Abstract
Introduction
Pseudoaneurysm of the right subclavian artery is very rare, and its most serious complication is rupture, which is unpredictable and fatal. Among the infectious causes, tuberculous pseudoaneurysms represent an exceptionally rare but significant subset, arising from the direct invasion of the arterial wall by Mycobacterium tuberculosis.
Case report
We present the case of a 60-year-old hypertensive male diagnosed with a right subclavian artery septic pseudoaneurysm, which is rare but serious, often resulting from an infection that weakens the arterial wall. Although bacterial infections are the most common etiologies, mycobacterial infections, such as those caused by Mycobacterium tuberculosis, should also be considered in regions with a high prevalence of tuberculosis or in patients with risk factors for this infection.
The patient was successfully treated through a cervicotomy and challenging dissection of major neck vessels. A bypass graft between the distal right subclavian artery and the right carotid artery was performed, restoring vascular flow. Postoperative outcomes were favorable, with full recovery at one week and three months follow-up.
Discussion
This case underscores the importance of timely diagnosis and surgical intervention in managing septic pseudoaneurysms, including those of tuberculous origin, to avoid life-threatening complications such as rupture or systemic sepsis. Comprehensive management should include appropriate antimicrobial therapy tailored to the underlying infectious agent to ensure long-term recovery and graft patency.
Conclusion
Early diagnosis is crucial to prevent the potentially life-threatening complications of a right subclavian artery pseudoaneurysm; therefore, this condition should be considered in patients with a history of trauma or infection presenting with a pulsatile supraclavicular mass or unexplained upper limb symptoms.
Keywords: Hypertension, Subclavian artery, Septic pseudoaneurysm, Tuberculosis, Vascular surgery, Cervicotomy
Highlights
-
•
Rare and life-threatening vascular complication of tuberculosis.
-
•
Diagnosis is challenging due to nonspecific symptoms.
-
•
Often asymptomatic until rupture or compressive symptoms.
-
•
Incidental finding on imaging or during evaluation for systemic TB.
-
•
Management involves anti-tuberculous therapy and surgical or endovascular intervention.
1. Introduction
Pseudoaneurysms are abnormal, localized dilations of blood vessels that occur when the arterial wall is breached, and blood escapes into surrounding tissue, which forms a false lumen. Unlike true aneurysms, pseudoaneurysms lack the involvement of all three layers of the arterial wall. Septic pseudoaneurysms are particularly dangerous as they result from infectious processes that weaken the vessel wall [1], often due to bacterial invasion. Common sources of infection include intravenous drug use, infected central venous lines, or contiguous spread from adjacent infected tissue. Rarely, pseudoaneurysms can also arise from tuberculous infections, referred to as tuberculous pseudoaneurysms, which result from the direct erosion of Mycobacterium tuberculosis into the arterial wall. These lesions are uncommon but highly concerning due to their association with extensive tissue damage and systemic infection.
When these lesions occur in the subclavian artery, they represent a surgical challenge, given the artery's proximity to critical structures like the brachial plexus, trachea, and esophagus. Septic pseudoaneurysms, including those caused by tuberculosis, can cause severe complications, such as rupture, hemorrhage, and distal ischemia [2]. The presence of infection further complicates surgical management, as the choice of graft material and the need for prolonged antibiotic therapy must be carefully considered. This case highlights the successful management of a subclavian artery pseudoaneurysm in a patient with a history of hypertension and no prior traumatic or invasive risk factors.
The discussion focuses on the surgical approach, the importance of controlling infection, including appropriate antimicrobial therapy for mycobacterial infections when indicated, and postoperative follow-up to ensure long-term graft patency and patient recovery.
This case report has been reported in line with the updated SCARE 2025 guidelines [3].
2. Case report
A 60-year-old retired male, BMI normal, presented to the emergency department of vascular surgery CHU Ibn Sina, in Rabat, with chest pain that radiated to his right shoulder and upper arm. The pain had progressively worsened over six days, leading the patient to seek medical attention. The patient's medical history was significant for long-standing hypertension, managed with beta-blockers. He denied any history of trauma, recent surgeries, or intravenous drug use, or other comorbidities. There was no known family history of vascular or inflammatory diseases.
On physical examination, a pulsatile and tender mass was palpated in the right supraclavicular fossa. The skin overlying the mass was a little bit erythematous, and there was mild swelling, raising suspicion for an underlying inflammatory or infectious process. The patient's radial pulse on the right side was diminished compared to the left, but no signs of distal limb ischemia, such as cyanosis or pallor, were present. He was afebrile, with a blood pressure reading of 160/100 mmHg.
Initial laboratory workup revealed an elevated white blood cell count (19,700/mm3) and an elevated C-reactive protein (CRP) level of 125 mg/L, both suggestive of a systemic inflammatory or infectious process. Blood cultures were drawn, and broad-spectrum antibiotics were started empirically.
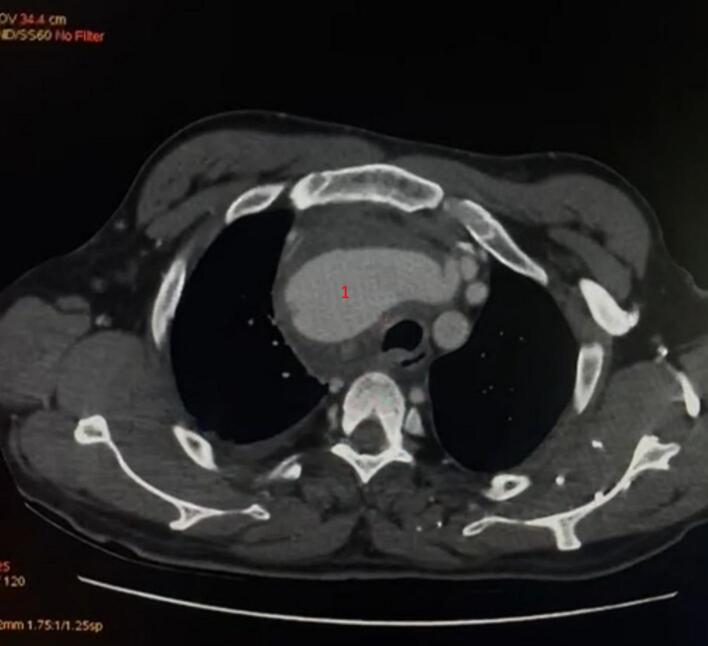
The CT scan confirmed the presence of a dilated aneurysm of the right subclavian artery starting 13 mm from its origin and extending to the cervical level, measuring a maximum diameter of 35 mm, with significant surrounding soft tissue inflammation, consistent with infection, but no signs of rupture. The lesion was closely associated with the brachial plexus and the subclavian vein, but no compression of these structures was evident. The CT scan also demonstrated a posterior aneurysmal fissure associated with a mediastinal hematoma and a small right-sided pleural effusion. Additionally, the scan revealed calcified mediastinal and hilar lymph nodes, which may have contributed to the vascular involvement by weakening the arterial wall through chronic inflammatory changes Fig. 1, Fig. 2.
Fig. 1.
Coronal and Sagittal CT showing a pseudoaneurysm of the right subclavian artery.
Fig. 2.
Axial CT image showing the pseudoaneurysm of the right subclavian artery, with the mass effect on surrounding structures.
Given the size of the pseudoaneurysm, the infectious component, the proximity to critical structures, the severity of the findings and the high risk of rupture, we discussed the necessity of urgent surgical intervention with the patient. It was explained that delaying the procedure could lead to life-threatening complications, and immediate action was essential. After obtaining the patient's consent, an anesthesiologist was consulted to evaluate his overall condition and assess his fitness for surgery. The patient's clinical stability and his ability to undergo the procedure were reviewed thoroughly, and preparations were made to proceed with surgery as soon as possible. The decision was made to perform a cervicotomy to access the affected vessels and to plan for a possible vascular bypass to restore circulation to the right upper limb.
2.1. Surgical procedure
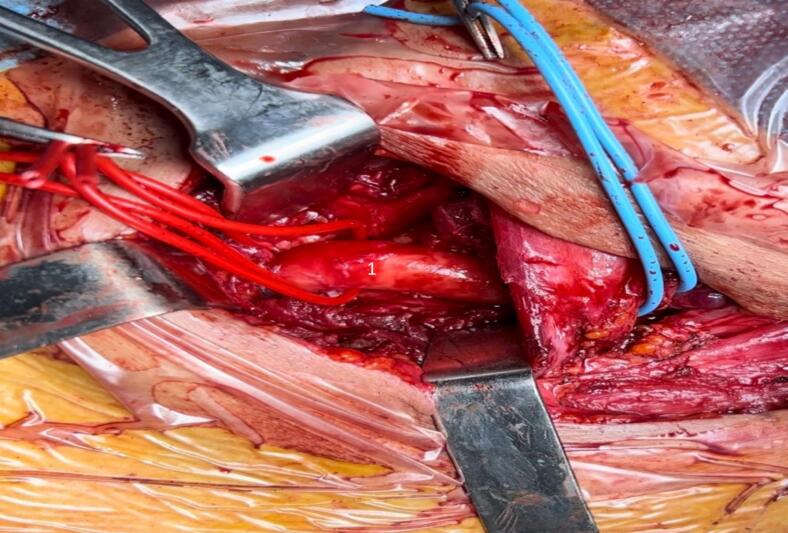
The patient was taken to the operating room under general anesthesia. A transverse cervicotomy was performed to access the right subclavian artery. The dissection was particularly challenging due to dense inflammatory adhesions encasing the vessels, making identification and control of the arterial branches difficult. The brachiocephalic trunk (TABC) Fig. 3 and the right common carotid artery were carefully dissected and controlled proximally and distally to ensure hemostasis. The subclavian artery was also exposed and clamped proximally and distally. The infected segment of the subclavian artery was resected, and extensive debridement of surrounding infected tissue was performed to reduce the risk of persistent or recurrent infection.
Fig. 3.
The brachiocephalic trunk.
To restore vascular continuity, a synthetic PTFE graft was chosen for the bypass between the distal right subclavian artery and the right common carotid artery Fig. 4. The decision to use a synthetic graft, rather than an autologous vein graft, was made due to the large caliber mismatch and the need for robust, infection-resistant material. The anastomosis was performed carefully, ensuring good blood flow through the graft to the distal subclavian artery.
Fig. 4.
A bypass graft between the distal right subclavian artery and the right carotid artery.
The resected false aneurysm was sent for pathological examination to confirm the diagnosis and assess any underlying infectious or inflammatory processes.
2.2. Postoperative course
The patient was closely monitored in the intensive care unit postoperatively. Immediate postoperative Doppler ultrasonography confirmed the patency of the bypass graft, with good blood flow to the distal right upper limb. The patient remained hemodynamically stable, and his white blood cell count and CRP levels began to normalize within the first week.
To further investigate the suspected infectious etiology of the septic false aneurysm, a series of diagnostic evaluations were undertaken while awaiting the pathological examination results. A GeneXpert test was performed to rapidly identify Mycobacterium tuberculosis. This molecular diagnostic tool provides results within hours, allowing for timely initiation of appropriate treatment. Concurrently, a chest radiograph was conducted, revealing pulmonary lesions consistent with tuberculosis. Once the pathological examination was completed, it confirmed the presence of a tuberculous pseudoaneurysm. In light of these findings, the patient was subsequently referred to internal medicine for further tuberculosis management, including a comprehensive evaluation for extrapulmonary tuberculosis involvement. Given the positive GeneXpert results, the initiation of anti-tuberculosis treatment was conducted according to the Moroccan national protocol, which typically involves a combination of Rifampicin, Isoniazid, Pyrazinamide, and Ethambutol for an initial intensive phase of two months, followed by a continuation phase of Rifampicin and Isoniazid for an additional four months. This regimen ensured effective treatment of the underlying infection.
At discharge, the patient was placed on a six-week course of oral antibiotics to support the eradication of the infection while ensuring compatibility with his ongoing anti-tuberculosis treatment. His wound healing progressed without complications, and follow-up evaluations conducted in internal medicine were arranged to monitor his response to the tuberculosis therapy. Postoperative follow-up at one month and three months showed satisfactory clinical and radiological outcomes and confirmed continued patency of the bypass graft, with no signs of infection or recurrence of the pseudoaneurysm, Fig. 5, Fig. 6. This comprehensive approach facilitated the management of both the surgical and infectious aspects of his condition, ensuring the best possible outcome for the patient.
Fig. 5.
Follow-up contrast-enhanced CT scan at 3 months postoperatively showing a patent bypass graft between the distal right subclavian artery and the right common carotid artery.
Fig. 6.
Clinical photograph at 3 months postoperatively showing a well-healed cervicotomy scar with no signs of local infection, swelling, or dehiscence.
3. Discussion
Septic pseudoaneurysms of the subclavian artery, while rare, can result from various causes, including trauma, iatrogenic injury during medical procedures, or infections [1,2]. In this case, the patient's tuberculous infection likely contributed to the formation of the pseudoaneurysm. The clinical presentation of subclavian artery pseudoaneurysms often includes pain, a pulsatile mass, and sometimes neurological symptoms such as hoarseness or motor dysfunction [2].
The primary causes of septic pseudoaneurysms include trauma and infection. Infections can weaken the arterial wall, leading to the formation of a pseudoaneurysm [4]. In this patient, the chronic tuberculosis infection likely led to the formation of the pseudoaneurysm. Tuberculosis can cause a granulomatous reaction that erodes through the vessel wall [5], resulting in a false aneurysm [6].
Diagnosis of subclavian artery pseudoaneurysms involves imaging techniques such as Doppler ultrasound, CT angiography, and sometimes MRI [3]. Doppler ultrasound allows for a quick, non-invasive assessment of blood flow, while CT angiography provides detailed images of the aneurysm and surrounding vessels [7,8].
Blood cultures were sterile. Due to the emergent nature of the case, preoperative FNAC or biopsy of the cervical lymph nodes was not feasible. The diagnosis of tuberculosis was confirmed postoperatively via histopathological analysis and GeneXpert testing of the resected tissue.
The management of such cases involves addressing both the mechanical defect in the artery and the underlying infection [9]. Surgery remains the gold standard for treatment, especially when the pseudoaneurysm is large, symptomatic, or at risk of rupture [4].
In the case described, surgery was necessary to remove the infected tissue and bypass the damaged portion of the artery, it was complicated by the need to carefully dissect the inflamed and adhered tissues around the major vessels of the neck. Control of the brachiocephalic trunk and carotid artery was essential for safely resecting the infected segment of the subclavian artery without causing catastrophic bleeding. Although a mini-sternotomy could have provided a more direct access for an inline subclavian-to-subclavian graft, this approach was not pursued. In our case, a cervicotomy was preferred due to adequate exposure of the affected arterial segment through the neck, the presence of dense inflammatory adhesions, and proximity to vital neurovascular structures. Additionally, the surgical team had greater familiarity with the supraclavicular approach, and a more extensive thoracic procedure was avoided to minimize surgical morbidity in a patient with active infection. This decision was based on intraoperative findings and weighed against the risks of a deeper dissection in an infected and anatomically complex region.
The choice of graft material is also critical in such cases. Autologous vein grafts are often preferred in infected fields because of their lower risk of graft infection. However, in this case, the size of the pseudoaneurysm and the infected field led to the decision to use a synthetic PTFE graft, which offers durability and resistance to infection. To minimize the risk of graft infection in the contaminated surgical field, the PTFE graft was soaked in a rifampicin solution prior to implantation, following our institutional protocol. Additionally, a muscle flap using the sternocleidomastoid was mobilized and placed over the vascular anastomosis to provide soft tissue coverage and further protection of the graft. These steps were taken to enhance local infection control and reduce the risk of postoperative complications.
Long-term follow-up is required to monitor for graft complications such as infection or occlusion. The patient was also treated with antibiotics [10] to address the underlying tuberculous infection [11,12].
In addition to infectious etiologies, pseudoaneurysms of large arteries can also be observed in rare systemic conditions such as vasculitis. Although less common, vascular inflammation in disorders like Takayasu arteritis or Behçet's disease may lead to pseudoaneurysm formation, particularly in major vessels such as the aorta or subclavian artery. A recent case highlights a large-artery pseudoaneurysm in a patient with vasculitis, emphasizing the importance of considering autoimmune causes in the differential diagnosis, especially when infectious workup is inconclusive [13].
Early diagnosis and surgical intervention are key to preventing complications such as rupture, distal ischemia, or sepsis. In cases involving the subclavian artery, the risk of neurovascular injury is significant, given the proximity of the brachial plexus and other vital structures. A multidisciplinary approach, involving vascular surgeons, infectious disease specialists, and intensive care teams, is crucial for managing these complex cases.
4. Conclusion
A right subclavian artery septic pseudoaneurysm is a rare condition that requires timely intervention to prevent severe complications. In this case, the tuberculous origin of the pseudoaneurysm was confirmed, and the patient was successfully treated with surgery and antibiotics. Ongoing follow-up in internal medicine was necessary to manage the underlying tuberculosis and prevent recurrence [14].
Consent
A consent was obtained from the patient to publish this case report and accompanying images.
Ethical approval
This case report is exempt from ethical approval in our institute, Ibn Sina University Hospital Center.
Funding
The authors declare that there is no funding or grant support.
Author contribution
Imane HALAOUATE, Imane Boulahroud: performed surgery, paper writing and editing.
Tarik BAKKALI, Ayoub BOUNSSIR, BRAHIM LEKEHEL: literature review, Supervision.
Imane HALAOUATE, Imane BOULAHROUD, Yassine EDDICH, Manuscript editing, picture editing.
Guarantor
Imane Halaouate M.D., Vascular and Endovascular Department, CHU Ibn Sina Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco.
Research registration number
Not applicable.
Conflict of interest statement
The authors declare that they have no competing interests relevant to the content of this article.
Contributor Information
Imane HALAOUATE, Email: Imane.halaouate@gmail.com.
Imane BOULAHROUD, Email: imaneboulahroud1@gmail.com.
Yassine EDDICH, Email: eddichyassine@gmail.com.
Tarik BAKKALI, Email: drtarikbakkali@gmail.com.
Ayoub BOUNSSIR, Email: ayoubbounssir@gmail.com.
Brahim LEKEHEL, Email: pr.lekehelbrahim@gmail.com.
References
- 1.Lokesh Koumar Sivanandam, Jhoond Manpreet Kaur, Sujanyal Saurabh Ashok, et al. A rare extrapulmonary manifestation of tuberculosis in a chronic kidney disease patient. Clin. Infect. Dis. 2023;48(12):2020. doi: 10.1002/ccr3.7807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moulakakis Konstantinos G., Alexiou Vangelis G., Sfyroeras George S., et al. European Journal of Vascular Medicine. Eur. J. Vasc. Endovasc. Surg. 2017;51(3) doi: 10.1024/0301-1526/a000572. [DOI] [Google Scholar]
- 3.Kerwan A., Al-Jabir A., Mathew G., Sohrabi C., Rashid R., Franchi T., Nicola M., Agha M., Agha R.A. Revised surgical CAse REport (SCARE) guideline: an update for the age of artificial intelligence. Prem. J. Sci. 2025;10 [Google Scholar]
- 4.Reinders Folmer Eline I., Von Meijenfeldt Gerdine C.I., et al. Diagnostic imaging in vascular graft infection: a systematic review and meta-analysis. Eur. J. Vasc. Endovasc. Surg. 2018:719–729. doi: 10.1016/j.ejvs.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 5.David M., Leonard Michael K., LoBue Philip A., Lewinsohn David M., et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention clinical practice guidelines: diagnosis of tuberculosis in adults and children. Clin. Infect. Dis. 2017;64:1–33. doi: 10.1093/cid/ciw778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baliyan Vinit, Shaqdan Khalid, Hedgire Sandeep, et al. Vascular computed tomography angiography technique and indications. Cardiovasc. Diagn. Ther. 2019:14–27. doi: 10.21037/cdt.2019.07.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moll F.L., Powell J.T., Fraedrich G., Verzini F., Haulon S., Waltham M., van Herwaarden J.A., et al. Société européenne de chirurgie vasculaire. Prise en charge des anévrismes de l’aorte abdominale : recommandations de pratique clinique de la Société européenne de chirurgie vasculaire. Eur. J. Vasc. Endovasc. Surg. 2011 janv;41(Suppl. 1):S1–S58. doi: 10.1016/j.ejvs.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Atik MD a Fernando A., Navia MD a Jose L., Svensson MD, PhD a Lars G., Vega MD a Pablo Ruda, Feng MS b Jingyuan, et al. Surgical treatment of pseudoaneurysm of the thoracic aorta. J. Thorac. Cardiovasc. Surg. 2006;132:379–385. doi: 10.1016/j.jtcvs.2006.03.052. [DOI] [PubMed] [Google Scholar]
- 9.Kim Young-wook. Infected aneurysm: current management. Ann. Vasc. Dis. 2010:7–15. doi: 10.3400/avd.AVDctiia09003. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kapoor Baljendra S., MD, Haddad Heather L., MD, Saddekni Souheil, MD, FSIR, Lockhart Mark E., MD, MPH Diagnosis and management of pseudoaneurysms: an update. Curr. Probl. Diagn. Radiol. 2009;38:170–188. doi: 10.1067/j.cpradiol.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Sharma Praveen K., Garisa Sai Sindhura, Kumaran S. Vinod, Varma Sparsh. Mycotic (infected) pseudoaneurysm, a diagnostic challenge - case series. J. Clin. Imaging Sci. 2020 doi: 10.25259/JCIS_134_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yi Shengwu, MD, Wang Lei., MD Clinical features of tuberculous pseudoaneurysm and risk factors for mortality. J. Vasc. Surg. 2022;57:1729–1738. doi: 10.1016/j.jvs.2021.10.048. [DOI] [PubMed] [Google Scholar]
- 13.Ascoli Marchetti A., Belvivere L., Argirò R., Kroegler B., Oddi F.M., Pennetta F., Giorgi A., et al. A rare but fatal Behçet variant: the Hughes-Stovin syndrome-successful case report and new evidence from literature review. Aorta (Stamford) 2023 Aug;11(4):156–161. doi: 10.1055/s-0043-1777994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soares Ana Raquel, Eusébio Sofia, Fiúza Pedro, pack Tiago, Ribeiro Tiago F. Tuberculous subclavian artery pseudoaneurysm in a young male with hemoptysis. Cureus. 2024 doi: 10.7759/cureus.75638. [DOI] [PMC free article] [PubMed] [Google Scholar]