Abstract
Late-onset atrioventricular (AV) block is an infrequent but life-threatening complication after surgical repair of congenital heart disease. We present a rare case of late-onset AV block in an adolescent who developed high-grade AV block long after undergoing an arterial switch operation and ventricular septal defect (VSD) patch closure. The patient had a significant past medical history of ventricular ectopy detected two and a half years before her presentation with AV block, for which an ablation of a slow ventricular tachycardia was performed close to the superior border of the VSD patch. On follow-up, a few years later, she was noted to have a high-grade AV block during stress testing and an electrophysiology study and underwent a pacemaker implantation. AV heart block is a life-threatening complication that needs to be monitored for in all patients with a history of a VSD repair.
Keywords: Arterial switch repair, atrioventricular block, congenital heart disease, dextro- transposition of great arteries, late complications
INTRODUCTION
Congenital heart disease patients, particularly those with defects in close proximity to the atrioventricular (AV) node, are susceptible to AV conduction disturbances that can manifest at different stages of their lives.[1] One of the most prevalent causes of AV block in this population is immediate postoperative injury to the conduction system during ventricular septal defect (VSD) surgical repair, with an incidence ranging from 1% to 3%.[2] This injury can result from local edema, inflammation, or direct trauma to the AV node (AVN) or adjacent conduction pathways. The emergence of heart block several years after cardiac repair for congenital heart disease, although rare, occurs in up to 0.3%–0.7% of patients.[3] The majority of individuals who experience late-onset heart block usually have a history of early transient block either intraoperatively or in the immediate postoperative period.[1] The etiology of this delayed presentation of heart block may be attributed to progressive fibrosis and gradual sclerosis affecting the congenitally delicate conduction pathways.[4] This report explores the presentation, causative mechanisms, and implications of late-onset heart block in a patient several years after an arterial switch repair and a VSD patch.
CASE REPORT
An early adolescent with transposition of great arteries (TGA) who had undergone an arterial switch repair and a VSD patch closure as an infant presented to the cardiology clinic for her routine annual visit. She was reportedly asymptomatic, and physical exam findings were unremarkable except for a well-healed sternotomy scar.
Past medical history until the age of 15 was unremarkable. Like most patients with repaired TGA, the patient was followed with annual clinic visits, electrocardiograms, echocardiograms, Holter monitoring, and stress testing. At age 15, a routine exercise test was significant for ventricular ectopy in the form of frequent ventricular premature complexes at lower heart rates [Figure 1]. The ectopy was less frequent at peak exercise; however, at recovery, she had slow ventricular tachycardia at 150–170 bpm. The ventricular ectopy demonstrated a left bundle branch block morphology and an inferior axis, suggesting an origin from the anterior superior right ventricle. The patient underwent an extensive workup at that stage, which included a right and left heart catheterization and coronary angiography, which were normal. She was then taken to the electrophysiology lab, and as the earliest focus was mapped to the right ventricle anterior basal septum [Figure 2], a radiofrequency (RF) lesion at this site suppressed ventricular ectopy. There was no evidence of AH or HV prolongation at the time of the ablation, and she was monitored closely in the 3 years postablation. No further ventricular ectopy was noted, and there was no evidence of AV block on serial Holter monitoring.
Figure 1.

Stress test at 15 years of age demonstrating slow ventricular tachycardia at peak exercise
Figure 2.

Right anterior oblique (a) and posterior (b) orientation of three-dimensional electroanatomical map depicting successful ablation site at the superior antero-basal region of the right ventricle
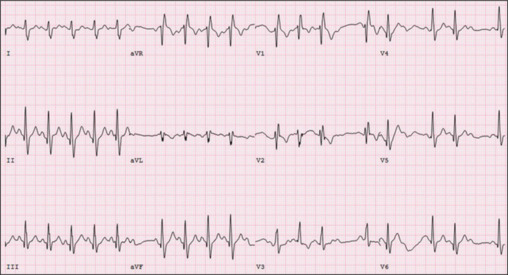
Despite being reportedly asymptomatic, a routine exercise stress test at her current presentation showed a blunting in peak heart rate (90 bpm) due to 2:1 AV block at higher levels of effort (Modified Bruce level 4) [Figure 3]. Further investigation with a 24-h Holter monitor revealed asymptomatic high-grade AV block occurring abruptly at relatively high sinus rates [Figure 4].
Figure 3.
A recent treadmill stress test demonstrated a 2:1 atrioventricular block at peak exercise
Figure 4.

Holter demonstrating high-grade atrioventricular block with several nonconducted P waves. AV: Atrioventricular
A comprehensive electrophysiology study revealed high-grade infra-Hisian AV block that worsened with the administration of isoproterenol [Figure 5]. Despite an aggressive ventricular stimulation protocol, no ventricular tachycardia was induced. Considering the high-grade AV block observed during stress testing, ambulatory monitoring, and the findings from the electrophysiology study, the patient met a Class 1 indication for pacemaker implantation. The patient received a dual-chamber pacemaker and was discharged the following day.
Figure 5.

High-grade infra-Hisian noted during electrophysiology study
Follow-up
At her first postoperative visit, she reported a significant improvement in energy levels. She is enrolled in remote pacemaker transmissions and is seen in person every 6–12 months. A year later, she now plays competitive volleyball for her university. On her last clinic visit a few months ago, she stated that having a pacemaker was the best thing that ever happened to her and completely turned her life around. She had no idea how much better she could perform in sports until she got her pacemaker.
DISCUSSION
Complete heart block after congenital surgery is a rare occurrence, affecting only 1%–3% of infants.[2] Typically, postoperative AV heart block resolves within 10 days.[1] However, a small percentage of patients develop AV heart block years later.[1,3]
Late-presenting AV heart block following a VSD repair is a complex phenomenon with no single, clear etiology. Kabbani et al. describe various mechanisms, including the proximity of the VSD patch to the conduction tissue, resulting in direct traumatic compression.[4] In addition, the VSD patch can induce an inflammatory reaction, creating scar tissue that damages the AVN. Sutures or patch materials can also compromise coronary circulation, leading to ischemia in the AVN. Progressive fibrosis over the years can lead to a late presentation of AV block, typically occurring 2–6 years after surgery.[4]
Nasser et al. describe a case where pooling of blood between the septal leaflet of the tricuspid valve and VSD led to progressive fibrosis and late complete heart block.[5] The association between arterial switch operations and AV block remains uncertain. Caudron et al. presented a study suggesting that an arterial switch operation without a VSD can contribute to AV block, possibly due to the closure of an associated atrial septal defect created during a Rashkind septostomy.[6] However, the exact mechanisms remain unclear. Altaweel et al. noted that a change in QRS axis, resultant branch block, occurrence of bifascicular block, and the proximity of the VSD patch to the conduction system are potential predictors of heart block after cardiac surgery.[7] Other predictors of late-presenting AV block include a long PR interval and a change in QRS morphology postsurgery.[8] Higher systolic blood pressures and elevated glucose levels are also listed as risk factors for postsurgical AV heart block.[9]
Our unique case involves an adolescent who developed an AV heart block nearly two decades after her initial arterial switch repair. In addition, she had undergone RF ablation on the superior aspect of the VSD patch, 3 years before the heart block, possibly causing further damage to the conduction system. The heart block in our patient could be attributed to either or both effects, contributing to progressive fibrosis and further scar tissue. This case highlights a rare electrophysiological complication years after a VSD patch repair. Patients who undergo congenital heart surgery should be closely monitored for the remainder of their lives, especially if certain predictors are noted after the initial surgical procedure.
CONCLUSIONS
While postoperative AV block is known to occur in up to 3% of infants undergoing surgery near the AVN, the presentation of AV block several years after the initial surgery is unusual. The underlying cause of late AV block may be attributed to progressive fibrosis affecting delicate conduction tissue. Permanent pacing can significantly improve the patient’s lifestyle. This case highlights two uncommon electrophysiology complications manifesting years after an arterial switch repair and underscores the importance of lifelong surveillance for patients with congenital heart disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Funding Statement
Nil.
REFERENCES
- 1.Gross GJ, Chiu CC, Hamilton RM, Kirsh JA, Stephenson EA. Natural history of postoperative heart block in congenital heart disease: Implications for pacing intervention. Heart Rhythm. 2006;3:601–4. doi: 10.1016/j.hrthm.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 2.Bonatti V, Agnetti A, Squarcia U. Early and late postoperative complete heart block in pediatric patients submitted to open-heart surgery for congenital heart disease. Pediatr Med Chir. 1998;20:181–6. [PubMed] [Google Scholar]
- 3.Lin A, Mahle WT, Frias PA, Fischbach PS, Kogon BE, Kanter KR, et al. Early and delayed atrioventricular conduction block after routine surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2010;140:158–60. doi: 10.1016/j.jtcvs.2009.12.050. [DOI] [PubMed] [Google Scholar]
- 4.Kabbani MS, Munshi F, Alhabshan F, Al Mutairi M. Unusual delayed presentation of life-threatening complete heart block after ventricular septal defect (VSD) closure with amplatzer device. Eur Heart J Suppl. 2014;16:B72–4. [Google Scholar]
- 5.Nasser BA, Mesned AR, Mohamad T, Kabbani MS. Late-presenting complete heart block after pediatric cardiac surgery. J Saudi Heart Assoc. 2016;28:59–62. doi: 10.1016/j.jsha.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caudron G, Hascoet S, Dulac Y, Maury P. Late atrio-ventricular block after arterial switch for D-transposition of the great vessels with intact interventricular septum. Cardiol Res. 2011;2:243–5. doi: 10.4021/cr69w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altaweel H, Kabbani MS, Hijazi O, Hammadah HM, Al Ghamdi S. Late presenting complete heart block after surgical repair of ventricular septal defect. Egypt Heart J. 2018;70:455–9. doi: 10.1016/j.ehj.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Villain E, Ouarda F, Beyler C, Sidi D, Abid F. Predictive factors for late complete atrio-ventricular block after surgical treatment for congenital cardiopathy. Arch Mal Coeur Vaiss. 2003;96:495–8. [PubMed] [Google Scholar]
- 9.Kerola T, Eranti A, Aro AL, Haukilahti MA, Holkeri A, Junttila MJ, et al. Risk factors associated with atrioventricular block. JAMA Netw Open. 2019;2:e194176. doi: 10.1001/jamanetworkopen.2019.4176. [DOI] [PMC free article] [PubMed] [Google Scholar]


