Abstract
Background
Episiotomy, although occasionally required during labor, can result in postpartum discomfort, perineal trauma, and delayed healing. This study offers a comprehensive comparison of the safety and effectiveness of routine, restrictive, and non-episiotomy approaches on maternal and neonatal outcomes.
Methods
We systematically searched PubMed, Web of Science, Scopus, and Cochrane. We included randomized clinical trials (RCTs), comparing routine, restrictive, and non-episiotomy approaches in primiparous pregnant women. We excluded non-randomized trials, conference abstracts, and observational studies. The Cochrane ROB tool 2 was employed to appraise the selected RCTs. We conducted our analysis using the “netmeta” package of RStudio software (v.4.3.0). Dichotomous outcomes were pooled as risk ratios (RR), while continuous outcomes were pooled as the mean differences (MD). We used the random effect model for all outcomes.
Results
Sixteen studies, involving 10,738 patients, were included in the network meta-analysis. The findings revealed that the non-episiotomy group had a significantly higher risk of experiencing 1st-degree perineal tear compared to the routine episiotomy group (RR = 4.69, 95% CI [2.04; 10.74], P > 0.01). Similarly, the restrictive episiotomy group showed a significantly higher risk compared to the routine group (RR = 3.88, 95% CI [1.63; 9.26], P > 0.01). However, there were no significant differences observed between the routine, restrictive, and non-episiotomy groups regarding the duration of the 2nd stage of labor, postpartum perineal pain, and the occurrence of 2nd-, 3rd-, and 4th-degree perineal tears.
Conclusion
In conclusion, non-episiotomy approaches prove superior, with lower risks of complications compared to routine episiotomy. While restrictive episiotomy performs better than routine, it falls short of non-episiotomy methods. Therefore, non-episiotomy strategies are preferred, followed by restrictive episiotomy, with routine episiotomy being the least favorable. However, individual patient factors should guide treatment decisions, and further research is necessary to refine clinical practices.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12978-025-02132-9.
Keywords: Episiotomy, Perineal trauma, Post-partum morbidities
Introduction
The practice of episiotomy—a surgical incision to widen the birth canal—dates back to 1742 when Sir Fielding Ould first introduced it to minimize maternal trauma [1]. Despite its initial adoption without robust scientific evidence, episiotomy gained widespread acceptance in the 20th century following recommendations from leading obstetricians like Gabbe and DeLee [2, 3]. Consequently, its routine use led to a sharp rise in episiotomy rates, particularly in hospital-based deliveries, increasing from 5% in 1900 to nearly 80% by 1950 [4]. Currently, episiotomies are performed in one in three vaginal deliveries, with rates 8.8 times higher in primiparous than multiparous women [5]. Despite the WHO’s 1996 recommendation to limit episiotomies to 10% of vaginal deliveries, global rates vary significantly, ranging from 8% in the Netherlands to 25% in the US, with Taiwan reaching 100% [6]. However, rising complications have prompted a shift toward a more conservative approach [7].
Historically, episiotomy was believed to prevent severe perineal tears, neonatal complications, and long-term maternal sequelae [8]. However, emerging evidence has challenged these assumptions. The landmark 1983 review by Thacker and Banta found insufficient evidence supporting routine episiotomy and instead highlighted its associated risks, including perineal pain, hematoma, infection, dyspareunia, and healing complications [9]. As a result, professional organizations, including the American Congress of Obstetricians and Gynecologists, have shifted away from routine episiotomy in favor of a restrictive approach, reserving the procedure for specific clinical indications [10, 11].
Despite this shift, the effectiveness of different episiotomy strategies remains a subject of debate. While some studies suggest that restrictive episiotomy reduces complications [1, 12]. others, including a meta-analysis by Pereira et al., found no significant differences between restrictive and non-episiotomy approaches [13–15]. Given this ongoing controversy, a more sophisticated analytical approach is required to compare these strategies comprehensively.
To date, no study has employed network meta-analysis to evaluate episiotomy strategies. Network meta-analysis enables simultaneous comparison of multiple interventions, integrating both direct and indirect evidence to improve statistical power and precision [16–18].
This study aims to address this gap by conducting a network meta-analysis to assess the effects of routine, restrictive, and non-episiotomy strategies on maternal and neonatal outcomes in primiparous patients. By synthesizing available evidence, our findings will provide a clearer ranking of episiotomy strategies to inform clinical decision-making.
Methods
We performed our network meta-analysis (NMA) according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19] and the Cochrane handbook of systematic intervention [20].
Literature search and data collection
We searched PubMed, Web of Science, Scopus, and Cochrane library from inception until December 15, 2023. We used the following terms: episiotomy, episiotomies, perineotomy, and non-episiotomy. The detailed search strategy for each database is provided in Supplementary file Table 1.
We searched for any published results of ongoing trials. Duplications were removed using Endnote software version 21.2 for Windows, and all search received criteria assessed the eligibility through a title, abstract, and full-text screening, we included the papers that matched our criteria. We searched manually for other included studies for other related documents. We updated our search again on March 25, 2024, to avoid missing any recently published studies.
Eligibility criteria and study selection
We included all relevant randomized clinical trials (RCTs), which compared routine, restrictive episiotomy, and non-episiotomy (spontaneous tear) approaches in primiparous pregnant women. Exclusion criteria for this meta-analysis encompass non-randomized trials, observational studies, and those not explicitly comparing routine, restrictive, and non-episiotomy approaches in primiparous women. Additionally, studies lacking sufficient data, not published in English were excluded. Non-peer-reviewed sources and conference abstracts were also excluded to prioritize high-quality evidence and ensure the robustness of the analysis.
Methodological quality assessment
We conducted a rigorous quality assessment using the Cochrane Risk of Bias 2 tool [21] to evaluate the methodological quality of the included studies. This tool enabled a comprehensive evaluation across key domains such as randomization, deviations from intended interventions, missing outcome data, outcome measurement, and selection of reported results. The systematic categorization of each study into low, some concerns, or high risk of bias within these domains enhances the transparency and credibility of our NMA.
Data extraction
In our data retrieval process, we organized essential information into Excel sheets, encompassing various key elements. The first sheet, labeled “Summary,” includes details, such as study ID, site, country, National Clinical Trial (NCT) identifier, inclusion criteria, study intervention, sample size, and conclusion. The second sheet, titled “Baseline characteristics,” comprises study ID, mother’s age, intervention and control details, gestational age at delivery, birth weight, and BMI. Finally, the third sheet captures the study outcomes. Our primary outcomes included the duration of 2nd stage of labor, post-partum perineal pain, 1st, 2nd, 3rd, and 4th degrees perineal tear. However, our secondary outcomes were divided into maternal outcomes, such as post-partum blood loss > 500 ml, wound hematoma, wound infection, urinary incontinence, and anal incontinence, and neonatal outcomes, such as 1st minute and 5-minute Apgar score < 7. Two independent authors were responsible for data extraction and a third author was consulted to resolve any discrepancies.
Outcomes definition
The maternal outcomes assessed in this study encompass a range of health indicators. Wound infection is defined by the presence of infectious microorganisms at the episiotomy site, clinically evident through signs such as redness and swelling [22]. Postpartum blood loss exceeding 500 milliliters signifies excessive hemorrhage during the postpartum period [23]. The duration of the second stage of labor measures the time from complete cervical dilation to the baby’s delivery, offering insights into the labor progress [24]. Wound hematoma refers to blood accumulation at the episiotomy site, causing swelling. Postpartum perineal pain reflects discomfort experienced by mothers and can be self-reported or clinically assessed [25]. Anal incontinence signifies the inability to control bowel movements, while urinary incontinence refers to the involuntary loss of urine [26]. Additionally, the classification of perineal tears from 1st to 4th degree provides a comprehensive evaluation of perineal trauma. Neonatal outcomes, including 1st-minute and 5-minute Apgar scores below 7, serve as indicators of potential neonatal distress shortly after birth [26].
Data synthesis
The NMAs were executed through Frequency analysis in the R program (v.4.3.0) with the “netmeta” package [27] in RStudio, adhering to our study protocol. For dichotomous outcomes, risk ratios (RR) were computed, and mean differences (MD) were aggregated for continuous outcomes. Each NMA generated three visual representations tailored to our study’s specific focus: (A) a network plot illustrating patient distribution in each group with lines delineating direct comparisons among routine, restrictive, and non-episiotomy (spontaneous tear) approaches, (B) a forest plot depicting the effect estimate of each approach relative to the reference group, and (C) a league table organizing approaches based on their superiority. Statistical significance was determined at P values < 0.05. Heterogeneity was assessed using the I² test, with significance declared at P value < 0.1. The random-effect model was employed for all outcomes because we suspected the presence of heterogeneity among the included studies. The order of ranking was depicted using surface under the cumulative ranking curves (SUCRA), where a higher SUCRA value indicated a greater probability of the intervention being in the top-ranking position [28].
Results
Literature search results
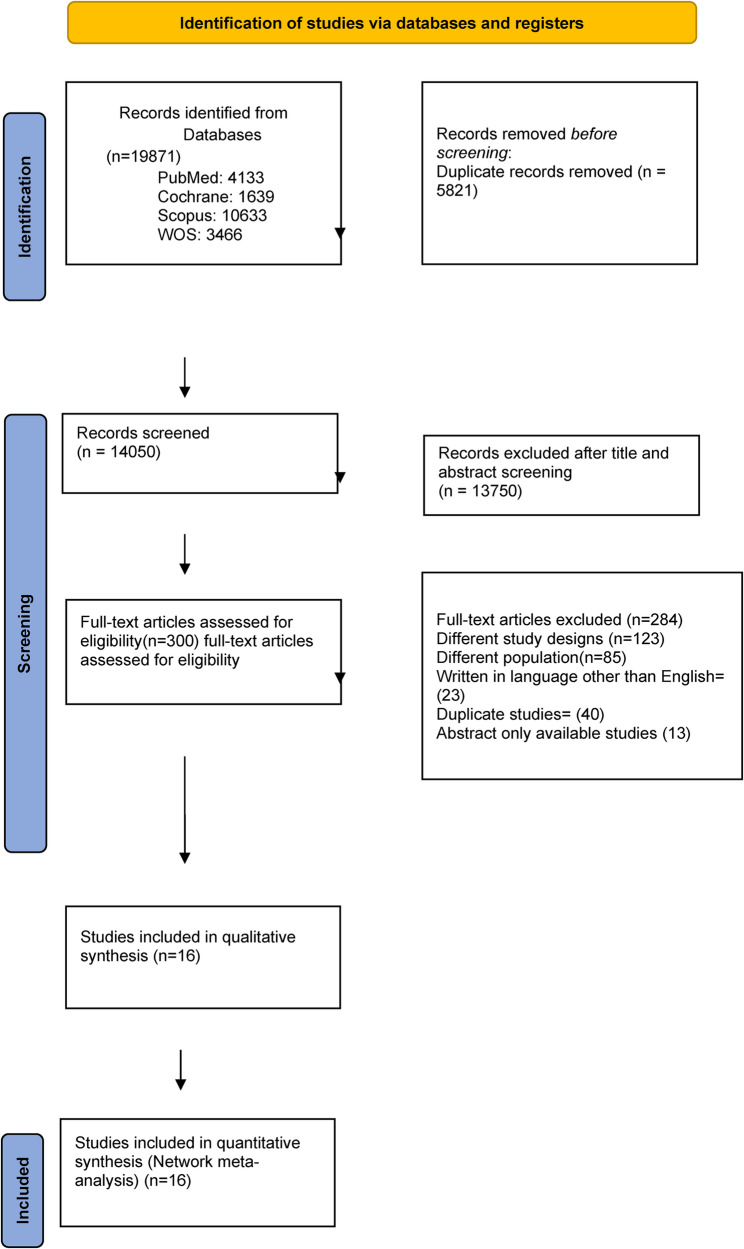
Applying our search strategy to different databases retrieved 19,871 records. After screening the titles and abstracts of these records, we had 300 articles for full-text screening. Sixteen eligible articles [4, 14, 29–42] were incorporated in our network meta-analysis (Fig. 1).
Fig. 1.
PRISMA flow diagram for included studies
Characteristics of the included studies
Nine studies compared routine with restrictive episiotomy [4, 29–31, 35, 37, 38, 41, 42], whereas three studies compared routine episiotomy with no episiotomy [32, 39, 40], and four studies compared restrictive episiotomy with no episiotomy [14, 33, 34, 36]. The mean age of mothers ranged across studies from 19.7 in Rodriguez et al. [31] to 28.5 in Sajid et al. [40]. The mean gestational age at delivery ranged from 37.9 weeks to 40.5 weeks. The mean Birth weight ranged across studies from 2899 gram in Rodriguez et al. [31] to 3589 gram in Murphy et al. [35]. The included studies span from 1988 to 2021 and were conducted across eleven countries: Brazil (1), Iran (1), Sweden (1), Israel (1), Pakistan (2), the United Kingdom (4), Malaysia (1), Colombia (1), Thailand (4), Saudi Arabia (1), and Argentina (1) (Supplementary file Table 2 and Table 3).
All 16 studies showed a low risk of bias regarding missing outcome data, except for two studies [4, 40]. Similarly, in terms of outcome measurement, all studies were at low risk, except for four studies [4, 33, 36, 40]. Ten studies demonstrated low risk of bias for the randomization process [4, 14, 29, 33–37, 41, 42], while seven studies were at low risk for deviation from the intended intervention [14, 29, 30, 34, 35, 41, 43]. Most studies had an unclear risk of bias in terms of selection of reported results, except for four studies [14, 33, 34, 36] which were low risk (Supplementary file Fig. 1).
Primary outcomes
Duration of 2nd stage of labor
Pairwise meta-analysis result
Four studies [14, 33, 34, 36] comparing between the restrictive group and the non-episiotomy group showed a non-significant mean difference (MD = 4.45, 95% CI [−4.27, 13.16]). Additionally, one study [32] comparing between the routine group and the non-episiotomy group found a non-significant mean difference (MD = 3.00, 95% CI [−10.15, 16.15]). Furthermore, two studies [29, 37] comparing between the restrictive and the routine episiotomy group revealed a non-significant mean difference (MD = −3.54, 95% CI [−14.94, 7.87]) (Figs. 2A and 3A).
Fig. 2.
Network graphs for primary outcomes
Fig. 3.
Pairwise meta-analysis for primary outcomes A Duration of 2nd stage; B Post-partum perineal pain; C 1st degree perineal tear; D 2nd degree perineal tear; E 3rd degree perineal tear; F 4th degree perineal tear
Network meta-analysis result and ranking
The non-episiotomy groups ranked first, followed by the restrictive episiotomy group and, subsequently, routine episiotomy group. The network meta-analysis demonstrated non-significant effects between the routine and non-episiotomy groups (MD = 5.27, 95% CI [−4.42, 14.97]), and the restrictive and non-episiotomy groups (MD = 3.45, 95% CI [−4.35, 11.24]). The pooled studies were heterogenous (I² = 59.8%, P = 0.03) (Figs. 4A and 5A).
Fig. 4.
Forest plots of network meta-analysis for primary outcomes A Duration of 2nd stage; B Post-partum perineal pain; C 1st degree perineal tear; D 2nd degree perineal tear; E 3rd degree perineal tear; F 4th degree perineal tear
Fig. 5.
League tables for primary outcomes A Duration of 2nd stage; B Post-partum perineal pain; C 1st degree perineal tear; D 2nd degree perineal tear; E 3rd degree perineal tear; F 4th degree perineal tear
Post-partum perineal pain
Pairwise meta-analysis result
In three studies [14, 34, 36] comparing between the non-episiotomy and restrictive groups, a non-significant risk reduction was observed (RR = 0.96, 95% CI [0.68; 1.36]). Conversely, in one study [32] comparing between the routine and the non-episiotomy groups, a significant decrease in risk was observed with the non-episiotomy group (RR = 0.20, 95% CI [0.08; 0.50]). Additionally, four studies [4, 29, 41, 42] comparing between the restrictive and routine episiotomy groups indicated a non-significant risk reduction (RR = 1.12, 95% CI [0.96; 1.29]) (Figs. 2B and 3B).
Network meta-analysis result and ranking
The non-episiotomy group ranked first, followed by the restrictive episiotomy group, and finally, routine episiotomy group. The routine episiotomy group exhibited a non-significant effect, compared to the restrictive episiotomy group (RR = 1.16, 95% CI [1.00; 1.34]). Similarly, the non-episiotomy group was comparable to the restrictive episiotomy group (RR = 0.80, 95% CI [0.58; 1.10]). The pooled studies were heterogenous (I² = 88%, P < 0.0001) (Figs. 4B and 5B).
1st degree perineal tear
Pairwise meta-analysis result
In one study [34] comparing between the non-episiotomy and restrictive episiotomy groups, a non-significant increased risk was observed (RR = 1.01, 95% CI [0.28; 3.67]). Conversely, in three studies [29, 30, 37] comparing between the non-episiotomy and routine episiotomy groups, a significant increase in risk was observed with the non-episiotomy group (RR = 5.18, 95% CI [1.99; 13.51]). Finally, three studies [32, 39, 40] comparing between the restrictive and routine episiotomy groups showed a significant increase in risk was with the restrictive episiotomy group (RR = 3.45, 95% CI [1.23; 9.71]) (Figs. 2C and 3C).
Network meta-analysis result and ranking
Routine episiotomy group ranked first, followed by restrictive episiotomy group, and finally, the non-episiotomy group. Notably, non-episiotomy episiotomy group exhibited a significantly higher effect than the routine episiotomy group (RR = 4.69, 95% CI [2.04; 10.74], P > 0.01). Similarly, the restrictive episiotomy group showed a significantly higher effect than the routine group (RR = 3.88, 95% CI [1.63; 9.26], P > 0.01). The pooled studies were heterogenous (I² = 58.9%, P = 0.03) (Figs. 4C and 5C).
2nd degree perineal tear
Pairwise meta-analysis result
In one study [34] comparing between the non-episiotomy and the restrictive episiotomy groups, a non-significant increase in risk was observed (RR = 1.01, 95% CI [0.24; 4.19]). Similarly, in three studies [29, 30, 37] comparing between the non-episiotomy and routine episiotomy groups, a non-significant risk reduction was found (RR = 0.55, 95% CI [0.20; 1.49]). Finally, three studies [32, 39, 40] comparing between the restrictive and routine episiotomy groups indicated a non-significant higher risk (RR = 1.63, 95% CI [0.63, 4.23]) (Figs. 2D and 3D).
Network meta-analysis result and ranking
The non-episiotomy group ranked first, followed by the routine episiotomy group, and finally the restrictive episiotomy group. The network meta-analysis revealed non-significant effects between the non-episiotomy versus routine episiotomy groups (RR = 0.72, 95% CI [0.31; 1.72]), and the restrictive episiotomy versus routine episiotomy groups (RR = 1.27, 95% CI [0.55; 2.92]). The pooled studies were heterogenous (I² = 81.6%, P < 0.0001) (Figs. 4D and 5D).
3rd degree perineal tear
Pairwise meta-analysis result
In one study [34] comparing between the non-episiotomy and restrictive episiotomy groups, a non-significant risk reduction was observed (RR = 0.34, 95% CI [0.03; 3.78]). Similarly, in three studies [29–31] comparing between the non-episiotomy and routine episiotomy groups, a non-significant risk reduction was found (RR = 0.86, 95% CI [0.21; 3.55]). Finally, three studies [32, 39, 40] comparing between the restrictive and routine episiotomy groups indicated a non-significant risk reduction (RR = 0.32, 95% CI [0.07, 1.39]) (Figs. 2E and 3E).
Network meta-analysis result and ranking
The restrictive episiotomy group ranked first, followed by the non-episiotomy group, and finally the routine episiotomy group. The network meta-analysis revealed non-significant effects between the non-episiotomy versus the routine episiotomy groups (RR = 0.57, 95% CI [0.24; 2.02]), and the restrictive episiotomy groups versus the routine episiotomy groups (RR = 0.50, 95% CI [0.14; 1.84]). The pooled studies were heterogenous (I² = 56.4%, P = 0.04) (Figs. 4E and 5E).
4th degree perineal tear
Pairwise meta-analysis result
In two studies [39, 40] comparing the non-episiotomy and routine episiotomy groups, a non-significant risk reduction was found (RR = 0.88, 95% CI [0.19; 3.97]). Additionally, one study [31] comparing between the restrictive and routine episiotomy groups indicated a non-significant risk reduction (RR = 0.50, 95% CI [0.13; 2.00]) (Figs. 2F and 3F).
Network meta-analysis result and ranking
The restrictive episiotomy group ranked first, followed by the non-episiotomy group, and finally the routine episiotomy group. The network meta-analysis revealed non-significant effects between the non-episiotomy versus routine episiotomy groups (RR = 0.88, 95% CI [0.19; 3.97]), and the restrictive versus routine episiotomy groups (RR = 0.50, 95% CI [0.13; 2.00]). The pooled studies were homogeneous (I² = 12.4%, P = 0.29) (Figs. 4F and 5F).
Secondary outcomes
We summarized the results of our secondary outcomes in Table 1. Also, we provide the detailed results of our secondary outcomes in the supplementary file from page 11 to page 21.
Table 1.
Summary of our analysis
| Outcome | Comparison | MA model |
Number of studies |
Estimate | 95% CI |
P
value |
Heterogeneity P value | |
|---|---|---|---|---|---|---|---|---|
| Maternal outcomes | Post-partum blood loss > 500 ml | Restricted vs. no episiotomy | Direct | 3 | 0.77 | [0.47; 1.26] | - | 0.46 |
| NMA | - | 0.89 | [0.57; 1.39] | 0.61 | ||||
| Routine vs. no episiotomy | Direct | 1 | 1.76 | [0.89; 3.46] | - | |||
| NMA | - | 1.34 | [0.79; 2.27] | 0.28 | ||||
| Restricted vs. routine episiotomy | Direct | 1 | 0.88 | [0.44; 1.76] | - | |||
| NMA | - | 0.67 | [0.39; 1.13] | 0.13 | ||||
| Wound hematoma | No vs. restricted episiotomy | Direct | 2 | 1.34 | [0.25; 7.07] | - | 0.48 | |
| NMA | - | 0.46 | [0.21; 0.99] | 0.05 | ||||
| No vs. routine episiotomy | Direct | 1 | 0.33 | [0.15; 0.71] | - | |||
| NMA | - | 0.41 | [0.20; 0.83] | 0.01 | ||||
| Routine vs. restricted episiotomy | Direct | 2 | 1.06 | [0.72; 1.55] | - | |||
| NMA | - | 1.12 | [0.77; 1.63] | 0.55 | ||||
| Wound infection | Restricted vs. no episiotomy | Direct | 2 | 2.07 | [0.79; 5.43] | - | 0.62 | |
| NMA | - | 2.72 | [1.13; 6.54] | 0.03 | ||||
| Routine vs. no episiotomy | Direct | 1 | 10.7 | [1.51; 76.07] | - | |||
| NMA | - | 3.44 | [1.24; 9.58] | 0.01 | ||||
| Restricted vs. routine episiotomy | Direct | 3 | 0.92 | [0.45; 1.88] | - | |||
| NMA | - | 0.79 | [0.40; 1.56] | 0.02 | ||||
| Urinary incontinence | No vs. restricted episiotomy | Direct | 2 | 0.64 | [0.33; 1.25] | - | 0.51 | |
| NMA | - | 0.64 | [0.33; 1.25] | 0.19 | ||||
| No vs. routine episiotomy | Direct | 0 | - | - | - | |||
| NMA | - | 1.26 | [0.21; 7.65] | 0.79 | ||||
| Routine vs. restricted episiotomy | Direct | 1 | 0.51 | [0.10; 2.72] | - | |||
| NMA | - | 0.51 | [0.10; 2.72] | 0.34 | ||||
| Anal incontinence | No vs. restricted episiotomy | Direct | 1 | 0.31 | [0.01; 7.65] | - | 0.45 | |
| NMA | - | 0.12 | [0.02; 1.00] | 0.05 | ||||
| No vs. routine episiotomy | Direct | 1 | 0.06 | [0.01; 0.44] | - | |||
| NMA | - | 0.09 | [0.01; 0.50] | 0.01 | ||||
| Routine vs. restricted episiotomy | Direct | 1 | 1.02 | [0.15; 7.10] | - | |||
| NMA | - | 1.44 | [0.26; 8.09] | 0.68 | ||||
| Neonatal outcomes | 1st minute Apgar score < 7 | No vs. restricted episiotomy | Direct | 2 | 0.84 | [0.49; 1.44] | - | 0.79 |
| NMA | - | 0.8 | [0.48; 1.35] | 0.41 | ||||
| No vs. routine episiotomy | Direct | 1 | 0.36 | [0.04; 3.37] | - | |||
| NMA | - | 0.8 | [0.44; 1.45] | 0.46 | ||||
| Routine vs. restricted episiotomy | Direct | 5 | 0.99 | [0.73; 1.33] | - | |||
| NMA | - | 1 | [0.75; 1.35] | 0.99 | ||||
| 5-minute Apgar score < 7 | No vs. restricted episiotomy | Direct | 2 | 0.34 | [0.05; 2.26] | - | 0.88 | |
| NMA | - | 0.35 | [0.06; 1.87] | 0.22 | ||||
| No vs. routine episiotomy | Direct | 1 | 0.35 | [0.01; 8.73] | - | |||
| NMA | - | 0.34 | [0.04; 2.75] | 0.31 | ||||
| Routine vs. restricted episiotomy | Direct | 1 | 1.02 | [0.14; 7.39] | - | |||
| NMA | - | 1.01 | [0.18; 5.80] | 0.99 | ||||
MA Meta-analysis, NMA Network meta-analysis, CI Confidence interval.
Discussion
Summary of the findings
In our pairwise meta-analysis, comparisons between restrictive episiotomy and non-episiotomy groups, as well as routine episiotomy and non-episiotomy groups, showed non-significant effects across various parameters, including the duration of the 2nd stage, postpartum blood loss > 500 ml, wound hematoma, wound infection, postpartum perineal pain, urinary incontinence, anal incontinence, 1st, 2nd, and 3rd-degree perineal tears, and 1st and 5th-minute Apgar scores < 7. In contrast, our network meta-analysis found that routine episiotomy significantly increased the risk of wound infection, postpartum perineal pain, and anal incontinence compared to the non-episiotomy group, but significantly decreased the risk of 1st-degree perineal tears. Additionally, comparisons between restrictive and routine episiotomy groups showed non-significant effects across most parameters, except for a significant increase in the risk of 1st-degree perineal tears in the restrictive episiotomy group.
Explanation of our finding
Our network meta-analysis reveals that routine episiotomy significantly increases the risk of wound infection, hematoma, postpartum perineal pain, and anal incontinence compared to the non-episiotomy group. This heightened risk is primarily due to the unnecessary trauma caused by episiotomy, which leads to greater pain and complications such as wound hematomas [44–46]. The disruption of the perineum’s natural tissue integrity, combined with the increased susceptibility to infection from the incision, further contributes to discomfort and delayed healing [47–49] Additionally, the impact of episiotomy on pelvic floor muscles may worsen anal incontinence [45]. These findings highlight the importance of reconsidering routine episiotomy practices to minimize unnecessary harm and optimize maternal health outcomes.
Perineal body and fibers of external anal sphincter are involved in the incisive plane of midline episiotomy in 14.3% and 16.6% of females, respectively. This specific anatomy may contribute to the higher incidence of postpartum perineal pain and anal incontinence in the episiotomy group. Additionally, the incisive plane of mediolateral episiotomy endangers superficial and deep perineal nerve branches, along with posterior labial nerves, further contributing to postpartum perineal pain [50]. Furthermore, hematomas may arise due to rupture pf subcutaneous blood vessels, taking into consideration the increased vascularity and perineal connective tissue softening during pregnancy [51, 52].
Moreover, our analysis showed no significant differences in most outcomes between restrictive and routine episiotomy groups. However, the restrictive approach was associated with a higher risk of 1st-degree perineal tears. This suggests that routine episiotomy, by providing a controlled incision, may help prevent spontaneous superficial lacerations. In contrast, the restrictive strategy, while reducing unnecessary incisions, may leave the perineum more susceptible to minor tears. Clinically, this highlights the need to balance minimizing episiotomy-related trauma with the potential risk of increased spontaneous perineal tears.
Current guidelines advocate for a restrictive approach, reserving episiotomy for necessary situations such as operative vaginal delivery, shoulder dystocia, or when managing a non-reassuring neonatal heart tracing [8]. Despite this, a systematic review on the efficacy of episiotomy for preventing and managing shoulder dystocia found no supporting evidence [53].
The American College of Obstetricians and Gynecologists (ACOG) acknowledges the lack of sufficient evidence-based criteria for episiotomy indications. The ACOG supports that clinical considerations should guide the decision-making process to perform an episiotomy and asserts that a restrictive approach is advisable [11]. Additionally, the WHO recommends against routine episiotomy during spontaneous vaginal delivery during spontaneous vaginal delivery [54]. Our findings go in alignment with WHO recommendations regarding the need to restrict routine episiotomy usage.
However, a global misinterpretation of evidence against episiotomies has led some physicians to avoid the procedure entirely, aiming to encourage the “naturalization” of delivery. This perspective has even labeled episiotomy as an “obstetrical violation” in certain institutions. Episiotomy, when performed based on indications and proper techniques, can be beneficial, preventing serious lacerations and expediting delivery in fetuses believed to be hypoxic. It is crucial to emphasize that while episiotomy may not be beneficial in all cases, failure to perform it when indicated can be equally detrimental [6].
Furthermore, key outcomes such as spontaneous laceration, the need for perineal suturing, suturing difficulty, dyspareunia, prolapse, maternal satisfaction, and wound dehiscence could not be fully assessed in our analysis due to insufficiently reported data in the included studies. These outcomes are essential to understanding the broader impact of perineal trauma and its management. Perineal injuries affect up to 90% of women during vaginal delivery and are associated with both short- and long-term complications, including persistent pain, dyspareunia, pelvic floor disorders, and depression [55]. Ensuring accurate assessment and appropriate repair of perineal trauma is crucial to reducing these complications [56]. By improving the reporting and analysis of these outcomes in future studies, we can enhance clinical decision-making and optimize patient care.
Agreements and disagreements with previous studies
Our network analysis includes 16 studies, incorporating a substantial pooled sample size of 10,738 patients. In contrast, a meta-analysis by Pereira et al. [15] involved only 2 studies, compromising 546 patients, comparing restrictive episiotomy versus no episiotomy. Another Cochrane meta-analysis in 2017 [57] included 12 studies, compromising 6,177 patients, focusing on the comparison between restrictive and routine episiotomy.
Pereira et al. [15] and the Cochrane study [57] both observed no significant difference in perineal pain and postpartum blood loss between restrictive episiotomy and either no episiotomy or routine episiotomy, aligning with our results.
Concerning the duration of the 2nd stage, Pereira et al. [15] found no significant difference between restrictive episiotomy and no episiotomy. Similarly, the Cochrane study [57] reported no significant difference in 5-minute Apgar scores < 7 and urinary incontinence between restrictive and routine episiotomy. Both findings align with our results.
In terms of wound hematoma and wound infection, Rockner et al. [32] documented a noteworthy increase associated with routine episiotomy compared to no episiotomy. This finding is consistent with our results for wound hematoma but contradicts our results for wound infection. Additionally, studies by Ali et al. [28] and the Argentine Episiotomy Trial Collaborative Group [42] found no significant difference in wound hematoma and infection between routine episiotomy and restrictive episiotomy. Furthermore, Sagi-Dain 2017 [34] and Sagi-Dain 2021 [33], reported no significant difference in these parameters when comparing restrictive episiotomy to no episiotomy, consistent with our findings.
In terms of anal incontinence, Moini et al. [39] reported a significant increase with routine episiotomy compared to no episiotomy, consistent with our findings. Additionally, Murphy et al. [35], found no significant difference between routine episiotomy and restrictive episiotomy. Furthermore, Sagi-Dain [34] and Sagi-Dain [33], comparing restrictive episiotomy to no episiotomy, also found no significant difference, aligning with our results.This highlights the ongoing debate regarding the necessity of routine episiotomy and suggests that a more restrictive approach may be preferable to minimize complications.
Aquino et al. conducted a study to examine the incidence of obstetric anal sphincter injuries (OASIS) and identify potential risk factors [58]. They reported an OASIS incidence of 1.1%. Their analysis identified several significant risk factors for severe perineal tears, including nulliparity, previous cesarean section, use of assisted reproductive technology, weight gain during pregnancy, induced labor, oxytocin augmentation, epidural analgesia, gestation beyond 40 weeks, maternal position at delivery, labor duration, vacuum-assisted delivery, and newborn weight and head circumference [58]. These findings highlight the multifactorial nature of perineal trauma and underscore the importance of individualized risk assessment during labor and delivery.
Regarding first-degree perineal tear, Moini et al. [39] and Rockner et al. [32] found a significant decrease favoring routine episiotomy, similar to our results. Sajid et al. [40], however, found a non-significant difference, contrasting with our results. For second and third-degree perineal tear, Moini et al. [39] reported a significant increase with routine episiotomy, contrasting our findings, while Rockner et al. [32] and Sajid et al. [40] found non-significant differences, aligning with our results. For fourth-degree perineal tear, both Moini et al. [39] and Sajid et al. [40] reported non-significant differences, in line with our findings.
Moreover, in studies by Eltorky et al. [37], Sulaiman et al. [30], and House et al. [29] comparing routine episiotomy to restrictive episiotomy, Sulaiman et al. [30] and House et al. [29] found a significant decrease favoring routine episiotomy, aligning with our findings. Eltorky et al. [27], however, found a non-significant difference, contrasting with our results. For second-degree perineal tear, Eltorky et al. [37] and House et al. [29] reported a significant decrease favoring routine episiotomy, in contrast to our findings, while Sulaiman et al. [30] found a significant increase with routine episiotomy, also contrasting with our findings. In third-degree perineal tear, studies by Rodriguez et al. [30, 31], Sulaiman et al. [30], and House et al. [29] found a non-significant difference, aligning with our findings. For fourth-degree tear, Rodriguez et al. [31] found a non-significant difference, aligning with our findings. Sagi-Dain et al. 2017 [34], in their study comparing restrictive episiotomy to non-episiotomy, found a non-significant difference in first, second, third, and fourth-degree perineal tear which align with our finding.
Strength points and limitations
Currently, this study represents the most comprehensive network meta-analysis comparing non-episiotomy, routine episiotomy, and restrictive episiotomy in primiparous women in relation to maternal and infant outcomes. We considered RCTs only to provide strong evidence. Encompassing 16 clinical trials with a total of 10,738 patients, we systematically evaluated 11 maternal outcomes and 2 neonatal outcomes, providing a robust overview of the current evidence.
Despite these strengths, our study has several limitations, which warrant acknowledgment. Firstly, the analysis was confined to studies conducted in English, potentially introducing a publication bias, and limiting the generalizability of our findings to a more diverse linguistic context. Secondly, we identified heterogeneity among the included trials, which may impact the consistency and general applicability of our findings. Furthermore, certain outcomes, including spontaneous laceration, the need for perineal suturing, suturing difficulty, pain scores, time to return to normal activities, dyspareunia, prolapse, maternal satisfaction, and wound dehiscence, could not be assessed in our analysis due to insufficiently reported data in the included studies. Also, we could not perform a subgroup analysis based on episiotomy type due to inconsistent reporting across studies. Even when the type was reported, the outcomes were not consistently included, potentially introducing confounding bias since complications differ between midline and mediolateral episiotomies. However, within each study, this variation was controlled. For instance, studies using midline episiotomies in the routine group also used them in the restrictive group, and the same was true for mediolateral episiotomies. This consistency helped significantly reduce bias. This limitation underscores the incompleteness of the available evidence and emphasizes the importance of more comprehensive reporting in future studies.
Implications of our findings in practice
In our network meta-analysis, the routine episiotomy group exhibited significantly higher impacts on wound hematoma, wound infection, post-partum perineal pain, and anal incontinence, indicating potential drawbacks associated with this approach. Conversely, the restrictive episiotomy group demonstrated non-significantly higher effects than the non-episiotomy group, except for wound infection. These findings underscore the need for a reevaluation of the current practices surrounding episiotomies, encouraging a more restrictive and individualized approach based on the specific needs and conditions of each patient. Healthcare providers should consider these results when making decisions regarding episiotomy procedures, aiming to optimize maternal and neonatal outcomes while minimizing unnecessary interventions and associated complications.
Recommendations
Future research in the field of episiotomy should prioritize several aspects to enhance our understanding and improve obstetric care practices. First and foremost, there is a need for well-designed, large-scale studies with rigorous methodologies to provide more robust evidence on the impact of episiotomy on maternal and neonatal outcomes. These studies should encompass diverse populations to ensure the generalizability of findings. Including outcomes such as spontaneous laceration, the need for perineal suturing, suturing difficulty, pain scores, time to return to normal activities, dyspareunia, prolapse, maternal satisfaction, and wound dehiscence in future research would provide a more comprehensive understanding of the procedure’s implications. Moreover, exploring the long-term effects of episiotomy on maternal and neonatal health could guide clinical decision-making. Also, future research should address the limitations of inconsistent reporting for episiotomy types. Standardizing the reporting of episiotomy types would enable robust subgroup analyses and clarify the distinct complications associated with midline versus mediolateral episiotomies. Lastly, assessing the impact of cultural and contextual factors on episiotomy rates and outcomes may help tailor recommendations for different settings. Overall, future research endeavors should strive for methodological rigor, inclusivity, and a holistic examination of the various facets of episiotomy to inform evidence-based obstetric care. Future research should aim to include studies in multiple languages to enhance the external validity of the results.
Conclusion
Non-episiotomy approaches consistently perform best, reducing the risk of complications like wound hematoma and infection. Routine episiotomy, on the other hand, shows higher risks, especially in wound infection. While restrictive episiotomy fares better than routine, it still lags behind non-episiotomy methods. In essence, non-episiotomy strategies are preferred, followed by restrictive episiotomy, with routine episiotomy being the least favorable. Nonetheless, individual patient factors should guide treatment decisions, and more research is needed to validate these findings and refine clinical practices.
Supplementary Information
Acknowledgements
not applicable.
Authors’ contributions
Mahmoud Shaban Abdelgalil led the team, overseeing the development and execution of the search strategy, and played a key role in conducting the analysis and discussion sections. Basma Ehab Amer contributed significantly to the analysis and took the lead in writing the discussion section, as well as editing the tables. Elsayed Eldesouky and Elsayed Farag were involved in title-abstract screening, full-text screening, and assessing the risk of bias (RoB). Moaz Yasser Darwish addressed the peer review comments. Attia Mohamed and Mohammed Ali focused on data extraction, with Attia also contributing to editing the tables and Mohammed Ali writing the introduction. Alaa Abdelsalam participated in data extraction and contributed to writing the introduction. Zeinab Yousef Hashem participated in data extraction, revised the RoB assessments, prepared the RoB table and figure. Esraa Elsayed wrote the results and the study protocol, while Reem M. Elsapagh performed full-text screening and title-abstract screening. Marwa M. Badawy contributed to writing the methods section. Mohamed Abd-ElGawad and Almandouh H. Bosilah supervised the project.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). All author(s) received no financial support for the research, authorship, and/or publication of this article.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database of Systematic Reviews. 2009;(1). Available from: https://pubmed.ncbi.nlm.nih.gov/19160176/. Cited 2024 Feb 4. [DOI] [PMC free article] [PubMed]
- 2.Myers-Helfgott MG, Helfgott AW. Routine use of episiotomy in modern obstetrics. Should it be performed? Obstet Gynecol Clin North Am. 1999;26(2):305–25. Available from: https://pubmed.ncbi.nlm.nih.gov/10399764/. Cited 2024 Feb 5. [DOI] [PubMed] [Google Scholar]
- 3.DeLee JB, Gabbe SG. The prophylactic forceps operation. Am J Obstet Gynecol. 2002;187(1):254–5. Available from: https://pubmed.ncbi.nlm.nih.gov/12114924/. Cited 2024 Feb 5. [DOI] [PubMed] [Google Scholar]
- 4.Sleep J, Grant A, Garcia JO. West Berkshire perineal management trial, vol. 289. Br Med J; 1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh S, Thakur T, Chandhiok N, Dhillon BS. Pattern of episiotomy use & its immediate complications among vaginal deliveries in 18 tertiary care hospitals in India. Indian J Med Res. 2016;143(4):474. Available from: /pmc/articles/PMC4928554. Cited 2024 Feb 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghulmiyyah L, Sinno S, Mirza F, Finianos E, Nassar AH. Episiotomy: history, present and future - a review. J Matern Fetal Neonatal Med. 2022;35(7):1386–91. Available from: https://pubmed.ncbi.nlm.nih.gov/32338105/. Cited 2024 Feb 5. [DOI] [PubMed] [Google Scholar]
- 7.Perineal care - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/19445799/. Cited 2024 Feb 5.
- 8.Myers V, Goldberg J, Episiotomy. An evidence-based approach. Obstet Gynecol Surv. 2006;61(8):491–2 https://journals.lww.com/obgynsurvey/fulltext/2006/08000/episiotomy__an_evidence_based_approach.1.aspx. [DOI] [PubMed] [Google Scholar]
- 9.Benefits and risks. of episiotomy: an interpretative review of the English language literature, 1860–1980 - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/6346168/. Cited 2024 Feb 5. [PubMed]
- 10.Association between median episiotomy. and severe perineal lacerations in primiparous women - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/9084384/. Cited 2024 Feb 4. [PMC free article] [PubMed]
- 11.Practice Bulletin No. 165: Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstetrics and gynecology. 2016;128(1):e1–15. Available from: https://pubmed.ncbi.nlm.nih.gov/27333357/. Cited 2024 Feb 5. [DOI] [PubMed]
- 12.Jostin BGR, Pirnet EEV, Nuelly PMS, Cesar MJ, Clautaire I, Herve IL. Restriction of episiotomy: obstetrical indications and perineal prognosis in two maternity wards in Brazzaville (Republic of Congo). J Gynecol Obstet. 2020;8(6):174–8 https://www.sciencepg.com/article/10.11648/j.jgo.20200806.14. [Google Scholar]
- 13.Miranda G, Pereira V, Sugahara Hosoume R, Marilene, De Castro Monteiro V, Cassia. &, Selective episiotomy versus no episiotomy for severe perineal trauma: a systematic review with meta-analysis. Available from: 10.1007/s00192-020-04308-2. Cited 2024 Jul 4.
- 14.M Amorim M, Coutinho IC, Melo I, Katz L. Selective episiotomy vs. implementation of a non-episiotomy protocol: a randomized clinical trial. Reprod Health. 2017;14(1):55. 10.1186/s12978-017-0315-4. [DOI] [PMC free article] [PubMed]
- 15.Sagi-Dain L, Sagi S. The role of episiotomy in prevention and management of shoulder dystocia: a systematic review. Obstet Gynecol Surv. 2015;70(5):354–62. Available from: 10.1097/OGX.0000000000000179. Cited 2024 Jul 4. [DOI] [PubMed] [Google Scholar]
- 16.Caldwell DM, Ades AE, Higgins JPT. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331(7521):897–900 https://www.bmj.com/content/331/7521/897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mills EJ, Thorlund K, Ioannidis JPA. Demystifying trial networks and network meta-analysis. BMJ. 2013;346. Available from: https://www.bmj.com/content/346/bmj.f2914. Cited 2024 Jul 4. [DOI] [PubMed]
- 18.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84. Available from: https://pubmed.ncbi.nlm.nih.gov/26030634/. Cited 2024 Jul 4. [DOI] [PubMed] [Google Scholar]
- 19.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. Available from: https://www.bmj.com/content/372/bmj.n71. Cited 2024 Jan 20. [DOI] [PMC free article] [PubMed]
- 20.Cochrane Handbook for Systematic Reviews of Interventions. | Cochrane Training. Available from: https://training.cochrane.org/handbook#how-to-cite. Cited 2024 Jan 20.
- 21.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(7829). Available from: https://www.bmj.com/content/343/bmj.d5928. Cited 2024 Jan 20. [DOI] [PMC free article] [PubMed]
- 22.Boushra M, Rahman O. Postpartum Infection. Obstetric Evidence Based Guidelines [Internet]. 2023;201–5. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560804/. Cited 2025 Feb 25.
- 23.21.2 Postpartum Hemorrhage. - Maternal Newborn Nursing | OpenStax. Available from: https://openstax.org/books/maternal-newborn-nursing/pages/21-2-postpartum-hemorrhage. Cited 2025 Feb 25.
- 24.7.1 Prolonged. labour | MSF Medical Guidelines. Available from: https://medicalguidelines.msf.org/en/viewport/ONC/english/7-1-prolonged-labour-51417461.html. Cited 2025 Feb 25.
- 25.Wesselmann U. Pain in childbirth. Senses: Compr Ref. 2008;5:579–83. [Google Scholar]
- 26.Arnold MJ, Sadler K, Lacerations O. Obstetric lacerations: prevention and repair. Am Fam Physician. 2021;103(12):745–52. Available from: https://www.aafp.org/pubs/afp/issues/2021/0615/p745.html. Cited 2025 Feb 25. [PubMed] [Google Scholar]
- 27.Balduzzi S, Rücker G, Nikolakopoulou A, Papakonstantinou T, Salanti G, Efthimiou O, et al. netmeta: an R package for network meta-analysis using frequentist methods. J Stat Softw. 2023;106(2):1–40. Available from: https://www.jstatsoft.org/index.php/jss/article/view/v106i02. Cited 2024 Jan 20.37138589 [Google Scholar]
- 28.Chapter 15. Interpreting results and drawing conclusions | Cochrane Training. Available from: https://training.cochrane.org/handbook/current/chapter-15. Cited 2024 Jan 20.
- 29.House MJ, Cario G, Jones MH. Episiotomy and the perineum: A random controlled trial. J Obstet Gynaecol (Lahore). 1986;7(2):107–10. [Google Scholar]
- 30.Rahman R. A randomized control trial evaluating the prevalence of obstetrical anal sphincter injuries in primigravida in r Related papers. Available from: www.smj.org.sa. [PubMed]
- 31.Rodriguez A, Arenas EA, Osorio AL, Mendez O, Zuleta JJ. Selective vs routine midline episiotomy for the prevention of third- or fourth-degree lacerations in nulliparous women. Am J Obstet Gynecol. 2008;198(3):285.e1-285.e4. [DOI] [PubMed] [Google Scholar]
- 32.Röckner G, Henningsson A, Wahlberg V, Olund A. Evaluation of episiotomy and spontaneous tears of perineum during childbirth. Scand J Caring Sci. 1988;2(1):19-24. 10.1111/j.1471-6712.1988.tb00026.x. [DOI] [PubMed]
- 33.Sagi-Dain L, Kreinin-Bleicher I, Shkolnik C, Bahous R, Sagi S. In women with spontaneous vaginal delivery, repair of perineal tears might be easier compared to episiotomy. Available from: 10.1007/s00192-020-04642-5. [DOI] [PubMed]
- 34.Sagi-Dain L, Bahous R, Caspin O, Kreinin-Bleicher I, Gonen R, Sagi S. No episiotomy versus selective lateral/mediolateral episiotomy (EPITRIAL): an interim analysis. Int Urogynecol J. 2018;29(3):415–23. [DOI] [PubMed] [Google Scholar]
- 35.Murphy DJ, Macleod M, Bahl R, Goyder K, Howarth L, Strachan B. A randomised controlled trial of routine versus restrictive use of episiotomy at operative vaginal delivery: A multicentre pilot study. BJOG. 2008;115(13):1695–703. [DOI] [PubMed] [Google Scholar]
- 36.Sagi-Dain L, Kreinin-Bleicher I, Bahous R, Gur Arye N, Shema T, Eshel A, et al. Is it time to abandon episiotomy use? A randomized controlled trial (EPITRIAL). Int Urogynecol J. 2020;31(11):2377–85. [DOI] [PubMed] [Google Scholar]
- 37.Eltorkey MM, Al Nuaim MA, Kurdi AM, Sabagh TO, Clarke F. Episiotomy, elective or selective: A report of a random allocation trial. J Obstet Gynaecol (Lahore). 1994;14(5):317–20. [Google Scholar]
- 38.Ali SS, Malik M, Iqbal J, Faruqi NJ. Routine episiotomy versus selective episiotomy in primigravidae. Ann King Edw Med Univ. 2004;10(4). Available from: https://annalskemu.org/journal/index.php/annals/article/view/1272. Cited 2024 Feb 4.
- 39.Moini A, Yari REA, Eslami B. Episiotomy and third- and fourth-degree perineal tears in primiparous Iranian women. Int J Gynaecol Obstet. 2009;104(3):241–2. Available from: https://pubmed.ncbi.nlm.nih.gov/19159878/. Cited 2024 Feb 4. [DOI] [PubMed] [Google Scholar]
- 40.Sajid A, Ali HS, Sajid A, Hanif A. Comparison of perineal tears in primigravida during vaginal delivery at term with and without medio -lateral episiotomy. Ann King Edw Med Univ. 2019;25(3). Available from: https://annalskemu.org/journal/index.php/annals/article/view/3037. Cited 2024 Feb 4.
- 41.Sangkomkamhang U, Kongwattanakul K, Kietpeerakool C, Thinkhamrop J, Wannasiri P, Khunpradit S, et al. Restrictive versus routine episiotomy among Southeast Asian term pregnancies: a multicentre randomised controlled trial. BJOG. 2020;127(3):397–403. Available from: https://pubmed.ncbi.nlm.nih.gov/31749273/. Cited 2024 Feb 4. [DOI] [PubMed] [Google Scholar]
- 42.Routine vs selective episiotomy. a randomised controlled trial. Argentine Episiotomy Trial Collaborative Group - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/7902901/. Cited 2024 Apr 9. [PubMed]
- 43.Sulaiman AS, Ahmad S, Ismail NAM, Rahman RA, Jamil MA, Mohd Dali AZ. A randomized control trial evaluating the prevalence of obstetrical anal sphincter injuries in primigravida in routine versus selective mediolateral episiotomy. Saudi Med J. 2013;34(8):819–23. [PubMed] [Google Scholar]
- 44.Röckner G, Wahlberg V, Ölund A. Episiotomy and perineal trauma during childbirth. J Adv Nurs. 1989;14(4):264–8. Available from: https://pubmed.ncbi.nlm.nih.gov/2786892/. Cited 2024 Jul 6. [DOI] [PubMed] [Google Scholar]
- 45.Walling AD. Effect of episiotomy on pelvic floor weakness. Am Fam Physician. 2005;71(3):588–588. Available from: https://www.aafp.org/pubs/afp/issues/2005/0201/p588.html. Cited 2024 Jul 6. [Google Scholar]
- 46.Kawashima M, Tokushige H. Analysis of puerperal hematoma: a retrospective study. J Rural Med. 2021;16(3):139. Available from: /pmc/articles/PMC8249368IF: NA NA NA/. Cited 2024 Jul 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, Kenton K, Gossett DR. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125(5):1088–93. Available from: https://pubmed.ncbi.nlm.nih.gov/25932836/. Cited 2024 Jul 6. [DOI] [PubMed] [Google Scholar]
- 48.Girsang BM, Elfira E. A literature review on postpartum perineal wound care: epidemiology, impact, and future interventions. Open Access Maced J Med Sci. 2023;11(F):73–80. Available from: https://oamjms.eu/index.php/mjms/article/view/11073. Cited 2024 Jul 6. [Google Scholar]
- 49.Healthcare-associated infections. surgical site infections - Annual Epidemiological Report for 2018–2020. Available from: https://www.ecdc.europa.eu/en/publications-data/healthcare-associated-infections-surgical-site-annual-2018-2020. Cited 2024 Jul 8.
- 50.Garner DK, Patel AB, Hung J, Castro M, Segev TG, Plochocki JH, et al. Midline and mediolateral episiotomy: risk assessment based on clinical anatomy. Diagnostics. 2021;11(2):221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cunningham FG, Leveno KJ, Dashe JS, Hoffman BL, Catherine Y, Spong, Brian M. Casey. Williams Obstetrics. 26th ed. 2022;54. https://accessmedicine.mhmedical.com/book.aspx?bookid=2977.
- 52.Guo X, Wu Y, Shao H, Zhang Y. Risk factors and management of perinatal genital hematoma: A single, tertiary medical center retrospective study in China. Int J Gynecol Obstet. 2024;166(2):879–85. [DOI] [PubMed] [Google Scholar]
- 53.Sagi-Dain L, Sagi S. The role of episiotomy in prevention and management of shoulder dystocia: a systematic review. Obstet Gynecol Surv. 2015;70(5):354–62. Available from: https://pubmed.ncbi.nlm.nih.gov/25974732/. Cited 2024 Feb 5. [DOI] [PubMed] [Google Scholar]
- 54.Organization WH. WHO recommendations on intrapartum care for a positive childbirth experience. 2018. Available from: https://books.google.com/books?hl=en&lr=&id=hHOyDwAAQBAJ&oi=fnd&pg=PR5&dq=World+Health+Organization.+WHO+recommendations+on+intrapartum+care+for+a+positive+childbirth+experience.+World+Health+Organization%3B+2018.&ots=eeAtTgDBTh&sig=V9PTyf-4GtPXWH6YbLCr_b1AKDE. Cited 2025 Jun 5. [PubMed]
- 55.Schmidt PC, Fenner DE. Repair of episiotomy and obstetrical perineal lacerations (first–fourth). Am J Obstet Gynecol. 2024;230(3):S1005-13. Available from: https://www.ajog.org/action/showFullText?pii=S0002937822005415. Cited 2025 Feb 24. [DOI] [PubMed] [Google Scholar]
- 56.Webb S, Sherburn M, Ismail KMK. Managing perineal trauma after childbirth. BMJ. 2014;349. Available from: https://www.bmj.com/content/349/bmj.g6829. Cited 2025 Feb 24. [DOI] [PubMed]
- 57.JiangH GP. Cochrane library Cochrane database of systematic reviews selective versus routine use of episiotomy for vaginal birth (Review). 2017. Available from: www.cochranelibrary.com. Cited 2024 Feb 5. [DOI] [PMC free article] [PubMed]
- 58.Aquino CI, Tivano A, Sala F, Della, Colagiorgio S, Scalisi L, Alemu TE et al. The ideal birth: the occurrence of severe perineal lacerations, related factors and the possibility of identifying patients at higher risk. Healthcare (Basel). 2024;12(24). Available from: https://pubmed.ncbi.nlm.nih.gov/39766010/. Cited 2025 Feb 25. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.