Abstract
Background
Pericardial cysts are rare, affecting 1 in 100,000 people and affecting both males and females equally.
Case Summary
We present the atypical presentation of a progressive, left-sided pericardial cyst. The patient underwent surgical resection with recurrence within 5 months.
Discussion
The rarity of pericardial cysts and their predominantly right-sided location highlight the unusual nature of this case, compounded by the lack of understanding regarding factors contributing to cyst growth and recurrence. This case also raises the question of whether incomplete excision increases the risk of recurrence.
Key Words: atypical, cyst, pericardial, recurrence, resection
Visual Summary

History of Presentation
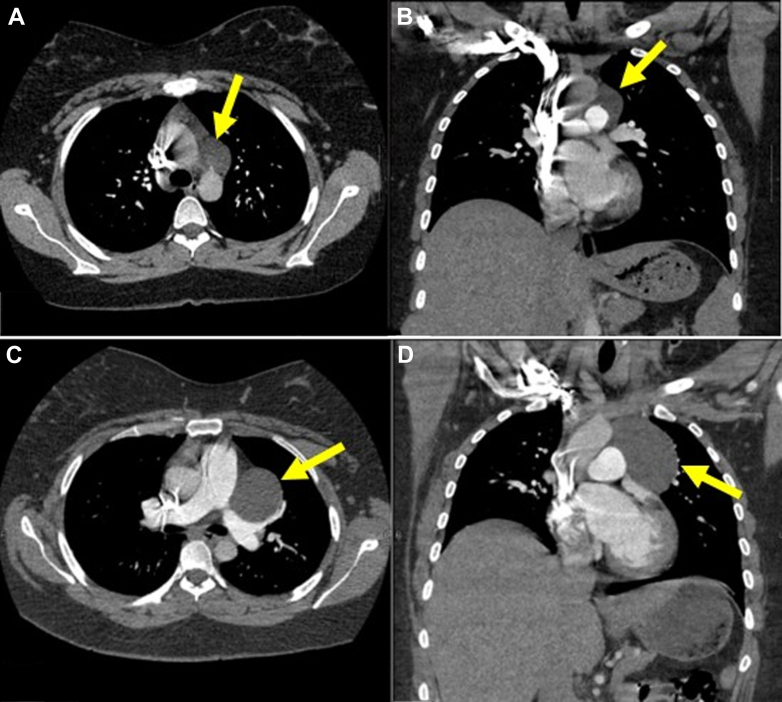
A 21-year-old woman presented to the emergency department in August 2018 with chest pain and dyspnea. Her vital signs were within normal limits, and she had negative coronary ischemia, pulmonary embolism, and infection work-ups. The laboratory results, including troponin and erythrocyte sedimentation rate, were within normal limits. However, the chest computed tomography angiography (CTA) at the time revealed a low-density mass approximately 3.6 cm × 2.1 cm in size in the aortopulmonary window region (Figures 1A and 1B). At the time, the patient’s symptoms seemed to be musculoskeletal because they were reproducible with palpation. She was advised to take ibuprofen, was discharged, and was lost to follow-up evaluation.
Take-Home Messages
-
•
There are few documented cases of pericardial cyst recurrence after surgical resection, and currently there are no data to suggest the recurrence rate after any intervention except for percutaneous aspiration or ethanol sclerosis.
-
•
Most pericardial cysts are found incidentally on imaging, and symptoms and/or cyst growth with nearby compression may be indications for surgery if complete excision is possible.
Figure 1.
CT Angiography Imaging
(A) Axial and (B) coronal views of the chest via computed tomography angiogram from August 2018 showing a low-density mass approximately 3.6 cm × 2.1 cm in size in the aortopulmonary window region (yellow arrows). Axial (C) and coronal (D) views of the chest via computed tomography angiogram from January 2024 revealing the same indeterminate low-density mass within the anterior mediastinum now increased in size, measuring approximately 6.3 cm × 5.4 cm (yellow arrows).
Five years later, the patient was seen in the same emergency department reporting sharp, nonexertional chest pain. A repeat chest CTA revealed the same indeterminate, low-density mass within the anterior mediastinum but now increased in size, measuring approximately 6.3 cm × 5.4 cm (Figures 1C and 1D). Given this interval increase in cystic size along with the possible associated symptoms, thoracic surgery was consulted.
Past Medical History
The patient had a past medical history of polycystic ovary syndrome (PCOS), cholecystectomy, and cesarean delivery. She also had a pertinent family history of pericardial effusion in her mother, the source of which was never elucidated.
Differential Diagnosis
The differential diagnosis included pericardial cyst, bronchogenic cyst, mediastinal teratoma, pericardial diverticulum, and thymic cyst.
Investigations
Chest magnetic resonance imaging (MRI) with and without contrast (Figure 2) revealed a thin-walled cystic mass abutting the superior margin of the left ventricle, main pulmonary artery segment, and left pulmonary artery measuring 5.8 cm × 4.8 cm × 7.6 cm. There was no associated solid mass component or abnormal enhancement, mediastinal lymphadenopathy, or pericardial effusion. The findings were most consistent with a pericardial cyst.
Figure 2.
MR Imaging
(A) Axial T2, (B) axial T1 precontrast, (C) coronal T2, and (D) axial postcontrast T1 views of the chest via magnetic resonance imaging in February 2024 revealing a thin-walled simple cystic mass abutting the superior margin of the left ventricle, main pulmonary artery segment, and left pulmonary artery measuring 5.8 cm × 4.8 cm × 7.6 cm (yellow arrows). There is no associated solid mass component or abnormal enhancement, mediastinal lymphadenopathy, or pericardial effusion. These findings are most consistent with a pericardial cyst.
Management
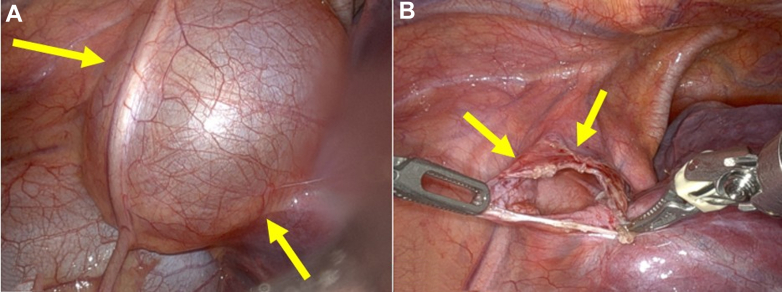
The patient consented to robotic-assisted left mediastinal cyst resection with diagnostic bronchoscopy in February 2024. During the procedure, a cystic structure was visualized to be subparietal pleural. This structure was opened between the phrenic nerve and the superior pulmonary vein, and the fluid was collected for cytology. Next, a vertical incision with the Maryland bipolar dissector was made along the entire length of the cyst, and the inner cyst sac wall was peeled out. A large portion of the lateral cyst wall was removed while leaving the phrenic nerve intact. The pulmonary artery and superior pulmonary vein were visualized easily through the medial attached cyst wall and were left intact. There was likely residual cyst wall tissue along the posterior pedicle of the phrenic nerve, aorta, superior left pulmonary vein, and the main pulmonary artery extending onto the left main pulmonary artery (Figure 3).
Figure 3.
Intraoperative Imaging
(A) Presurgical and (B) postsurgical images of the pericardial cyst resection performed in February 2024. There was likely residual cyst wall along the posterior pedicle of the phrenic nerve, aorta, superior left pulmonary vein, and the main pulmonary artery extending onto the left main pulmonary artery seen in image B (yellow arrows).
Tissue samples were collected and sent to pathology (Table 1). The excised mediastinal cyst tissue was consistent with benign fibrous tissue, and the cyst fluid was consistent with benign mesothelium without malignant cells. A station #10R lymph node along the superior pulmonary vein was collected and found to be benign.
Table 1.
Robotic-Assisted Left Mediastinal Cyst Resection With Diagnostic Bronchoscopy: Equipment List
|
|
|
|
Outcome and Follow-Up
Five months after surgical resection of the cyst, the patient returned for outpatient follow-up complaining of intermittent, nonexertional chest pain and palpitations. Repeat chest CT without contrast (Figure 4) revealed interval recurrence of the pericardial cyst in a similar location in the anterior mediastinum abutting the superior margin of the left ventricle, main pulmonary artery, and anterior margin of the left pulmonary artery. The cystic structure measured approximately 5.6 cm × 4.1 cm × 5.7 cm, almost identical in size to the original cyst that was resected. There was no sizable pleural or pericardial effusion.
Figure 4.
Postsurgical CT Imaging
(A) Axial and (B) coronal views of the chest via computed tomography imaging without contrast from September 2024 showing interval recurrence of the pericardial cyst in a similar location in the anterior mediastinum abutting the superior margin of the left ventricle, main pulmonary artery, and anterior margin of the left pulmonary artery (yellow arrows). The cystic structure measured approximately 5.6 cm × 4.1 cm × 5.7 cm.
The patient was referred to cardiology for further work-up of her new-onset palpitations and recurrent cyst. Echocardiogram showed normal left ventricular systolic function with ejection fraction > 55% and no valvular dysfunction. Holter monitor revealed no significant arrhythmia. Her symptoms of palpitations were thought to be unrelated to the pericardial cyst because the imaging did not suggest compression of nearby structures.
After extensive discussion with cardiology and thoracic surgery, the decision was made to not pursue further surgical intervention of the recurrent pericardial cyst given the risk of injury to the phrenic nerve, recurrent laryngeal nerve, pulmonary artery, and thoracic duct, and lack of compression of nearby structures. The patient will continue to follow with cardiology and thoracic surgery for interval imaging every 12 months. The institutional review board at Fulton County Medical Center did not approve this study because it was not required, and the patient provided informed written consent for publication.
Discussion
With the majority of pericardial cysts presenting asymptomatically (50%-75%), they are often found incidentally on radiographic imaging. Estimated at an incidence of 1 in every 100,000 people and affecting both males and females equally, the condition is exceedingly rare.1 The pathophysiology of their development is predominantly congenital in origin, stemming from a failure of fusion of one of the mesenchymal lacunae that form the pericardial sac. The cyst itself is benign and consists of 1 layer of mesothelial cells, encapsulating serous fluid that communicates with the pericardial space.2 However, inflammatory responses brought about by various conditions including tuberculosis, rheumatic pericarditis, trauma, and cardiac surgery are hypothesized secondary etiologies of pericardial cysts.3
One retrospective observational study following 103 patients with confirmed pericardial cysts found that cysts most often regressed in size or remained the same; the cysts that grew required only continued monitoring due to asymptomatic patient presentations.4
Anatomically, the preponderance of pericardial cysts originate at the right costophrenic angle (70%) with less common presentation at the left costophrenic angle and posterior or anterior-superior aspect of the mediastinum.1 Symptomatic presentation is based on the compressive force of surrounding structures. Because of this, the symptoms vary widely and may include chest pain, dyspnea, palpitations, infection, pericardial effusion, chronic cough, and arrhythmias.1,4
When a cyst is identified on radiographic findings, evaluation and management are conducted through a systematic approach that first assesses the shape, size, location, and presentation.1 Frequently the mass is discovered on chest X-ray, but CT scans are considered to be the best imaging modality in diagnosis.3,4 MRI T2 weighted diffusion is useful in assessing the contents of the cyst as well as the level of compression on surrounding structures.
Asymptomatic patients are treated conservatively with serial cross-sectional imaging to assess the change of size of the cyst as well as monitoring for mechanical sequelae. Symptomatic patients or patients with greater chances of complications are often treated initially with percutaneous aspiration or ethanol sclerosis with a recurrence rate of 25%-33%.1 If the cyst recurs, surgical resection is considered, but the decision is based on severity of symptoms and risk of procedure as well as the potential success of the procedure.
In light of our patient’s initial presentation with increasing cyst size and possible symptoms related to the cyst, the decision was made to resect her pericardial cyst. Five months after surgery, imaging revealed recurrence of the pericardial cyst in the same location and essentially the same size. Incomplete excision may have led to early recurrence in this case. After recurrence, it was felt that the patient’s symptoms were likely not related to the cyst. Given further imaging suggesting that complete excision of the cyst would potentially injure nearby structures, repeat surgery was not recommended. The patient now thankfully reports no symptoms.
At the time of this case report, only 2 other recurrences of surgically resected pericardial cysts had been documented.2,5 This supports the notion that resection is highly effective in treating symptomatic cysts but also indicates the factors contributing to cyst recurrence are not fully understood. Our patient’s cyst recurrence within 5 months after surgical resection was considerably more rapid than in previous patients. Moreso, the cyst’s delicate location abutting the superior margin of the left ventricle, main pulmonary artery, and anterior margin of the left pulmonary artery and phrenic nerve presents significant surgical risk. The current literature is lacking on identifying the factors that determine recurrence of pericardial cysts. Additionally, this patient has a history of PCOS, which potentially may contribute to the development of cysts although there have been no documented reports or studies to support this hypothesis.
This case raises suspicion that the inability to fully resect the cyst tissue may have contributed to the repeat occurrence. In this way, optimal imaging to assess the possibility of complete resection should be considered before proceeding with surgery.
Conclusions
We present the atypical presentation of a progressive, left-sided pericardial cyst. The cyst was resected but completely recurred within 5 months. The rarity of pericardial cysts and their predominantly right-sided location highlight the unusual nature of this case, compounded by the lack of understanding regarding factors contributing to cyst growth and recurrence. The patient’s outcome, with the recurrence of the pericardial cyst and the decision to opt for continued monitoring, underscores the need for long-term follow-up in similar cases. This case raises the question of whether incomplete excision promotes the risk of recurrence. Given this question, one wonders whether continued observation should be preferred over excision in cases where preoperative imaging has suggested that complete excision of the cyst may not be possible.
Ultimately, the management of this patient’s recurrent pericardial cyst exemplifies the complexities and uncertainties involved in addressing rare and challenging clinical presentations, necessitating ongoing research and collaboration among medical specialties to improve patient outcomes.
Visual Summary.
Timeline of the Pericardial Cyst
| August 2018 | A 21-year-old woman presented to the ED with chest pain and shortness of breath. Chest CTA showed a low-density mass approximately 3.6 cm × 2.1 cm in size in the aortopulmonary window region. The patient was discharged home with ibuprofen and was lost to follow-up evaluation. |
| January 2024 | The patient presented to the same ED complaining of sharp, atypical chest pain. A repeat chest CTA revealed an increasing indeterminate low-density mass within the anterior mediastinum now measuring approximately 6.3 cm × 5.4 cm. |
| February 2024 | Chest MRI with and without contrast showed a thin-walled simple cystic mass abutting the superior margin of the left ventricle, main pulmonary artery segment, and left pulmonary artery measuring 5.8 cm × 4.8 cm × 7.6 cm. There was no associated solid mass component or abnormal enhancement, mediastinal lymphadenopathy, or pericardial effusion. The findings were most consistent with a pericardial cyst. The patient underwent a robotic-assisted left mediastinal cyst resection with diagnostic bronchoscopy. The mediastinal cyst excision was consistent with benign fibrous tissue, and the cyst fluid was consistent with benign mesothelium and negative for malignant cells. A station #10R lymph node was collected and benign. |
| September 2024 | When the patient returned for outpatient follow-up, she reported intermittent chest pain and palpitations. A chest computed tomography without contrast revealed interval recurrence of the pericardial cyst in similar location at the anterior mediastinum abutting the superior margin of the left ventricle, main pulmonary artery, and anterior margin of the left pulmonary artery. Holter monitor did not reveal significant arrhythmias. Given the risk of injury to nearby structures compounded with the lack of mechanical compression suggesting causative symptoms, the decision was made to not pursue further surgical intervention of the recurrent pericardial cyst. |
CTA = computed tomography angiography; ED = emergency department; MRI = magnetic resonance imaging.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Kar S.K., Ganguly T. Current concepts of diagnosis and management of pericardial cysts. Indian Heart J. 2017;69(3):364–370. doi: 10.1016/j.ihj.2017.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamdan J.A., Khan A., Mora A., Randhawa A., Castano M. A recurrent case of mesothelial pericardial cyst. Cureus. 2024;16(2) doi: 10.7759/cureus.53522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel J., Park C., Michaels J., Rosen S., Kort S. Pericardial cyst: case reports and a literature review. Echocardiogr J Card. 2004;21(3):269–272. doi: 10.1111/j.0742-2822.2004.03097.x. [DOI] [PubMed] [Google Scholar]
- 4.Alkharabsheh S., Ayache A., Halabi S.A., et al. Pericardial cysts: do they grow over time? J Am Coll Cardiol. 2016;67(13):1752. (suppl) [Google Scholar]
- 5.Horita K., Sakao Y., Itoh T. Excision of a recurrent pericardial cyst using video-assisted thoracic surgery. Chest. 1998;114:1203–1204. doi: 10.1378/chest.114.4.1203. [DOI] [PubMed] [Google Scholar]