Abstract
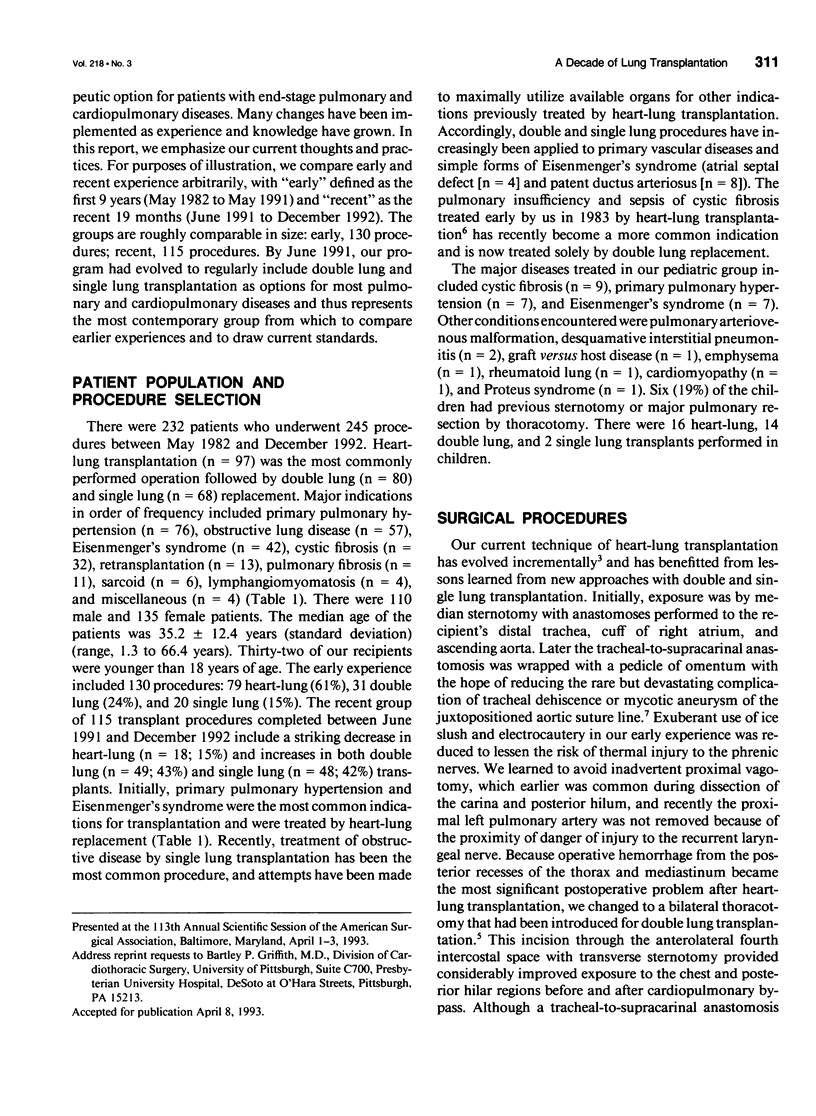
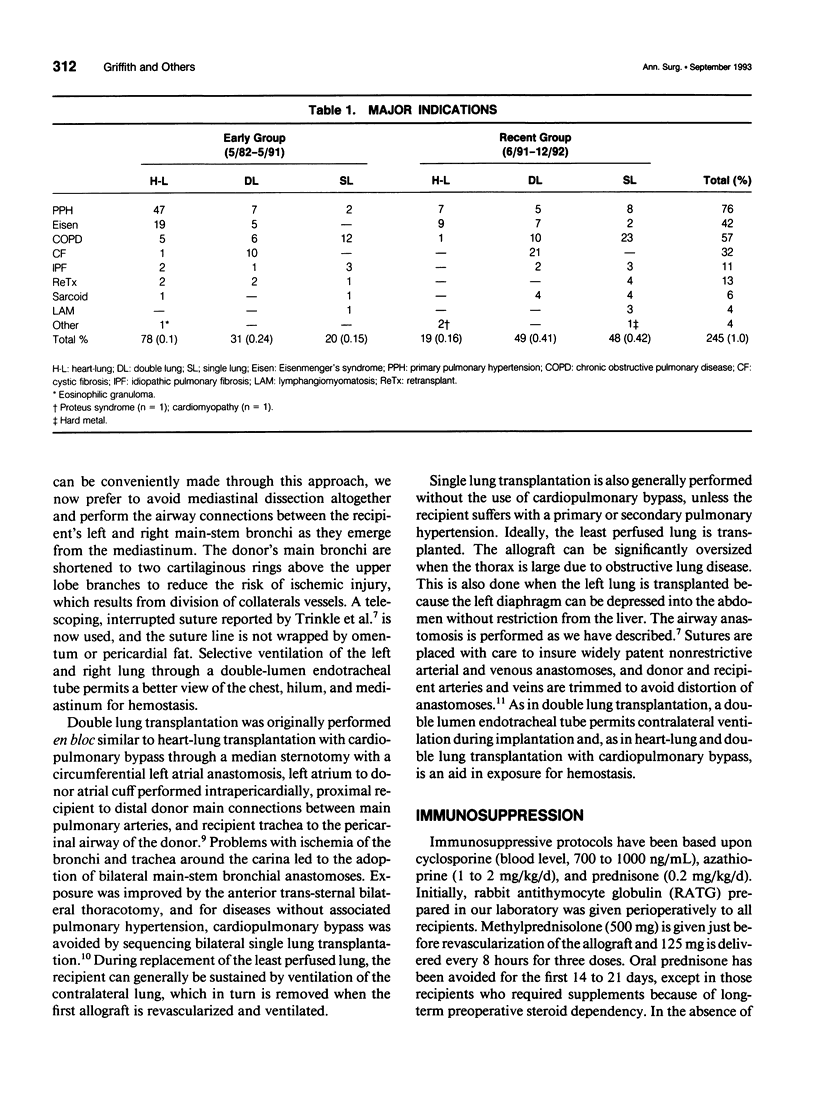
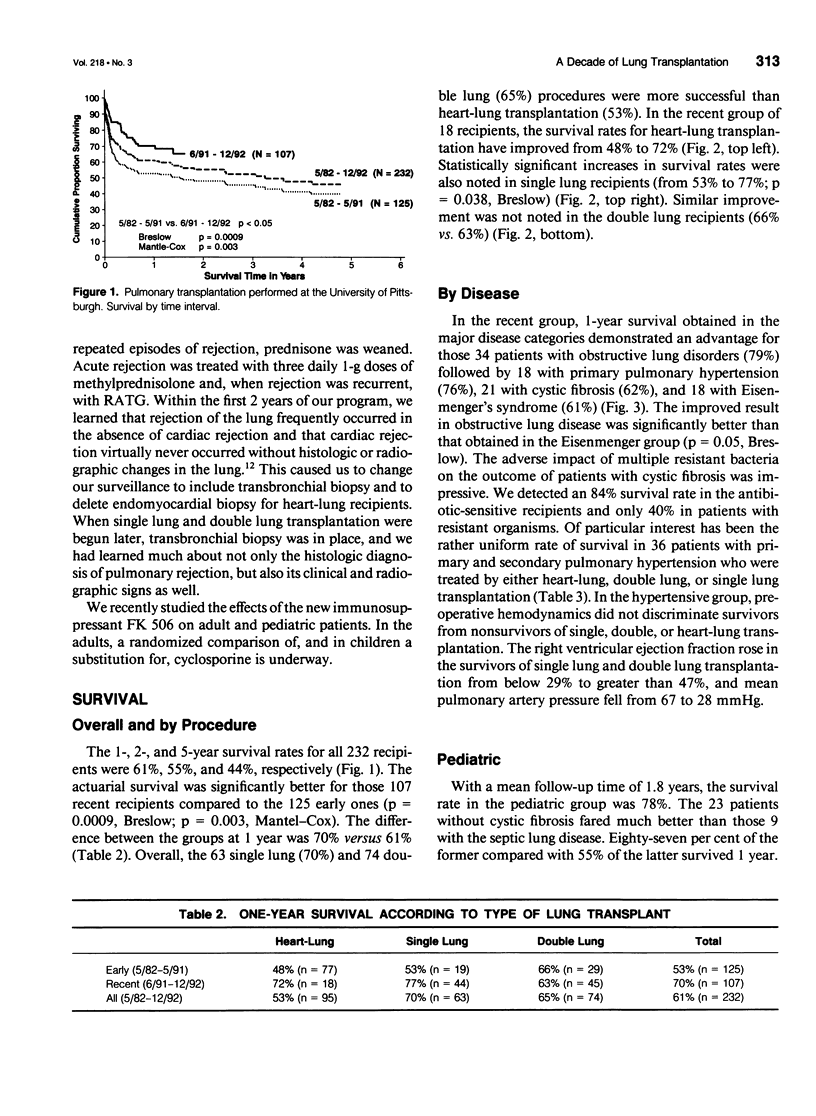
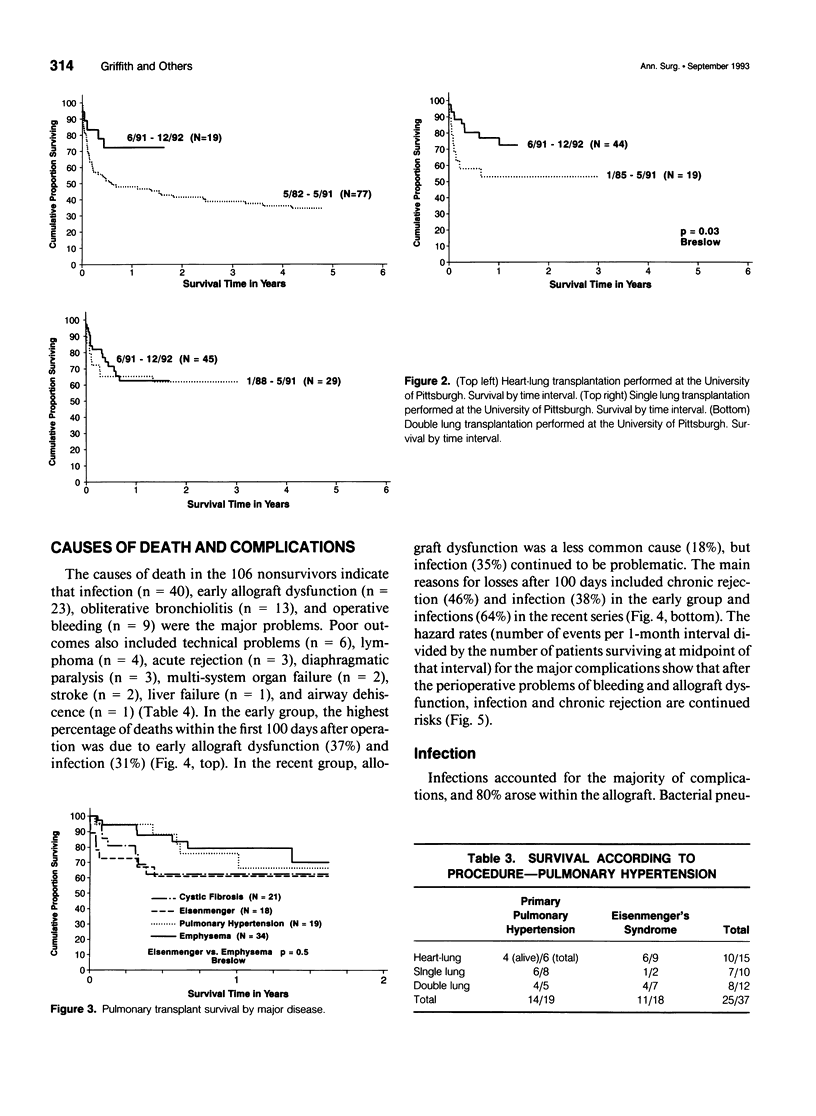
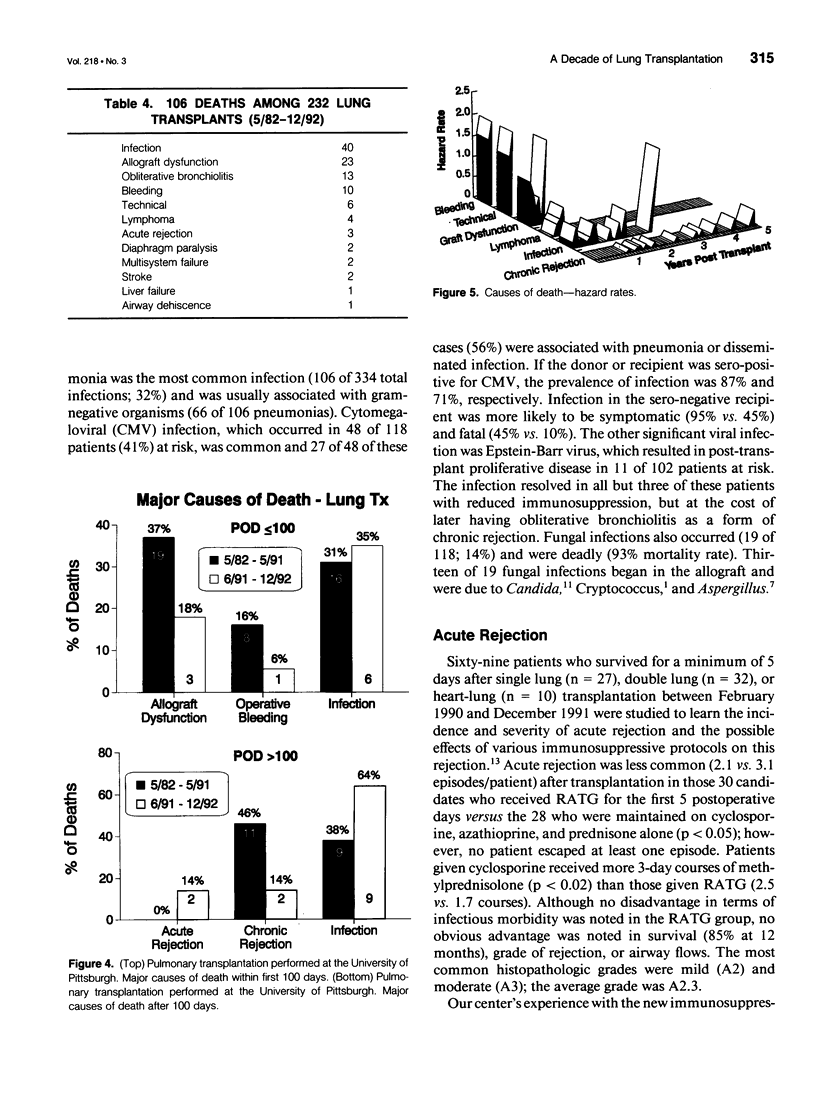
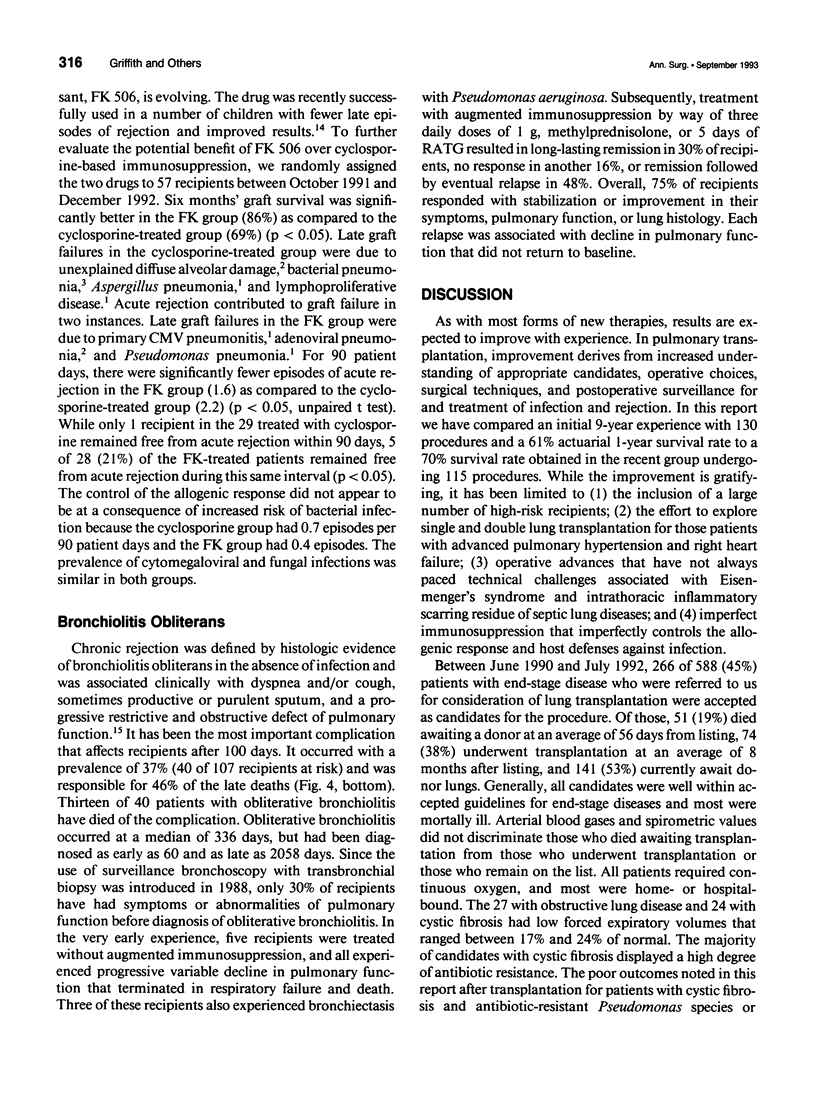
OBJECTIVE: The experience accrued at the University of Pittsburgh between March 1982 and December 1992 in the various forms of lung transplantation, including heart-lung, double lung, and single lung, is discussed. SUMMARY BACKGROUND DATA: Heart-lung (n = 97) was the most commonly performed operation followed by double lung (n = 80) and single lung (n = 68). Major indications included primary pulmonary hypertension (n = 76), obstructive lung disease (n = 57), Eisenmenger's syndrome (n = 42), cystic fibrosis (n = 32), and retransplantation (n = 13). Since May 1991, 115 procedures have been performed and heart-lung transplantation has decreased from 61% to 15% of the cases with a corresponding doubling in double lung from 24% to 43% and single lung from 15% to 42%. RESULTS: The 1-, 2-, and 5-year survival rates in all 232 recipients were 61%, 55%, and 44%, respectively. The actuarial survival rate was significantly better for those 107 recent recipients compared to the 125 early recipients (70% vs. 61%). Overall, the 63 single (70%) and 74 double (65%) lung procedures were more successful than heart-lung transplantation (53%). Recently, however, lung transplantation has been associated with an improvement in the survival rate from 48% to 72%. The survival rate has also improved from 53% to 77% for single lung transplant recipients. The causes of death in 106 recipients included infection (n = 40), early allograft dysfunction (n = 23), obliterative bronchiolitis (n = 13), and inoperative bleeding (n = 10). Poor outcomes also included technical problems (n = 6), lymphoma (n = 4), acute rejection (n = 3), diaphragmatic paralysis (n = 2), multisystem organ failure (n = 2), stroke (n = 2), liver failure (n = 1), and airway dehiscence (n = 1). CONCLUSIONS: The long-term outlook for lung transplant recipients has improved. There appears to be significant conservation of organs with single lung and double lung transplantation, finding greater acceptance for diseases once exclusively treated by heart-lung transplantation alone. The improved long-term outlook will be dependent upon better treatment for chronic rejection of the airways that histologically is defined by obliterative bronchiolitis.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armitage J. M., Fricker F. J., Kurland G., Hardesty R. L., Michaels M., Morita S., Starzl T. E., Yousem S. A., Jaffe R., Griffith B. P. Pediatric lung transplantation. The years 1985 to 1992 and the clinical trial of FK 506. J Thorac Cardiovasc Surg. 1993 Feb;105(2):337–346. [PMC free article] [PubMed] [Google Scholar]
- Bahnson H. T., Starzl T. E., Hakala T. R., Hardesty R. L., Griffith B. P., Iwatsuki S. Development and organization of a multiple organ transplantation program. Ann Surg. 1986 Jun;203(6):620–625. doi: 10.1097/00000658-198606000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calhoon J. H., Grover F. L., Gibbons W. J., Bryan C. L., Levine S. M., Bailey S. R., Nichols L., Lum C., Trinkle J. K. Single lung transplantation. Alternative indications and technique. J Thorac Cardiovasc Surg. 1991 May;101(5):816–825. [PubMed] [Google Scholar]
- Cooper J. D., Patterson G. A., Grossman R., Maurer J. Double-lung transplant for advanced chronic obstructive lung disease. Am Rev Respir Dis. 1989 Feb;139(2):303–307. doi: 10.1164/ajrccm/139.2.303. [DOI] [PubMed] [Google Scholar]
- Dowling R. D., Baladi N., Zenati M., Dummer J. S., Kormos R. L., Armitage J. M., Yousem S. A., Hardesty R. L., Griffith B. P. Disruption of the aortic anastomosis after heart-lung transplantation. Ann Thorac Surg. 1990 Jan;49(1):118–122. doi: 10.1016/0003-4975(90)90368-g. [DOI] [PubMed] [Google Scholar]
- Griffith B. P., Hardesty R. L., Armitage J. M., Kormos R. L., Marrone G. C., Duncan S., Paradis I., Dauber J. H., Yousem S. A., Williams P. Acute rejection of lung allografts with various immunosuppressive protocols. Ann Thorac Surg. 1992 Nov;54(5):846–851. doi: 10.1016/0003-4975(92)90635-h. [DOI] [PubMed] [Google Scholar]
- Griffith B. P., Hardesty R. L., Trento A., Bahnson H. T. Asynchronous rejection of heart and lungs following cardiopulmonary transplantation. Ann Thorac Surg. 1985 Nov;40(5):488–493. doi: 10.1016/s0003-4975(10)60105-1. [DOI] [PubMed] [Google Scholar]
- Griffith B. P., Hardesty R. L., Trento A., Paradis I. L., Duquesnoy R. J., Zeevi A., Dauber J. H., Dummer J. S., Thompson M. E., Gryzan S. Heart-lung transplantation: lessons learned and future hopes. Ann Thorac Surg. 1987 Jan;43(1):6–16. doi: 10.1016/s0003-4975(10)60157-9. [DOI] [PubMed] [Google Scholar]
- Griffith B. P., Paradis I. L., Zeevi A., Rabinowich H., Yousem S. A., Duquesnoy R. J., Dauber J. H., Hardesty R. L. Immunologically mediated disease of the airways after pulmonary transplantation. Ann Surg. 1988 Sep;208(3):371–378. doi: 10.1097/00000658-198809000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novick R. J., Kaye M. P., Patterson G. A., Andréassian B., Klepetko W., Menkis A. H., McKenzie F. N. Redo lung transplantation: a North American-European experience. J Heart Lung Transplant. 1993 Jan-Feb;12(1 Pt 1):5–16. [PubMed] [Google Scholar]
- Patterson G. A., Cooper J. D., Goldman B., Weisel R. D., Pearson F. G., Waters P. F., Todd T. R., Scully H., Goldberg M., Ginsberg R. J. Technique of successful clinical double-lung transplantation. Ann Thorac Surg. 1988 Jun;45(6):626–633. doi: 10.1016/s0003-4975(10)64763-7. [DOI] [PubMed] [Google Scholar]
- Reitz B. A., Wallwork J. L., Hunt S. A., Pennock J. L., Billingham M. E., Oyer P. E., Stinson E. B., Shumway N. E. Heart-lung transplantation: successful therapy for patients with pulmonary vascular disease. N Engl J Med. 1982 Mar 11;306(10):557–564. doi: 10.1056/NEJM198203113061001. [DOI] [PubMed] [Google Scholar]
- Unilateral lung transplantation for pulmonary fibrosis. Toronto Lung Transplant Group. N Engl J Med. 1986 May 1;314(18):1140–1145. doi: 10.1056/NEJM198605013141802. [DOI] [PubMed] [Google Scholar]


