Abstract
A 13-year-old girl developed infective endocarditis (IE) on the native mitral valve after hospitalization for osteomyelitis. The clinical course was complicated by intramyocardial abscess and severe mitral regurgitation. Blood cultures were positive for Stenotrophomonas maltophilia, a rare cause of IE, which is known to be resistant to the first-line agents used for the treatment of IE, and has a propensity to cause a myocardial abscess. Hence, an increased awareness regarding endocarditis due to S. maltophilia is warranted.
Keywords: Cardiac abscess, infective endocarditis, Stenotrophomonas maltophilia
INTRODUCTION
Myocardial abscesses during infective endocarditis (IE) are uncommon and could be missed. Such abscesses suggest a malignant course and are associated with high mortality. Stenotrophomonas maltophilia is an opportunistic, Gram-negative bacillus that is increasingly reported to cause nosocomial infections and is known to be multidrug-resistant.[1] IE caused by this organism could lead to intramyocardial abscesses.[2] We report a case of IE due to S. maltophilia in the native mitral valve of a young patient, which was complicated by the myocardial abscess. Awareness of such cases is important, as the treatment differs from that of the usual IE and can be challenging.
CASE REPORT
A 13-year-old girl developed acute osteomyelitis of the left knee following trauma sustained from an accidental fall. During the hospitalization for the same, she developed high-grade fever and rapidly worsening dyspnea over the next 2 weeks. A contrast-enhanced CT of the chest done at a local hospital showed the possibility of septic pulmonary emboli in both lungs, and an echocardiographic study revealed severe mitral regurgitation with a vegetation attached to the posterior mitral leaflet. The patient was referred to us for further management at this stage. She had been completely well before the current illness, with normal physical development and exercise capacity.
On examination, the patient was febrile, pulse rate was 134/min, respiratory rate was 33/min, oxygen saturation was 99% on room air, and blood pressure was 90/60 mm Hg. Her left knee had mild swelling. On auscultation, a holosystolic murmur of mitral regurgitation and bilateral basal crepitations over the lung fields were found. The chest X-ray showed cardiomegaly and mild pulmonary congestion. An electrocardiogram revealed sinus tachycardia with no chamber enlargements. The laboratory examination showed leukocytosis with a total leukocyte count of 18,260/mm3. Hemoglobin was 10.5 gm/dL. C-reactive protein was 228 mg/L. Two blood cultures grew S. maltophilia, a Gram-negative bacillus, sensitive to cotrimoxazole, levofloxacin, and minocycline but resistant to penicillin, cephalosporins, and vancomycin. The transthoracic echocardiogram demonstrated the presence of a large vegetation attached to the posterior mitral valve leaflet (PMVL), causing an eccentric jet of severe mitral regurgitation and moderate pericardial effusion. Adjacent to the PMVL, a hypoechoic shadow extending to the lateral left ventricular wall was noted, indicating a myocardial abscess [Figure 1 and Supplementary Video 1]. Cardiac computed tomography (CT) done subsequently also showed the evidence of an abscess as a hypodense area with peripheral enhancement below PMVL [Figure 2]. Additionally, a pseudoaneurysm arising superior to the mitral valve below the left atrial appendage was identified [Figure 3]. Evidence of septic pulmonary emboli was identified on the CT lung images.
Figure 1.
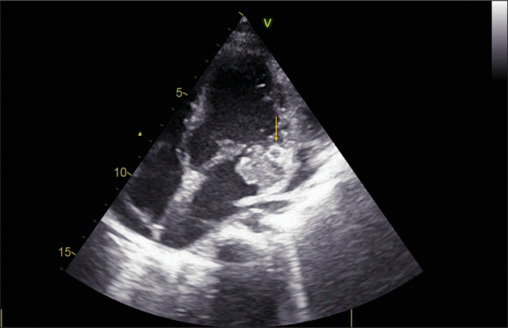
Transthoracic echocardiographic apical 4-chamber view showing hypoechoic shadow adjacent to posterior mitral valve leaflet (arrow)
Figure 2.

Cardiac computerized tomography (axial section) showing a hypodense area with peripheral enhancement below the posterior mitral valve leaflet (arrow)
Figure 3.
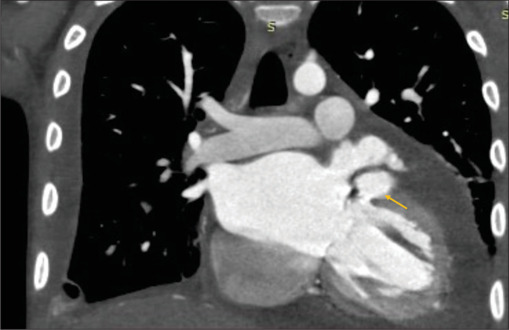
Cardiac computerized tomography (coronal section) showing a pseudoaneurysm emerging from the left atrium, below the left atrial appendage (arrow)
The patient was started on intravenous cotrimoxazole 200 mg BD and levofloxacin 250 mg OD. Unfortunately, the patient developed widespread sepsis with multi-organ involvement and died after 10 days of hospitalization. Surgical treatment for IE was considered but could not be done as the patient was considered a poor candidate in view of multiorgan dysfunction.
DISCUSSION
IE due to S. maltophilia is very rare. Nearly 50 cases have been reported worldwide, and most reports have been in adults with immunodeficiency, broad-spectrum antibiotic use, or indwelling lines.[2,3] To the best of our knowledge, IE due to S. maltophilia in children has been reported only once previously.[4]
It is important to be aware of this entity because the organism has intrinsic resistance to the commonly used first-line agents for IE, has a propensity to form a biofilm, and the disease is associated with high mortality.[3] A high incidence of complications, including myocardial abscess, has been reported with IE due to S. maltophilia,[5,6] although it has not been highlighted as such. Of the 55 cases found in the PubMed search to date, annular or myocardial abscess occurred in nearly 18% (10 out of 55 cases).
Aortic or mitral annular abscesses are well-recognized complications of IE and are identified with the use of transesophageal echocardiography (TEE), but the intramyocardial abscesses are rarely diagnosed during IE. Most cases of myocardial abscesses are seen in the course of systemic pyemia and are of little additional clinical consequence due to serious overall multi-organ sepsis. Most often, myocardial abscesses have been diagnosed at the autopsy. However, intramyocardial abscesses can be diagnosed by careful two-dimensional2Dechocardiography, as seen in this case. Intramyocardial abscesses can be echo-dense or echo-lucent. Multimodality imaging using TEE, CT, magnetic resonance imaging, and fluorodeoxyglucose-positron emission tomography can now be expected to identify intramyocardial abscesses earlier during the clinical course. In patients with IE, such an occurrence indicates a severe clinical course of the illness and might also require special considerations during the surgical management. Interestingly, in the pre-antibiotic era, an autopsy series of myocardial abscesses highlighted the relation of myocardial abscess with osteomyelitis (as seen in this patient also).[7] In the present times, intramyocardial abscesses occur due to disseminated Staphylococcal, Clostridial, Gram-negative, or fungal infections.[8]
Treatment of endocarditis caused by S. maltophilia involves appropriate antibiotic therapy and removal of any indwelling, infected foreign material in the body. S. maltophilia is resistant to penicillin, cephalosporin, and carbapenems. Sulfamethoxazole–trimethoprim is used as a first-line antibiotic,[9] although increasingly resistant organisms to this drug have also been reported. Minocycline, tigecycline, and fluoroquinolones are often effective. Synergistic treatment with two drugs is recommended to treat the IE.
S. maltophilia endocarditis is associated with high morbidity and mortality rates. The diagnosis of the organism by 16s rRNA gene sequencing is possible in culture-negative cases.[10]
A higher awareness of IE due to S. maltophilia and also of the intramyocardial abscesses during the course of any IE, seems warranted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Supplementary Video available on: https://journals.lww.com/aopc
Funding Statement
Nil.
REFERENCES
- 1.Chang YT, Lin CY, Chen YH, Hsueh PR. Update on infections caused by Stenotrophomonas maltophilia with particular attention to resistance mechanisms and therapeutic options. Front Microbiol. 2015;6:893. doi: 10.3389/fmicb.2015.00893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan IA, Mehta NJ. Stenotrophomonas maltophilia endocarditis: A systematic review. Angiology. 2002;53:49–55. doi: 10.1177/000331970205300107. [DOI] [PubMed] [Google Scholar]
- 3.Adegoke AA, Stenström TA, Okoh AI. Stenotrophomonas maltophilia as an emerging ubiquitous pathogen: Looking beyond contemporary antibiotic therapy. Front Microbiol. 2017;8:2276. doi: 10.3389/fmicb.2017.02276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alshammary A, Hervas-Malo M, Robinson JL. Pediatric infective endocarditis: Has Staphylococcus aureus overtaken viridans group streptococci as the predominant etiological agent? Can J Infect Dis Med Microbiol. 2008;19:63–8. doi: 10.1155/2008/867342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crum NF, Utz GC, Wallace MR. Stenotrophomonas maltophilia endocarditis. Scand J Infect Dis. 2002;34:925–7. doi: 10.1080/0036554021000026977. [DOI] [PubMed] [Google Scholar]
- 6.Bayle S, Rovery C, Sbragia P, Raoult D, Brouqui P. Stenotrophomonas maltophilia prosthetic valve endocarditis: A case report. J Med Case Rep. 2008;2:174. doi: 10.1186/1752-1947-2-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flaxman N. Myocardial abscess. JAMA. 1943;122:804–6. [Google Scholar]
- 8.Ramos Tuarez FJ, Yelamanchili VS, Sharma S, Law MA. StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. Cardiac abscess. [PubMed] [Google Scholar]
- 9.Dignani MC, Grazziutti M, Anaissie E. Stenotrophomonas maltophilia infections. Semin Respir Crit Care Med. 2003;24:89–98. doi: 10.1055/s-2003-37920. [DOI] [PubMed] [Google Scholar]
- 10.Balasubramanian R, Fournier PE, Menon T. Culture-negative endocarditis caused by Stenotrophomonas maltophilia: A report of two cases. Future Microbiol. 2022;17:819–22. doi: 10.2217/fmb-2021-0313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


