Abstract
Background and Objective:
Myocardial infarction (MI) is one of the most prevalent cardiovascular disorders and a progressively debilitating condition. Patients with MI often experience a reduced quality of life (QoL), primarily due to the severe complications associated with the disease. Enhancing QoL and self-care practices in these patients is essential. Self-care training is a potential strategy to improve QoL in this population. Consequently, this study aimed to explore the impact of implementing Orem’s self-care model on the QoL of MI patients admitted to the ICU.
Methods:
This study utilized a quasi-experimental design and was conducted between February 2021 and August 2022. The study population consisted of 70 MI patients hospitalized in the ICU of a hospital in Ilam City. Eligible patients, based on inclusion and exclusion criteria, were divided into intervention and control groups. Data were collected using a questionnaire comprising 3 sections: 1) demographic information, 2) needs assessment based on Orem’s model, and 3) the MacNew Heart Disease Health-related Quality of Life questionnaire. The intervention group received four self-care training sessions (each lasting 30–45 minutes) delivered through in-person, virtual, and phone-based methods, along with a self-care training booklet. Participants in both groups completed the QoL and self-care questionnaires before the intervention, as well as 2 weeks and 2 months after the intervention, via face-to-face visits or phone/virtual interviews. The collected data were analyzed using SPSS, version 26. The normality of the data was confirmed using the Kolmogorov-Smirnov test, and repeated-measures ANOVA was employed to compare QoL scores across different dimensions between the intervention and control groups before and after the implementation of Orem’s model.
Results:
The findings revealed no significant difference in the mean QoL scores between the intervention and control groups before the intervention (mean difference =5.2±2.3; P=0.05). However, after the intervention, a significant difference in the mean QoL scores was observed between the 2 groups (mean difference =15.9±8.1; P=0.001).
Conclusion:
Orem’s self-care training effectively enhanced the QoL of MI patients, indicating that the approach is a viable non-pharmaceutical strategy for improving QoL in this patient population.
Keywords: Orem’s self-care, Quality of life, Myocardial infarction
Introduction
Cardiovascular diseases (CVDs) stand as the leading cause of mortality worldwide.1 According to reports from the American Heart Association (AHA), the Centers for Disease Control and Prevention, and the US National Institute of Health, CVDs claim approximately 17.3 million lives annually, with a projected increase to over 23.6 million by 2030.2 AHA statistics indicate that of the 26.8 million patients seeking outpatient care, 16 million are related to myocardial infarction (MI).1
In Iran specifically, CVDs account for more than 90 thousand deaths each year, which highlights the urgent need for effective strategies to combat the growing burden of CVDs, both globally and in Iran. MI, commonly known as a heart attack, results from reduced or completely disrupted blood supply to a portion of the myocardium.2 This event can profoundly impact an individual’s physical, psychological, and social functioning, as well as their ability to carry out daily activities. MI survivors often face long-term physical challenges, including dyspnea, fatigue, and pain, which can significantly affect their overall quality of life (QoL).3
Research has highlighted the importance of follow-up care in reducing pain, anxiety, and heart failure rates among MI patients while also enhancing their physical capabilities, social and familial interactions, and overall QoL.4 QoL encompasses a complex, multi-dimensional concept, which refers to an individual’s perception of their health status, evaluation of well-being and welfare across various life aspects, and satisfaction with their current situation.5
Assessing QoL is particularly crucial for patients with chronic diseases, as these conditions not only impact physical health but also significantly affect psychosocial well-being, often leaving patients with diminished hope for recovery.6 Given that CVDs fall under the umbrella of chronic conditions, evaluating QoL in these patients becomes an essential task, influencing decisions regarding therapeutic interventions and care strategies.6 Essentially, QoL is a concept deeply intertwined with nursing practice, as nurses play a pivotal role in enhancing patients’ QoL through the provision of care services and involvement in nursing research. A fundamental goal in disease management is to elevate patients’ patients’ performance and QoL to a satisfactory level. 7
One approach to enhancing the QoL of patients with chronic diseases involves providing self-care programs and devising effective strategies to meet this objective. Weber et al8 cited the World Health Organization’s (WHO) definition of self-care as the capacity of individuals, families, and communities to maintain and improve health, prevent disease, and cope with illness or disability, either independently or with the assistance of healthcare providers. A significant outcome of self-care is the empowerment of patients to make informed decisions about their healthcare needs and self-care behaviors. Self-care serves as a crucial component for individuals from all walks of life, enabling them to lead well-rounded lives across various health dimensions and at all levels of care.8
One significant health model is Orem’s self-care model, which emphasizes individuals’ capacities and self-care needs, enabling patients to engage in self-care activities.9 As a nursing model, it primarily focuses on self-care aspects. Orem’s self-care model provides one of the most extensive self-care theories, offering valuable clinical guidance for planning and executing self-care programs.10 Orem, a prominent nursing self-care theorist, defined self-care as voluntary and purposeful activities carried out by an individual or caregiver to enhance performance, maintain life, promote health, and address personal needs.11 Self-care involves activities individuals undertake to preserve their lives and promote health and well-being. Numerous studies have explored the application of Orem’s self-care model in providing nursing care to patients with chronic conditions, including those undergoing hemodialysis, suffering from CVDs, multiple sclerosis, and the elderly population.
In a study conducted by Naji et al,7 researchers evaluated the self-care levels and educational-support needs of MI patients using Orem’s self-care model. The results indicated self-care levels of 58%, 42%, and 44% in the knowledge, motivation, and skills dimensions, respectively. Blood glucose and triglyceride levels were significantly associated with self-care levels in the skills (P=0.03) and knowledge (P=0.04) dimensions, although no significant correlation was observed with other variables. These findings revealed a considerable gap between actual and desired self-care levels in MI patients, emphasizing the necessity for Orem model-based self-care training and support to enhance self-care capabilities among this population.12
Considering the high mortality rates among MI patients and the substantial costs associated with their care and complication management, it is crucial to investigate self-care determinants in this population. Nonetheless, there is a dearth of research on this topic in Iran, particularly in Ilam City. Accordingly, this study aimed to examine the impact of implementing a self-care program based on Orem’s model on the QoL of MI patients admitted to the CCU at Mostafa Khomeini Teaching Hospital in Ilam City between 2021 and 2022.
Methods
This study utilized a randomized pretest-posttest control group design, incorporating control and intervention groups. The research population comprised 70 MI patients, with the sample size calculated with α=5% and β=10 using the following formula:
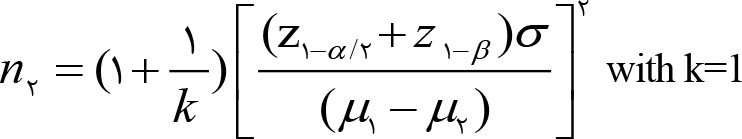 |
Participants were recruited from patients admitted to the CCU and post-CCU of Mostafa Khomeini Hospital in Ilam City between February 2021 and August 2022. Participants were randomly assigned to either the intervention or control group.
Inclusion criteria stipulated that participants must have a confirmed MI diagnosis, possess reading and writing literacy, and receive specialist approval regarding their capability to perform self-care. Exclusion criteria included a lack of interest in self-care activities, recurrent MI following the initiation of self-care, and failure to participate in the provided training for more than 3 days. The study employed convenience sampling for patient enrollment.
To control for potential confounding variables and ensure an equal chance of assignment to either group, block randomization was employed for participant allocation. This method allowed for balancing the distribution of participants between the experimental and control groups until the desired sample size was attained.
The statistical population was divided into 2 groups—test and control—using random allocation. Randomization ensures each participant has an equal likelihood of being assigned to either the test or control group. This process was carried out in 2 stages: First, a random sequence was generated to determine group assignments. Second, the generated sequence was concealed (random assignment hiding) to maintain allocation blindness.
This two-stage randomization process was executed as follows:
Stage 1: Creating a random sequence: The block randomization method was employed, as it maintains balance in sample allocation across the test and control groups. This approach also facilitates equality in the number of participants assigned to each group, particularly in cases where interim analyses are required. Blocks of 4 were created, each containing 2 participants designated for the test group and 2 for the control group. Within these blocks of 4, 6 distinct sequences were possible: 1) PPMM; 2) PMMP; 3) PMPM; 4) MPMP; 5) MMPP; and 6) MPPM.
Stage 2: Concealment of random assignment: Card selection was determined using the Software Allocation Random software’s random numbers table. A person not directly involved in the research conducted blocking and allocation sequence concealment. Based on the obtained blocks and allocation sequence, participants were subsequently allocated to either the test or control group.
In this study, the MacNew Heart Disease Health-Related Quality of Life Questionnaire (MacNew QoL) was used as one of the data collection tools. Developed in 1991, the MacNew QoL questionnaire comprises 27 items assessing QoL across 3 dimensions: emotional (12 items), physical (10 items), and social (5 items). Each question is rated on a 7-point scale, where respondents indicate their answer on a continuum from “always” to “never.” The highest and lowest scores for each dimension are 7 and 1, respectively. Total scores on the MacNew QoL scale range from 27 to 198, with scores of 27–67, 68–108, 109–149, and 150–189 denoting poor, moderate, acceptable, and excellent QoL, respectively. The lowest possible score of 27 reflects the poorest QoL, while the maximum score of 189 corresponds to the best possible QoL.
The MacNew QoL has demonstrated validity and reliability for use in MI patients. Asadi-Lari et al13 (2003) employed the MacNew QoL in MI patients, confirming the instrument’s overall internal consistency (Cronbach’s α=0.95) and the reliability of the emotional (Cronbach’s α=0.92) and physical dimensions (Cronbach’s α=0.92), as well as the social dimension (Cronbach’s α =0.94).
The Myocardial Infarction Self-Care Ability Questionnaire (Myocardial Infarction Self-Care Brief) is a self-report instrument that evaluates 3 dimensions: awareness, skills, and willingness. The skills dimension comprises 22 items, addressing various self-care activities pertinent to MI patients. These activities include diet (6 questions), MI-related tests (1 question), pharmaceutical care (9 questions), and stress management and education (6 questions). Responses to each item are scored on a scale of 1 to 5, with the total score for this dimension (range: 22–110) calculated as the sum of the individual item scores. The awareness dimension of the Myocardial Infarction Self-Care Brief comprises 25 items that assess patients’ knowledge of self-care activities and various aspects of MI. These aspects include the cardiovascular system (5 questions), the nature of MI (3 questions), MI complications (4 questions), MI care (8 questions), MI diet (3 questions), and MI medications with their usage instructions (2 questions). Each item in this dimension is scored from 1 to 5, and the total self-care score for the awareness dimension (range: 25–125) is calculated as the sum of individual item scores. The willingness dimension consists of 7 items examining MI patients’ motivation to adhere to self-care activities. Items in this scale are also scored from 1 to 5, yielding a total self-care score for the willingness dimension (range: 7–35).
A needs assessment form was developed based on Orem’s model, consisting of the following 4 sections: 1) Demographic information: This section collected data on contact details, age, gender, marital status, literacy level, occupation, and medical history. 2) Self-care gaps: This section evaluated health deviations, clinical diagnoses, and disease-related information and skills. 3) General self-care needs: This part addressed various aspects, including respiration, blood circulation, body temperature, skin and lip color, daily routine, eating habits, oral and dental care, defecation status, laboratory test results, skin, hair, and nail health, daily activities, self-perception, self-confidence, self-care ability, and patient dependence or independence in carrying out tasks. 4) Self-care needs specific to health conditions: This section focused on needs related to growth and development, disease management, health maintenance and promotion, medication regimens, physical activity, and dietary regimens.
Orem’s self-care model assesses patients’ strengths and weaknesses, enabling the development and implementation of tailored nursing interventions to address their specific needs. In this study, the application of Orem’s model involved the following steps: The first step entailed evaluating MI patients’ needs across 3 dimensions: general self-care, developmental self-care, and self-care during health deviations. The second step consisted of recognizing self-care gaps as nursing diagnoses and determining patients’ ability to overcome these deficiencies. At the third stage, based on the identified patient needs and capacities, an appropriate plan was designed to address self-care gaps and promote optimal health outcomes.
In this study, all participants received support from a nursing system that included education, counseling, and follow-up care to enhance their self-care abilities. For the intervention group, individual in-person training sessions were conducted, comprising four 30- to 45-minute sessions covering various topics such as etiology, clinical symptoms, appropriate dietary regimens, medication adherence, timely medication intake, regular testing, the importance of physical activity, self-care instructions, and potential drug side effects. Following the training sessions, an educational pamphlet summarizing the covered content was provided to the intervention group patients. Participants were monitored over an 8-week period, and upon completion, the data collection tools were administered to all patients once again.
Statistical Analysis
The data were analyzed using SPSS, version 26. Descriptive statistics, including mean, standard deviation, frequency, and percentage, were used to summarize the data. The normality of the data was confirmed using the Kolmogorov-Smirnov test. Consequently, repeated-measures ANOVA was employed to compare QoL scores across different dimensions between the intervention and control groups before and after the implementation of Orem’s model.
Ethical Considerations
This study was approved by the Ethics Committee of Ilam University of Medical Sciences (IR.MEDILAM.REC.1401.151). The study objectives were clearly explained to all participants, and they were assured of the confidentiality of their information. Written informed consent was obtained from each participant before their involvement in the study.
Results
The study involved 70 patients diagnosed with MI, with 35 participants assigned to each of the intervention and control groups. The mean ages of the participants were 59.24±5.22 years in the intervention group and 64.44±3.26 years in the control group (Table 1). The normality of the data was confirmed using the Kolmogorov-Smirnov test. Repeated-measures ANOVA was utilized to compare QoL scores across different dimensions between the intervention and control groups before and after the implementation of Orem’s model.
Table 1.
Comparison of the mean and standard deviation of quality-of-life scores at 3 time points between the study groups
| Quality of Life | Groups | P-value | |
|---|---|---|---|
| Intervention mean ± SD | Control mean ± SD | ||
| Pre-intervention | 58.94±13.65 | 54.69±10.35 | 0.97 |
| Two weeks post-intervention | 169.63±16.60 | 70±9.24 | <0.001 |
| Two months post-intervention | 168.43±12.50 | 72±12.45 | <0.001 |
The mean and standard deviation of QoL scores before the intervention were 58.94±13.56 in the test group and 54.69±10.35 in the control group, showing no statistically significant difference (P>0.05). Nonetheless, 2 weeks after the intervention, the mean and standard deviation of QoL scores were 169.63±16.60 in the test group and 70.0±9.24 in the control group, demonstrating a significant difference (P<0.05).
Two months after the intervention, the mean and standard deviation of QoL scores were 168.43±12.50 in the test group and 72±12.45 in the control group.
Regarding self-care skill scores, the mean and standard deviation before the intervention were 38.63±3.77 in the test group and 34.60±4.83 in the control group, indicating no significant difference. Two weeks after the intervention, the mean and standard deviation of self-care skill scores were 100.80±5.23 in the test group and 43.80±7.18 in the control group, showing a significant difference (P<0.005). Two months after the intervention, these scores reached 102.10±4.80 in the test group and 53.03±9.65 in the control group, also representing a significant difference (P<0.005).
The mean and standard deviation of self-care tendency scores before the intervention were 13.83±2.01 in the test group and 13.74±1.86 in the control group, showing no significant difference. Two weeks after the intervention, the mean and standard deviation of self-care tendency scores were 31.17±2.82 in the test group and 17.00±1.69 in the control group, denoting a significant difference P<0.005). Two months after the intervention, these scores reached 31.60±2.81 in the test group and 17.46±1.50 in the control group, which also demonstrated a significant difference (P<0.005).
The mean and standard deviation of self-care awareness scores before the intervention were 38.03±6.74 in the test group and 38.74±6.46 in the control group, showing no significant difference. Two weeks after the intervention, the mean and standard deviation of self-care awareness scores were 111.23±11.50 in the test group and 40.80±6.60 in the control group, indicating a significant difference (P<0.005). Two months after the intervention, these scores reached 112.77±20.235 in the test group and 41.74±6.56 in the control group, also denoting a significant difference (P<0.005).
Table 2.
Comparison of mean scores for quality of life and its dimensions (emotional, physical, and social) among elderly individuals experiencing myocardial infarction across the 2 study groups at 3 time points: before the intervention, 2 weeks after, and 2 months after the intervention
| Variables | Intervention Group | Control Group | P-value (General Linear Model) | F test | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Emotional performance | Pre-intervention | 34.89 | 5.01 | 23.09 | 6.20 | ||
| Two weeks post-intervention | 51.26 | 10.19 | 23.09 | 6.20 | 0.001 | 101.949 | |
| Two months post-intervention | 53.03 | 9.65 | 23.10 | 6.21 | |||
| Physical performance | Pre-intervention | 27.80 | 6.15 | 26.06 | 3.96 | ||
| Two weeks post-intervention | 48.94 | 11.84 | 26.06 | 3.96 | 0.001 | 203.567 | |
| Two months post-intervention | 51.26 | 9.63 | 26.06 | 3.96 | |||
| Social performance | Pre-intervention | 11.47 | 3.54 | 11.80 | 2.89 | ||
| Two weeks post-intervention | 25.09 | 5.91 | 11.77 | 2.88 | 0.001 | 358.030 | |
| Two months post-intervention | 26.06 | 4.91 | 11.77 | 2.88 | |||
| Quality of life | Pre-intervention | 1.17 | 0.382 | 1.14 | 0.355 | ||
| Two weeks post-intervention | 3.40 | 0.497 | 1.14 | 0.355 | 0.001 | 356.746 | |
| Two months post-intervention | 3.49 | 0.507 | 1.14 | 0.355 | |||
Discussion
In this study, we assessed the impact of implementing Orem’s self-care model on the QoL of MI patients. The results revealed that the mean total QoL score increased significantly from 1.17±0.382 before the intervention to 3.49±0.507 two months after the intervention, indicating improvements across all QoL dimensions.
These findings align with those of Khayam-Nekoui et al15 (2014), who investigated the effect of self-care training based on Orem’s model on the QoL of patients with heart failure. The results of their study, consistent with our findings, demonstrated that self-care training based on Orem’s model significantly improved the QoL of heart failure patients. This was evidenced by a notable increase in the mean QoL score following the implementation of the self-care model compared with pre-intervention levels (P=0.124). In contrast, our findings differ from those of Mahmoudi et al16 (2019), who evaluated the effect of a self-care training program on the QoL of patients with sickle cell anemia. Their study found no significant change in the overall QoL score before and after the intervention in patients who received self-care training. This discrepancy in results may be attributed to differences in the nature and duration of the diseases, as well as the varying age ranges of the participants.
Davodabadi et al17 (2017) conducted a study to examine the effect of Orem’s self-care model on the QoL of elderly individuals across various dimensions. Their findings revealed that this approach positively influenced multiple aspects of QoL, including mental health, physical health, social relationships, and spiritual health in the studied population. Furthermore, the study provided evidence that Orem’s self-care model could enhance self-care practices and self-efficacy, leading to improved mental health management and overall QoL in the elderly. Consistent with our findings, the results of this study support the use of Orem’s self-care model by healthcare professionals as an effective strategy to enhance the QoL and well-being of elderly individuals.
Madmouli et al18 (2019) evaluated the effectiveness of Orem’s self-care model in improving QoL among patients with β-thalassemia major and demonstrated significant improvements in the mean scores of QoL dimensions within the intervention group. These findings align with the results of the present study. It is important to note that patients with thalassemia major not only face the financial burden of their condition but also frequently experience physical complications, reduced physical function, anxiety, depression, and limited familial support—all of which negatively impact their QoL. The study highlighted that Orem’s self-care model could significantly enhance the QoL of these patients compared with the pre-intervention phase.
In another study, Khademian et al11 (2020) examined the effect of Orem’s self-care nursing model on the QoL of patients with hypertension. Their findings indicated that self-care training based on Orem’s model could enhance the QoL of these patients. Specifically, the results showed that 8 weeks after the intervention, the mean QoL score was significantly higher in the experimental group than in the control group (106.5±26.5 vs 85.5±22.5; P=0.03). Nevertheless, no significant difference was observed immediately after the intervention (94.4±25.3 vs 87.2±22.8; P=0.32). Based on these findings, designing and implementing Orem’s self-care model to address the specific needs of patients with chronic diseases (eg, MI, heart failure, and hypertension), along with regular follow-ups, can effectively improve their QoL. Since significant improvements in QoL were noted 8 weeks post-intervention, it is crucial for nurses to actively follow up with patients and address their concerns.
The findings of the present study align with those of numerous other studies examining the effectiveness of Orem’s self-care model in enhancing QoL. For instance, it has been reported that self-care programs based on Orem’s model positively impacted the QoL of patients with migraine or multiple sclerosis, as well as those undergoing hemodialysis.19
In a study by Naroi et al7 (1390), the effect of Orem’s self-care model on the QoL of hemodialysis patients was evaluated. The results showed a significant increase in the overall mean QoL score following the implementation of the self-care program compared to the pre-intervention phase (56.65±4.98 vs 46.4±9.36; P=0.001). The researchers suggested that the low QoL scores observed in their patients could be due to insufficient self-care training provided by medical staff, the social characteristics of the patients, and their limited awareness of the disease, its treatments, complications, and self-care methods. In the present study, we observed that after self-care training, patients’ scores across all QoL dimensions significantly increased, aligning more closely with the scores reported in other similar studies. Active participation in treatment and care processes is essential to effectively manage disease-related problems and complications and enhance patients’ QoL. This requires increasing patients’ awareness, and self-care training serves as an effective tool to achieve this goal. Consistent with the findings of Naroei and colleagues, we noted relatively low QoL scores in our patients, underscoring the insufficient emphasis on self-care training for individuals with chronic diseases in nursing education. It is, therefore, crucial to enhance nurses’ knowledge and skills in self-care training, particularly through modern approaches such as Orem’s model, not only during their academic training but also via in-service education programs.
Consistent with our findings, the results of a study by Madmouli et al17 (2019) demonstrated that the application of Orem’s self-care model significantly improved the QoL of thalassemia patients compared with the control group. This finding suggests that these patients are at risk of ineffective self-management and, as a result, can benefit from self-care training and related counseling services.
In contrast to the findings of the present study, Davoodi et al17 (2007) examined the effect of a self-care training program on patients with esophageal cancer and reported no significant difference in the overall QoL score between the intervention and control groups. This discrepancy with our results may be attributed to differences in the types of diseases studied and the varying number of training sessions provided.
Zhou et al20 (2021) conducted a study to evaluate the effect of Orem’s self-care model on the QoL and rehabilitation of patients with acute coronary syndrome following percutaneous coronary intervention. Their results indicated that QoL was significantly higher in the intervention group than in the control group, highlighting the comprehensive effectiveness of Orem’s self-care model in improving various aspects of patients’ QoL.20 Similarly, in our study, we analyzed the emotional, physical, and social dimensions of QoL and found that patients in the intervention group scored higher in all these dimensions than the control group. In alignment with our findings, Zhou and colleagues reported that QoL scores across multiple dimensions—including general health, physiological performance, physical role, physical pain, vitality, social performance, emotional role, and mental health—were significantly higher in the intervention group than in the control group (P<0.05).
Our findings chime with those of Madmouli et al18 (2019), who examined the effect of self-care training on the QoL of patients with thalassemia major. In their study, the mean scores of QoL dimensions—including emotional health, physical health, social functioning, fatigue, emotional well-being, pain, and mental health—significantly increased in the intervention group. In contrast, these parameters either declined over time or remained unchanged in the control group. Notably, the intervention group demonstrated a significant improvement in the mean scores of these QoL dimensions compared to baseline levels.
Consistent with the results of the present study, Yildiz et al21 (2020) found that Orem’s training program significantly enhanced self-care practices and QoL dimensions in patients with coronary artery disease. The application of self-care theories in nursing practice helps systematize care planning and organizes professional knowledge within a conceptual framework, offering nurses a clear guide on what actions to take and why they are necessary. In concordance with Yildiz and colleagues’ findings, in our study, the mean QoL score post-intervention was significantly higher in the experimental group, both in within-group and between-group comparisons with the control group. Therefore, Orem-based educational programs can increase patients’ awareness of coronary artery disease, improve their lifestyle and healthy behaviors, and empower them to adopt self-care practices.
By providing consistent follow-up care for MI patients, it is possible to prevent further complications, enhance their recovery process, and take significant steps toward improving their QoL and life expectancy.22, 23 Additionally, implementing effective training programs can help reduce workplace violence against nurses, thereby improving both the quantity and quality of nursing care and fostering a more supportive and principled work environment.24, 25
The benefits of education include improving health outcomes, reducing medication errors, increasing life expectancy, enhancing the quality of care, and lowering mortality rates.26–30
Tieyan Zhu et al31 (2021) concluded that nursing interventions based on Orem’s model were highly effective for MI patients, significantly reducing their stress and anxiety. Similarly, in a national study conducted by Khademian et al32 (2020), the results demonstrated that education played a critical role in managing patients with heart conditions. The study recommended the use of Orem’s model for individuals with heart disease.
In a 2023 study conducted in Pakistan on MI patients using Orem’s care model, researchers found that nursing interventions were statistically significant and impactful.33
Limitations
The study faced several limitations, including the initial non-cooperation of caregivers due to concerns about their patients’ treatment. This issue was addressed by providing detailed explanations about the treatment process to alleviate their concerns. In addition, the timing of the study coincided with the onset of the COVID-19 pandemic, which led to a decrease in hospitalization rates among the elderly and prolonged the sampling process. Another challenge was the inability to access some participants due to incomplete or outdated contact information, which hindered their participation in the second stage of data collection.
Given the effectiveness of Orem’s self-care model in improving the QoL of MI patients, several future research directions are recommended. These include investigating the effect of Orem’s self-care model, with a focus on exercise, on depression levels in patients and the elderly; examining the impact of self-care education centered on self-efficacy on the QoL of patients and the elderly; exploring the role of children and other family members in fostering motivation and desire for self-care among patients and the elderly; assessing the influence of self-care on self-understanding and self-efficacy levels in patients and the elderly; and conducting a comparative study on the implementation of self-care programs in men and women with MI.
Conclusion
Our findings demonstrated that MI patients experienced poor QoL, and the application of Orem’s self-care model by nurses positively influenced the QoL and self-care abilities of these patients. Considering these results, implementing Orem’s model-based self-care programs for hospitalized MI patients is recommended as a cost-effective, nonpharmacological complementary method to enhance health-related QoL. This approach can also serve as an effective educational intervention to promote healthier lifestyles and accelerate patients’ return to their daily routines.
It is worth noting that in recent years, substantial efforts have been made to encourage people to adopt health-related self-care behaviors. Consequently, numerous patients and organizations have engaged in counseling and prioritizing self-care practices. In patient care, there is a growing emphasis on involving patients in treatment decision-making to encourage self-management of chronic conditions. Incorporating psychological training and self-management interventions is essential to ensure the successful implementation of these initiatives. The term “self-management” signifies the transfer of responsibility from healthcare professionals to patients themselves for the day-to-day management of their health conditions.
These programs have expanded over the years, leading to the development of “expert patient” programs in the United States and the United Kingdom.
Acknowledgments
This article is based on a master’s thesis in geriatric nursing and received approval under the ethics code IR.MEDILAM.REC.1401.151 from Ilam University of Medical Sciences.
Footnotes
Conflict of Interest
The authors declare no conflicts of interest related to this article.
Notes:
This paper should be cited as: Heidari M , Aazami S, Sayehmiri K , Taghinejad H. The Effect of Implementing Orem’s Self-Care Model on the Quality of Life of Patients with Myocardial Infarction: A Quasi-Experimental Study. J Teh Univ Heart Ctr 2024;19(S1):32-39.
References
- 1.Ghorbanibirgani A, Hakim A. editors. Quality of life in patients with myocardial infarction. CIRCULATION; 2012: LIPPINCOTT WILLIAMS & WILKINS TWO COMMERCE SQ, 2001 MARKET ST, PHILADELPHIA …. [Google Scholar]
- 2.Ojha N, Dhamoon AS, Chapagain R. Myocardial Infarction (Nursing). 2021. [PubMed] [Google Scholar]
- 3.Lyngå P. Self-care in patients with heart failure with emphasis on weight monitoring and interactive technology: Karolinska Institutet; (Sweden: ); 2012. [Google Scholar]
- 4.Shahrbabaki PM, Farokhzadian J, Hasanabadi Z. Effect of self-care education on patient’s knowledge and performance with heart failure. Procedia-Social and Behavioral Sciences. 2012;31:918–22. [Google Scholar]
- 5.Abd Elalem SM, Shehata O, Shattla SI. The effect of self-care nursing intervention model on self-esteem and quality of life among burn patients. Clin Nurs Stud. 2018;6(2):79–90. [Google Scholar]
- 6.Kang K, Gholizadeh L, Inglis SC, Han H-R. Interventions that improve health-related quality of life in patients with myocardial infarction. Quality of Life Research. 2016;25:2725–37. [DOI] [PubMed] [Google Scholar]
- 7.Naji A, Naroie S, Abdeyazdan G, Dadkani E. Effect of Applying Self-Care Orem Model on Quality of Life in the Patient under Hemodialysis. Zahedan Journal of Research in Medical Sciences. 2012;14(1):8-. [Google Scholar]
- 8.Martínez N, Connelly CD, Pérez A, Calero P. Self-care: A concept analysis. International journal of nursing sciences. 2021;8(4):418–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartweg DL, Metcalfe SA. Orem’s Self-Care Deficit Nursing Theory: Relevance and Need for Refinement. Nursing Science Quarterly. 2022;35(1):70–6. [DOI] [PubMed] [Google Scholar]
- 10.Mohammadpour A, Rahmati Sharghi N, Khosravan S, Alami A, Akhond M. The effect of a supportive educational intervention developed based on the Orem’s self-care theory on the self-care ability of patients with myocardial infarction: A randomised controlled trial. Journal of Clinical Nursing. 2015;24(11–12):1686–92. [DOI] [PubMed] [Google Scholar]
- 11.Khademian Z, Ara FK, Gholamzadeh S. The effect of self-care education based on Orem’s nursing theory on quality of life and self-efficacy in patients with hypertension: a quasi-experimental study. International journal of community based nursing and midwifery. 2020;8(2):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammadpor A, Rahmati Sharghi N, Khosravan S, Alami A. Investigating the level of self-care and supportiv eeducative needs of patients with myocardial infarction, based on Orem’s model. Journal of Research and Health. 2013;3(4):489–96. [Google Scholar]
- 13.Asadi-Lari M, Javadi HR, Melville M, Oldridge NB, Gray D. Adaptation of the MacNew quality of life questionnaire after myocardial infarction in an Iranian population. Health and quality of life outcomes. 2003;1(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dixon T, Lim LL-Y, Oldridge NB. The MacNew heart disease health-related quality of life instrument: reference data for users. Quality of life Research. 2002;11:173–83. [DOI] [PubMed] [Google Scholar]
- 15.Nekouei ZK, Yousefy A, Doost HTN, Manshaee G, Sadeghei M. Structural Model of psychological risk and protective factors affecting on quality of life in patients with coronary heart disease: A psychocardiology model. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences. 2014;19(2):90. [PMC free article] [PubMed] [Google Scholar]
- 16.Mahmoudi G, Fayazi S, Jahani S, Keikhaee B, Latifi M. The effect of self care program on quality of life in patients with sickle cell anemia. Jondi-Shapour Med Sci J. 2012;963. [Google Scholar]
- 17.Davoodi A, Rezazadeh H, Somi MH, Rahmani A, Dizaji SL, Bakhshian AA. Effect of educating self-care program on quality of life in patients with gastric cancer after gastrectomy in Tabriz Hospitals. Medical Journal of Tabriz University of Medical Sciences. 2012;34(1):48–55. [Google Scholar]
- 18.Madmoli Y, Salimi M, Madmoli M, Maraghi E, Pelarak F, Korkini N, et al. The effect of Orem self-care model on health-related quality of life of patients with thalassemia major. J Res Med Dent Sci. 2019;7(2):170–6. [Google Scholar]
- 19.Seifi K, Moghaddam HE. The effectiveness of self-care program on the life quality of patients with multiple sclerosis in 2015. Journal of the National Medical Association. 2018;110(1):65–72. [DOI] [PubMed] [Google Scholar]
- 20.Zhu T, Liu H, Han A, Gu H, Li X. Orem’s self-care to treat acute coronary syndrome after PCI helps improve rehabilitation efficacy and quality of life. American Journal of Translational Research. 2021;13(4):2752. [PMC free article] [PubMed] [Google Scholar]
- 21.Yildiz FT, Kasikci M. Impact of training based on Orem’s theory on self-care agency and quality of life in patients with coronary artery disease. J Nurs Res. 2020;28(6):e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Norozi S, Rai A, Salimi E, Tavan H. The incidence of major cardiovascular events relied on coronary vessels after angioplasty and stent types complications. Tehran University of Medical Sciences Journal. 2018;75(10):722–9. [Google Scholar]
- 23.Qavam S, Ahmadi MH, Tavan H, Yaghobi M, Mehrdadi A. High-sensitive C-reactive protein in patients with acute coronary syndrome in statin therapy and its impact on prognosis. Tehran University Medical Journal. 2016;74(4):289–96. [Google Scholar]
- 24.Sohrabzadeh M, Menati R, Tavan H, Mozafari M, Menati W. Survey on patient against female nurses and lack of reporting aggressive event in Ilam hospitals at 2012. ioh 2015; 12 (1):47–55 [Google Scholar]
- 25.Aivazi A.A., Tavan H. Prevalence of conceived violence against nurses at educational hospitals of Ilam, Iran, 2012. International Journal of Africa Nursing Sciences, 2, pp. 65–68 [Google Scholar]
- 26.Tavan H., Sayehmiri K., Taghinejad H., Mousavi Moghadam S.R.-M. Factor analysis of spiritual health from the Islam viewpoint. Iranian Journal of Public Health, 2015,44(11):1572–1573 [PMC free article] [PubMed] [Google Scholar]
- 27.Shi W, Ghisi GLM, Zhang L, Hyun K, Pakosh M, Gallagher R. A systematic review, meta-analysis, and meta-regression of patient education for secondary prevention in patients with coronary heart disease: Impact on psychological outcomes. Eur J Cardiovasc Nurs. 2022. Oct 14;21(7):643–654. doi: 10.1093/eurjcn/zvac001. PMID: 35134883. [DOI] [PubMed] [Google Scholar]
- 28.Shohani M., Tavan H. Factors affecting medication errors from the perspective of nursing staff. Journal of Clinical and Diagnostic Research, 2018,12(3): IC01–IC04 [Google Scholar]
- 29.Petrelli A, Sebastiani G, Di Napoli A, Macciotta A, Di Filippo P, Strippoli E, Mirisola C, d’Errico A. Education inequalities in cardiovascular and coronary heart disease in Italy and the role of behavioral and biological risk factors. Nutr Metab Cardiovasc Dis. 2022. Apr;32(4):918–928. doi: 10.1016/j.numecd.2021.10.022. Epub 2021 Nov 25. PMID: 35067447. [DOI] [PubMed] [Google Scholar]
- 30.Khaing W, Vallibhakara SA, Attia J, McEvoy M, Thakkinstian A. Effects of education and income on cardiovascular outcomes: A systematic review and meta-analysis. Eur J Prev Cardiol. 2017. Jul;24(10):1032–1042. doi: 10.1177/2047487317705916. Epub 2017 Apr 13. PMID: 28406328. [DOI] [PubMed] [Google Scholar]
- 31.Zhu T, Liu H, Han A, Gu H, Li X. Orem’s self-care to treat acute coronary syndrome after PCI helps improve rehabilitation efficacy and quality of life. Am J Transl Res. 2021. Apr 15;13(4):2752–2762. PMID: 34017438; PMCID: . [PMC free article] [PubMed] [Google Scholar]
- 32.Khademian Z, Kazemi Ara F, Gholamzadeh S. The Effect of Self Care Education Based on Orem’s Nursing Theory on Quality of Life and Self-Efficacy in Patients with Hypertension: A Quasi-Experimental Study. Int J Community Based Nurs Midwifery. 2020. Apr;8(2):140–149. doi: 10.30476/IJCBNM.2020.81690.0. PMID: 32309455; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sultan A, Khanum S. Effectiveness of Orem self-care theory intervention for improvement in self-care practices among Myocardial infarction patients; A quasi-Experimental study. J Postgrad Med Inst 2024;38(1):3–8. 10.54079/jpmi.38.1.3256 [DOI] [Google Scholar]


