Abstract
Introduction
The outcome of reverse shoulder arthroplasty (RSA) is strongly correlated to the accuracy of implantation, particularly with regard to inclination of the glenoid component. 3D planning has become more prevalent and with this has come the development of patient-specific instruments (PSI). In our centre, since 2019, all elective RSAs have been planned with a 3D printed PSI. We hypothesised that PSI has improved the inclination of the glenoid component since its introduction.
Methodology
Retrospective analysis identified 50 elective RSAs pre and post the use of PSI. Post-operative radiographs were assessed in the anterior–posterior orientation to identify an inclination angle by two investigators.
Findings
The interrater reliability (ICC 3K) between the two investigators was 0.960 (CI 0.94–0.97). The mean inclination of the none PSI group was +7.53° (SD ±14.31) while the mean inclination of the PSI group was +2.95° (SD ±7.82) (p = 0.0498).
Conclusion
This study demonstrates that routine use of an additional intra-operative adjunct, such as a PSI jig for all cases of RSA should be considered, to improve the ability of the surgeon to reproduce the surgical plan faithfully.
Keywords: Arthroplasty, reverse shoulder arthroplasty, PSI
Introduction
Since the development of the reverse shoulder arthroplasty (RSA) by Paul Grammont and his first eight reported cases in 1987, implant technology and surgical techniques have progressed significantly. 1 The principles first proposed by Grammont regarding the medialisation of the centre of rotation still remain the same with the modern prostheses but we now possess technology that allows us to improve on these principles in order to obtain improved outcomes. Such technology includes three-dimensional imaging, pre-operative planning software platforms and patient-specific instrumentation (PSI).
RSA is now widely carried out for several indications affecting the glenohumeral joint such as rotator cuff tear arthropathy, irreparable rotator cuff tears, glenohumeral osteoarthritis, revision surgery for failed anatomical total shoulder arthroplasty (ASA) and proximal humerus fractures. 2
The National Joint Registry of England, Wales and Northern Ireland (NJR) reported in 2022 that there were 5099 RSAs carried out (71% of primary shoulder arthroplasties), an increase from 2014 when 2238 reverse shoulder arthroplasties were performed (40% of primary shoulder arthroplasties). 3 Interrogating the same database showed that in 2022 there were 662 revision cases reported. Of the 662 revisions, 100 were due to instability, 76 for aseptic glenoid loosening, 63 for dislocation/subluxation and 63 for glenoid implant wear. With the growing number of RSAs performed over the 10-year period of monitoring in the NJR and with the current number of revision cases performed for instability, loosening, dislocation and implant wear, one may deduce that revision numbers would also be expected to increase in years to come. With this in mind, the need to reduce preventable risk factors for revision would seem a sensible strategy.3,4
Traditionally, placement of the central guide pin, which dictates inclination and version of the glenoid component in RSA, is performed freehand based on the surgeon correlating intraoperative findings with pre-operative imaging, either in the form of plain radiographs or computerised tomography (CT). This relies heavily on surgeon's skill and previous experience, in order to ensure an optimal position of the glenoid component. Patient-specific instruments (PSIs) aim to improve accuracy and reproducibility of glenoid positioning.5,6 PSI involves the generation of a custom guide based on an individual's anatomy to facilitate placement of the guide pin in the optimal version, inclination and location. Although some units reserve the use of PSI for patients with complex anatomy, our centre has been using 3D printed PSI jigs for all elective reverse shoulder arthroplasties since 2019. We hypothesise that routine use of PSI will improve inclination of the glenoid component in RSA, compared to arthroplasties performed without the use of a PSI jig.
Materials and methods
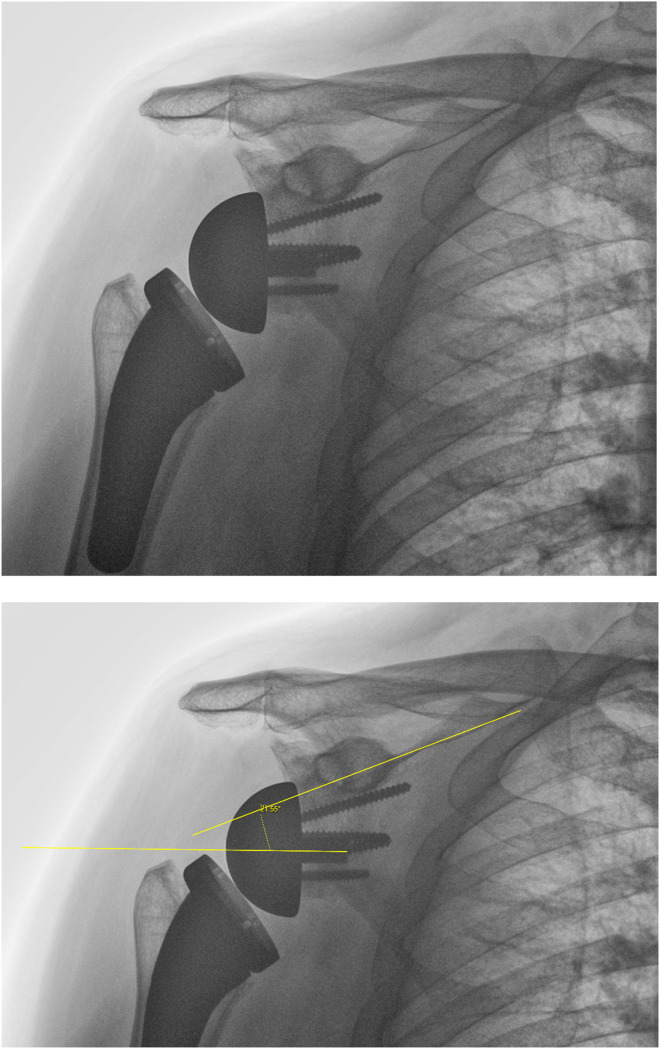
A retrospective analysis was carried out of all primary RSAs performed at our centre, to identify 50 elective cases performed before the introduction of PSI jigs and 50 cases that were carried out after PSI jigs started to be used for all elective shoulder arthroplasties. All 100 of the patients included in this study had a pre-operative surgical plan on the Blueprint software (Stryker Corporation, Kalamazoo, MI), which has been in use in our unit for several years. Those who had RSA performed for revision or acute fracture were excluded from analysis as were all those without adequate or missing post-operative radiographs. Post-operative radiographs were assessed in anterior–posterior orientation, and an inclination angle was measured using the angle between the central screw of the base plate and the sclerotic line of the supraspinatus fossa as a reference, as described by Boileau and Maurer,7,8 using the Philips Vue Picture Archiving and Communication System (PACS). An example of the measurements of inclination are shown in Figures 1 and 2 (an inferiorly inclined angle was denoted as having a negative value (-) while a superiorly inclined angle was denoted with a positive value (+), a value of zero would denote the central peg of the baseplate being parallel to the supraspinatus fossa. Measurements were carried out by two investigators who were blinded to the use of PSI.
Figure 1.
How inclination angle was measured using anterior–posterior radiographs.
Figure 2.
An example of an inclination angle with a positive value.
Five surgeons, all with upper limb fellowship training, performed the procedures included in this study, between 2015 and 2024. All surgeries were carried out in the beach-chair position, through a delto-pectoral approach and with the aid of a pneumatic arm holder. The implants used on the glenoid were the Aequalis Reversed II baseplate, the Tornier Perform Reversed baseplate and the Tornier Perform Reversed Augmented Glenoid, all made and supplied by Stryker (Stryker Corporation, Kalamazoo, MI). All patients underwent a subscapularis peel off the lesser tuberosity, if the tendon was present. The tendon was repaired through trans-osseous sutures at the end of the procedure, where feasible. With regards to glenoid management, a 360° debridement of capsulolabral tissue was carried out, prior to PSI jig placement. The operating surgeons did not debride any glenoid osteophytes prior to central wire insertion, in order for the PSI jig to accurately find its correct position on the glenoid, as planned with these osteophytes in situ. The surgeons did not alter their surgical technique or exposure between the two cohorts, as the PSI jig that was used is low profile and easy to insert by hand onto the glenoid surface.
A pilot analysis of the first 20 RSA radiographs was performed. Inclination was measured in 10 cases with a PSI and 10 without a PSI. A power calculation with effect size of 1.159, alpha error of 0.05 and power of 0.8 demonstrated that a minimum of 13 patients would be needed in each group when investigating inclination.
The final dataset was shown to be parametric through the use of a Kolmogrov–Smirnov test and thus a t-test for two independent samples was used to determine the statistical significance of any differences in inclination. The interrater reliability was measured with the intra-class correlation coefficient (ICC 3 K) where an outcome of 1 indicates identical correlation and 0 indicates no correlation at all. All statistical analysis was performed programmatically using Python 3.8 with the following packages: Numpy 2.1, Pandas 2.2.2, Scipy 1.12.1 and Statsmodels.
Results
We identified a total of 205 patients who underwent an RSA, between 2015 and 2024. We excluded cases of acute trauma (n = 34), revision cases (n = 29), patients without an appropriate post-operative radiograph (n = 31), those that had the incorrect procedure documented (n = 6), one case of intraoperative fracture (n = 1), patients who were lost to follow-up and did not have a post-operative radiograph (n = 3) and a case where the guide had been ordered but was unclear whether it had been used (n = 1). This resulted to a non-PSI cohort of 50 patients and a PSI group of 50 patients (Figure 3). The indications for RSA for each cohort are shown in Table 1.
Figure 3.
Flowchart shows the total number of patients and the final number of the included patients.
Table 1.
Indications for RSA in PSI and non-PSI groups.
| No PSI | PSI | |
|---|---|---|
| Trauma sequalae | 9 | 3 |
| Cuff tear arthropathy | 20 | 25 |
| Osteoarthritis | 16 | 18 |
| Avascular necrosis | 3 | 2 |
| Other inflammatory arthropathy | 2 | 2 |
| Total | 50 | 50 |
The average age of the non-PSI cohort was 74.90 years while the average age of the PSI cohort was 73.38. Both the PSI and non-PSI cohort had 12 males and 38 females. The Walch classification for each cohort is shown in Table 2.
Table 2.
Walch classification of PSI and non-PSI group.
| Walch classification | PSI (%) | Non-PSI |
|---|---|---|
| A1 | 30 | 55 |
| A2 | 16 | 12.5 |
| B1 | 16 | 7.5 |
| B2 | 10 | 15 |
| B3 | 16 | 0 |
| C | 0 | 0 |
| D | 12 | 10 |
The average difference between the two investigators measurements was −1.96. The interrater reliability measured with the ICC 3 K between the two investigators was 0.960 (CI 0.94–0.97), which showed excellent correlation between their measurements.
The mean baseplate inclination of the non-PSI group was +7.53° (SD ±14.31) while the mean inclination of the PSI group was +2.95° (SD ±7.82) and these were different to a statistically significant degree (p = 0.0498).
Discussion
In considering the rising number of primary RSA cases and the expected increase in revision cases, the German registry reported that between 2014 and 2018, the most common indications for revision of a RSA were instability, glenoid loosening and ‘unspecified reason’ 9 which is similar to the report from the Australian registry. 10 Boileau et al. suggested that prosthetic instability is the main cause for revision, accounting for 38% of revisions for their cohort between 1993 and 2013. 11 Gauci et al. also analysed the most commons indications for re-intervention in an analysis of failed arthroplasties and reported instability to be the cause in 32% of RSA revisions. 12
Aseptic loosening
Aseptic baseplate loosening was a common complication with the early Grammont style prosthesis. 2 Analysis of more modern prosthesis implanted between 2007 and 2021, found only 0.74% of prostheses with evidence of aseptic glenoid loosening (53 out of 7162). 13 Analysis of this patient cohort identified several potential patient risk factors, such as rheumatoid arthritis and diabetes mellitus and implant/anatomical risk factors, including Walch Glenoid Types B2 and 3, lateralised glenoid components and augmented baseplates. The need for bone grafting at index surgery also appears to correlate with an increase likelihood of aseptic baseplate loosening. An analysis of 753 primary RSAs showed 23 patients with baseplate failures, of which 22 received glenoid bone grafting. 14 The reason for these revisions may be due to failure of graft incorporation or due to a worse starting point with increased glenoid erosion pre-operatively, necessitating a graft.
Fifteen degrees of inferior inclination of the baseplate has been shown to demonstrate the most uniform compressive force and the least amount of tensile force and micro motion, compared to both neutral and superior inclination. 15 One could therefore infer that a superiorly inclined baseplate would have a higher risk of glenoid loosening. This was also suggested by Boileau et al. when they presented their measurement of ‘the reverse shoulder arthroplasty angle’. 7
Instability
Biomechanical models have demonstrated the effects of component positioning on instability after RSA. Lateralisation of the glenoid implant has been shown to reduce the risk of instability. 16 Version of the humeral component is a critical component according to Favre et al., with significant retroversion of the glenoid component (>20°) resulting to decreased stability. 17 More recent cadaveric biomechanical models have demonstrated significant correlation between inclination angle and anterior dislocation, suggesting that inferior inclination of the baseplate positively correlates with prosthetic stability. 18 Randelli et al. compared their patients’ radiographs who sustained dislocations, to those that were stable and demonstrated a significant association between glenosphere tilt and post-operative dislocation, where stable patients had an average of 10° inferior tilt, compared to a superior tilt of 2.2° in unstable patients. 19 With a larger patient cohort of 97 patients, Tashjian et al. also reported that a greater superior baseplate inclination is significantly associated with instability. 20
Scapular notching
Current evidence suggests that scapular notching results in worse patient outcomes following RSA. 21 Patients with pre-operative superior glenoid wear have been shown to present with an increased incidence of post-operative scapular notching, as shown by Lavigne et al. on their analysis of 337 of their patients undergoing RSA. 22 This was corroborated by Falaise et al., where patients without notching had a pre-operative glenoid inclination of 92.3°, while those with notching had an inclination of 85°. Both authors hypothesised that a preoperative superiorly inclined glenoid likely resulted in a glenoid component in superior inclination, although this is yet to be shown in the literature as a statistically significant correlation. Finally, patients without notching have been shown to have a significantly more inferiorly translated position of the glenoid component compared to those with notching. 23
It therefore becomes evident that appropriate placement of the glenoid baseplate in RSA is vital in reducing the risk for early revision. Malpositioning can lead to aseptic loosening, instability, impingement, reduced range of motion and scapular notching. 24 These complications likely share an association with superior tilt of the glenoid component.13,15,18–20,22,25 It follows that comprehensive pre-operative assessment of glenoid pathology and planning of implant positioning is likely to have a positive impact on clinical outcomes and to reduce the need for revision surgery.
Cadaveric studies comparing 3D preoperative plans with postoperative CT implant placement in both RSA and ASA have shown increased reliability and precision in glenoid component positioning when using patient specific instrumentation compared to cases without PSI.26–30 Hao et al. showed that glenoid implant placement was not accurate in patients with or without glenoid wear, with 53% of glenoid implants malpositioned when surgeons were blinded to a computer navigation system, compared to the pre-operative plan. 31 There is a variety of pre-operative planning software platforms and PSI systems currently available in the market and these vary in measurement techniques used to estimate glenoid anatomical parameters. 32
Some units reserve the use of PSI for patients with complex anatomy, rather than using it in all patients. It is however well documented that superior tilt of the glenoid component needs to be avoided in implantation to avoid early loosening, risk of dislocation and revision.7,15,20,33,34 With this in mind, all techniques and technological advancements that may increase the reliability and accuracy of implant placement should be considered by surgeons performing RSA. Our results demonstrate improvement of radiographic baseplate inclination with an increase in inferior inclination but also narrower standard deviation with the use of PSI. One could hypothesise that this could correlate in the future with better outcomes in terms of stability and reduced risk of aseptic loosening based on published literature, but this is yet to be shown through an appropriate study design.
Elsheikh et al. reported no significant difference in clinical outcomes for PSI cases compared to non-PSI cases, in their study of 53 patients at a median follow-up of 46 months. 34 The authors did report a higher probability of achieving appropriate baseplate position in the PSI group, but this did not achieve statistical significance. Hess et al. carried out a meta-analysis in the use of 3D-printed guides in several sub-specialties in Trauma and Orthopaedics and with regards to shoulder arthroplasty they demonstrated an average of 2.95° of deviation between the pre-operative plan and the post-operative implant position, in patients who had a guide used in their operations. They suggested the use of 3D printed guides for complex arthroplasty cases. 35 These results were similar to a shoulder arthroplasty specific meta-analysis published by Villatte et al., which demonstrated reduced deviation in version, inclination and entry point, when using PSI jigs as compared to standard instrumentation. 6 When assessing implant inclination, the PSI group demonstrated deviation from the surgical plan of 1.89°, whereas the standard instrumentation group showed a deviation from the surgical plan of 5.78°. The difference was statistically significant.
While discussing the accuracy of implantation and relevant strategies to improve this, one should also consider clinical outcomes, especially aseptic loosening and instability/dislocation rates. Navarro et al. performed a large retrospective cohort study of more than 8000 procedures, investigating both the use of pre-operative CT scans and also the use of PSI. 36 Notwithstanding that patients with PSI were more likely to have a Walch B or C type glenoid, they reported no difference in one year aseptic loosening-related revision rates but found that the 90-day risk of deep infection was increased with the use of PSI.
Our study is not without limitations. The two cohorts were operated on over several years within our unit and there is a possibility of the PSI group benefiting from increased surgeon experience over the study timeline, as well as from other improvements in surgical technique and instrumentation. The aim of this study, however, was to compare current practice (PSI use), to practice that is now historical in our unit (non-PSI use), and the above limitation could not have been avoided. More definitive conclusions on this topic would require a randomised controlled prospective study, directly comparing baseplate inclination and functional outcomes between PSI cases and non PSI cases for primary RSAs. Also, there is a cost implication with the use of PSI and the need for early pre-operative planning, to allow ordering and delivery of the PSI jigs, but we feel that these cost differences are justified by the increase in reliability of glenoid positioning and the patient functional benefits that may derive from this. Finally, we only used a plain antero-posterior (AP) radiograph in measuring glenoid inclination and not a CT scan; however, the angle that we measured is one that may reliably be measured from an AP radiograph and does not require more complex imaging modalities.
In our study, all cases had a pre-operative surgical plan with the use of the Blueprint software. We compared the ability of surgeons to enact a previously determined precise surgical plan, using palpable and visual anatomical landmarks intra-operatively (non-PSI group), versus the same intra-operative assessment and also a PSI jig (PSI group). In essence, in both groups the surgeon's understanding and knowledge of the anatomy was the same and despite this, PSI use still improved accuracy. We therefore suggest that routine use of an additional intra-operative adjunct, such as a PSI jig for all cases of RSA should be considered, to improve the ability of the surgeon to reproduce the surgical plan accurately.
Footnotes
Contributorship: GL, WD, AS and HU were responsible for data collection and analysis. HU, AA, AR and CY were responsible for the concept and design of the work. GL, HU, SS, AA, AR and CY were responsible for drafting and revising the article. All authors have approved the article submitted.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Local Trust Audit Committee—2023/24_Trust_T&O_8.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Guarantor: HU.
Informed consent: Not required.
ORCID iDs: George Lee https://orcid.org/0000-0002-4332-9231
Angelos Assiotis https://orcid.org/0000-0002-8802-9048
Adam Rumian https://orcid.org/0000-0001-8158-8384
Simran Sahota https://orcid.org/0009-0008-1727-9059
Trial registration: Not required.
References
- 1.Grammont P, Trouilloud P, Laffay J, et al. Study and development of a new shoulder prosthesis [in French]. Rhumatologie 1987; 39: 407–418. [Google Scholar]
- 2.Boileau P, Watkinson DJ, Hatzidakis AM, et al. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 2005; 14: 147S–161S. [DOI] [PubMed] [Google Scholar]
- 3.National Joint Registry England, Wales and Northern Ireland . 11th Annual Report 2014 [Internet], https://reports.njrcentre.org.uk/Portals/1/PDFdownloads/NJR%2011th%20Annual%20Report%20-%20Online%20appendices%202014.pdf (2014).
- 4.National Joint Registry England, Wales and Northern Ireland . 20th Annual Report 2023 [Internet], https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2020th%20Annual%20Report%202023.pdf (2023).
- 5.Levins JG, Kukreja M, Paxton ES, et al. Computer-assisted preoperative planning and patient-specific instrumentation for glenoid implants in shoulder arthroplasty. JBJS Rev 2021; 9(9):e20.00236. [DOI] [PubMed] [Google Scholar]
- 6.Villatte G, Muller AS, Pereira B, et al. Use of Patient-Specific Instrumentation (PSI) for glenoid component positioning in shoulder arthroplasty. A systematic review and meta-analysis. PLoS One 2018; 13: e0201759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boileau P, Gauci MO, Wagner ER, et al. The reverse shoulder arthroplasty angle: a new measurement of glenoid inclination for reverse shoulder arthroplasty. J Shoulder Elbow Surg 2019; 28: 1281–1290. [DOI] [PubMed] [Google Scholar]
- 8.Maurer A, Fucentese SF, Pfirrmann CW, et al. Assessment of glenoid inclination on routine clinical radiographs and computed tomography examinations of the shoulder. J Shoulder Elbow Surg 2012; 21: 1096–1103. [DOI] [PubMed] [Google Scholar]
- 9.Kircher J, Ohly B, Fal MF, et al. Analysis of revision shoulder arthroplasty in the German nationwide registry from 2014 to 2018. JSES Int 2021; 5: 382–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Australian Orthopaedic Association National Joint Replacement Registry . 20th Annual Report 2019 [Internet], https://aoanjrr.sahmri.com/documents/10180/668596/Hip%2C(Knee(%26(Shoulder(Arthroplasty/c287d2a3-22df-a3bb-37a2-91e6c00bfcf0 (2020).
- 11.Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res 2016; 102: S33–S43. [DOI] [PubMed] [Google Scholar]
- 12.Gauci MO, Cavalier M, Gonzalez JF, et al. Revision of failed shoulder arthroplasty: epidemiology, etiology, and surgical options. J Shoulder Elbow Surg 2020; 29: 541–549. [DOI] [PubMed] [Google Scholar]
- 13.Schell LE, Roche CP, Eichinger JK, et al. Aseptic glenoid baseplate loosening after reverse total shoulder arthroplasty with a single prosthesis. J Shoulder Elbow Surg 2023; 32: 1584–1593. [DOI] [PubMed] [Google Scholar]
- 14.Lo EY, Witt A, Ouseph A, et al. Comparison of early and late aseptic baseplate failure in primary reverse shoulder arthroplasty with and without structural glenoid autograft. J Shoulder Elbow Surg 2025; 34: 820–827. [DOI] [PubMed] [Google Scholar]
- 15.Gutiérrez S, Greiwe RM, Frankle MA, et al. Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg 2007; 16: S9–S12. [DOI] [PubMed] [Google Scholar]
- 16.Guarrella V, Chelli M, Domos P, et al. Risk factors for instability after reverse shoulder arthroplasty. Shoulder Elbow 2021; 13: 51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Favre P, Sussmann PS, Gerber C. The effect of component positioning on intrinsic stability of the reverse shoulder arthroplasty. J Shoulder Elbow Surg 2010; 19: 550–556. [DOI] [PubMed] [Google Scholar]
- 18.Pastor MF, Nebel D, Becker LM, et al. Does glenoid inclination affect the anterior stability of reverse total shoulder arthroplasty? A biomechanical study. Eur J Orthop Surg Traumatol 2024; 34: 2353–2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Randelli P, Randelli F, Arrigoni P, et al. Optimal glenoid component inclination in reverse shoulder arthroplasty. How to improve implant stability. Musculoskelet Surg 2014; 98: 15–18. [DOI] [PubMed] [Google Scholar]
- 20.Tashjian RZ, Martin BI, Ricketts CA, et al. Superior baseplate inclination is associated with instability after reverse total shoulder arthroplasty. Clin Orthop Relat Res 2018; 476: 1622–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jang YH, Lee JH, Kim SH. Effect of scapular notching on clinical outcomes after reverse total shoulder arthroplasty. Bone Joint J 2020; 102-B: 1438–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friedman RJ, Barcel DA, Eichinger JK. Scapular notching in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2019; 27: 200–209. [DOI] [PubMed] [Google Scholar]
- 23.Kolmodin J, Davidson IU, Jun BJ, et al. Scapular notching after reverse total shoulder arthroplasty: prediction using patient-specific osseous anatomy, implant location, and shoulder motion. J Bone Joint Surg Am 2018; 100: 1095–1103. [DOI] [PubMed] [Google Scholar]
- 24.Rodriguez J, Entezari V, Iannotti JP, et al. Pre-operative planning for reverse shoulder replacement: the surgical benefits and their clinical translation. Ann Joint 2019; 4: 4. doi: 10.21037/aoj.2018.12.09 [DOI] [Google Scholar]
- 25.Gutiérrez S, Walker M, Willis M, et al. Effects of tilt and glenosphere eccentricity on baseplate/bone interface forces in a computational model, validated by a mechanical model, of reverse shoulder arthroplasty. J Shoulder Elbow Surg 2011; 20: 732–739. [DOI] [PubMed] [Google Scholar]
- 26.Throckmorton TW, Gulotta LV, Bonnarens FO, et al. Patient-specific targeting guides compared with traditional instrumentation for glenoid component placement in shoulder arthroplasty: a multi-surgeon study in 70 arthritic cadaver specimens. J Shoulder Elbow Surg 2015; 24: 965–971. [DOI] [PubMed] [Google Scholar]
- 27.Levy JC, Everding NG, Frankle MA, et al. Accuracy of patient-specific guided glenoid baseplate positioning for reverse shoulder arthroplasty. J Shoulder Elbow Surg 2014; 23: 1563–1567. [DOI] [PubMed] [Google Scholar]
- 28.Walch G, Vezeridis PS, Boileau P, et al. Three-dimensional planning and use of patient-specific guides improve glenoid component position: an in vitro study. J Shoulder Elbow Surg 2015; 24: 302–309. [DOI] [PubMed] [Google Scholar]
- 29.Eraly K, Stoffelen D, Vander Sloten J, et al. A patient-specific guide for optimizing custom-made glenoid implantation in cases of severe glenoid defects: an in vitro study. J Shoulder Elbow Surg 2016; 25: 837–845. [DOI] [PubMed] [Google Scholar]
- 30.Yoon JP, Kim DH, Jung JW, et al. Patient-specific guides using 3-dimensional reconstruction provide accuracy and reproducibility in reverse total shoulder arthroplasty. Clin Shoulder Elb 2019; 22: 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hao KA, Sutton CD, Wright TW, et al. Influence of glenoid wear pattern on glenoid component placement accuracy in shoulder arthroplasty. JSES Int 2022; 6: 200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rojas J, Lievano, Jiménez AM, et al. Preoperative planning in reverse shoulder arthroplasty: plain radiographs vs. computed tomography scan vs. navigation vs. augmented reality. Ann Joint 2023; 8: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laver L, Garrigues GE. Avoiding superior tilt in reverse shoulder arthroplasty: a review of the literature and technical recommendations. J Shoulder Elbow Surg 2014; 23: 1582–1590. [DOI] [PubMed] [Google Scholar]
- 34.Elsheikh AA, Galhoum MS, Mokhtar MA, et al. Patient-specific instrumentation versus standard surgical instruments in primary reverse total shoulder arthroplasty: a retrospective comparative clinical study. J Shoulder Elb Arthroplast 2022; 6: 24715492221075449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hess S, Husarek J, Müller M, et al. Applications and accuracy of 3D-printed surgical guides in traumatology and orthopaedic surgery: a systematic review and meta-analysis. J Exp Orthop 2024; 11: e12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Navarro RA, Chan PH, Prentice HA, et al. Use of preoperative CT scans and patient-specific instrumentation may not improve short-erm adverse events after shoulder arthroplasty: results from a large integrated health-care system. JB JS Open Access 2023; 8: e22.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]