Abstract
Background
Platypnea-orthodeoxia syndrome (POS) is a rare condition characterized by dyspnea and hypoxia exacerbated by an upright position. It is often associated with intracardiac or pulmonary shunting.
Case Summary
An 82-year-old woman presented with increasing fatigue, dizziness, and worsening dyspnea on exertion for 1 month. She was hypoxic, requiring high-flow oxygen. Initial work-up, including imaging and right heart catheterization, revealed an aneurysmal interatrial septum with a right-to-left shunt through a patent foramen ovale (PFO). The patient underwent successful percutaneous closure of the PFO, resulting in resolution of hypoxia and dyspnea.
Discussion
POS should be suspected in cases of positional hypoxia. The pathophysiology involves anatomical and hemodynamic factors that promote right-to-left shunting in specific positions. PFO closure is the definitive treatment, leading to symptom resolution.
Take-Home Messages
POS should be considered in patients with unexplained positional hypoxia. PFO closure can significantly improve symptoms and quality of life in affected patients.
Key words: cardiovascular disease, congenital heart defect, echocardiography, hypoxemia
Visual Summary
History of Presentation
An 82-year-old woman presented to the emergency department with increasing fatigue, decreased functional capacity, dizziness, and worsening dyspnea on exertion for 1 month. She had no prior cardiac history or hospital admissions for dyspnea. Notably, her symptoms worsened in the upright position.
Take-Home Messages
-
•
POS should be considered in patients with unexplained positional hypoxia.
-
•
PFO closure can significantly improve symptoms and quality of life in affected patients.
Past Medical History
Her past medical history included hypertension, hyperlipidemia, and gastroesophageal reflux disease.
Differential Diagnosis
The differential diagnoses considered in her case included pulmonary embolism, chronic obstructive pulmonary disease exacerbation, congestive heart failure, and platypnea-orthodeoxia syndrome secondary to intracardiac shunt.
Investigations
-
•
Laboratory tests: mild leukocytosis (12.1 K/μL), mild transaminitis (aspartate aminotransferase 56 U/L and alanine aminotransferase 96 U/L), elevated troponin (initially 70 ng/L, peaking at 637 ng/L).
-
•
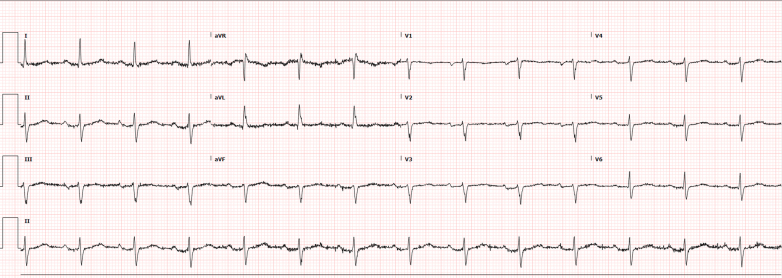
Electrocardiogram: sinus rhythm, borderline left-axis deviation (−29°), and no ischemic changes (Figure 1).
-
•
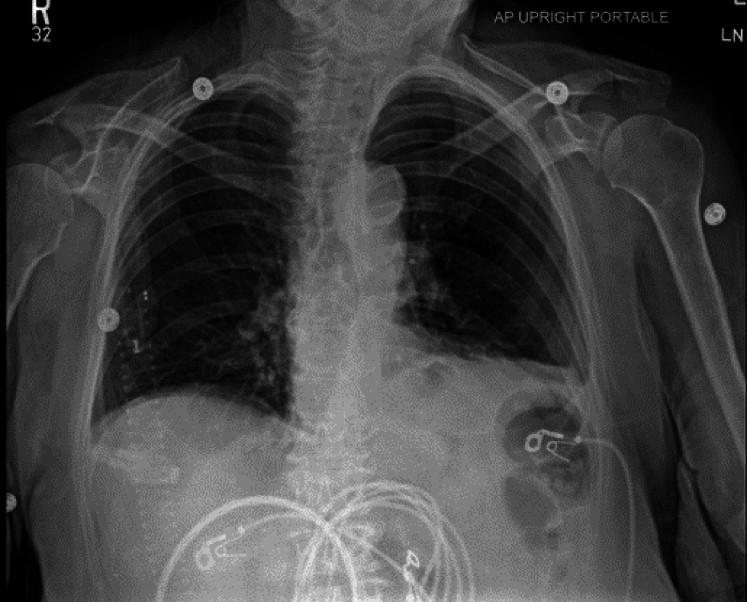
Chest radiograph: no acute cardiopulmonary pathology (Figure 2).
-
•
CT pulmonary angiography: no pulmonary embolism, mild granulomatous disease, and hiatal hernia.
-
•
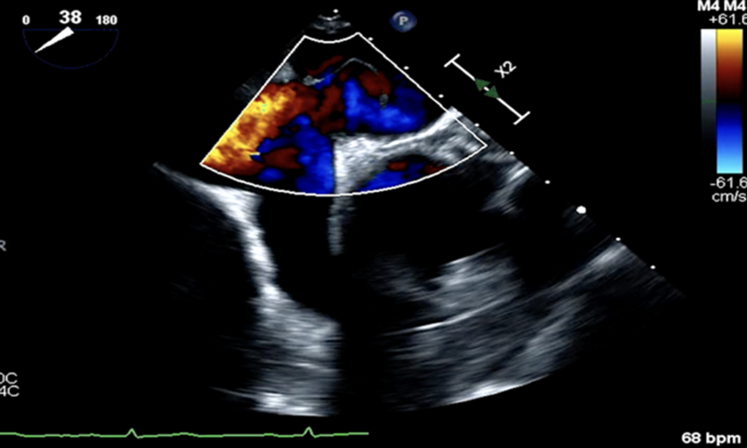
Echocardiography: left ventricular ejection fraction of 55% to 60%, aneurysmal atrial septum with a large shunt on agitated saline study, suggesting PFO (Figure 4).
-
•Right heart catheterization (RHC):
-
○Right atrial pressure: 7 mm Hg
-
○Pulmonary artery pressure: 28/10 mm Hg (mean 17 mm Hg)
-
○Pulmonary vascular resistance: 102 dynes-sec/cm5 (normal range)
-
○Oxygen saturation assessment:
-
▪right atrium: 97% → right ventricle: 73% → pulmonary artery: 74% → left atrium: 78% → aorta: 98%
-
▪
-
○Findings confirmed a significant right-to-left shunt.
-
○
-
•
Left heart catheterization: mild coronary artery disease without flow-limiting lesions.
Figure 1.
Electrocardiogram: Sinus Rhythm, Borderline Left-Axis Deviation
Figure 2.
Chest Radiograph Pre-PFO Closure: No Acute Pathology
Normal chest radiograph with no evidence of acute cardiopulmonary disease. PFO = patent foramen ovale.
Figure 4.
TEE Pre-PFO Closure: Right-to-Left Shunt on Doppler
TEE with Doppler imaging showing significant right-to-left shunting across the atrial septum. PFO = patent foramen ovale; TEE = transesophageal echocardiogram.
Management
The patient was initially managed with high-flow nasal cannula and bilevel positive airway pressure, but bilevel positive airway pressure worsened hypoxia. Nasal high-flow oxygen at 60 L/min improved oxygenation. Given the significant right-to-left shunting and positional hypoxia, a PFO occlusion procedure was pursued (Figure 3).
Figure 3.
Chest Radiograph Post-PFO Closure: No Acute Pathology
Chest radiograph with atrial septal defect closure device. PFO = patent foramen ovale.
Intervention
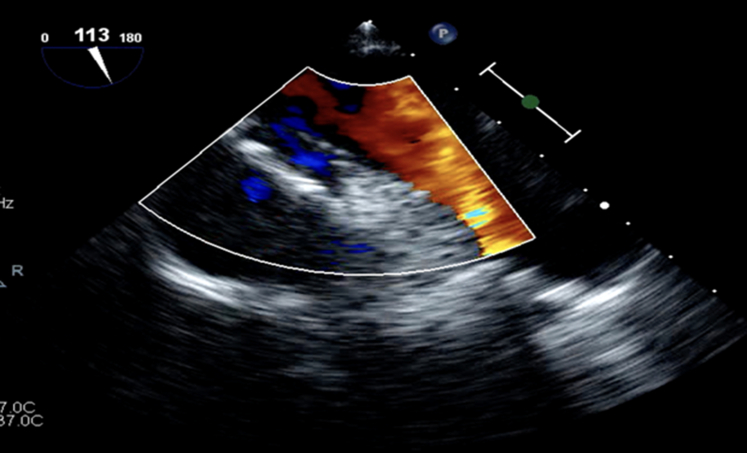
A transesophageal echocardiogram (TEE) confirmed a large PFO with a 2.3-cm tunnel length (Figure 4). Under fluoroscopic and echocardiographic guidance, a 35-mm Amplatzer PFO occluder device (Abbott) was implanted (Figure 5, Table 1). Postprocedure TEE showed minimal residual right-to-left shunting with a well-positioned occluder (Figure 6).
Figure 5.
Fluoroscopy: PFO Occlude Deployment
Fluoroscopic guidance during percutaneous PFO occlusion device placement. PFO = patent foramen ovale.
Table 1.
Equipment List for PFO Closure Procedure
| Category | Equipment |
|---|---|
| Imaging tools | Transesophageal echocardiography |
| Imaging tools | Fluoroscopic guidance |
| Closure device | 35 mm Amplatzer PFO occluder |
| Catheterization equipment | Guidewire and delivery sheath |
| Catheterization equipment | Balloon sizing catheter |
| Medications used | Dual antiplatelet therapy (aspirin, clopidogrel) |
PFO = patent foramen ovale.
Figure 6.
TEE Post-PFO Closure: Resolution of Shunting
TEE postclosure demonstrating minimal residual right-to-left shunting. PFO = patent foramen ovale; TEE = transesophageal echocardiogram.
Outcome and Follow-Up
After PFO closure, the patient's oxygen saturation improved significantly, and she was weaned off supplemental oxygen. She was discharged on dual antiplatelet therapy (aspirin 81 mg and clopidogrel 75 mg daily) for 6 months. At a 2-week follow-up, she remained asymptomatic.
Discussion
POS is a rare yet significant cause of positional hypoxia, primarily driven by intracardiac or pulmonary shunting.1,2 This case demonstrated a large PFO with right-to-left shunting, confirmed by RHC and TEE findings (Figure 4). The preferential streaming of deoxygenated blood from the inferior vena cava into the left atrium via the PFO exacerbated hypoxia, particularly in the upright position.3
The pathophysiology of POS is complex and involves multiple anatomical and hemodynamic factors. The upright position leads to changes in venous return, right atrial pressure, and interatrial pressure gradients, facilitating a right-to-left shunt through a PFO.2,4
The diagnosis of POS requires a high index of suspicion because symptoms can mimic other causes of hypoxemia such as pulmonary embolism, chronic lung disease, or heart failure.1,4 Contrast-enhanced transthoracic echocardiography or TEE with a bubble study is the gold standard for detecting a PFO and confirming the presence of a right-to-left shunt (Figure 4).3 RHC is often required to assess hemodynamics and confirm the presence of abnormal shunting.5
Guideline-supported treatment for POS includes percutaneous PFO closure, which has been demonstrated to significantly improve symptoms and oxygenation in affected patients.1,3 Several studies report that percutaneous closure leads to rapid and sustained symptomatic relief, with marked improvements in arterial oxygen saturation and quality of life.2,4 A large case series demonstrated that closure of the PFO in symptomatic patients resulted in nearly complete resolution of hypoxia and orthodeoxia within days of the procedure.5
Despite its relative rarity, POS should remain a key consideration in the differential diagnosis of positional dyspnea, particularly in older adults with no clear etiology for their symptoms.2,4 Recognizing this condition early and referring patients for appropriate intervention can significantly improve outcomes and prevent unnecessary diagnostic delays.1,3,5
Guideline Associations
-
•
The American College of Cardiology and American Heart Association recommend PFO closure for cryptogenic stroke but highlight its benefit in symptomatic POS.
-
•
POS cases with documented right-to-left shunting and hypoxia benefit significantly from percutaneous closure, as seen in this case.
Conclusions
POS should be suspected in patients with unexplained positional hypoxia. Recognition and timely intervention with percutaneous PFO closure led to resolution of symptoms and improved quality of life.
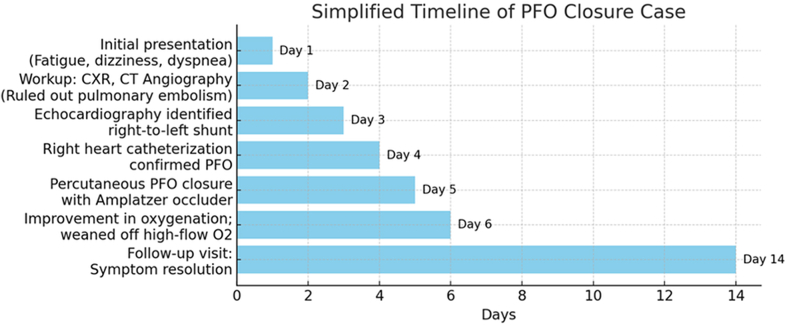
Visual Summary.
Timeline Summarizing Case Progression From Initial Presentation to Diagnosis and PFO Closure
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Alotaibi F.F., Alotaibi R.M., Almalki M.E., et al. Patent foramen ovale-induced platypnea-orthodeoxia syndrome: a case report and literature review. Cureus. 2022;14(12) doi: 10.7759/cureus.32203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medina-Bielski S., Crerar V., Garel A., Chandra A. Platypnea-orthodeoxia syndrome, an unusual cause of dyspnea. J Am Med Dir Assoc. 2023;24(5):B12. doi: 10.1016/j.jamda.2023.02.036. [DOI] [Google Scholar]
- 3.Prognosis after percutaneous foramen ovale closure among patients with platypnea-orthodeoxia syndrome. J Am Coll Cardiol. 2021;78(18):1844–1846. doi: 10.1016/j.jacc.2021.08.050. [DOI] [PubMed] [Google Scholar]
- 4.Santos F., Teixeira Reis A., Pessoa A., Agudo M., Brigas D. Platypnea-orthodeoxia syndrome: two case reports. Cureus. 2023;15(8) doi: 10.7759/cureus.43807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ribeiro R., Fialho I., Boavida L. Platypnea-orthodeoxia syndrome: a case of persistent hypoxemia. Circulation. 2021;144:115–117. doi: 10.1161/CIRCULATIONAHA.121.054424. [DOI] [PubMed] [Google Scholar]