Abstract
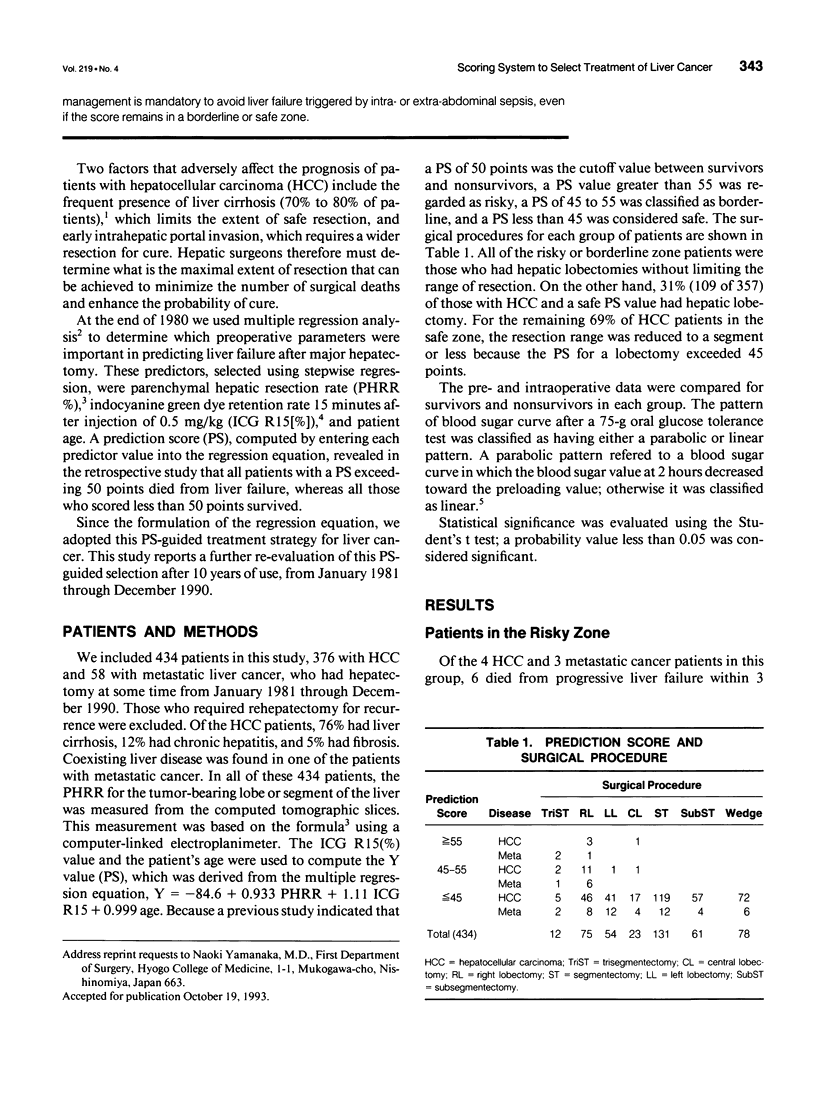
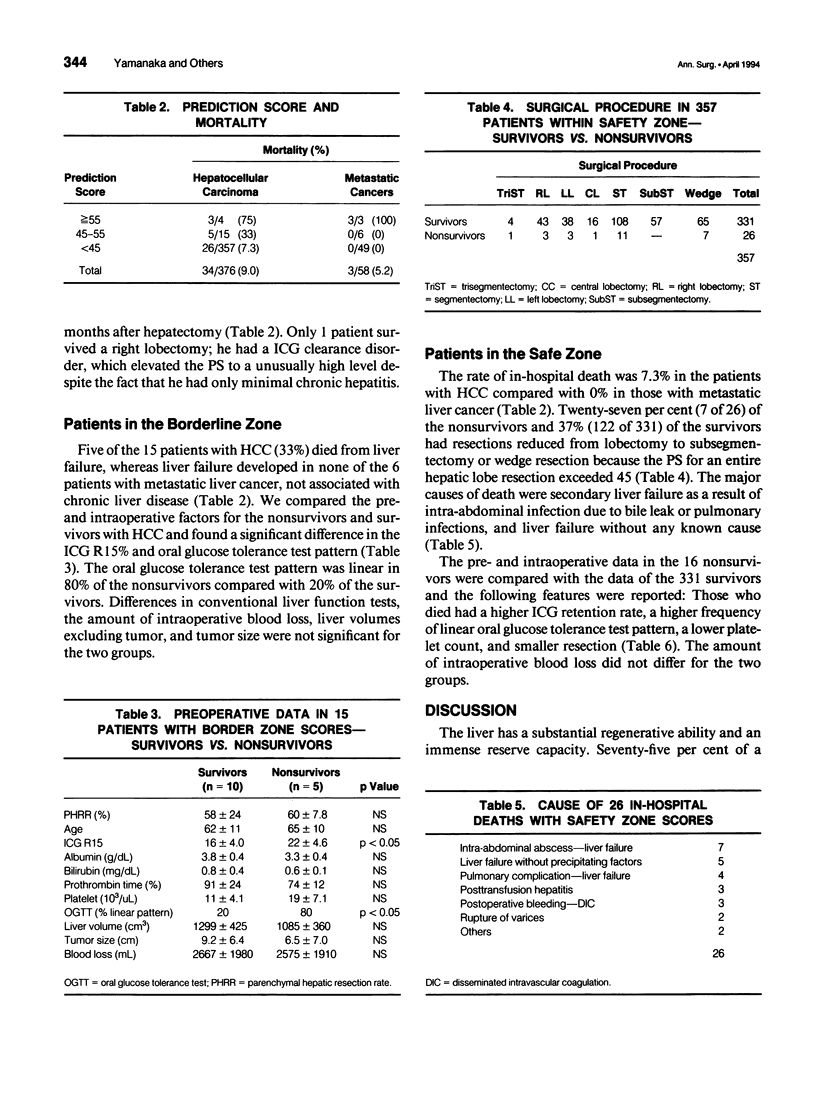
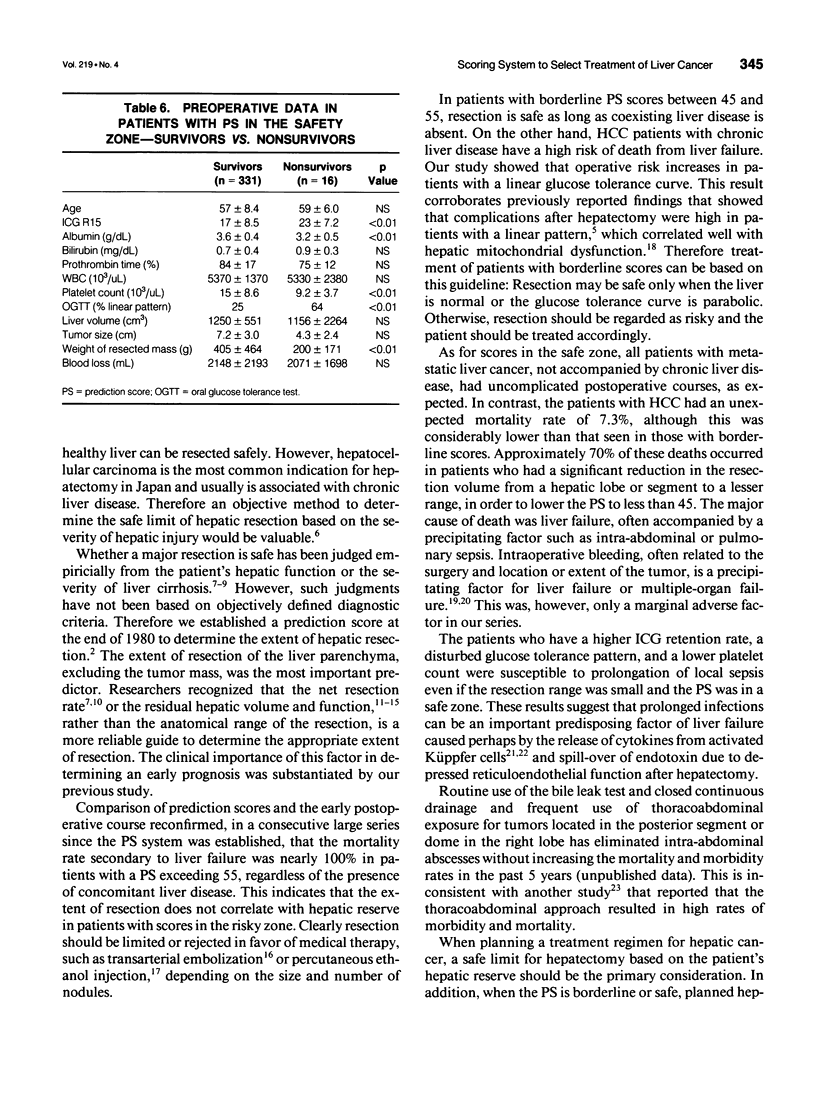
OBJECTIVE: This study reports further refinement of a prediction scoring system, which was established in 1980 as a guide to determine a safe limit for hepatectomy, based on 10 years of use. SUMMARY BACKGROUND DATA: In the past, whether major resection was safe was judged empirically from the net resection volume or the residual hepatic volume combined with the patient's liver function. However, such judgment was not based on objectively defined criteria. METHODS: Patients with hepatocellular carcinoma (HCC; n = 376) and metastatic cancer (n = 58) who had hepatectomy at some time from 1981 through 1990 were entered into this study. A prediction score (PS) was computed using a multiple regression equation that consists of computed tomographic scan-estimated resection rate, indocyanine green retention rate, and the patient's age. A PS greater than 55 was classified as a risky zone, a PS of 45 to 55 was considered borderline and a PS less than 45 was a safe zone. RESULTS: With HCC and chronic liver disease, all patients in the risky zone died, whereas 33% in the borderline zone died and 7.3% died who were in the safe zone. With metastatic cancer with normal liver, all patients in the risky zone died, whereas no patient in either the borderline or safe zones died. The major cause of death in the risky zone was liver failure due to excessive resection. In the borderline and safe zones, liver failure developed primarily after abdominal sepsis or pulmonary infection, particularly for those with adverse prognostic factors such as disturbed glucose tolerance, lower platelet count, and higher indocyanine green retention rate. CONCLUSION: Prediction scores can eliminate deaths related to excessive resection for patients with normal or injured livers. When patients have adverse prognostic factors, careful surgery and postoperative management is mandatory to avoid liver failure triggered by intra- or extra-abdominal sepsis, even if the score remains in a borderline or safe zone.
Full text
PDF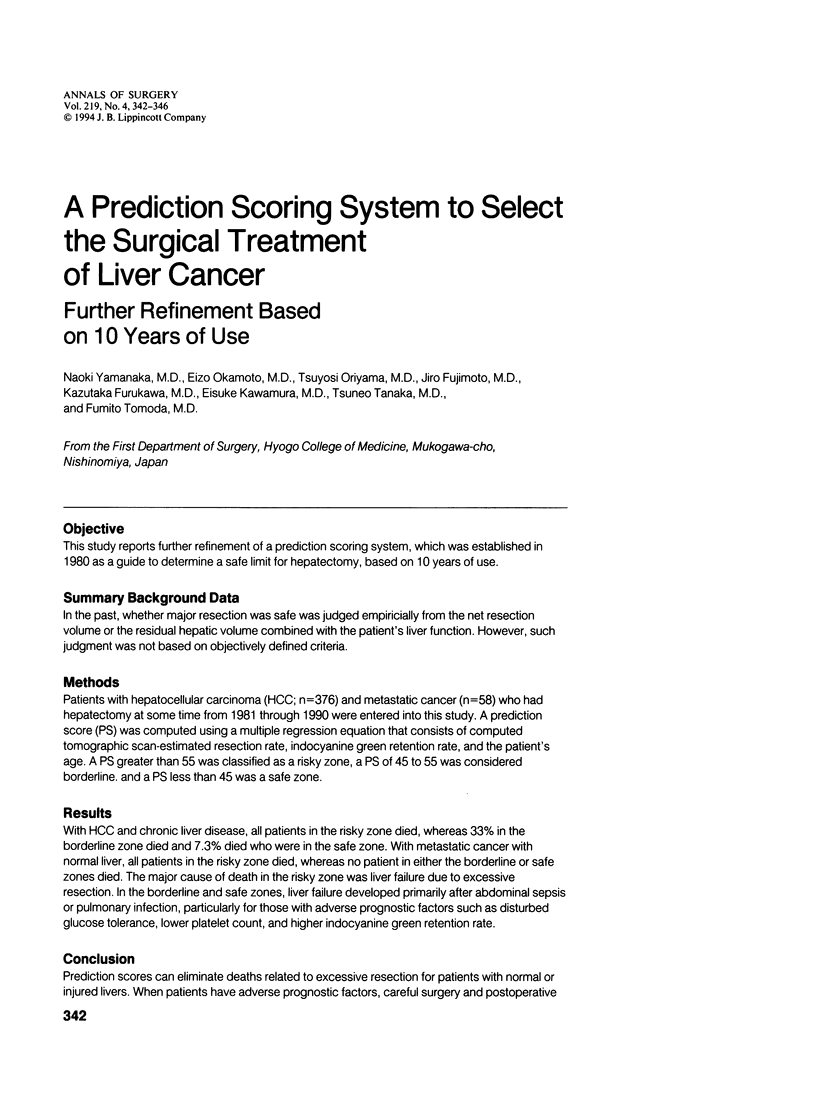

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bismuth H., Houssin D., Castaing D. Major and minor segmentectomies "réglées" in liver surgery. World J Surg. 1982 Jan;6(1):10–24. doi: 10.1007/BF01656369. [DOI] [PubMed] [Google Scholar]
- Brown D. A., Pommier R. F., Woltering E. A., Fletcher W. S. Nonanatomic hepatic resection for secondary hepatic tumors with special reference to hemostatic technique. Arch Surg. 1988 Sep;123(9):1063–1066. doi: 10.1001/archsurg.1988.01400330039005. [DOI] [PubMed] [Google Scholar]
- Didolkar M. S., Fitzpatrick J. L., Elias E. G., Whitley N., Keramati B., Suter C. M., Brown S. Risk factors before hepatectomy, hepatic function after hepatectomy and computed tomographic changes as indicators of mortality from hepatic failure. Surg Gynecol Obstet. 1989 Jul;169(1):17–26. [PubMed] [Google Scholar]
- Fujiwara K., Ogata I., Mochida S., Yamada S., Hirata K., Tomiya T., Ohta Y. Activated Kupffer cells as a factor of massive hepatic necrosis after liver resection. Hepatogastroenterology. 1990 Apr;37(2):194–197. [PubMed] [Google Scholar]
- Lee N. W., Wong J., Ong G. B. The surgical management of primary carcinoma of the liver. World J Surg. 1982 Jan;6(1):66–75. doi: 10.1007/BF01656375. [DOI] [PubMed] [Google Scholar]
- Malt R. A. Surgery for hepatic neoplasms. N Engl J Med. 1985 Dec 19;313(25):1591–1596. doi: 10.1056/NEJM198512193132507. [DOI] [PubMed] [Google Scholar]
- Monden K., Arii S., Itai S., Sasaoki T., Adachi Y., Funaki N., Higashitsuji H., Tobe T. Enhancement and hepatocyte-modulating effect of chemical mediators and monokines produced by hepatic macrophages in rats with induced sepsis. Res Exp Med (Berl) 1991;191(3):177–187. doi: 10.1007/BF02576673. [DOI] [PubMed] [Google Scholar]
- Nagorney D. M., van Heerden J. A., Ilstrup D. M., Adson M. A. Primary hepatic malignancy: surgical management and determinants of survival. Surgery. 1989 Oct;106(4):740–749. [PubMed] [Google Scholar]
- Noguchi T., Imai T., Mizumoto R. Preoperative estimation of surgical risk of hepatectomy in cirrhotic patients. Hepatogastroenterology. 1990 Apr;37(2):165–171. [PubMed] [Google Scholar]
- Okamoto E., Kyo A., Yamanaka N., Tanaka N., Kuwata K. Prediction of the safe limits of hepatectomy by combined volumetric and functional measurements in patients with impaired hepatic function. Surgery. 1984 May;95(5):586–592. [PubMed] [Google Scholar]
- Ong G. B., Lee N. W. Hepatic resection. Br J Surg. 1975 Jun;62(6):421–430. doi: 10.1002/bjs.1800620602. [DOI] [PubMed] [Google Scholar]
- Ozawa K., Ida T., Yamada T., Honjo I. Significance of glucose tolerance as prognostic sign in hepatectomized patients. Am J Surg. 1976 May;131(5):541–546. doi: 10.1016/0002-9610(76)90006-4. [DOI] [PubMed] [Google Scholar]
- Savage A. P., Malt R. A. Elective and emergency hepatic resection. Determinants of operative mortality and morbidity. Ann Surg. 1991 Dec;214(6):689–695. doi: 10.1097/00000658-199112000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone H. H., Long W. D., Smith R. B., 3rd, Haynes C. D. Physiologic considerations in major hepatic resections. Am J Surg. 1969 Jan;117(1):78–84. doi: 10.1016/0002-9610(69)90288-8. [DOI] [PubMed] [Google Scholar]
- Trede M., Raute M. Surgical therapy of primary liver tumors. Recent Results Cancer Res. 1986;100:197–211. doi: 10.1007/978-3-642-82635-1_26. [DOI] [PubMed] [Google Scholar]
- Wu M. C., Chen H., Zhang X. H., Yao X. P., Yang J. M. Primary hepatic carcinoma resection over 18 years. Chin Med J (Engl) 1980 Oct;93(10):723–728. [PubMed] [Google Scholar]
- Yamada R., Nakatsuka H., Nakamura K., Sato M., Itami M., Kobayashi N., Minakuchi K., Onoyama T., Kanno T., Monna T. Hepatic artery embolization in 32 patients with unresectable hepatoma. Osaka City Med J. 1980;26(2):81–96. [PubMed] [Google Scholar]
- Yamanaka N., Okamoto E., Kuwata K., Tanaka N. A multiple regression equation for prediction of posthepatectomy liver failure. Ann Surg. 1984 Nov;200(5):658–663. doi: 10.1097/00000658-198411000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]


