Abstract
Background
The significant heterogeneity among individuals who die by suicide complicates prevention, suggesting that a “one-size-fits-all” approach is insufficient. It is crucial to identify distinct subgroups for targeted strategies. This study aims to characterize suicide profiles based on trait impulsivity and related factors.
Methods
Data from the FRieNDS project (Factores de Riesgo en Defunciones por Suicidio – Risk Factors in Suicide Deaths), a psychological autopsy study of 408 suicide deaths, were used. After determining the optimal number of clusters via stability analysis through agglomerative nesting, a final cluster analysis was performed on 391 valid suicide deaths (defined as cases with no missing data on the variables used for clustering) using k-means on a lower-dimensional representation of the data encoded by an autoencoder. Key clustering variables included sex, impulsivity (Barratt Impulsivity Scale-11), aggression, intent to die, previous history of suicide attempts, history of substance abuse, psychotic and affective disorders, and the presence of a depressive episode at the time of death.
Results
We identified three clusters: (1) Impulsive-aggressive (29.8%), characterized by high rates of Cluster B disorders, substance abuse, more stressful events, and low lethal intent; (2) depressive prior attempters (24.5%), which comprised mostly women and showed greater behavioural changes before death; and (3) non-impulsive/aggressive (45.7%), a group with no clear psychopathological profile, less healthcare contact, and minimal communicated intent to die, despite having few prior attempts.
Conclusions
Our study identified three suicide clusters with varying impulsivity levels, highlighting the need for tailored interventions and community-level research for better suicide prevention strategies.
Keywords: aggression, impulsivity, psychological autopsy, suicide, suicide deaths
Introduction
Global estimates indicate that suicide accounts for between 692,000 and 800,000 deaths per year [1]. Still, suicide remains a major public health challenge due to its multifactorial nature, involving genetic, neurophysiological, psychological, social, and cultural factors [2]. These complexities hinder prevention efforts. While psychiatric disorders are strongly associated with suicide [3], a significant proportion of cases occur without identified pathology [4]. Prior attempts are the strongest predictor of future suicide [5, 6], yet most suicides occur on the first attempt, limiting their predictive value [7]. Sex differences introduce further complexities: for instance, males who die by suicide are less likely than their female counterparts to have a diagnosed mental disorder and more likely to have experienced life stressors before death [8–10].
Impulsivity is closely linked to suicidal behaviour [11, 12]. Psychological autopsy studies consistently report higher trait impulsivity in suicide decedents compared to both living community controls [13–21] and individuals with similar clinical profiles [22, 23] or sudden deaths due to disease or accidents [24]. Among adults who die by suicide, high levels of impulsivity are present in both men and women, even if the prevalence is generally lower in females [18, 25]. However, impulsivity is higher in attempters than in those who die by suicide [26].
Many suicides occur in individuals with low impulsivity, who display unique characteristics. In terms of psychopathology, this group often presents with less overall diagnosed psychopathology, particularly a lower likelihood of Cluster B personality disorders and substance or alcohol use disorders [27, 28]. However, some research has linked this profile to a higher likelihood of depression [29]. Paradoxically, this lower externalizing profile is associated with a higher intent to die [28, 29], which may involve methods of high lethality [30]. Therefore, understanding this low-impulsivity profile is essential, as these individuals may be overlooked by traditional risk assessment tools that are heavily focused on overt crisis behaviours [31].
These findings underscore a key challenge in suicide prevention. Despite its multifactorial nature, distinct risk and protective factors likely apply to different subgroups. Evidence for suicidal subtypes emerges from two observations: (1) inconsistent relationships between risk factors and suicidal behaviour, and (2) associations between clinical profiles and neurobiological patterns [32]. A systematic review and meta-analysis suggest two primary subtypes of suicide decedents: impulsive and non-impulsive [33]. However, this dichotomy is further nuanced by the interplay of other critical factors. For instance, the presence of severe depression can significantly influence suicidal planning and intent regardless of impulsivity levels [30, 34], while acute life stressors may further impact risk for fatal suicide behaviour in this population [35]. Recognizing these distinctions is crucial for effective prevention and intervention.
Rationale and objectives
This study aims to characterize suicide decedents based on trait impulsivity using psychological autopsy methods. We hypothesize two groups: (i) a highly impulsive group, expected to be younger, with higher Cluster B personality and substance use disorders, and lower intent to die; and (ii) a low impulsive group, anticipated to be older, with more depressive and schizophrenia spectrum disorders, and higher intent to die.
Additionally, these groups are expected to differ in suicide pathways. The highly impulsive group is likely to face more recent negative life events and financial or work problems, while the low impulsive group may have more health issues and reduced social support. Gender differences will also be examined, as low impulsivity is a suicide risk factor in depressed women [36].
Beyond these hypotheses, we will explore potential intermediate profiles, refining impulsivity-based suicide risk models. The variables align with prior systematic review findings [33] and the study database [37].
Methods
Sample description
This study utilized data from the FRienDS research project (Factores de Riesgo en Defunciones por Suicidio – Risk Factors in Suicide Deaths) [26]. Psychological autopsies were conducted through structured interviews with relatives or close contacts of the deceased. Ethical approval was granted by the Ethics and Health Research Committee of the Virgen Macarena Hospital Area in Seville, registry number 982, adhering to the Declaration of Helsinki. The sample comprised 408 suicide decedents from Seville, Spain (2006–2018).
Procedure
Forensic doctors informed relatives about the study at the Pathology Service, explaining objectives and methodology before seeking consent. Participants received a consent form with study details and a contact number for further inquiries or withdrawal. Families were approached at least 9 months postmortem. This waiting period was implemented both to reduce the potential for recall bias in the data and, crucially, as an ethical consideration to protect the families during their most difficult time of mourning. Consequently, most interviews were conducted 12–18 months after death.
Measures
Psychological autopsies were conducted by trained psychiatrists or health psychologists, all of whom had completed at least five autopsies under senior supervision. Interviews lasted 2–4 h, following a structured protocol [38].
Data collection included sociodemographic variables, suicide history, negative life events (past year), healthcare use (final 3 months), behavioural changes (last 2 weeks), and attitudes towards death. Psychiatric diagnoses were obtained using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) Structured Clinical Interview for DSM Disorders (SCID I and II) [39, 40]. The SCID-I was used for Axis I disorders, whereas the SCID-II was used for personality disorders. Both interviews were administered by trained clinicians who established diagnoses based on fulfillment of DSM-IV-TR diagnostic criteria.
Barratt Impulsivity Scale-11: A 30-item Spanish version assessing trait impulsivity [41, 42]. Items are rated on a 4-point Likert scale (range: 30–120), covering cognitive, unplanned, and motor impulsivity. In the current sample, the scale demonstrated excellent internal consistency (Cronbach’s α = 0.889)
Brown–Goodwin Life History of Aggression (BGLHA): Evaluates aggression across childhood, adolescence, and adulthood through 11 areas (e.g., school discipline, antisocial behaviour, self-injury), scored on a 4-point Likert scale (range: 0–44) [43, 44]. The internal consistency in our sample was also excellent (Cronbach’s α = 0.946).
Beck Suicidal Intent Scale (SIS): An 18-item (range: 0–36), interviewer-rated tool assessing intent during self-harm, validated in Spanish (Cronbach’s α = 0.8) [45, 46].
Paul Ramsey Life Experience Scale: Rates acute stressful events over 6 months on a 7-point Likert severity scale (range: 0–49), with excellent test–retest reliability (r = .95) [47].
Holmes and Rahe Social Adjustment Scale: Measures chronic stress from 46 life events over a year, using the Spanish version [48, 49]. The scale is a checklist of life events, where each event is assigned a specific weighted score known as a Life Change Unit (LCU). The total score is the sum of the LCUs for all events experienced by the individual in the past year.
Life Threatening Events Questionnaire (LTE-Q): Lists 12 major life events (e.g., job loss and illness), summing checked events (range: 0–12). The Spanish adaptation shows good reliability (κ = 0.61–0.83) [50, 51].
Statistical analysis
All statistical analyses were conducted using R version 4.4.1 [52]. Cluster analysis was performed on 391 valid suicide cases, first encoding data into a lower-dimensional representation via autoencoders [53], then clustering with k-means. The number of autoencoder neurons and k-means clusters was optimized for cluster-wise stability, assessed through bootstrap resampling (1,000 samples) and Jaccard similarity [54]. A solution was considered highly stable if the mean Jaccard similarity exceeded 0.85; the selected three-cluster solution demonstrated excellent stability for the total population (mean Jaccard = 0.87) and for the sex-segregated analyses of males (0.94) and females (0.99).
Cluster variables included: sex, age, BIS, BGLHA, SIS, lifetime suicide attempts (none, one, two, or more), and psychiatric diagnoses, each treated as a binary (presence/absence) variable: depressive disorder, psychotic disorder, anxiety disorder, substance abuse disorder, and DSM-IV Cluster A personality disorder, DSM-IV Cluster B personality disorder, and DSM-IV Cluster C personality disorder. Key continuous variables, such as impulsivity and aggression scores, were included without prior categorization to preserve the full range of variance and allow the data-driven algorithm to identify natural groupings without imposing clinical thresholds.
Clusters derived from our analysis were named based on significant attributes, with sex-separated analyses conducted for men and women.
Cluster differences were assessed via a multinomial model, followed by pairwise logistic models. To account for multiple comparisons, p-values from all models were adjusted using the false discovery rate correction with the Benjamini–Hochberg procedure; these adjusted values are reported as q-values throughout the tables. Additional examined variables included the following:
Sociodemographic: Marital status, children, education, employment, income, economic dependents, living alone, and social contact.
Negative life events: Holmes–Rahe scale, Paul Ramsey scale, and LTE-Q.
Healthcare contact (last 3 months): General practitioner, psychiatrist, emergency psychiatrist, and psychologist.
Warning signs: Suicidal thoughts/intent, hospital referral, and family warning.
Behavioural changes (last 2 weeks): Work engagement, task quality, work shame, social conflicts, anger, worry, and reduced social contact.
Attitudes towards death/suicide: Preference for death over aging/being a burden, wish to die, and suicide reasons/method.
Results
Cluster analysis
The optimal number of clusters was determined using mean Jaccard similarity (Figure 1). Cluster analysis identified three distinct profiles among suicide decedents. See Table 1 for comprehensive characteristics and Figure 2 for a visual representation of the cluster profiles.
The first profile, termed “Impulsive-aggressive” (n = 108; 27.6% of the sample), was distinguished by the highest levels of impulsivity and aggression, an elevated prevalence of substance abuse, and lower suicidal intent compared to the other two clusters. This cluster was mostly male (n = 100; 93% of the cluster).
The second profile, labelled “Depressive prior attempters” (n = 105; 26.6% of the sample), exhibited the highest prevalence of current depressive episodes and a notable proportion of individuals with a history of suicide attempts. This group presented lower impulsivity and aggression than Cluster 1, while their suicidal intent was higher than that of Cluster 1 and comparable to that of Cluster 3. This cluster had the lower proportion of men (n = 19; 18%). Finally, the third profile, named “Non-impulsive/aggressive cases with no prior attempts” (n = 178; 45.5% of the sample), was characterized by the lowest levels of impulsivity and aggression. Most of its members had no history of previous suicide attempts, markedly distinguishing it from the other two profiles. This cluster comprised almost entirely of men (n = 177; 99%).
Figure 1.
Determination of the optimal number of clusters using stability analysis. This plot displays the mean Jaccard similarity for cluster solutions ranging from k = 2 to k = 15, obtained through bootstrap resampling. The Jaccard similarity coefficient measures the stability and reproducibility of the clusters. The three-cluster solution was selected as optimal because it yielded the highest mean Jaccard similarity, indicating the most stable classification of the data.
Table 1.
Characterization of the cluster according to defining variables
| Characteristic | Distribution | Multinomial model | 1 vs. 2 | 1 vs. 3 | 2 vs. 3 | ||||
|---|---|---|---|---|---|---|---|---|---|
| Impulsive-aggressive,N = 108 | Depressive prior attempters,N = 105 | Non-impulsive-aggressive,N = 178 | OR (CI)1 vs. 2 | OR (CI)1 vs. 3 | Global q-value a | q-value b | q-value b | q-value b | |
| Sex | <0.001 | ||||||||
| Male | 100 (93%) | 19 (18%) | 177 (99%) | — | — | ||||
| Female | 8 (7.4%) | 86 (82%) | 1 (0.6%) | 56.6, (23.6,136) | 0.07, (0.01,0.57) | <0.001 | 0.039 | <0.001 | |
| Age | 50 (17) | 56 (17) | 55 (22) | 1.02, (1.00,1.03) | 1.01, (1.00,1.03) | 0.051 | 0.037 | 0.13 | >0.9 |
| BIS total | 69 (25) | 49 (25) | 42 (22) | 0.97, (0.96,0.98) | 0.96, (0.94,0.97) | <0.001 | <0.001 | <0.001 | 0.038 |
| BGHA score | 26 (21) | 11 (13) | 8 (11) | 0.95, (0.93,0.97) | 0.93, (0.91,0.95) | <0.001 | <0.001 | <0.001 | 0.2 |
| Number of SA | <0.001 | ||||||||
| Two or more | 38 (35%) | 42 (40%) | 8 (4.5%) | — | — | ||||
| One | 26 (24%) | 29 (28%) | 28 (16%) | 1.01, (0.51,2.01) | 5.12, (2.02,13.0) | >0.9 | 0.002 | 0.002 | |
| None | 44 (41%) | 34 (32%) | 142 (80%) | 0.70, (0.37,1.31) | 15.3, (6.66,35.3) | 0.8 | <0.001 | <0.001 | |
| SIS score | 21 (9) | 28 (7) | 27 (7) | 1.10, (1.06,1.14) | 1.09, (1.06,1.12) | <0.001 | <0.001 | <0.001 | >0.9 |
| Depressive disorder – current | 69 (64%) | 80 (76%) | 88 (49%) | 1.81, (1.00,3.28) | 0.55, (0.34,0.90) | <0.001 | 0.2 | 0.053 | <0.001 |
| Any psychotic spectrum disorder | 17 (16%) | 34 (32%) | 30 (17%) | 2.56, (1.33,4.96) | 1.09, (0.57,2.08) | 0.004 | 0.015 | >0.9 | 0.009 |
| Substance abuse | 78 (72%) | 9 (8.6%) | 44 (25%) | 0.04, (0.02,0.08) | 0.13, (0.07,0.22) | <0.001 | <0.001 | <0.001 | 0.004 |
| Any anxiety disorder | 19 (18%) | 27 (26%) | 30 (17%) | 1.62, (0.84,3.14) | 0.95, (0.50,1.79) | 0.2 | 0.5 | >0.9 | 0.2 |
| Cluster A PD | 26 (24%) | 26 (25%) | 18 (10%) | 1.04, (0.56,1.94) | 0.35, (0.18,0.68) | 0.001 | >0.9 | 0.006 | 0.004 |
| Cluster B PD | 103 (95%) | 27 (26%) | 4 (2.2%) | 0.02, (0.01,0.05) | 0.00, (0.00,0.00) | <0.001 | <0.001 | <0.001 | <0.001 |
| Cluster C PD | 35 (32%) | 44 (42%) | 41 (23%) | 1.50, (0.86,2.63) | 0.62, (0.37,1.06) | 0.004 | 0.5 | 0.2 | 0.003 |
Abbreviations: BGHA, Brown–Goodwin Life History of Aggression; BIS, Barratt Impulsiveness Scale; CI, 95% confidence interval; OR, odds ratio; PD, personality disorder; SA, suicide attempt; SIS, Beck Suicidal Intent Scale.
Note: Data in distribution columns are presented as n (%) for categorical variables and mean (SD) for continuous variables. Bold type indicates statistical significance at the q < .05 level.
q-values for the global multinomial model were adjusted using the false discovery rate (FDR) correction.
q-values for the pairwise comparisons were adjusted using the Bonferroni correction.
Figure 2.
Radar plot of cluster profiles. Note: BGLHA, Brown–Goodwin Life History of Aggression; BIS, Barratt Impulsiveness Scale; SIS, Suicide Intent Scale. This plot provides a visual representation of the three cluster profiles across eight key variables. To allow for comparison across scales with different ranges, values for each variable have been normalized and then shifted so that the minimum value is plotted at a visible baseline (labelled “Min”) instead of the centre (r = 0). This method highlights the relative strengths and weaknesses of each profile while ensuring all cluster shapes are fully visible.
Suicide pathways within each cluster
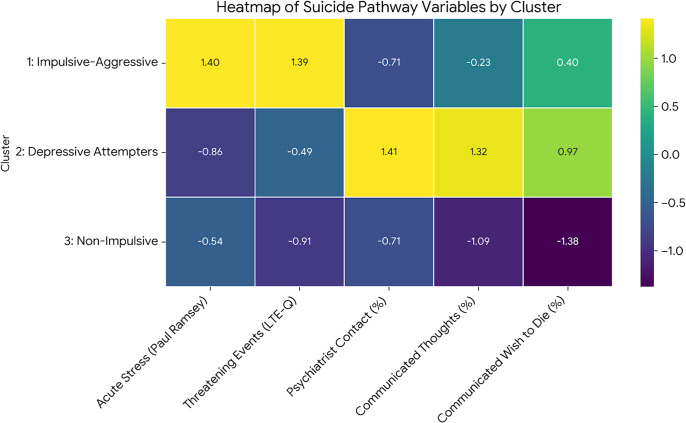
Distinct suicide pathways emerged following cluster identification. See Table 2 for full details and Figure 3 for a heatmap visualization of these pathways.
Table 2.
Suicide pathway between the clusters regarding events in the last year of life
| Distribution | Multinomial model | 1 vs. 2 | 1 vs. 3 | 2 vs. 3 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Impulsive-aggressive,N = 108 | Depressive prior attempters,N = 105 | Non-impulsive-aggressive,N = 178 | OR (CI)1 vs. 2 | OR (CI)1 vs. 3 | Global q-value a | q-value b | q-value b | q-value b | |
| Last year of life | |||||||||
| Holmes–Rahe Stress Scale | 174 (114) | 149 (87) | 149 (100) | 1.00, (0.99,1.00) | 1.00, (0.99,1.00) | 0.6 | >0.9 | 0.8 | >0.9 |
| Paul Ramsey Life Experience Scale | 11.6 (5.3) | 8.1 (4.6) | 8.6 (4.9) | 0.87, (0.83,0.93) | 0.89, (0.85,0.94) | <0.001 | <0.001 | <0.001 | >0.9 |
| LTE-Q | 1.79 (1.33) | 1.30 (1.02) | 1.19 (0.96) | 0.69, (0.53,0.88) | 0.62, (0.49,0.78) | <0.001 | 0.013 | <0.001 | >0.9 |
| Last 3 months of life | |||||||||
| Had contact with a healthcare professional | 82 (79%) | 85 (83%) | 130 (74%) | 1.34, (0.66,2.71) | 0.78, (0.43,1.38) | 0.3 | >0.9 | >0.9 | 0.3 |
| Had contact with a psychiatrist 3 months before | 19 (18%) | 50 (48%) | 32 (18%) | 4.26, (2.28,7.96) | 1.03, (0.55,1.92) | <0.001 | <0.001 | >0.9 | <0.001 |
| Communicated thoughts of suicide | 15 (14%) | 27 (26%) | 13 (7.3%) | 2.15, (1.07,4.32) | 0.49, (0.22,1.07) | <0.001 | 0.10 | 0.2 | <0.001 |
| Reported suicide intent | 12 (11%) | 20 (19%) | 10 (5.6%) | 1.88, (0.87,4.08) | 0.48, (0.20,1.14) | 0.011 | 0.3 | 0.3 | 0.002 |
| Last month of life | |||||||||
| Communicated a wish to die | 33 (48%) | 34 (56%) | 29 (23%) | 1.37, (0.69,2.74) | 0.33, (0.18,0.62) | <0.001 | >0.9 | 0.002 | <0.001 |
| Communicated their desire to die by suicide | 26 (38%) | 19 (31%) | 17 (14%) | 0.75, (0.36,1.55) | 0.28, (0.14,0.56) | 0.004 | >0.9 | 0.001 | 0.026 |
| Commented on any method of suicide | 18 (27%) | 14 (23%) | 14 (12%) | 0.83, (0.37,1.86) | 0.36, (0.17,0.79) | 0.054 | >0.9 | 0.032 | 0.14 |
| Gave a reason for taking their life | 21 (31%) | 22 (38%) | 21 (18%) | 1.37, (0.65,2.86) | 0.48, (0.24,0.97) | 0.031 | >0.9 | 0.13 | 0.012 |
| Last 2 weeks of life | |||||||||
| Kept an interest in their task | <0.001 | ||||||||
| All the time | 77 (85%) | 60 (66%) | 135 (93%) | — | — | — | — | — | |
| Nearly always- Rarely | 8 (8.8%) | 9 (9.9%) | 4 (2.8%) | 1.44, (0.53,3.97) | 0.29, (0.08,0.98) | >0.9 | 0.14 | 0.027 | |
| Never | 6 (6.6%) | 22 (24%) | 6 (4.1%) | 4.71, (1.79,12.3) | 0.57, (0.18,1.83) | 0.005 | >0.9 | <0.001 | |
| They were more irritable | 0.2 | ||||||||
| Was the same | 55 (75%) | 51 (74%) | 107 (85%) | — | — | — | — | — | |
| With everybody | 13 (18%) | 16 (23%) | 13 (10%) | 1.33, (0.58,3.03) | 0.51, (0.22,1.18) | >0.9 | 0.4 | 0.062 | |
| With some people | 5 (6.8%) | 2 (2.9%) | 6 (4.8%) | 0.43, (0.08,2.32) | 0.62, (0.18,2.11) | >0.9 | >0.9 | >0.9 | |
| They were angrier | 0.062 | ||||||||
| Was the same | 64 (77%) | 55 (73%) | 120 (88%) | — | — | — | — | — | |
| With everybody | 15 (18%) | 17 (23%) | 10 (7.4%) | 1.32, (0.60,2.88) | 0.36, (0.15,0.84) | >0.9 | 0.054 | 0.007 | |
| With some people | 4 (4.8%) | 3 (4.0%) | 6 (4.4%) | 0.87, (0.19,4.07) | 0.80, (0.22,2.94) | >0.9 | >0.9 | >0.9 | |
| Last week of life | |||||||||
| Communicated a wish to die | 24 (38%) | 31 (54%) | 23 (20%) | 1.99, (0.96,4.11) | 0.41, (0.21,0.81) | <0.001 | 0.2 | 0.030 | <0.001 |
| Communicated their desire to die by suicide | 21 (31%) | 16 (28%) | 15 (13%) | 0.85, (0.39,1.85) | 0.33, (0.16,0.69) | 0.020 | >0.9 | 0.011 | 0.055 |
| Commented on any method of suicide | 17 (26%) | 15 (26%) | 13 (11%) | 1.01, (0.45,2.25) | 0.36, (0.16,0.79) | 0.032 | >0.9 | 0.034 | 0.041 |
| Gave a reason for taking their life | 19 (29%) | 20 (36%) | 17 (15%) | 1.35, (0.63,2.89) | 0.42, (0.20,0.89) | 0.019 | >0.9 | 0.071 | 0.008 |
Abbreviations: CI, 95% confidence interval; LTE-Q, Life-Threatening Events Questionnaire; OR, odds ratio.
Note: Data in distribution columns are presented as n (%) for categorical variables and mean (SD) for continuous variables. Bold type indicates statistical significance at the q < .05 level.
q-values for the global multinomial model were adjusted using the false discovery rate (FDR) correction.
q-values for the pairwise comparisons were adjusted using the Bonferroni correction.
Figure 3.
Heatmap of suicide pathway variables by cluster. Note: LTE-Q, Life Threatening Events – Questionnaire. This heatmap visualizes the differences in key suicide pathway variables across the three clusters. The values shown are Z-scores, which represent for each variable how many standard deviations a cluster’s value is from the mean of all clusters. Positive values indicate a higher-than-average score for that variable, while negative values indicate a lower-than-average score. This allows for a direct comparison of the relative prominence of each pathway characteristic.
Cluster 1 (impulsive-aggressive) was notably distinguished by experiencing significantly higher acute life stress in the year preceding death compared to the other clusters.
Cluster 2 (depressive prior attempters) showed markedly greater contact with psychiatric services and more frequent communication of suicidal thoughts and intent to others in the 3 months before death, relative to the other groups.
In contrast, Cluster 3 (non-impulsive/aggressive cases with no prior attempts) communicated significantly less about their distress or suicidal plans in the period leading up to death, including being less likely to express a wish to die or suicidal intentions than the other clusters.
Sex-segregated analysis
Sex-segregated analyses revealed three male clusters (low, medium, and high impulsivity/aggression). The impulsive-aggressive cluster was highly stable, while the low-impulsivity cluster had more prior attempts, higher personality disorder prevalence, and depression at death.
Women formed two less distinct clusters (Figure 4), but impulsivity/aggression was linked to previous attempts and lower lethal intent (see Supplementary Material).
Figure 4.
Reorganization of cases in clusters following sex-segregated analysis. Note: C, Cluster. This alluvial plot illustrates the flow and reorganization of individuals from the initial three clusters (left nodes) into the new clusters derived from the subsequent sex-segregated analyses (right nodes). The blue bands represent male decedents, and the yellow bands represent female decedents. The plot shows that men were classified into three distinct clusters (Men clusters 1, 2, and 3), while women formed two less-differentiated clusters (Women clusters 1 and 2). The flow demonstrates the stability of certain profiles (e.g., Cluster 1 for men) and the redistribution patterns across the different subgroups.
In male clusters, the non-impulsive-aggressive group had more healthcare contact, suicidal communications, and anger expressions before death, unlike the medium-impulsivity cluster, where these were rare.
Among women, the most impulsive group communicated suicidal intent more often and showed greater anger expressions in the weeks before death than less impulsive/aggressive women (see Supplementary Material).
Discussion
This study aimed to characterize suicide decedents based on impulsivity and related factors. Our first hypothesis – expecting two groups (high versus low impulsivity) – was partially confirmed. Cluster 1 (impulsive-aggressive) matched expectations, showing high stability across the full sample and male subset. However, among low-impulsivity individuals, we identified two clusters: medium (Cluster 2) and low (Cluster 3) impulsivity, with greater differentiation in men. Both had high suicidal intent, comparable to Cluster 1. Contrary to expectations, depression was more prevalent in the medium-impulsivity cluster, especially in men. In women, clustering was less distinct, although impulsivity/aggression correlated with prior attempts and lower lethal intent.
Our second hypothesis – expecting distinct suicide pathways per cluster – was also partially confirmed. Cluster 1 experienced more negative life events in the year before death, particularly relationship, work, and financial issues. Among women, higher impulsivity was linked to more suicidal communications and anger expressions pre-death. Among men, suicidal communication and behavioural changes were consistent in high- and low-impulsivity clusters, while the medium-impulsivity cluster showed lower rates of both.
Cluster 1: Impulsive-aggressive substance abusers
A correlation exists between trait impulsivity and lifetime aggression across clusters, with Cluster 1 as the clearest example. This aligns with research linking impulsivity to risky behaviours, including aggression [55, 56]. Impulsivity has been proposed as an endophenotype associated with serotonergic and Hypothalamic-Pituitary-Adrenal axis dysfunction [57, 58], increasing risk for suicidal behaviour, personality disorders, and substance use [12], supporting Cluster 1’s structure.
Additionally, impulsivity/aggression negatively correlate with lethal intent, consistent with prior psychological autopsy studies [28, 29]. However, only extreme impulsivity lowers lethal intent, while medium and low impulsivity clusters show similarly high lethal intent scores.
Cluster 2: Depressive prior attempters
This cluster is primarily defined by suicide history: 80% had prior attempts, over half had two or more, and 75% experienced depression at death.
Notably, this cluster had a higher proportion of women, although men (one-third of the cluster) had the highest depression and attempt rates. Conversely, women showed greater behavioural changes in the 2 weeks pre-death, including reduced task interest, increased irritability, and anger (see Supplementary Material). Among impulsive women, these changes were more pronounced, with more frequent suicidal thoughts than their less impulsive counterparts.
This pattern in women’s suicides is significant. Anger expression carries higher social costs for women than men [59]. The high proportion of women displaying increased rage pre-suicide suggests a loss of emotional restraint, highlighting emotional dysregulation as a key factor, particularly in high-impulsivity women.
Cluster 3: Non-impulsive aggressive cases with no prior attempts
The emergence of Cluster 3, the largest profile in our sample, represents a significant challenge for suicide prevention. This profile is not merely defined by an absence of impulsivity or aggression; our data reveal its core characteristics. It is composed almost exclusively of males (99%) for whom the fatal act was their first suicide attempt (80% without prior attempts). Crucially, this profile combines a high, deliberate intent to die (as shown by SIS scores comparable to Cluster 2) with a profound lack of communication regarding this intent. This combination of high internal intentionality and a lack of external warning signs makes this group an empirical manifestation of a “silent” or “invisible” suicide pathway.
This finding is strongly supported by recent large-scale research, which has identified similar “invisible profiles” characterized by a lack of mental health contact and low rates of intent disclosure [60]. In fact, this aligns with foundational work by Logan et al. (2011), who were among the first to empirically identify a subgroup of suicide decedents with few traditional risk factors [61].
To understand the drivers of this silent distress, theoretical frameworks focusing on unbearable psychological pain, or psychache, may be more useful than traditional psychopathological models [62]. Furthermore, contemporary ideation-to-action frameworks, such as the Three-Step Theory, can help contextualize this pathway: a combination of pain and hopelessness may escalate suicidal desire, which then progresses to a lethal attempt in individuals with low social connectedness (reflected in their lack of communication) and high capability for suicide [63]. The importance of this “capability” component is underscored by recent findings showing that decedents using high-lethality methods were significantly less likely to have a history of mental health treatment seeking [64]. These theoretical lenses suggest that prevention for this group must expand beyond psychiatric screening to primary care and community settings to identify and alleviate the underlying sources of pain and isolation.
Gender-specific suicide pathways
Our findings revealed profound gender differences, suggesting distinct suicide pathways for men and women. The clusters showed a stark sex-based separation: Cluster 2 was predominantly female (82%), while Clusters 1 and 3 were almost exclusively male (93 and 99%, respectively). Furthermore, our sex-segregated analyses indicated that impulsivity and aggression served as clearer organizing principles for the male profiles than for the female profiles, suggesting that other factors may be more central to the suicide pathways of women.
The clinical and sociocultural implications of this are significant. The profile of women in Cluster 2, characterized by depression, prior attempts, and pre-death expressions of interpersonal conflict and anger, may reflect gender differences in expressing distress. This may reflect gender-specific pathways to suicide that emerge early in life; for instance, research in adolescents has shown that suicide risk in males is more strongly associated with externalizing behaviours like substance use and impulsivity (mirroring our Cluster 1), while in females, risk is more associated with internalizing symptoms like depression and poor emotional regulation (mirroring our Cluster 2) [65]. Furthermore, women’s internalizing symptoms may manifest as relational turmoil [66], which may explain the increase in anger expressions before death in Cluster 2. Acknowledging these gender-specific patterns of distress is crucial for improving both risk assessment and the therapeutic alliance.
Implications for further research
This study adds to the growing evidence identifying distinct suicide pathways. Our finding that Cluster 1 was characterized by the highest levels of recent life stressors provides a real-world psychosocial parallel to laboratory findings on biological stress reactivity. For instance, research using the Trier Social Stress Test has demonstrated that high-impulsivity suicide attempters exhibit greater cortisol reactivity [67]. This neurobiological hyper-reactivity may provide a potential mechanism explaining why individuals with an impulsive-aggressive profile are more susceptible to the impact of acute life stressors, which could precipitate a suicidal crisis. Our findings extend this literature, suggesting that impulsivity and aggression vary by sex – more distinct in men and more diffuse in women, indicating possible sex-related biological or psychosocial differences in impulsive suicide pathways.
Consistent with Bernanke et al., who identified stress-responsive and non-stress-responsive suicide attempters [32], our findings align Cluster 1 (impulsive-aggressive) with stress-responsive individuals and Cluster 2 (depressive attempters) with non-stress-responsive individuals. The sex-segregated analysis refines these subtypes: Women in Cluster 2 showed emotional reactivity (irritability and anger) pre-death, while men exhibited depression and prior attempts, aligning with the depressive diathesis model. A history of depression correlates with higher lethal intent and attempt severity [68], consistent with our results.
Cluster 3 lacked a distinct profile, which aligns with its low visibility – it does not stand out in personality, psychopathology, healthcare use, or suicidal communication. However, among men, this cluster split into two: (i) one with low impulsivity but prior depression and attempts, and (ii) another with medium impulsivity but minimal psychopathology. These subgroups highlight suicide risk among men who evade clinical detection.
This hidden group is challenging to identify, as clinical samples underrepresent them. Psychological autopsy is crucial for understanding suicide beyond clinical settings. Given this group’s size and invisibility, further research must examine stressors and life experiences contributing to suicidality, considering sex-specific differences. Community-based strategies, rather than sole reliance on clinical indicators, are essential for detecting individuals at risk.
Implications for clinical practice
Our findings, by identifying three distinct profiles of suicide decedents, underscore the need for tailored prevention strategies and help explain the limited sensitivity of some universal risk assessment tools [31]. While traditional risk factors like prior attempts may help identify individuals similar to Cluster 2, they are likely to be less effective for the “impulsive-aggressive” (Cluster 1) and, most notably, the large “non-impulsive” (Cluster 3) profiles.
The profile of Cluster 1 aligns with literature identifying impulsivity, aggression, and substance use as key risks, particularly in male suicides [22] and those with Cluster B traits [23]. This suggests that prevention for this group may require interventions focused on stress management and dual diagnosis. Furthermore, the externalizing behaviours in this profile may undermine the benefits of traditional social support [69], indicating that perceived support, rather than simple social contact, is a more crucial target for intervention prevention [70].
In contrast, Cluster 2 was predominantly female, and its profile, characterized by hostility and interpersonal conflict before death, mirrors findings in depressed women [36]. A key clinical implication arises from the paradox that while this group had high healthcare engagement, they showed very low rates of receiving specific evidence-based treatments. This suggests that for individuals with this profile, prevention strategies must address significant barriers to effective care, such as stigma or fear of negative consequences [71, 72].
Furthermore, women in our Clusters more likely exhibited interpersonal conflict and anger before death than their male counterparts. These observations suggest that certain signs may indicate elevated suicide risk in a gender-specific manner.
Finally, the large “non-impulsive” Cluster 3 poses a unique prevention challenge due to its lack of clear psychopathology or classic warning signs. The “invisible” nature of this group highlights the necessity of developing community-based detection strategies and underscores the need for research that extends beyond clinical samples to better understand the environmental stressors and social determinants that contribute to suicide in this large population. The existence of these distinct groups generates testable hypotheses for future research on the differential effectiveness of interventions across these different suicide phenotypes. This includes therapies such as cognitive behavioural therapy, which targets the maladaptive cognitions that may be prominent in depressive profiles like our Cluster 2, and dialectical behaviour therapy, which focuses on emotional dysregulation and distress tolerance, core features of the impulsive-aggressive profile seen in our Cluster 1 [73].
Strengths and limitations
This study’s strengths lie in its methodological approach, particularly cluster analysis, where variables were rationally selected based on a prior systematic review [33] . This enabled the identification of distinct suicide profiles, offering a nuanced understanding of suicide pathways. The three-cluster model underscores suicidal heterogeneity, aiding tailored prevention strategies. Findings align with literature on impulsivity, aggression, and suicidal behaviour, reinforcing result validity and reliability.
However, limitations exist. The retrospective design and reliance on psychological autopsies may introduce several potential biases. Beyond simple recall bias, our data are also subject to informant bias, as next-of-kin may not have been aware of all aspects of the decedent’s life (e.g., private help-seeking behaviours), and hindsight bias, where knowledge of the suicide may have influenced the informant’s retrospective appraisal of the decedent’s state of mind. Furthermore, a key limitation is the absence of a non-suicide decedent comparison group. Consequently, our findings are relative and describe differences between profiles of suicide decedents, but they cannot be used to identify factors that discriminate individuals who die by suicide from those who do not.
While psychological autopsy is validated [74, 75], its inability to establish causality limits understanding of suicide mechanisms. Another limitation of our study is the exclusion of detailed data on medical comorbidities and full pharmacological histories from the clustering model. While some healthcare variables were described, they were not used to define the profiles. Future research should incorporate this data to provide a more refined understanding of the identified suicide pathways.
Conclusions
This study identified three suicide clusters, revealing differences in impulsivity and related factors. While the impulsive-aggressive cluster was expected, two additional medium- and low-impulsivity clusters emerged, both with high suicidal intent. Unexpectedly, the medium-impulsivity cluster was linked to depression and prior attempts.
Sex-segregated analysis showed men in the impulsive-aggressive cluster had substance use disorders, while women displayed interpersonal conflict and anger pre-death. In medium- and low-impulsivity clusters, women showed mood/behavioural changes, while low-impulsivity men had depression and prior attempts.
Findings stress the need for tailored suicide prevention and community-based research, particularly for the largest, least understood group, which lacks clear psychopathology or healthcare engagement. This approach could enhance suicide prevention strategies.
Supporting information
Sanz-Gomez et al. supplementary material
Acknowledgments
The authors would like to thank all participants who were interviewed about their close ones during the psychological autopsy procedure. The authors would also like to thank the staff at the Instituto de Medicina Legal and the Instituto Anatómico Forense of Seville who participated in the FRienDS project, as well as the research personnel who carried out the psychological autopsies.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1192/j.eurpsy.2025.10070.
Data availability statement
The data that support the findings of this study are not publicly available due to their sensitive nature and ethical restrictions related to participant privacy and confidentiality.
Financial support
Sergio Sanz-Gómez’s work is supported by the VI-PPITUS (Universidad de Sevilla).
Competing interests
The authors declare none.
References
- [1].GBD 2021. Suicide collaborators. Global, regional, and national burden of suicide, 1990–2021: A systematic analysis for the global burden of disease study 2021. Lancet Public Health. 2025; 10:e189–202. 10.1016/S2468-2667(25)00006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Turecki G, Brent DA, Gunnell D, O’Connor RC, Oquendo MA, Pirkis J, et al. Suicide and suicide risk. Nat Rev Dis Prim. 2019;5 10.1038/s41572-019-0121-0. [DOI] [PubMed] [Google Scholar]
- [3].Sutar R, Kumar A, Yadav V. Suicide and prevalence of mental disorders: A systematic review and meta-analysis of world data on case-control psychological autopsy studies. Psychiatry Res. 2023;329:115492 10.1016/j.psychres.2023.115492. [DOI] [PubMed] [Google Scholar]
- [4].Cho SEJ, Na KS, Cho SEJ, Im JS, Kang SG. Geographical and temporal variations in the prevalence of mental disorders in suicide: Systematic review and meta-analysis. J Affect Disord. 2016;190:704–13. 10.1016/j.jad.2015.11.008. [DOI] [PubMed] [Google Scholar]
- [5].Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Jaroszewski AC, et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 2017;143:187–232. 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- [6].de la Torre-Luque A, Pemau A, Ayad-Ahmed W, Borges G, Fernandez-Sevillano J, Garrido-Torres N, et al. Risk of suicide attempt repetition after an index attempt: A systematic review and meta-analysis. Gen Hosp Psychiatry. 2023;81:51–6. 10.1016/j.genhosppsych.2023.01.007. [DOI] [PubMed] [Google Scholar]
- [7].Barker J, Oakes-Rogers S, Leddy A. What distinguishes high and low-lethality suicide attempts in older adults? A systematic review and meta-analysis. J Psychiatr Res. 2022;154:91–101. 10.1016/j.jpsychires.2022.07.048. [DOI] [PubMed] [Google Scholar]
- [8].Wilson MM, Pollock NJ, Power ND, Karaivanov Y, Mulay S, Reccord C. Sex differences in suicide mortality in Newfoundland and Labrador: An observational study with medical examiner data from 1997 to 2016. Heal Reports. 2022;33:31–8. 10.25318/82-003-x202200800003-eng. [DOI] [PubMed] [Google Scholar]
- [9].McQuaid RJ, Nikolitch K, Vandeloo KL, Burhunduli P, Phillips JL. Sex differences in determinants of suicide risk preceding psychiatric admission: An electronic medical record study. Front Psych. 2022;13:1–9. 10.3389/fpsyt.2022.892225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Fowler KA, Kaplan MS, Stone DM, Zhou H, Stevens MR, Simon TR. Suicide among males across the lifespan: An analysis of differences by known mental health status. Am J Prev Med. 2022;63:419–22. 10.1016/j.amepre.2022.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].O’Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1:73–85. 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- [12].Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;19:1227–39. 10.1016/S0140-6736(15)00234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chachamovich E, Kirmayer LJ, Haggarty JM, Cargo M, McCormick R, Turecki G. Suicide among Inuit: Results from a large, epidemiologically representative follow-back study in Nunavut. Can J Psychiatr. 2015;60:268–75. 10.1177/070674371506000605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gao Q, Zhang J, Jia C. Psychometric properties of the Dickman impulsivity instrument in suicide victims and living controls of rural China. J Affect Disord. 2011;132:368–74. 10.1016/j.jad.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Law YW, Yip PSF, Zhang Y, Caine ED. The chronic impact of work on suicides and under-utilization of psychiatric and psychosocial services. J Affect Disord. 2014;168:254–61. 10.1016/j.jad.2014.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lin L, Zhang J, Zhou L, Jiang C. The relationship between impulsivity and suicide among rural youths aged 15-35 years: A case-control psychological autopsy study. Pyschological Heal Med. 2016;21:330–7. 10.1080/13548506.2015.1051555.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lu CF, Jia CX, Xu AQ, Dai AY, Qin P. Psychometric characteristics of Chinese version of Barratt impulsiveness scale-11 in suicides and living controls of rural China. Omega (United States). 2012;66:215–29. 10.2190/OM.66.3.b. [DOI] [PubMed] [Google Scholar]
- [18].Niu L, Ma Z, Jia C, Zhou L. Gender-specific risk for late-life suicide in rural China: A case-control psychological autopsy study. Age Ageing. 2020; 10.1093/ageing/afaa036. [DOI] [PubMed] [Google Scholar]
- [19].Sun L, Zhang J. Characteristics of Chinese rural young suicides: Who did not have a strong intent to die. Compr Psychiatry. 2015;57:73–8. 10.1016/j.comppsych.2014.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Zhang J, Wieczorek W, Conwell Y, Tu XM, Wu BYW, Xiao S, et al. Characteristics of young rural Chinese suicides: A psychological autopsy study. Psychol Med. 2010;40:581–9. 10.1017/S0033291709990808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhang J, Lin L. The moderating effects of impulsivity on Chinese rural young suicide. J Clin Psychol. 2014;70:579–88. 10.1002/jclp.22039. [DOI] [PubMed] [Google Scholar]
- [22].Dumais A, Lesage AD, Alda M, Rouleau G, Dumont M, Chawky N, et al. Risk factors for suicide completion in major depression: A case-control study of impulsive and aggressive behaviors in men. Am J Psychiatry. 2005;162:2116–24. 10.1176/appi.ajp.162.11.2116. [DOI] [PubMed] [Google Scholar]
- [23].McGirr A, Paris J, Lesage A, Renaud J, Turecki G. Risk factors for suicide completion in borderline personality disorder: A case-control study of cluster B comorbidity and impulsive aggression. J Clin Psychiatry. 2007;68:721–9. 10.4088/jcp.v68n0509. [DOI] [PubMed] [Google Scholar]
- [24].Ross V, Kõlves K, De-Leo D. Beyond psychopathology: A case – control psychological autopsy study of young adult males. Int J Soc Psychiatry. 2017;63:151–60. 10.1177/0020764016688041. [DOI] [PubMed] [Google Scholar]
- [25].McGirr A, Séguin M, Renaud J, Benkelfat C, Alda M, Turecki G. Gender and risk factors for suicide: Evidence for heterogeneity in predisposing mechanisms in a psychological autopsy study. J Clin Psychiatry. 2006;67:1612–7. [DOI] [PubMed] [Google Scholar]
- [26].Giner L, Blasco-Fontecilla H, Mercedes Perez-Rodriguez M, Garcia-Nieto R, Giner J, Guija JA, et al. Personality disorders and health problems distinguish suicide attempters from completers in a direct comparison. J Affect Disord. 2013;151:474–83. 10.1016/j.jad.2013.06.029. [DOI] [PubMed] [Google Scholar]
- [27].Zouk H, Tousignant M, Seguin M, Lesage A, Turecki G. Characterization of impulsivity in suicide completers: Clinical, behavioral and psychosocial dimensions. J Affect Disord. 2006;92:195–204. 10.1016/j.jad.2006.01.016. [DOI] [PubMed] [Google Scholar]
- [28].Shelef L, Korem N, Yavnai N, Yedidya R, Ginat K, Shahar G, et al. Depression and impulsiveness among soldiers who died by suicide: A psychological autopsy study. J Affect Disord. 2018;235:341–7. 10.1016/j.jad.2018.04.068. [DOI] [PubMed] [Google Scholar]
- [29].Lin L, Zhao S, Zhang J. Impulsivity kills some who did not plan to die by suicide: Evidence from Chinese rural youths. Omega – J Death Dying. 2019;79:446–60. 10.1177/0030222818786417. [DOI] [PubMed] [Google Scholar]
- [30].Gomez SH, Overholser J, McGovern C, Silva C, Stockmeier CA. The role of premeditation in suicide: Identifying factors associated with increased planning among suicide decedents. J Clin Psychol. 2023;79:2768–80. 10.1002/jclp.23577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Runeson B, Odeberg J, Pettersson A, Edbom T, Adamsson IJ, Waern M. Instruments for the assessment of suicide risk: A systematic review evaluating the certainty of the evidence. PLoS One. 2017;12:1–13. 10.1371/journal.pone.0180292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Bernanke JA, Stanley BH, Oquendo MA. Toward fine-grained phenotyping of suicidal behavior: The role of suicidal subtypes. Mol Psychiatry. 2017;22:1080–1. 10.1038/mp.2017.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Sanz-Gómez S, Vera-Varela C, Alacreu-Crespo A, Perea-González MI, Guija JA, Giner L. Impulsivity in fatal suicide behaviour: A systematic review and meta-analysis of psychological autopsy studies. Psychiatry Res. 2024;337:1–12. 10.1016/j.psychres.2024.115952. [DOI] [PubMed] [Google Scholar]
- [34].Aaltonen K, Sund R, Hakulinen C, Pirkola S, Isometsä E. Variations in suicide risk and risk factors after hospitalization for depression in Finland, 1996-2017. JAMA Psychiatry. 2024;81:506–15. 10.1001/jamapsychiatry.2023.5512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Athey A, Overholser J, Bagge C, Dieter L, Vallender E, Stockmeier CA. Risk-taking behaviors and stressors differentially predict suicidal preparation, non-fatal suicide attempts, and suicide deaths. Psychiatry Res. 2018;270:160–7. 10.1016/j.psychres.2018.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Dalca IM, McGirr A, Renaud J, Turecki G. Gender-specific risk factors for suicide in major depressive disorder. J Clin Psychiatry. 2013;74:1209–16. 10.4088/JCP.12m08180. [DOI] [PubMed] [Google Scholar]
- [37].de la Vega D, Guija JA, Pérez-Moreno P, Kelly SA, Santos M, Oquendo MA, et al. Association of Religious Activity with male suicide deaths. Suicide Life-Threatening Behav 2020;50:449–60. 10.1111/sltb.12600. [DOI] [PubMed] [Google Scholar]
- [38].Giner L. Diferencias en la conducta suicida. Estudio comparativo entre los intentos de suicidio y suicidio consumado. [PhD Thesis] Madrid, Spain: Universidad Autónoma de Madrid; 2010. [Google Scholar]
- [39].First MB, Spitzer RL, Gibbon M, Williams JBW, others. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. New York; NY: New York Biometrics Res Dep New York State Psychiatr Inst; 2002. [Google Scholar]
- [40].First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured clinical interview for DSM-IV-TR Axis II personality disorders (SCID-II) version 2.0. New York; NY: New York Biometrics Res Dep New York State Psychiatr Inst; 1994. [Google Scholar]
- [41].Patton JH, Stanford M, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74. 10.1002/1097-4679(199511)51:63.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- [42].Oquendo MA, Baca-Garcia E, Graver R, Morales M, Montalvan V, Mann JJ. Spanish adaptation of the Barratt impulsiveness scale (BIS-11). Eur J Psychiatry. 2001;15:147–55. [Google Scholar]
- [43].Brown GL, Goodwin FK. Cerebrospinal fluid correlates of suicide attempts and aggression. Ann N Y Acad Sci. 1986;487:175–88. 10.1111/j.1749-6632.1986.tb27897.x. [DOI] [PubMed] [Google Scholar]
- [44].Coccaro EF, Berman ME, Kavoussi RJ. Assessment of life history of aggression: Development and psychometric characteristics. Psychiatry Res. 1997;73:147–57. 10.1016/S0165-1781(97)00119-4. [DOI] [PubMed] [Google Scholar]
- [45].Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The scale for suicide ideation. J Consult Clin Psychol. 1979;47:343–52. 10.1037/0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- [46].Diaz FJ, Baca-Garcia E, Diaz-Sastre C, García Resa E, Blasco H, Braquehais Conesa D, et al. Dimensions of suicidal behavior according to patient reports. Eur Arch Psychiatry Clin Neurosci. 2003;253:197–202. 10.1007/s00406-003-0425-6. [DOI] [PubMed] [Google Scholar]
- [47].Paykel ES. Methodological aspects of life events research. J Psychosom Res. 1983;27:341–52. 10.1016/0022-3999(83)90065-X. [DOI] [PubMed] [Google Scholar]
- [48].Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967;11:213–8. 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- [49].González de Rivera J, Morera Fumero A. La valoración de sucesos vitales: Adaptación Española de la escala de Holmes y Rahe. Psiquis (Mexico). 1983;4:7–11. [Google Scholar]
- [50].Brugha T, Bebbington P, Tennant C, Hurry J. The list of threatening experiences: A subset of 12 life event categories with considerable long-term contextual threat. Psychol Med. 1985;15:189–94. [DOI] [PubMed] [Google Scholar]
- [51].Motrico E, Moreno-Küstner B, De Dios Luna J, Torres-González F, King M, Nazareth I, et al. Psychometric properties of the list of threatening experiences-LTE and its association with psychosocial factors and mental disorders according to different scoring methods. J Affect Disord. 2013;150:931–40. 10.1016/j.jad.2013.05.017. [DOI] [PubMed] [Google Scholar]
- [52].R Core Team. R: a Language and Environment for Statistical Computing [Computing Software]. Vienna, Austria: R Found Stat Comput; 2024. [Google Scholar]
- [53].Fryda T, LeDell E, Gill N, Aiello S, Fu A, Candel A, et al. h2o: R Interface for the “H2O” Scalable Machine Learning Platform. Vienna, Austria: R Found Stat Comput; 2024. [Google Scholar]
- [54].Hennig C. FPC: Flexible Procedures for Clustering. R package version 2.2–13. Vienna, Austria: R Found Stat Comput; 2024. [Google Scholar]
- [55].Joiner T. Why People Die by Suicide: Further Development and Tests of the Interpersonal-Psychological Theory of Suicidal Behavior. Cambridge, MA: Harvard University Press; 2012. [Google Scholar]
- [56].Gvion Y, Apter A. Aggression, impulsivity, and suicide behavior: A review of the literature. Arch Suicide Res. 2011;15:93–112. 10.1080/13811118.2011.565265. [DOI] [PubMed] [Google Scholar]
- [57].Jimenez-Treviño L, Blasco-Fontecilla H, Braquehais MD, Ceverino-Dominguez A, Baca-Garcia E. Endophenotypes and suicide behaviour. Actas Esp Psiquiatr. 2011;39:61–9. [PubMed] [Google Scholar]
- [58].Gould TD, Georgiou P, Brenner LA, Brundin L, Can A , Courtet P, et al. Animal models to improve our understanding and treatment of suicidal behavior. Transl Psychiatry 2017;7. 10.1038/tp.2017.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Van Doren N, Soto JA. Paying the price for anger: Do women bear greater costs? Int J Psychol. 2021;56:331–7. 10.1002/ijop.12724. [DOI] [PubMed] [Google Scholar]
- [60].Xiao Y, Bi K, Yip PSF, Cerel J, Brown TT, Peng Y, et al. Decoding suicide decedent profiles and signs of suicidal intent using latent class analysis. JAMA Psychiatry. 2024;81:595–605. 10.1001/jamapsychiatry.2024.0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Logan J, Hall J, Karch D. Suicide categories by patterns of known risk factors: A latent class analysis. Arch Gen Psychiatry. 2011;68:935–41. 10.1001/archgenpsychiatry.2011.85. [DOI] [PubMed] [Google Scholar]
- [62].Verrocchio MC, Carrozzino D, Marchetti D, Andreasson K, Fulcheri M, Bech P. Mental pain and suicide: A systematic review of the literature. Front Psych. 2016;7. 10.3389/fpsyt.2016.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. 2016;12:307–30. 10.1146/annurev-clinpsy-021815-093204. [DOI] [PubMed] [Google Scholar]
- [64].Bond AE, Bandel SL, Rodriguez TR, Anestis JC, Anestis MD. Mental health treatment seeking and history of suicidal thoughts among suicide decedents by mechanism, 2003-2018. JAMA Netw Open. 2022;5:1–9. 10.1001/jamanetworkopen.2022.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Keyes KM, Platt JM. Annual research review: Sex, gender, and internalizing conditions among adolescents in the 21st century – Trends, causes, consequences. J Child Psychol Psychiatry Allied Discip. 2024;65:384–407. 10.1111/jcpp.13864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Nolen-Hoeksema S. Emotion regulation and psychopathology: The role of gender. Annu Rev Clin Psychol. 2012;8:161–87. 10.1146/annurev-clinpsy-032511-143109. [DOI] [PubMed] [Google Scholar]
- [67].Alacreu-Crespo A, Hidalgo V, Girod C, Olié E, Courtet P. The impulsiveness level influences the salivary cortisol response and social stress sensitivity in suicidal patients. J Psychiatr Res. 2022;156:159–67. 10.1016/j.jpsychires.2022.10.008. [DOI] [PubMed] [Google Scholar]
- [68].Mann JJ, Malone KM. Cerebrospinal fluid amines and higher-lethality suicide attempts in depressed inpatients. Biol Psychiatry. 1997;41:162–71. 10.1016/S0006-3223(96)00217-X. [DOI] [PubMed] [Google Scholar]
- [69].Zhang J, Lin L. The moderating effect of social support on the relationship between impulsivity and suicide in rural China. Community Ment Health J. 2015;51:585–90. 10.1007/s10597-014-9811-y. [DOI] [PubMed] [Google Scholar]
- [70].Mueller NE, Duffy ME, Stewart RA, Joiner TE, Cougle JR. Quality over quantity? The role of social contact frequency and closeness in suicidal ideation and attempt. J Affect Disord. 2022;298:248–55. 10.1016/j.jad.2021.10.065. [DOI] [PubMed] [Google Scholar]
- [71].Weng SC, Chang JC, Yeh MK, Wang SM, Chen YH. Factors influencing attempted and completed suicide in postnatal women: A population-based study in Taiwan. Sci Rep. 2016;6:1–9. 10.1038/srep25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Augsberger A, Yeung A, Dougher M, Hahm HC. Factors influencing the underutilization of mental health services among Asian American women with a history of depression and suicide. BMC Health Serv Res. 2015;15:1–11. 10.1186/s12913-015-1191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. 2016;3:646–59. 10.1016/S2215-0366(16)30030-X. [DOI] [PubMed] [Google Scholar]
- [74].Schneider B, Maurer K, Sargk D, Heiskel H, Weber B, Frölich L, et al. Concordance of DSM-IV Axis I and II diagnoses by personal and informant’s interview. Psychiatry Res. 2004;127:121–36. 10.1016/j.psychres.2004.02.015. [DOI] [PubMed] [Google Scholar]
- [75].Sanz-Gómez S, Alacreu-Crespo A, Guija JA, Giner-Jiménez L. Reliability and validity of proxy reports of impulsivity and aggression: An evidence-based assessment approach to psychological autopsy methods. Spanish J Psychiatry Ment Heal. 2023; 10.1016/j.sjpmh.2023.10.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sanz-Gomez et al. supplementary material
Data Availability Statement
The data that support the findings of this study are not publicly available due to their sensitive nature and ethical restrictions related to participant privacy and confidentiality.