Abstract
Background
Medial comminuted supracondylar humeral fracture (SCHF) is a common elbow injury in children, and there is no consensus on treatment yet. While crossed pinning offers biomechanical advantages for medial comminution, it carries inherent risks of iatrogenic ulnar nerve injury. This study aims to describe the surgical technique of lateral external fixation (LEF) combined with K-wire (KW) as an alternative technique and evaluate the clinical and radiological outcomes of this method.
Methods
We retrospectively analyzed 53 children (mean age 7.1 years; 28 males, 25 females) with Gartland type II (n=9) and III (n=44) SCHFs with medial comminution, treated between January 2019 and January 2022. All fractures were fixed with LEF and KW. Functional outcomes were assessed using Flynn’s criteria, with radiological parameters (carrying-angle loss, shaft condylar angle, Baumann’s angle) measured at a minimum 12-month follow-up (range, 12–26 months).
Results
At last follow-up, radiographic evaluation demonstrated a mean shaft condylar angle of 37.1°±4.4°, Baumann’s angle of 75.6°±3.6°, and carrying angle loss of 3.4°±2.0°. Range-of-motion loss averaged 3.5°±2.4°. According to Flynn’s criteria, 87% (46/53) achieved excellent and 13% (7/53) good outcomes. Subgroup analysis revealed significantly greater carrying-angle deviation (P<0.01) and motion loss (P=0.05) in Gartland III versus II fractures. Complications included two superficial pin-site infections (3.8%) resolved with oral antibiotics; no instances of iatrogenic nerve injury, vascular compromise, or malunion occurred.
Conclusions
For pediatric SCHF with medial comminution, external fixator (EF) plus KW is a feasible alternative without the risk of iatrogenic ulnar nerve injury.
Keywords: Supracondylar humeral fracture (SCHF), pediatric trauma, lateral external fixation (LEF), K-wire (KW), iatrogenic ulnar nerve injury
Highlight box.
Key findings
• For pediatric supracondylar humeral fracture (SCHF) with medial comminution, external fixator plus K-wire (KW) is a feasible alternative.
What is known and what is new?
• SCHFs with medial comminution in children are challenging due to instability and risk of reduction loss.
• This study demonstrates that combining lateral external fixation (LEF) with KW achieves excellent stability and functional outcomes in pediatric patients with medial comminution, without ulnar nerve injuries.
What is the implication, and what should change now?
• These findings may encourage surgeons to adopt LEF + KW for medial comminuted fractures to mitigate nerve injury risks. The technique’s success supports its inclusion in treatment guidelines for unstable fracture patterns. Future research should compare LEF + KW directly with crossed pinning in randomized trials to further establish efficacy and refine indications.
Introduction
Supracondylar humeral fracture (SCHF) is a common elbow injury in children, and completely displaced SCHF usually warrants surgical intervention (1). Closed reduction and percutaneous pinning (CRPP) remain the preferred surgical choice, but the optimal pinning configuration remains controversial for variable fracture patterns (2-5). In patients with unstable fracture patterns including medial column comminution, oblique fracture line, and high fracture line, loss of reduction has been reported in postoperative patients receiving CRPP (6,7).
Numerous biomechanics studies concerning the pinning configuration have been published (8-11). In patients with medial column comminution, crossed pinning provides better stability than lateral-only pinning (12). However, the risk of ulnar nerve injuries cannot be ignored. Lateral external fixation (LEF) has been proposed by Slongo in 2008 to treat displaced SCHF (13), and its effectiveness has been validated by certain authors for various conditions including delayed presentation, older children, and multi-directionally unstable fracture (14,15).
Medial comminution is defined as small butterfly fragments or comminuted small fragments after reduction, and it has been identified as a risk factor for reduction loss (16). This study focused on the displaced SCHF with medial column comminution and reviewed the effectiveness of LEF for this condition retrospectively. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-365/rc).
Methods
Pediatric patients with Gartland type II and III supracondylar fractures of humerus with comminuted medial columns were reviewed and retrieved from the hospital database between January 2019 and January 2022. In all, 53 patients received closed reduction and external fixation with additional K-wire (KW). External fixator (EF) was manufactured from Wuhan Yijiabao Biological Materials Co., Ltd. records and X-rays were collected from the database of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology.
Inclusion criteria were as follows: (I) patients younger than 14 years old at the time of surgery; (II) Gartland type II and III supracondylar fracture of the humerus with comminuted medial column; and (III) closed fracture without neurovascular compromise; and (IV) follow-up more than 12 months.
Exclusion criteria were as follows: (I) fractures concomitant with neurovascular compromise demanding open surgeries; (II) pathological fractures; (III) metabolic disorders; (IV) patients with polytrauma; and (V) earlier injury or earlier instrumentation in the same limb.
The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No. IORG0003571) and all guardians of patients signed written informed consent for participate.
Surgical technique
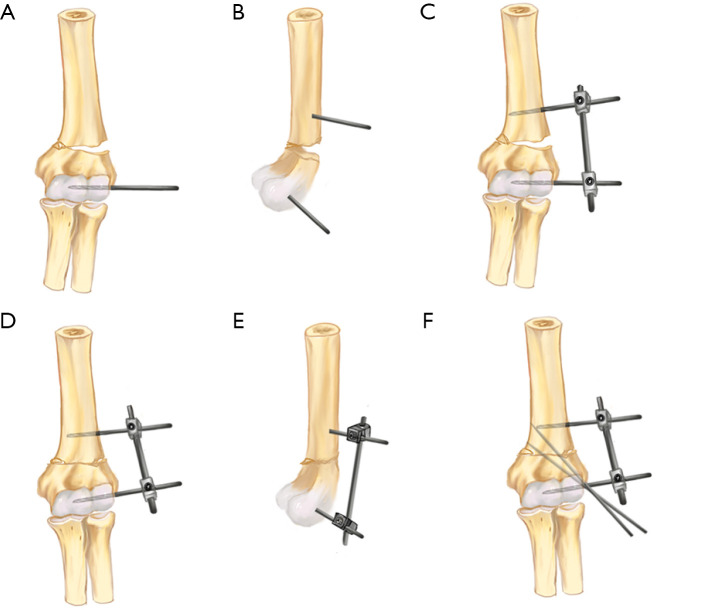
Supine position was adopted, and all surgeries were performed under general anesthesia without the application of a tourniquet. Schanz Screws (generally 3 or 4 mm in diameter) and KW with diameter 1.5 or 2.0 mm were employed in this study. Usually, one Schanz Screw was placed in the proximal and distal bone fragments, and after temporary fixation using LEF, one or two additional KW were employed to provide better anti-rotation stability. Following anesthesia, manual traction with elbow flexion was performed to reduce the fracture and restore the shaft-condylar angle and Baumann’s angle under fluoroscopic confirmation of fracture alignment and humeral capitellar physeal position. Subsequently, two 0.4 cm incisions were made 2–2.5 cm proximal to the fracture line, and the trochlea from the lateral condyle below the fracture line, avoiding the physeal line and radial nerve. Blunt dissection was carried down to the periosteum, followed by sequential insertion of two Schanz screws. With fracture reduction maintained under fluoroscopy, the EF was connected. Two KWs were then driven from the lateral epicondyle upward and medially, penetrating the fracture line to engage the medial cortex of the proximal humerus, with fluoroscopic verification of positioning and trajectory. The KWs may be configured in parallel or divergent fashion, depending on the surgeon’s preference (Figure 1).
Figure 1.
Schematic diagram of screw placement. (A) Anteroposterior view: locating the distal entry point; pin insertion into the trochlea from the lateral condyle below the fracture line. (B) Lateral view: proximal pin insertion 2–2.5 cm above the fracture line. (C) Connecting the EF after preliminary reduction. (D) Applying compression via the EF to correct medial impaction. (E) Lateral view showing satisfactory reduction. (F) Insertion of two titanium KWs. EF, external fixator; KW, K-wire.
Postoperative care and follow-up
A long-arm slab was used for 1–2 weeks to alleviate pain. All patients underwent scheduled clinical and radiographic evaluations at 3, 6, and 12 weeks postoperatively.
Implants were removed sequentially: KWs were extracted routinely without anesthesia at 3–4 weeks postoperatively in an outpatient clinic, contingent upon radiographic confirmation of definitive two-layer callus formation. Schanz screws were removed between 5 and 6 weeks postoperatively under local anesthesia in outpatient setting, requiring evidence of at least three-layer callus formation and cortical continuity on anteroposterior and lateral radiographs.
Subsequent follow-ups included quarterly radiographic assessments for 12 months. At the 1-year evaluation, clinical assessment (elbow range of motion, carrying angle) was prioritized, with radiographs obtained only if clinically indicated. Postoperative rehabilitation was not routinely prescribed; however, after cast and KW removal at 3 weeks, patients were encouraged in self-directed elbow range-of-motion exercises. Rehabilitation is recommended for patients with poor elbow motion (motion loss over 15°) during the 3-month outpatient follow-up. The recovery results of elbow joint function were evaluated based on the criteria of Flynn at their last follow-up.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) with ranges, while categorical variables are presented as frequencies and percentages. Independent samples t-tests were employed to compare outcome measures (carrying-angle loss, motion loss, shaft-condylar angle, Baumann’s angle) between subgroups stratified by fracture type (Gartland II and III), age group (<8 and ≥8 years), and sex. All analyses were conducted using IBM SPSS Statistics (version 26). A two-tailed P value <0.05 defined statistical significance.
Results
As shown in Table 1, 53 patients were enrolled in this study, including 28 boys and 25 girls. The fractures were distributed as follows: 32 cases involved the left side, and 21 cases involved the right side. According to the Gartland classification of SCHFs, 9 cases were type II and 44 cases were type III. The duration of follow-up ranged from 12 to 26 months. Table 2 summarizes the clinical parameters of patients at last follow-up. At final follow-up, Baumann’s angle measured 75.6°±3.6°, while the shaft-condylar angle was 37.1°±4.4° (range, 31–45°). The mean age was 7.1 years, and 35 of them were under 8 years old. The carrying angle deviation from the contralateral side averaged 3.4°±2.0° (range, 0–8°). Motion analysis revealed loss of 3.5°±2.4° (range, 0–10°). According to Flynn’s criteria, 46 patients (87%) achieved excellent outcomes and 7 (13%) good outcomes. Two patients (3.8%) developed superficial pin-site infections, successfully treated with oral cephalosporin without hardware removal. No deep infections, iatrogenic nerve injuries, vascular compromise, or malunions occurred. Figures 2,3 illustrate two typical cases.
Table 1. Clinical characteristics of patients.
| Variables | Data (n=53) |
|---|---|
| Age (years) | 7.1±2.4 |
| Male | 28 [53] |
| Injured side | |
| Left | 32 [60] |
| Right | 21 [40] |
| Gartland classification | |
| II | 9 |
| III | 44 |
| Follow-up (months) | 12–26 |
Data are presented as mean ± SD, number [%], number, or range. SD, standard deviation.
Table 2. Clinical parameters of patients at last follow-up.
| Parameters | Data (n=53) |
|---|---|
| Shaft condylar angle (°) | 37.1±4.4 [31–45] |
| Baumann’s angle (°) | 75.6±3.6 [70–81] |
| Carrying-angle loss (°) | 3.4±2.0 [0–8] |
| ROM loss (°) | 3.5±2.4 [0–10] |
| Postoperative scores | |
| Excellent | 46 |
| Good | 7 |
| Fair | 0 |
| Poor | 0 |
Data are presented as mean ± SD [range] or number. ROM, range of motion; SD, standard deviation.
Figure 2.
A 7-year-old female with a Gartland type III fracture in the left arm. (A) Preoperative anteroposterior and (B) lateral radiographs showing supracondylar fracture of the humerus. (C) Intraoperative anteroposterior and (D) lateral fluoroscopy confirming reduction and LEF + KW placement. (E) Three-month follow-up anteroposterior and (F) lateral radiographs after hardware removal (Flynn excellent; Baumann’s angle 77°; shaft condylar angle 38°). KW, K-wire; LEF, lateral external fixation.
Figure 3.
An 8-year-old female with a Gartland type III fracture in the right arm. (A) Preoperative anteroposterior and (B) lateral radiographs showing supracondylar fracture of the humerus. (C) Intraoperative anteroposterior and (D) lateral fluoroscopy confirming reduction and LEF + KW placement. (E) Three-month follow-up anteroposterior and (F) lateral radiographs after hardware removal (Flynn excellent; Baumann’s angle 75°; shaft condylar angle 45°). KW, K-wire; LEF, lateral external fixation.
Subgroup analyses (Table 3) demonstrated that Gartland type III fractures exhibited significantly larger carrying angle deviations compared to type II fractures (P<0.01) and greater range of motion loss (P=0.05). No statistically significant differences were observed between age groups or sexes across all measured parameters (P>0.05 for all comparisons).
Table 3. Subgroup analysis of outcomes by fracture type, age, and sex.
| Parameters | Fracture type | Age group (years) | Sex | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gartland II | Gartland III | P value | <8 | ≥8 | P value | Male | Female | P value | |||
| Number | 9 | 44 | – | 35 | 18 | – | 28 | 25 | – | ||
| Carrying-angle loss (°) | <0.01 | 0.83 | 0.56 | ||||||||
| Mean ± SD | 1.7±1.3 | 3.8±2.0 | 3.4±2.0 | 3.5±1.9 | 3.6±1.8 | 3.2±2.3 | |||||
| Range | 0–3 | 0–8 | 0–8 | 0–6 | 0–7 | 0–8 | |||||
| Motion loss (°) | 0.05 | 0.74 | 0.89 | ||||||||
| Mean ± SD | 2.1±1.8 | 3.8±2.4 | 3.4±2.5 | 3.7±2.3 | 3.5±2.5 | 3.6±2.4 | |||||
| Range | 0–4 | 0–10 | 0–10 | 0–8 | 0–10 | 0–9 | |||||
| Shaft condylar angle (°) | 0.29 | 0.24 | 0.59 | ||||||||
| Mean ± SD | 38.6±4.5 | 36.8±4.4 | 37.6±4.4 | 36.1±4.5 | 37.4±4.3 | 36.8±4.6 | |||||
| Range | 32–44 | 31–45 | 31–45 | 31–45 | 31–45 | 31–45 | |||||
| Baumann’s angle (°) | 0.28 | 0.56 | 0.62 | ||||||||
| Mean ± SD | 74.4±3.0 | 75.9±3.6 | 75.8±3.6 | 75.2±3.5 | 75.4±3.6 | 75.9±3.6 | |||||
| Range | 70–79 | 70–81 | 70–81 | 70–81 | 70–81 | 70–81 | |||||
| Excellent Flynn outcomes, n [%] | 9 [100] | 37 [84] | – | 31 [86] | 15 [83] | 25 [89] | 21 [84] | – | |||
An independent samples t-test was used to compare continuous variables between subgroups. P values <0.05 were considered statistically significant. SD, standard deviation.
Discussion
LEF delivers satisfactory outcomes in pediatric patients of SCHF with medial comminution. In our study, the incidence of complication is rare, no patient with ulnar injuries was reported, and the superficial infection of pin track was effectively ameliorated by oral antibiotics.
Supracondylar fracture is a common elbow injury in children, but discretion is required for managing this lesion due to its variability in fracture patterns (1,2,4). Closed reduction remains the preferred choice, but in patients with irreducible fractures, manual reduction seems impossible (17,18). Furthermore, various techniques were proposed to facilitate closed reduction, and mini-incision approach has been reported for easier reduction (19-21). Closed reduction followed by casting suffices for patients with stable fracture patterns. For patient with Gartland type II and III fracture, pinning is usually warranted after reduction maneuver. Lateral triple divergent pins suffices for displaced supracondylar fractures, and internal rotational stability test (IRST) is usually recommended to determine the necessity of additional KW (22).
In patients with medial comminution, crossed pinning is superior to lateral divergent pinning, but iatrogenic ulnar nerve injury seems unpredictable. Although certain authors advocated various technique tricks to lower the risk of ulnar nerve injury in crossed pinning, the underlying risk could not be eliminated due to the swelling elbow and possible anatomical variance (23). EF plus anti-rotation KW was firstly proposed by Slongo et al. for severely displaced supracondylar fracture of humerus in children, and its effectiveness has been verified by certain authors (13,14). For patients with medial comminution, EF provides strong stability after locking the screw and rod. During the procedure, adequate restoration of Baumann’s angle and anterior humeral line (AHL) was necessary, and the Baumann’s angle is supposed to be maintained as long as the EF remains in situ. In contrast to smooth KW, the EF provides better stability against the medial collapse due to fracture comminution. While the LEF alone provides stability comparable to three crossed KWs as per Li et al. [2018] (11), its resistance to valgus forces is inferior. Given the constraints of pediatric bone size limiting screw spacing (reducing rotational stability) and children’s high activity levels, additional KWs were deemed necessary to ensure adequate stability and optimal outcomes in our case series.
KW is easier to be removed in outpatient setting, and EF might require local anesthesia for removing the Schanz screws. In contrast to the mandatory casting after crossed pinning using KW, casting is not necessary for EF plus KW framework. Thus, it is easier for patients to initiate earlier rehabilitation (14). In contrast to smaller diameter and smoothness of KW, larger diameter of Schanz screws requires meticulous placement in the distal humerus for optimal purchase and seemingly longer learning curve. As for the placement of second Schanz screw in the proximal humerus, particular care is necessary to avoid accidental insult to the radial nerve. As shown in our study, there was no case of iatrogenic nerve and vascular injury, consistent with earlier reports (11,14,20,23). In contrast, accidental ulnar nerve injury is an uncommon complication in crossed pinning (24).
The absence of statistically significant subgroup differences likely reflects limited statistical power due to small sample size. Nevertheless, the consistent trend toward greater motion loss in type III fractures aligns with biomechanical evidence, suggesting potential clinical relevance despite statistical non-significance. Future studies with larger samples are needed to confirm these associations.
There were certain limitations in our study. Firstly, it was a retrospective study with relatively small sample size. The absence of a comparative group limits its level of evidence. Secondly, the control group using crossed pinning was not included in our study, and this reflects a deliberate institutional choice to avoid medial pinning in comminuted fractures due to safety concerns. Further multi-center comparative investigation with larger sample size and longer follow-up might be warranted. Notably, while this study focused on medial comminution, the LEF technique may also be suitable for fractures with lateral comminution, as its biomechanical stability could similarly mitigate collapse in such patterns.
Conclusions
For pediatric SCHF with medial comminution, EF plus KW is a feasible alternative without the risk of iatrogenic ulnar nerve injury.
Supplementary
The article’s supplementary files as
Acknowledgments
We sincerely thank Dr. Tang Xin for his valuable guidance during data collection.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No. IORG0003571) and all guardians of patients signed written informed consent for participate.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-365/rc
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-365/coif). The authors have no conflicts of interest to declare.
Data Sharing Statement
Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-365/dss
References
- 1.Mahan ST, Miller PE, Park J, et al. Fully displaced pediatric supracondylar humerus fractures: Which ones need to go at night? J Child Orthop 2022;16:355-65. 10.1177/18632521221119540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yavuz İA, Özdemir G, Akgül T, et al. Comparison of 4 surgical approaches in pediatric Gartland type 3 supracondylar humerus fractures treated by open reduction and pinning: A multicenter study. Acta Orthop Traumatol Turc 2023;57:50-4. 10.5152/j.aott.2023.22049 [DOI] [PubMed] [Google Scholar]
- 3.Yun YH, Kang HW, Lim C, et al. Use of lateral-exit crossed-pin fixation for pediatric supracondylar humeral fractures: a retrospective case series. J Pediatr Orthop B 2024;33:154-9. 10.1097/BPB.0000000000001087 [DOI] [PubMed] [Google Scholar]
- 4.Wang X, Feng C, Wan S, et al. Biomechanical analysis of pinning configurations for a supracondylar humerus fracture with coronal medial obliquity. J Pediatr Orthop B 2012;21:495-8. 10.1097/BPB.0b013e328355d01f [DOI] [PubMed] [Google Scholar]
- 5.Zhao J, Yao W, Ma J, et al. Finite element analysis of modified Slongo's external fixation in the treatment of supracondylar humeral fractures in older children. Medicine (Baltimore) 2024;103:e37979. 10.1097/MD.0000000000037979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Badin D, Boustany M, Lee RJ, et al. Incidence, risk factors, and consequences of radiographic pin migration after pinning of pediatric supracondylar humeral fractures. J Pediatr Orthop B 2023;32:575-82. 10.1097/BPB.0000000000001069 [DOI] [PubMed] [Google Scholar]
- 7.Jenkins SM, Mehlman CT, Denning JR. Unicolumnar Pin Fixation of Type III Supracondylar Humeral Fractures Is Associated With Over 3 Times Higher Odds of Lost Reduction. J Orthop Trauma 2022;36:e30-4. 10.1097/BOT.0000000000002152 [DOI] [PubMed] [Google Scholar]
- 8.Bloom T, Robertson C, Mahar AT, et al. Biomechanical analysis of supracondylar humerus fracture pinning for slightly malreduced fractures. J Pediatr Orthop 2008;28:766-72. 10.1097/BPO.0b013e318186bdcd [DOI] [PubMed] [Google Scholar]
- 9.Serbin R, Duemmler M, Bonvillain K, et al. Does Sagittal Alignment Matter? A Biomechanical Look at Pinning Pediatric Supracondylar Humerus Fractures. J Pediatr Orthop 2025;45:16-21. 10.1097/BPO.0000000000002809 [DOI] [PubMed] [Google Scholar]
- 10.Kamara A, Ji X, Liu C, et al. The most stable pinning configurations in transverse supracondylar humerus fracture fixation in children: A novel three-dimensional finite element analysis of a pediatric bone model. Injury 2021;52:1310-5. 10.1016/j.injury.2021.01.012 [DOI] [PubMed] [Google Scholar]
- 11.Li WC, Meng QX, Xu RJ, et al. Biomechanical analysis between Orthofix® external fixator and different K-wire configurations for pediatric supracondylar humerus fractures. J Orthop Surg Res 2018;13:188. 10.1186/s13018-018-0893-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaeblon T, Anthony S, Ogden A, et al. Pediatric Supracondylar Fractures: Variation in Fracture Patterns and the Biomechanical Effects of Pin Configuration. J Pediatr Orthop 2016;36:787-92. 10.1097/BPO.0000000000000554 [DOI] [PubMed] [Google Scholar]
- 13.Slongo T, Schmid T, Wilkins K, et al. Lateral external fixation--a new surgical technique for displaced unreducible supracondylar humeral fractures in children. J Bone Joint Surg Am 2008;90:1690-7. 10.2106/JBJS.G.00528 [DOI] [PubMed] [Google Scholar]
- 14.He M, Wang Q, Zhao J, et al. Lateral entry pins and Slongo's external fixation: which method is more ideal for older children with supracondylar humeral fractures? J Orthop Surg Res 2021;16:396. 10.1186/s13018-021-02541-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li J, Rai S, Tang X, et al. Surgical management of delayed Gartland type III supracondylar humeral fractures in children: A retrospective comparison of radial external fixator and crossed pinning. Medicine (Baltimore) 2020;99:e19449. 10.1097/MD.0000000000019449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwak YH, Kim JH, Kim YC, et al. Medial comminution as a risk factor for the stability after lateral-only pin fixation for pediatric supracondylar humerus fracture: an audit. Ther Clin Risk Manag 2018;14:1061-6. 10.2147/TCRM.S165825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years' experience with long-term follow-up. J Bone Joint Surg Am 1974;56:263-72. [PubMed] [Google Scholar]
- 18.Garg S, Weller A, Larson AN, et al. Clinical characteristics of severe supracondylar humerus fractures in children. J Pediatr Orthop 2014;34:34-9. 10.1097/BPO.0b013e31829c0046 [DOI] [PubMed] [Google Scholar]
- 19.Li Y, Feng Y, Chu X, et al. Minimally invasive techniques utilizing the "Joy Stick" method for managing irreducible flexion-type supracondylar fractures of the humerus in older children. J Orthop Surg Res 2024;19:441. 10.1186/s13018-024-04922-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu S, Peng Y, Liu J, et al. Small incision reduction and external fixation for the treatment of delayed over fourteen days supracondylar humeral fractures in children. Front Pediatr 2022;10:1039704. 10.3389/fped.2022.1039704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su Y, Nan G. Evaluation of A Better Approach for Open Reduction Of Severe Gartland Type III Supracondylar Humeral Fracture. J Invest Surg 2021;34:479-85. 10.1080/08941939.2019.1649766 [DOI] [PubMed] [Google Scholar]
- 22.Kaya Ö, Gencer B, Çulcu A, et al. Extra Lateral Pin or Less Radiation? A Comparison of Two Different Pin Configurations in the Treatment of Supracondylar Humerus Fracture. Children (Basel) 2023;10:550. 10.3390/children10030550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li M, Xu J, Hu T, et al. Surgical management of Gartland type III supracondylar humerus fractures in older children: a retrospective study. J Pediatr Orthop B 2019;28:530-5. 10.1097/BPB.0000000000000582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graff C, Dounas GD, Todd MRLC, et al. Management of Traumatic Nerve Palsies in Paediatric Supracondylar Humerus Fractures: A Systematic Review. Children (Basel) 2023;10:1862. 10.3390/children10121862 [DOI] [PMC free article] [PubMed] [Google Scholar]