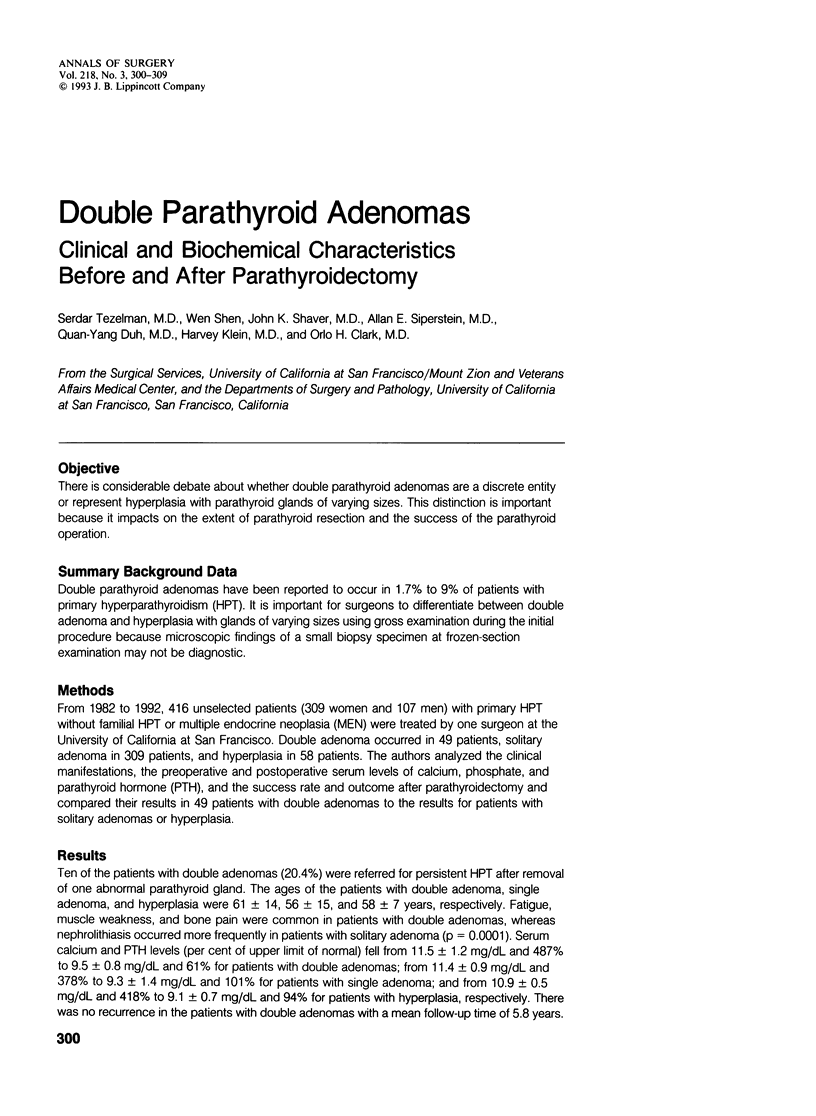


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akerström G., Malmaeus J., Bergström R. Surgical anatomy of human parathyroid glands. Surgery. 1984 Jan;95(1):14–21. [PubMed] [Google Scholar]
- Arnaud C. D., Goldsmith R. S., Bordier P. J., Sizemore G. W. Influence of immunoheterogeneity of circulating parathyroid hormone on results of radioimmunoassays of serum in man. Am J Med. 1974 Jun;56(6):785–793. doi: 10.1016/0002-9343(74)90806-7. [DOI] [PubMed] [Google Scholar]
- Arnold A., Kim H. G., Gaz R. D., Eddy R. L., Fukushima Y., Byers M. G., Shows T. B., Kronenberg H. M. Molecular cloning and chromosomal mapping of DNA rearranged with the parathyroid hormone gene in a parathyroid adenoma. J Clin Invest. 1989 Jun;83(6):2034–2040. doi: 10.1172/JCI114114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attie J. N., Bock G., Auguste L. J. Multiple parathyroid adenomas: report of thirty-three cases. Surgery. 1990 Dec;108(6):1014–1020. [PubMed] [Google Scholar]
- Backdahl M., Howe J. R., Lairmore T. C., Wells S. A., Jr The molecular biology of parathyroid disease. World J Surg. 1991 Nov-Dec;15(6):756–762. doi: 10.1007/BF01665311. [DOI] [PubMed] [Google Scholar]
- Black W. C., 3rd, Utley J. R. The differential diagnosis of parathyroid adenoma and chief cell hyperplasia. Am J Clin Pathol. 1968 Jun;49(6):761–775. doi: 10.1093/ajcp/49.6.761. [DOI] [PubMed] [Google Scholar]
- Block M. A., Frame B., Jackson C. E. The efficacy of subtotal parathyroidectomy for primary hyperparathyroidism due to multiple gland involvement. Surg Gynecol Obstet. 1978 Jul;147(1):1–5. [PubMed] [Google Scholar]
- Block M. A., Jackson C. E., Tashjian A. H., Jr Management of parathyroid glands in surgery for medullary thyroid carcinoma. Arch Surg. 1975 May;110(5):617–624. doi: 10.1001/archsurg.1975.01360110163027. [DOI] [PubMed] [Google Scholar]
- Bonjer H. J., Bruining H. A., Birkenhager J. C., Nishiyama R. H., Jones M. A., Bagwell C. B. Single and multigland disease in primary hyperparathyroidism: clinical follow-up, histopathology, and flow cytometric DNA analysis. World J Surg. 1992 Jul-Aug;16(4):737–744. doi: 10.1007/BF02067373. [DOI] [PubMed] [Google Scholar]
- Brothers T. E., Thompson N. W. Surgical treatment of primary hyperparathyroidism in elderly patients. Acta Chir Scand. 1987 Mar;153(3):175–178. [PubMed] [Google Scholar]
- COPE O., KEYNES W. M., ROTH S. I., CASTLEMAN B. Primary chief-cell hyperplasia of the parathyroid glands: a new entity in the surgery of hyperparathyroidism. Ann Surg. 1958 Sep;148(3):375–388. doi: 10.1097/00000658-195809000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark O. H., Okerlund M. D., Moss A. A., Stark D., Norman D., Newton T. H., Duh Q. Y., Arnaud C. D., Harris S., Gooding G. A. Localization studies in patients with persistent or recurrent hyperparathyroidism. Surgery. 1985 Dec;98(6):1083–1094. [PubMed] [Google Scholar]
- Clark O. H., Way L. W., Hunt T. K. Recurrent hyperparathyroidism. Ann Surg. 1976 Oct;184(4):391–402. doi: 10.1097/00000658-197610000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey R. J., Lee T. C., Canary J. J. The surgical treatment of primary hyperparathyroidism: a 20 year experience. Ann Surg. 1977 May;185(5):518–523. doi: 10.1097/00000658-197705000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duh Q. Y., Arnaud C. D., Levin K. E., Clark O. H. Parathyroid hormone: before and after parathyroidectomy. Surgery. 1986 Dec;100(6):1021–1031. [PubMed] [Google Scholar]
- Duh Q. Y., Udén P., Clark O. H. Unilateral neck exploration for primary hyperparathyroidism: analysis of a controversy using a mathematical model. World J Surg. 1992 Jul-Aug;16(4):654–662. doi: 10.1007/BF02067347. [DOI] [PubMed] [Google Scholar]
- Fulmer D. H., Rothschild E. O., Myers W. P. Recurrent parathyroid adenoma. Arch Intern Med. 1969 Oct;124(4):495–501. [PubMed] [Google Scholar]
- Goretzki P. E., Dotzenrath C., Roeher H. D. Management of primary hyperparathyroidism caused by multiple gland disease. World J Surg. 1991 Nov-Dec;15(6):693–697. doi: 10.1007/BF01665302. [DOI] [PubMed] [Google Scholar]
- Harness J. K., Ramsburg S. R., Nishiyama R. H., Thompson N. W. Multiple adenomas of the parathyroids: do they exist? Arch Surg. 1979 Apr;114(4):468–474. doi: 10.1001/archsurg.1979.01370280122018. [DOI] [PubMed] [Google Scholar]
- Harrison T. S., Duarte B., Reitz R. E., Princenthal R., Seaton J. F., Badder E. M., Graham W. P., 3rd Primary hyperparathyroidism: four- to eight-year postoperative follow-up demonstrating persistent functional insignificance of microscopic parathyroid hyperplasia and decreased autonomy of parathyroid hormone release. Ann Surg. 1981 Oct;194(4):429–437. doi: 10.1097/00000658-198110000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines J. R., Atiyah R., Kliefoth J., Beal J. M. Hyperparathyroidism: problems in surgical management. Am J Surg. 1982 Nov;144(5):504–510. doi: 10.1016/0002-9610(82)90568-2. [DOI] [PubMed] [Google Scholar]
- Jackson C. E., Cerny J. C., Block M. A., Fialkow P. J. Probable clonal origin of aldosteronomas versus multicellular origin of parathyroid "adenomas". Surgery. 1982 Nov;92(5):875–879. [PubMed] [Google Scholar]
- Kraimps J. L., Duh Q. Y., Demeure M., Clark O. H. Hyperparathyroidism in multiple endocrine neoplasia syndrome. Surgery. 1992 Dec;112(6):1080–1088. [PubMed] [Google Scholar]
- Lamers C. B., Froeling P. G. Clinical significance of hyperparathyroidism in familial multiple endocrine adenomatosis type I (MEA I). Am J Med. 1979 Mar;66(3):422–424. doi: 10.1016/0002-9343(79)91062-3. [DOI] [PubMed] [Google Scholar]
- Monchik J. M., Farrugia R., Teplitz C., Teplitz J., Brown S. Parathyroid surgery: the role of chief cell intracellular fat staining with osmium carmine in the intraoperative management of patients with primary hyperparathyroidism. Surgery. 1983 Dec;94(6):877–886. [PubMed] [Google Scholar]
- Nissenson R. A., Abbott S. R., Teitelbaum A. P., Clark O. H., Arnaud C. D. Endogenous biologically active human parathyroid hormone: measurement by a guanyl nucleotide-amplified renal adenylate cyclase assay. J Clin Endocrinol Metab. 1981 May;52(5):840–846. doi: 10.1210/jcem-52-5-840. [DOI] [PubMed] [Google Scholar]
- Paloyan E., Lawrence A. M., Oslapas R., Shah K. H., Ernst K., Hofmann C. Subtotal parathyroidectomy for primary hyperparathyroidism. Long-term results in 292 patients. Arch Surg. 1983 Apr;118(4):425–431. doi: 10.1001/archsurg.1983.01390040037008. [DOI] [PubMed] [Google Scholar]
- Proye C. A., Carnaille B., Bizard J. P., Quievreux J. L., Lecomte-Houcke M. Multiglandular disease in seemingly sporadic primary hyperparathyroidism revisited: where are we in the early 1990s? A plea against unilateral parathyroid exploration. Surgery. 1992 Dec;112(6):1118–1122. [PubMed] [Google Scholar]
- Roses D. F., Karp N. S., Sudarsky L. A., Valensi Q. J., Rosen R. J., Blum M. Primary hyperparathyroidism associated with two enlarged parathyroid glands. Arch Surg. 1989 Nov;124(11):1261–1265. doi: 10.1001/archsurg.1989.01410110015002. [DOI] [PubMed] [Google Scholar]
- Udén P., Chan A., Duh Q. Y., Siperstein A., Clark O. H. Primary hyperparathyroidism in younger and older patients: symptoms and outcome of surgery. World J Surg. 1992 Jul-Aug;16(4):791–798. doi: 10.1007/BF02067389. [DOI] [PubMed] [Google Scholar]
- WERMER P. Genetic aspects of adenomatosis of endocrine glands. Am J Med. 1954 Mar;16(3):363–371. doi: 10.1016/0002-9343(54)90353-8. [DOI] [PubMed] [Google Scholar]
- Wang C. A., Rieder S. V. A density test for the intraoperative differentiation of parathyroid hyperplasia from neoplasia. Ann Surg. 1978 Jan;187(1):63–67. doi: 10.1097/00000658-197801000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Heerden J. A., Grant C. S. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg. 1991 Nov-Dec;15(6):688–692. doi: 10.1007/BF01665301. [DOI] [PubMed] [Google Scholar]
- van Heerden J. A., Kent R. B., 3rd, Sizemore G. W., Grant C. S., ReMine W. H. Primary hyperparathyroidism in patients with multiple endocrine neoplasia syndromes. Surgical experience. Arch Surg. 1983 May;118(5):533–536. doi: 10.1001/archsurg.1983.01390050017003. [DOI] [PubMed] [Google Scholar]