Abstract
BACKGROUND
Traumatic vertebral artery injury (TVAI) is a serious yet underdiagnosed complication of cervical spine trauma, with an incidence ranging from 0.1% to 3.2%. While its neurological sequelae vary, the risk of vertebrobasilar ischemia can be as high as 33.3%. The authors present a rare case of bilateral vertebral artery occlusion with concomitant basilar artery occlusion following C4–5 anterolisthesis.
OBSERVATIONS
The patient initially exhibited no clinical signs of vertebrobasilar ischemia. Diagnosis was achieved through vascular imaging, and successful endovascular thrombectomy with thrombus removal was performed. Unique to this case, manual cervical reduction was carried out in the endovascular suite while maintaining catheter placement in an effort to prevent recurrent dissection or emboli migration.
LESSONS
Given the transient nature of vertebrobasilar ischemia, repeated imaging and neurological monitoring are crucial for timely intervention. This case highlights the importance of establishing standardized screening and treatment protocols to optimize outcomes and prevent further complications in patients with TVAI.
Keywords: traumatic vertebral artery injury, TVAI, bilateral vertebral artery occlusion, vertebrobasilar ischemia, endovascular thrombectomy
ABBREVIATIONS: ACDF = anterior cervical discectomy and fusion, CTA = CT angiography, DSA = digital subtraction angiography, TVAI = traumatic vertebral artery injury
Traumatic vertebral artery injury (TVAI) is a potentially serious complication of cervical spine trauma. A recent meta-analysis estimated the incidence of TVAI following cervical trauma to range from 0.1% to 3.2%.1 While the neurological sequelae of TVAI vary, the risk of vertebrobasilar ischemia has been reported to be as high as 33.3%,2 with an overall incidence of 8.8%.1 Rapid identification of patients at high risk for cerebrovascular damage is crucial to prevent significant disability and even death.
The management of TVAIs with concomitant vertebrobasilar ischemia is primarily determined by the extent of the injury, the severity of vascular compromise, and the available treatment options. Historically, patients with bilateral vertebral artery occlusion were managed with either antithrombotic therapy, thrombolytics, or, in some cases, no intervention at all.3–20 However, with advancements in endovascular interventions, these minimally invasive techniques can be utilized to restore blood flow and prevent ischemic complications.
We report a rare case of bilateral vertebral artery occlusion with concomitant basilar artery occlusion in a patient who sustained C4–5 anterolisthesis. Notably, the patient initially exhibited no clinical signs of vertebrobasilar ischemia.
Illustrative Case
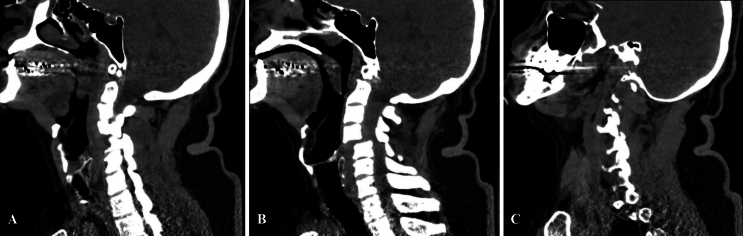
A 63-year-old male with no past medical history was brought to our trauma center after falling on his back from a height of 10–15 feet. The patient arrived 1 hour after the fall, fully conscious, with a Glasgow Coma Scale score of 15, quadriplegic, with a sensory deficit from the T4 dermatome below, positive Babinski signs bilaterally, and no rectal tone. CT imaging of the head revealed no evidence of intracranial pathology. CT imaging of the cervical spine showed 50% anterior subluxation with a right-sided perched facet, left-sided locked facet, posterior ligamentous injury, disruption of the intervertebral disc, and severe spinal cord compression at the C4–5 level (Fig. 1).
FIG. 1.
Sagittal CT images illustrating subluxation (A), left-sided locked facet (B), and right-sided perched facet (C).
Following these findings and neurosurgical evaluation, head and neck CT angiography (CTA) was ordered to facilitate cervical reduction, either closed or open with instrumentation and fusion. Because of institutional limitations, the CTA was delayed. Approximately 9 hours after admission and while awaiting CTA, the patient was found unresponsive to verbal and painful stimuli, with nonreactive pupils. The patient was subsequently intubated and, given his rapid neurological deterioration, urgent CTA of the head and neck was performed. CTA demonstrated nonopacification of the basilar artery, the right vertebral artery from C6 to C3, and the left vertebral artery from its origin to C3, consistent with thrombosis of the basilar and bilateral vertebral arteries.
The patient was transferred to the endovascular suite, where digital subtraction angiography demonstrated abrupt occlusion of the left vertebral artery proximal to the C4–5 level and a tandem occlusion at the level of the proximal basilar artery (Fig. 2A and B). Aspiration thrombectomy of the left V4 segment and basilar artery was performed, obtaining full reperfusion on the second pass and a modified treatment in cerebral infarction score of 3 (Fig. 2C and D). Closed reduction with cranial Gardner-Wells tongs and manual distraction were performed with the guide catheter in place in an effort to prevent recurrent dissection or emboli migration (Fig. 3).
FIG. 2.
A: Anteroposterior view of DSA injection into left vertebral artery showing occlusion of the V4 segment and basilar artery. B: Lateral view of DSA injection into left vertebral artery showing occlusion of the V4 segment and basilar artery. C: Intraoperative injection during deployment of the retrievable stent. D: Anteroposterior view of DSA injection into left vertebral artery showing full V4 segment and basilar artery reperfusion.
FIG. 3.
Lateral views of endovascular fluoroscopic radiographs prior to cervical reduction (A), mid-reduction maneuver (B), and after cervical reduction (C).
Postoperative CT imaging of the cervical spine confirmed adequate alignment of the C4–5 vertebrae. Gardner-Wells tongs were removed, and a cervical collar was placed. Postoperatively, the patient recovered consciousness and the capacity to follow commands with his eyes. The motor and sensory deficits remained unchanged. The patient was scheduled to undergo anterior cervical discectomy and fusion (ACDF) at the C4–5 level.
Unfortunately, the postoperative course was marked by a catastrophic reperfusion bleed that led to irreparable neurological injury from which the patient did not recover and eventually led to brain death.
Informed Consent
The necessary informed consent was obtained in this study.
Discussion
TVAI is a significant yet frequently underdiagnosed complication of cervical spine trauma, with incidence rates ranging from 0.1% to 3.2%.1 The risk is notably higher in cases of high-energy blunt trauma, particularly those involving cervical fracture dislocations, where vertebral artery entrapment, dissection, or occlusion may occur.21
While cervical spine trauma leading to TVAIs may originate from both blunt and penetrating mechanisms, blunt trauma predominates, with most cases associated with fractures involving the transverse foramen.22 This vulnerability likely stems from the natural anatomical course of the vertebral artery’s V2 segment, which traverses the transverse foramina from the C6 to C2 vertebrae,23 making it susceptible to injury in the setting of cervical fractures. Multiple studies have also shown an association between facet subluxation or dislocation and vertebral artery injury,24,25 as observed in our patient. Consequently, patients with cervical spine injuries that raise concern for TVAI should undergo vascular imaging to assess the integrity of the vertebral arteries, detect potential injuries, and evaluate blood flow dynamics.
Diagnostic imaging is crucial for detecting TVAI. DSA remains the gold standard for definitive diagnosis of acute cerebrovascular injuries.26 However, given its practicality and high sensitivity and specificity in trauma settings, CTA of the head and neck has become the preferred initial screening method.27 Nevertheless, the decision to obtain vascular imaging following nonpenetrating cervical trauma is complex and lacks standardized guidelines.28
Currently, there is no universally accepted protocol for managing vertebral artery injury following blunt cervical trauma; therefore, current practice generally relies on selective CTA screening guided by clinical judgment.28 The modified Denver screening criteria are commonly recommended as a potential tool to assist clinicians in determining the necessity of CTA screening.29 Although this screening tool has its limitations,30,31 it remains a valuable adjunctive method for identifying patients who may benefit from CTA. Nevertheless, the routine use of CTA screening in all patients who meet these criteria remains controversial, and individualized patient assessment combined with clinical judgment remains essential.28 In our case, the patient presented with cervical subluxation, meeting the modified Denver screening criteria, thereby warranting an initial CTA study. However, because of institutional limitations, the CTA study was delayed and could not be performed in a timely manner.
Initial imaging may fail to reveal vascular injuries or signs of vertebrobasilar ischemia due to the transient nature of TVAI. Some studies suggest that neurological symptoms may take up to 18 hours to manifest following cervical spine trauma,32 as examplified by our patient. Therefore, we recommed a low threshold for repeat imaging and emphasize close and frequent neurological examinations. Early detection of TVAI and associated complications is essential for timely and appropriate management.
The management of TVAI is determined by the extent of the injury and the severity of vascular compromise, guiding clinicians in deciding between intervention and a more conservative approach. Treatment options include antithrombotic therapy, such as anticoagulant or antiplatelet agents, as well as endovascular interventions.33 While no standardized treatment guidelines currently exist, all therapeutic strategies aim to prevent or reverse vertebrobasilar ischemia.
Timing of surgical intervention, particularly cervical reduction, is a critical consideration.34–36 Initially, our plan was cervical reduction and stabilization consistent with recommended practices. Unfortunately, rapid neurological deterioration led to a deviation from the scheduled surgical intervention. As a result, reduction was performed urgently and manually immediately following endovascular intervention. Subsequently, ACDF at the C4–5 level was scheduled, but ultimately canceled due to reperfusion hemorrhage.
To our knowledge, this case is among the few reported instances of bilateral vertebral artery occlusion with concomitant basilar artery occlusion due to artery-to-artery embolism successfully treated by endovascular thrombectomy and thrombus removal. The only previously documented case of thrombectomy for a similar presentation was reported by Ratnasabapathy et al.15 However, our case is unique as it is the first reported instance of manual cervical reduction performed in the endovascular suite while maintaining the catheter in an effort to prevent recurrent dissection or emboli migration. Although unconventional, this maneuver can potentially allow for cervical spine stabilization while minimizing the risk of further arterial dissection or emboli migration.
Despite advances in imaging and management, significant gaps remain in the standardization of screening protocols and treatment pathways for TVAI. Future research should focus on refining diagnostic criteria and establishing evidence-based management guidelines to improve outcomes and reduce the risk of stroke and long-term disability in these patients.
Observations
In our case, we present a rare instance of bilateral vertebral artery occlusion with concurrent vertebrobasilar ischemia following cervical spine trauma. Notably, the patient initially displayed no clinical signs of vertebrobasilar ischemia, underscoring the transient nature of this type of injury. While 1 case of endovascular thrombectomy for bilateral vertebral artery occlusion has been documented in the literature, this case represents the first reported case of manual cervical reduction in the endovascular suite while maintaining catheter placement in an effort to prevent recurrent dissection or emboli migration. This combination of cervical and vascular intervention has not been previously documented, making this case particularly noteworthy.
Lessons
This case underscores the use of endovascular management in treating patients with TVAIs and concomitant vertebrobasilar ischemia and the need for close and frequent serial examinations to detect vascular complications, which may not manifest immediately. The successful use of endovascular thrombectomy, in this case, highlights its potential to restore blood flow and prevent ischemic complications, even in complex scenarios. This case also highlights the urgent need for standardized screening protocols and evidence-based management guidelines to optimize outcomes and reduce the risk of stroke and long-term disability in patients with TVAI. However, it is essential to acknowledge that endovascular interventions have limitations and are not exempt from complications. Future research should focus on refining diagnostic criteria and treatment pathways to improve patient care.
Acknowledgments
We thank the patient’s family for their willingness to share their case and contribute to the advancement of knowledge in this field. Their cooperation and trust were invaluable in making this report possible.
We used Grammarly desktop in the writing of this paper.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: all authors. Acquisition of data: all authors. Analysis and interpretation of data: all authors. Drafting the article: all authors. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Vicenty-Padilla. Statistical analysis: Pastrana-Ramírez. Administrative/technical/material support: Calderón-Valero, Rivera-Rivera, Pastrana-Ramírez. Study supervision: Rivera-Rivera, Pastrana-Ramírez.
Correspondence
Juan C. Vicenty-Padilla: University of Puerto Rico–Medical Sciences Campus, San Juan, Puerto Rico. juan.vicenty@upr.edu.
References
- 1.Goyal K, Sunny JT, Gillespie CS.A systematic review and meta-analysis of vertebral artery injury after cervical spine trauma. Glob Spine J. 2024;14(4):1356-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Veras LM Pedraza-Gutiérrez S Castellanos J Capellades J Casamitjana J Rovira-Cañellas A.. Vertebral artery occlusion after acute cervical spine trauma. Spine (Phila Pa 1976). 2000;25(9):1171-1177. [DOI] [PubMed] [Google Scholar]
- 3.Benek B Yilmaz H Akçay E Yurt A.. Bilateral vertebral artery occlusion after traumatic complete disruption of the cervical spine associated with ankylosing spondylitis. Ulus Travma Acil Cerrahi Derg. 2021;27(6):697-701. [DOI] [PubMed] [Google Scholar]
- 4.Dobies-Krześniak B Tarnacka B.. Vertebral artery dissection following cervical spine injury as a diagnostic challenge. Case study. Ortop Traumatol Rehabil. 2019;21(5):369-378. [PubMed] [Google Scholar]
- 5.Son JI An TY Ko MJ Park SW Lee YS.. Occlusion of both vertebral arteries with development of collateral circulation from the deep cervical artery after cervical spine trauma. Korean J Neurotrauma. 2022;18(2):374-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiessling JW Whitney E Fiani B Khan YR Mahato D.. C2-3 fracture dislocation and bilateral vertebral artery occlusion without neurological injury: a case report. Cureus. 2019;11(8):e5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strickland B Lewis CS Pham MH.. Bilateral vertebral artery occlusion after cervical spine fracture dislocation. World Neurosurg. 2019;124:304-309. [DOI] [PubMed] [Google Scholar]
- 8.Elder T Tuma F.. Bilateral vertebral artery transection following blunt trauma. Int J Surg Case Rep. 2018;51:29-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Komatsu M, Suda K, Takahata M.Delayed bilateral vertebral artery occlusion after cervical spine injury: a case report. Spinal Cord Ser Cases. 2016;2:16031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golinvaux NS Basques BA Bohl DD Laurans MS Grauer JN.. Bilateral vertebral artery injury in a patient with upper cervical spine fractures leading to fatal vertebrobasilar infarction: a case report. Orthop Surg. 2015;7(3):281-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jang D Kim C Lee SJ Kim J.. Delayed brain infarction due to bilateral vertebral artery occlusion which occurred 5 days after cervical trauma. J Korean Neurosurg Soc. 2014;56(2):141-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graf AM Sakharuk I Drevets PD Abuzeid AM.. Acute basilar artery occlusion and death secondary to bilateral vertebral artery dissection. Cureus. 2022;14(8):e27927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galtés I, Borondo JC, Cos M.Traumatic bilateral vertebral artery dissection. Forensic Sci Int. 2012;214(1-3):e12-e15. [DOI] [PubMed] [Google Scholar]
- 14.Yoshihara H Vanderheiden TF Harasaki Y Beauchamp KM Stahel PF.. Fatal outcome after brain stem infarction related to bilateral vertebral artery occlusion—case report of a detrimental complication of cervical spine trauma. Patient Saf Surg. 2011;5:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ratnasabapathy U Purcell M Bhattacharya JJ.. Endovascular rescue of vertebro-basilar thrombosis in cervical spine injury. Spinal Cord Ser Cases. 2018;4:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muratsu H, Doita M, Yanagi T.Cerebellar infarction resulting from vertebral artery occlusion associated with a Jefferson fracture. J Spinal Disord Tech. 2005;18(3):293-296. [PubMed] [Google Scholar]
- 17.Taylor MW Senkowski CK.. Bilateral vertebral artery dissection after blunt cervical trauma: case report and review of the literature. J Trauma. 2002;52(6):1186-1188. [DOI] [PubMed] [Google Scholar]
- 18.Miyachi S Okamura K Watanabe M Inoue N Nagatani T Takagi T.. Cerebellar stroke due to vertebral artery occlusion after cervical spine trauma. Two case reports. Spine (Phila Pa 1976). 1994;19(1):83-88. [DOI] [PubMed] [Google Scholar]
- 19.Walsh GS Cusimano MD.. Vertebral artery injury associated with a Jefferson fracture. Can J Neurol Sci. 1995;22(4):308-311. [DOI] [PubMed] [Google Scholar]
- 20.Nowell M Nelson R.. Traumatic posterior atlantoaxial dislocation with associated C1 Jefferson fracture and bilateral vertebral artery occlusion without odontoid process fracture or neurological deficit. Eur Spine J. 2019;28(suppl 2):9-12. [DOI] [PubMed] [Google Scholar]
- 21.Zygogiannis K Benetos IS Evangelopoulos DS Koulalis D Pneumaticos SG.. Blunt traumatic vertebral artery injury after cervical fracture dislocation: a systematic review of the literature. Cureus. 2024;16(7):e65250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Temperley HC, McDonnell JM, O’Sullivan NJ.The incidence, characteristics and outcomes of vertebral artery injury associated with cervical spine trauma: a systematic review. Glob Spine J. 2023;13(4):1134-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eskander MS, Drew JM, Aubin ME.Vertebral artery anatomy: a review of two hundred fifty magnetic resonance imaging scans. Spine. 2010;35(23):2035-2040. [DOI] [PubMed] [Google Scholar]
- 24.El-Hajj VG, Habashy KJ, Cewe P.Traumatic vertebral artery injury after subaxial cervical spine injuries: incidence, risk factors, and long-term outcomes: a population-based cohort study. Neurosurgery. 2025;96(4):881-891. [DOI] [PubMed] [Google Scholar]
- 25.Chung D Sung JK Cho DC Kang DH.. Vertebral artery injury in destabilized midcervical spine trauma; predisposing factors and proposed mechanism. Acta Neurochir (Wien). 2012;154(11):2091-2098. [DOI] [PubMed] [Google Scholar]
- 26.Shaban S, Huasen B, Haridas A.Digital subtraction angiography in cerebrovascular disease: current practice and perspectives on diagnosis, acute treatment and prognosis. Acta Neurol Belg. 2022;122(3):763-780. [DOI] [PubMed] [Google Scholar]
- 27.Brommeland T, Helseth E, Aarhus M.Best practice guidelines for blunt cerebrovascular injury (BCVI). Scand J Trauma Resusc Emerg Med. 2018;26(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harrigan MR, Hadley MN, Dhall SS.Management of vertebral artery injuries following non-penetrating cervical trauma. Neurosurgery. 2013;72(suppl 2):234-243. [DOI] [PubMed] [Google Scholar]
- 29.Biffl WL, Moore EE, Elliott JP.The devastating potential of blunt vertebral arterial injuries. Ann Surg. 2000;231(5):672-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Biffl WL Egglin T Benedetto B Gibbs F Cioffi WG.. Sixteen-slice computed tomographic angiography is a reliable noninvasive screening test for clinically significant blunt cerebrovascular injuries. J Trauma. 2006;60(4):745-752. [DOI] [PubMed] [Google Scholar]
- 31.Berne JD Norwood SH McAuley CE Villareal DH.. Helical computed tomographic angiography: an excellent screening test for blunt cerebrovascular injury. J Trauma. 2004;57(1):11-19. [DOI] [PubMed] [Google Scholar]
- 32.Mueller CA, Peters I, Podlogar M.Vertebral artery injuries following cervical spine trauma: a prospective observational study. Eur Spine J. 2011;20(12):2202-2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desouza RM Crocker MJ Haliasos N Rennie A Saxena A.. Blunt traumatic vertebral artery injury: a clinical review. Eur Spine J. 2011;20(9):1405-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Badhiwala JH, Wilson JR, Witiw CD.The influence of timing of surgical decompression for acute spinal cord injury: a pooled analysis of individual patient data. Lancet Neurol. 2021;20(2):117-126. [DOI] [PubMed] [Google Scholar]
- 35.Fehlings MG, Vaccaro A, Wilson JR.Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One. 2012;7(2):e32037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ter Wengel PV De Witt Hamer PC Pauptit JC van der Gaag NA Oner FC Vandertop WP.. Early surgical decompression improves neurological outcome after complete traumatic cervical spinal cord injury: a meta-analysis. J Neurotrauma. 2019;36(6):835-844. [DOI] [PubMed] [Google Scholar]