Abstract
Objective:
This study aimed to investigate the relationships between situational vertigo, smartphone use, sleep duration, and headaches among college students.
Methods:
A cross-sectional, descriptive correlational design and survey methodology were used. A total of approximately 55,000 students from three public and three private universities were considered for participation. A nonproportional stratified sampling method was used to target a sample size of 395 students per university. Data were collected using the Situational Vertigo Questionnaire (SVQ), which includes questions about sociodemographic factors, smoking habits, electronics usage, working hours, housekeeping activities, sleep duration, and headaches. The SVQ was translated to Arabic and validated. The statistical analysis included descriptive statistics, linear regression, and Pearson’s correlation coefficient.
Results:
This study included 1,600 participants with a mean age of 26.58 years. Significant correlations between the SVQ score and older age, female sex, and smoking were found. The strongest correlation was between the SVQ score and sleep duration (r = −0.84), indicating that a shorter sleep duration is associated with a higher incidence of situational vertigo. Smartphone use was positively correlated with the SVQ score (r = 0.67) and negatively correlated with sleep duration (r = −0.74). Additionally, headaches were associated with higher SVQ scores (r = 0.24).
Conclusion:
We identified significant associations between situational vertigo and smartphone use, sleep duration, and headaches among college students. Female sex, older age, and smoking were also associated with higher susceptibility to vertigo. These findings suggest that excessive smartphone use may lead to sleep disturbances, which contribute to vertigo. Increased awareness of these relationships can inform the development of preventive measures and counseling strategies for students on college campuses and aid health care providers in managing patients with vertigo.
Keywords: vertigo, smartphone use, sleep duration, headaches, college students
Vertigo is a common disorder that causes the sensation of spinning or dizziness and can be experienced at any age. Individuals who experience vertigo feel as though they or their surroundings are moving or rotating when they are stationary. The lifetime prevalence of vestibular vertigo among adults is 29.5 percent (Neuhauser et al, 2005). Previous studies have linked vertigo with several conditions, including sleep deprivation, excessive smartphone use, and different types of headaches, such as tension headaches and migraines (Filippopulos et al, 2017). Therefore, college students may be at high risk for vertigo.
College students are particularly susceptible to sleep deprivation, which is two- to three-times more common among these individuals than it is among the general population (Jiang et al, 2015; Cao et al, 2017; Li et al, 2018). Smartphone use, which is prevalent among college students, has been suggested as a factor that contributes to sleep deprivation (Huang et al, 2020). Additionally, headaches, such as tension headaches and migraines, are commonly experienced by college students and have been associated with vertigo (Iljazi et al, 2020).
The complex interactions between sleep deprivation, smartphone use, and headaches and their effects on vertigo among college students are not sufficiently understood. We performed a thorough literature review and did not find any studies that specifically examined the associations between vertigo, sleep deprivation, smartphone use, and headaches among college students. To our knowledge, this is the first study to explore these associations.
The primary objective of this study was to investigate the relationships between situational vertigo, smartphone use, sleep duration, and headaches among college students. Understanding these relationships could be beneficial to the development of preventive measures and management strategies that reduce the overall impact of vertigo.
METHODS
Design
During this study, we used a cross-sectional, descriptive correlational design and survey methodology to investigate factors related to vertigo among college students.
Participants
We considered approximately 55,000 students from three public and three private universities for participation in this study. Students 18 years of age or older were eligible for participation. Individuals who were pregnant, unable to comprehend or complete the questionnaires, or had conditions such as congenital deformities, malignancies, amputations, prostheses, or severe disabilities were excluded because these conditions can lead to imbalance, thus potentially altering the results. Additionally, those with a history of otological disorders were excluded because such conditions can cause vertigo or imbalance, thereby altering the results.
Sampling and Sample Size
We selected a representative sample of students from all academic years using nonproportional stratified sampling. To achieve a sample size with an estimated vertigo prevalence of 45 percent, 95 percent confidence interval, and a significance level of 0.05, 395 students per university were required.
Procedure
The Institutional Review Board of Jordan University of Science and Technology approved this study. Participants were given an invitation that explained the study. After signing written consent forms, students in randomly selected classes with more than 40 students completed the survey with the instructor’s permission. Of the 2,000 questionnaires distributed, 1,600 were returned, yielding a response rate of 80 percent.
Survey Questionnaire
Participants completed the Situational Vertigo Questionnaire (SVQ) (Guerraz et al, 2001), which is used to assess vertigo symptoms in various situations with high reliability and validity. The SVQ consists of 19 items that are scored from 0 (no symptoms) to 4 (severe symptoms). Additional questions refer to sociodemographic factors, smoking habits, electronics usage, working hours, housekeeping activities, sleeping duration, and headaches.
Translation Procedure
Five bilingual university professors translated the SVQ to Arabic using a backward–forward translation process. A consensus was reached to resolve any discrepancies. A pilot study including 20 individuals tested the clarity and indicated necessary revisions of the SVQ. A subsequent pilot study confirmed that no further changes were necessary. Ten bilingual professors back-translated the Arabic version to English and reviewed it to ensure that all items met a similarity cutoff score of 0.80, thus maintaining the original meaning.
Data Processing and Statistical Analysis
We conducted a data analysis using IBM SPSS Statistics version 20 (SPSS Inc., Chicago, IL). Additionally, we calculated descriptive statistics, including frequency distributions, means, and standard deviations, for variables such as age, sex, marital status, education level, presence and types of diseases, smoking status, coffee intake (number of cups per day), smartphone use, sleep duration, and presence of headaches. A significance level of 0.05 was applied to all statistical tests.
Linear regression was used to examine the relationships between the dependent variable (SVQ score) and independent variables (smartphone use, sleep duration, and headaches). Additionally, Pearson’s correlation coefficient was used to study the associations among the SVQ score, smartphone use, sleep duration, and headaches.
The total SVQ score was categorized as “not at all,” “very slight,” “somewhat,” “quite a lot,” or “very much.” Scores were rounded to the nearest whole number. A higher SVQ score indicated more severe vertigo.
RESULTS
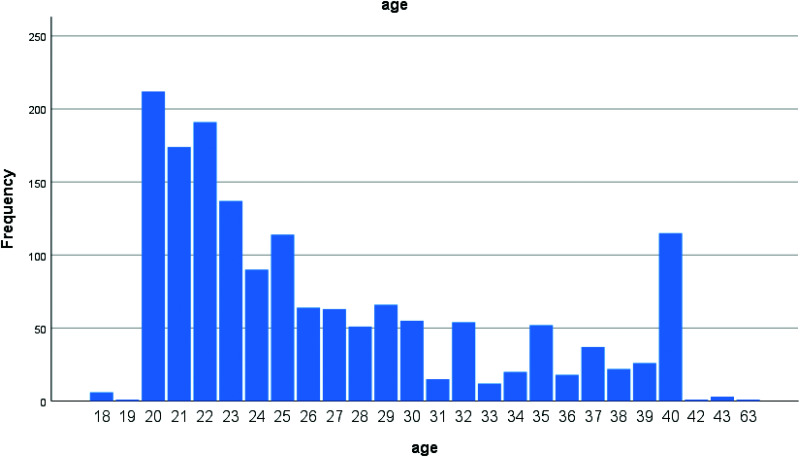
The mean age of the participants was 26.58 years (range, 18–63 years). Notably, the majority (99.7 percent) of participants were young adults 40 years of age or younger. The demographic data were further analyzed to include specific age ranges (Figure 1), socioeconomic statuses, and academic disciplines (Table 1), thus providing a deeper understanding of how these factors may influence the relationships between vertigo and the studied variables.
Figure 1.
Age distributions of the participants.
Table 1.
Demographic Data
| Frequency | Percent | |
|---|---|---|
| Sex | ||
| Male | 695 | 43.5 |
| Female | 905 | 56.5 |
| Marital status | ||
| Single | 1,026 | 64.2 |
| Married | 572 | 35.8 |
| Residencea | ||
| Town | 718 | 44.9 |
| City | 880 | 55.1 |
| Educationb | ||
| School | 290 | 18.1 |
| Diploma | 155 | 9.7 |
| Bachelor’s degree | 1,056 | 66.0 |
| Master’s degree | 71 | 4.4 |
| PhD | 28 | 1.8 |
| Smoking | ||
| Yes | 555 | 34.7 |
| No | 1,045 | 65.3 |
Town refers to a small village with a small population. City refers to an urban center with a larger geographical area and population.
School here refers to having a high school degree. Diploma refers to having a 2-year degree post high school.
Additional demographic data (Table 1) revealed that slightly more females (56.5 percent) than males were study participants. Most participants (93.8 percent) had an undergraduate degree or high school diploma. The data also indicated a high smoking rate of 34.7 percent. Significant correlations between SVQ scores and factors such as older age, smoking, and female sex were observed (Table 2).
Table 2.
Correlations among the Situational Vertigo Questionnaire Score, Age, Sex, and Smoking
| Variables | Pearson’s Correlation | p Value |
|---|---|---|
| Older age | 0.080 | 0.002 |
| Female | 0.138 | 0.000 |
| Smoking | 0.64 | 0.000 |
Table 3 presents the distribution of participants based on the presence and degree of difficulty associated with vertigo according to the SVQ scores. The results indicated that most participants experienced no difficulty (61.1 percent) or only very slight difficulty (32.9 percent). An analysis of situations for which participants reported significant difficulties (“quite a lot” or “very much”) revealed that the most common challenges involved heights, driving over the top part of the slope of a hill, driving around bends, and wide open spaces (Table 4).
Table 3.
Number and Percentage of Participants According to the Situational Vertigo Questionnaire Score
| Frequency | Percenta | Valid Percenta | Cumulative Percenta | |
|---|---|---|---|---|
| Validb | ||||
| Not at all | 974 | 60.9 | 61.1 | 61.1 |
| Very slight | 524 | 32.8 | 32.9 | 94.0 |
| Some what | 85 | 5.3 | 5.3 | 99.4 |
| Quite a lot | 10 | 0.6 | 0.6 | 100.0 |
| Very much | 0 | 0 | 0 | 100.0 |
| Total | 1,593 | 99.6 | 100.0 | |
| Missing Systemc | 7 | 0.4 | ||
| Total | 1,600 | 100.0 |
Percent: refers to percentage of SVQ score divided over (total number of participants). Valid percent: refers to percentage of SVQ score divided over (total number of participants minus the number of participants with missing data). Cumulative percent: refers to total percentages summed together.
For each category, the valid count represents the actual number and percentage of participants, calculated from the total number of participants excluding those with missing data.
Missing System: The number of participants with missing data, which is why they were excluded from the analysis.
Table 4.
Situations Associated with “Quite a Lot” or “Very Much” Difficulty According to the Responses to the Situational Vertigo Questionnaire
| Situation | Frequency |
|---|---|
| Riding as a passenger in a car on straight, flat roads | 96 |
| Riding as a passenger in a car on winding or bumpy roads | 150 |
| Walking in a supermarket aisle | 75 |
| Standing in a stopped elevator | 161 |
| Standing in an elevator while it moves at a steady speed | 162 |
| Riding in a car at a steady speed | 98 |
| Driving or stopping in a car | 102 |
| Standing in the middle of a wide open space | 121 |
| Sitting on a bus | 173 |
| Standing on a bus | 161 |
| Heights | 272 |
| Watching moving scenes on the television or at the movie theater | 121 |
| Riding on escalators | 134 |
| Looking at striped or moving surfaces | 156 |
| Looking at a scrolling computer screen or microfiche | 170 |
| Going through a tunnel while looking at the lights on the side | 145 |
| Going through a tunnel while looking at the light at the end | 138 |
| Driving over the top part of the slope of a hill, around bends, or in wide open spaces | 176 |
| Watching moving traffic or trains | 130 |
A linear regression analysis (Table 5) showed a significant association between the SVQ score (the dependent variable) and smartphone use, sleep duration, and headaches (the independent variables).
Table 5.
Linear Regression among the Situational Vertigo Questionnaire Scores and Headaches, Smartphone Use, and Sleep Duration
| ANOVAa | ||||
|---|---|---|---|---|
| Model 1 | df | Mean Square | F | Significance |
| Regression | 3 | 129.288 | 1373.336 | 0.000b |
| Residual | 1,577 | 0.094 | ||
| Total | 1,580 | |||
| Coefficientsa | |||||
|---|---|---|---|---|---|
| Unstandardized Coefficients | |||||
| Model 1 | Beta | SE | Standardized Coefficients Beta | t | Significance |
| Constant | 3.615 | 0.086 | 41.886 | 0.000 | |
| Sleep duration | −0.395 | 0.010 | −0.749 | −38.224 | 0.000 |
| Smartphone use | 0.032 | 0.006 | 0.104 | 5.331 | 0.000 |
| Headaches | −0.104 | 0.016 | −0.085 | −6.308 | 0.000 |
Dependent variable: Situational Vertigo Questionnaire score.
Predictors: constant headaches, smartphone use, and sleep duration.
ANOVA = analysis of variance; df = degrees of freedom; SE = standard error.
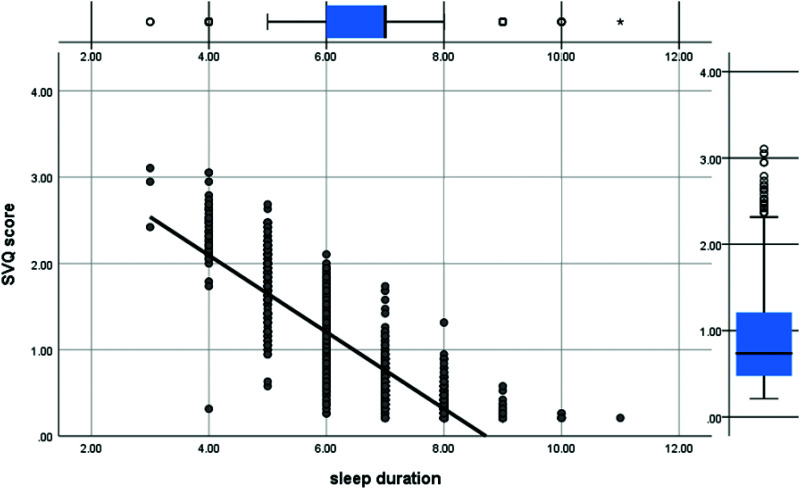
A Pearson correlation analysis (Table 6) demonstrated significant correlations between the SVQ score and each independent variable. The strongest correlation was between the SVQ score and sleep duration (r = −0.84), followed by smartphone use (r = 0.67) and headaches (r = 0.24). Additionally, sleep duration showed strong correlations with both smartphone use and headaches (Figures 2, 3, and 4).
Table 6.
Pearson Correlation among the Situational Vertigo Questionnaire Score and Sleep Duration, Smartphone Use, and Headache
| Sleep Duration | Smartphone Use | Headaches | SVQ Score | |
|---|---|---|---|---|
| Sleep duration | ||||
| Pearson correlation | 1 | −0.735** | 0.197** | −0.843** |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | |
| N | 1,584 | 1,582 | 1,583 | 1,584 |
| Smartphone use | ||||
| Pearson correlation | −0.735** | 1 | 0.188** | 0.671** |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | |
| N | 1,582 | 1,593 | 1,592 | 1,582 |
| Headaches | ||||
| Pearson correlation | 0.197** | 0.188** | 1 | 0.253** |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | |
| N | 1,583 | 1,592 | 1,599 | 1,583 |
| SVQ score | ||||
| Pearson correlation | −0.843** | 0.671** | 0.253** | 1 |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | |
| N | 1,584 | 1,582 | 1,583 | 1,584 |
** A significant correlation was considered at the level of 0.01 (two-tailed).
Figure 2.
Scatterplot graph of the correlation between the Situational Vertigo Questionnaire (SVQ) score and sleep duration.
Figure 3.
Scatterplot graph of the correlation between the Situational Vertigo Questionnaire (SVQ) score and smartphone use.
Figure 4.
Scatterplot graph of the correlation between smartphone use and sleep duration.
DISCUSSION
This study explored the relationships between situational vertigo, smartphone use, sleep duration, and headaches among college students and identified a significant correlation between age and vertigo, with older participants exhibiting a higher propensity for vertigo. This increased susceptibility of older adults can be attributed to the presence of additional risk factors such as diabetes, hypertension, heart disease, stroke, and cognitive decline. According to Neuhauser et al (2005), vertigo is three-times more common among the elderly population than it is among younger individuals (Neuhauser et al, 2005).
Participants older than typical college students (typical age, 18–25 years) were included in our study to account for the presence of postgraduate students, who are often older than undergraduate students. This inclusion was important because it provided a more comprehensive view of the population. However, only 0.003 percent of the participants were older than 40 years, which is a minimal proportion and, thus, unlikely to significantly impact the overall results.
Additionally, the higher incidence of vertigo among older participants may be related to longer exposure to risk factors such as smoking and prolonged use of smartphones. Over time, these factors can contribute to the deterioration of vestibular function, further justifying the observed results.
Our findings also indicated a higher prevalence of vertigo among females. A previous study similarly documented a higher incidence of vertigo among females compared to that among males (Teggi et al, 2016).
Additionally, during this study, we observed a significant correlation between smoking and vertigo. Formeister and Sharon (2021) reported that vertigo is 1.72 times more prevalent among smokers than it is among nonsmokers. Furthermore, Wada et al (2017) found that smokers are 2.7 times more likely than nonsmokers to experience vertigo. In our sample, a substantial proportion (34.7 percent) of participants were smokers.
Our study demonstrated a strong link between headaches/migraines and vertigo. Additionally, Iljazi et al (2020) reported that dizziness occurs in 33 percent of individuals during a headache episode. Moreover, Akdal et al (2013) observed that dizziness is highly prevalent among individuals with both migraine and tension headaches.
During our study, we found that sleep duration had a significant and the strongest correlation with the SVQ score (r = −0.84). This strong negative correlation indicated that shorter sleep durations are associated with a higher incidence of situational vertigo, as measured by the SVQ score. Poor sleep quality is prevalent and inversely associated with vertigo (Du et al, 2023). Kim et al (2018) used the Dizziness Handicap Inventory to study the effect of sleep deprivation on dizziness among 237 individuals and found a strong association between sleep quality and dizziness (Kim et al, 2018).
Furthermore, our results revealed high correlation between the SVQ score and smartphone use; this positive relationship suggested that longer smartphone use leads to higher SVQ scores. Excessive smartphone use contributes to vertigo; however, its mechanisms remain unclear. Prolonged screen time may lead to visual strain and vestibular system overload, resulting in vertigo. Additionally, smartphone use often disrupts sleep patterns, leading to sleep deprivation, which is strongly associated with an increased incidence of vertigo. This hypothesis is supported by studies that linked screen time to poor sleep quality and vertigo (Obermann et al, 2014; Chang et al, 2015; Toker et al, 2023).
During our study, smartphone use was negatively correlated with sleep duration (r = −0.74) and positively correlated with the SVQ score (r = 0.67). Other studies have also found strong associations between smartphone use and sleep quality and duration (Demirci et al, 2015; Lemola et al, 2015; Dewi et al, 2018; de Sá et al, 2023).
Several potential confounding variables, such as physical activity, dietary habits, and preexisting medical conditions, were not controlled for during this study. These factors may have influenced the observed relationships between vertigo, smartphone use, sleep duration, and headaches. Future studies should consider these variables to provide a more comprehensive analysis.
Importantly, the cross-sectional design of this study limited our ability to establish causality between variables. Future research should consider using longitudinal designs to determine causal relationships between situational vertigo, smartphone use, sleep duration, and headaches.
Study Limitations
This study had several limitations. First, the use of a cross-sectional design limited our ability to establish causality. Second, the self-reported nature of the data may have introduced bias, such as recall bias or social desirability bias. Third, the study sample was from a specific geographic region; therefore, the generalizability of the findings may be limited.
CONCLUSIONS
The results of this study identified a strong association between the SVQ score and smartphone use, headaches, and sleep duration among college students. Additionally, factors such as female sex, older age, and smoking were associated with higher susceptibility to situational vertigo. In particular, smartphone use may be the primary factor that precipitates sleep disturbances, subsequently leading to vertigo. Increasing awareness about the relationships between smartphone use, sleep disturbances, and vertigo can aid in the development of preventive measures and counseling strategies by health care providers on college campuses. Furthermore, health care providers may consider these factors when managing patients with vertigo to improve treatment outcomes. Future studies with longitudinal designs and more diverse populations should explore the effectiveness of interventions aimed at reducing smartphone use and promoting healthy sleep habits among college students. For instance, educational programs regarding the risks of excessive smartphone use and the importance of sleep could be developed and implemented on college campuses. Additionally, creating smartphone usage guidelines, such as limiting screen time before bed, could help mitigate the impact of vertigo. Additionally, studies should investigate the underlying neurobiological mechanisms that link sleep disturbances and vertigo as well as the role of neuropeptides in the relationship between headaches and vertigo.
Abbreviations
- SVQ
Situational Vertigo Questionnaire
Footnotes
Any mention of a product, service, or procedure in the Journal of the American Academy of Audiology does not constitute an endorsement of the product, service, or procedure by the American Academy of Audiology.
REFERENCES
- Akdal G, Ozge A, Ergör G. (2013) The prevalence of vestibular symptoms in migraine or tension-type headache. J Vestib Res 23(2):101–106. [DOI] [PubMed] [Google Scholar]
- Cao X-L, Wang S-B, Zhong B-L, et al. (2017) The prevalence of insomnia in the general population in China: a meta-analysis. PLoS One 12(2):e0170772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang AM, Aeschbach D, Duffy JF, Czeisler CA. (2015) Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci U S A 112(4):1232–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Sá S, Baião A, Marques H, et al. (2023) The influence of smartphones on adolescent sleep: a systematic literature review. Nurs Rep 13(2):612–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demirci K, Akgönül M, Akpinar A. (2015) Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict 4(2):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewi RK, Efendi F, Has EMM, Gunawan J. (2018) Adolescents’ smartphone use at night, sleep disturbance and depressive symptoms. Int J Adolesc Med Health 33(2). [DOI] [PubMed] [Google Scholar]
- Du Z, Wang G, Yan D, Yang F, Bing D. (2023) Relationships between the Pittsburgh sleep quality index (PSQI) and vertigo outcome. Neurol Res 45(4):291–299. [DOI] [PubMed] [Google Scholar]
- Filippopulos FM, Albers L, Straube A, et al. (2017) Vertigo and dizziness in adolescents: risk factors and their population attributable risk. PLoS One 12(11):e0187819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Formeister EJ, Sharon JD. (2021) The association between smoking and dizziness in U.S. adults: a population-based survey study. Hear Balance Commun 19(1):36–41. [Google Scholar]
- Guerraz M, Yardley L, Bertholon P, et al. (2001) Visual vertigo: symptom assessment, spatial orientation and postural control. Brain 124(Pt 8):1646–1656. [DOI] [PubMed] [Google Scholar]
- Huang Q, Li Y, Huang S, et al. (2020) Smartphone use and sleep quality in Chinese college students: a preliminary study. Front Psychiatry 11:352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iljazi A, Ashina H, Lipton RB, et al. (2020) Dizziness and vertigo during the prodromal phase and headache phase of migraine: a systematic review and meta-analysis. Cephalalgia 40(10):1095–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang XL, Zheng XY, Yang J, et al. (2015) A systematic review of studies on the prevalence of insomnia in university students. Public Health 129(12):1579–1584. [DOI] [PubMed] [Google Scholar]
- Kim SK, Kim JH, Jeon SS, Hong SM. (2018) Relationship between sleep quality and dizziness. PLoS One 13(3):e0192705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. (2015) Adolescents' electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc 44(2):405–418. [DOI] [PubMed] [Google Scholar]
- Li L, Wang Y-Y, Wang S-B, et al. (2018) Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res 27(3):e12648. [DOI] [PubMed] [Google Scholar]
- Neuhauser HK, von Brevern M, Radtke A, et al. (2005) Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology 65(6):898–904. [DOI] [PubMed] [Google Scholar]
- Obermann M, Wurthmann S, Steinberg BS, et al. (2014) Central vestibular system modulation in vestibular migraine. Cephalalgia 34(13):1053–1061. [DOI] [PubMed] [Google Scholar]
- Teggi R, Manfrin M, Balzanelli C, et al. (2016) Point prevalence of vertigo and dizziness in a sample of 2672 subjects and correlation with headaches. Acta Otorhinolaryngol Ital 36(3):215–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toker ÖG, Elibol NT, Erentürk Ö, et al. (2023) Effect of digital screen usage on the visual-vestibular system interaction. Egypt J Otolaryngol 39(1):140. [Google Scholar]
- Wada M, Takeshima T, Nakamura Y, et al. (2017) Association between smoking and the peripheral vestibular disorder: a retrospective cohort study. Sci Rep 7(1):16889. [DOI] [PMC free article] [PubMed] [Google Scholar]