Abstract
Purpose of Review
This article reviews alien hand, a neurological disorder that causes involuntary limb movements that appear to be purposeful. This review outlines the history that identified the three widely accepted forms of alien hand and their distinct clinical and neuroimaging findings. This material summarizes behavioral disturbances that can occur with alien hand but are seldom addressed in a single review article, including propensity for self-injury, pathological sexual behavior, alien hand activities during sleep, and communication disturbances of alien Quality. The article then presents other paroxysmal, involuntary disturbances that are not usually considered to be alien hand, despite their appearing to be purposeful. Finally, this article reviews all PubMed-listed articles from 2020 to mid-2025 that addressed either alien hand or limb, or anarchic hand, for trends in understanding and treating this illness.
Recent Findings
Meritorious advances in recent years included proposed checklists for the component behaviors for diagnosing alien hand, structured interviews for querying the patients’ experiences, and demonstrating white matter cerebral damage that extends far beyond the lesion boundaries that are identifiable on conventional structural brain MRI.
Summary
This review summarizes the diversity of the presentations of alien hand. Many behaviors that are encompassed by alien hand are not so far explained by clinical or experimental brain MRI findings.
Keywords: Alien hand, Anarchic hand, Diagonistic dyspraxia, Corpus callosotomy, Split-brain
Introduction
Origins, History of the Nomenclature
After Paul Broca’s seminal 1860 s finding that associated left hemispheric structural brain lesion with acquired aphasia, late-19th century neuroclinicians became alert for other remarkable and disabling behavioral disorders that also could be traced to verified brain disease, such as unilateral spatial neglect [1] and acquired alexia [2]. At the turn of the century, a peculiar motor behavior was newly described, which involved limb movements that were incorrect for the task that the patient was asked to perform or during spontaneous self-care activities [3, 4]. For example, a patient could reach for an object involuntarily, intermittently fail to move the limb despite being asked or wanting to move it, or move a pencil to the mouth instead to a sheet of paper following instruction to write [3]. Involuntary mutually antagonistic actions between the patient’s hands were also noted, such as purposely dressing oneself with one hand and simultaneously and involuntarily undressing with the other [5]. These abnormalities were not due to spasticity, tremor, or incoordination, but instead erroneous object selection or movement sequences. The general disturbance was called “apraxia,” coined in 1871 [6]. However, these aberrancies were exceptional because only one arm was affected in most instances, while the patients could control the other hand. The patients did not understand the source for the hand’s abnormal movement, despite its appearance of purpose. It also seemed to them that the hand behaved as if it had a mind of its own, as if it had its own purpose. The disturbances generally upset the patients.
These behaviors initially were observed in persons with midline brain tumors. In the 1940 s similar disturbances were observed in patients who had undergone elective corpus callosotomy (“split-brain” surgery, which longitudinally divides the corpus callosum) to alleviate intractable seizures [7, 8]. A more specific term was introduced, “diagonistic dyspraxia,” to refer to the mutually opposing activities between the hands, in which one hand obeyed the patient’s aware intent, while the other performed the opposite action (e.g., dressing vs. undressing) [9]. Decades later, Brion and Jedynak noted that similar patients perceived an apparent foreign presence that affected one of the hands following the onset of brain tumors. This involved either the sense of lacking self-ownership of one’s hand when it was voluntarily grasped by the other hand out of view, or in one case, gibberish printing of words by the left hand that was in view, unlike the other hand’s writing. The latter patient considered that his aberrant writing was produced as if by another individual. From these observations Brion and Jedynak coined the term “le signe de la main étrangère,” or in English, the sign of the foreign hand [10] for these two different behaviors.
Later in the 1970 s the American neurosurgeon Bogen also observed unilateral seemingly purposeful hand behavior that was dissociated from conscious intent following corpus callosotomy for some epileptic patients. Because these behaviors resembled those that had been noted in the 1940s by Akelaitis et al., Bogen referred to this not only by Brion and Jedynak’s term “la main étrangère” but also, in English translation, “alien hand” [11]. In 1981 the term “alien hand” entered the peer-reviewed journal literature following the observations of apparently autonomous and purposeful behavior by one hand following cerebral infarction [12]. This term then became widely adopted, with more than 260 articles listed in the PubMed research journal article registry that have used this term.
Starting in the 1980 s, observations were published of involuntary levitation or other posturing of a solitary limb without the patient’s immediate attention to it, and the patient’s perception of its seeming to have a purpose, dissociated from the patient’s sensing any agency. This, too, was initially called “alien hand” [13]. Subsequently a journal report of this behavior termed this instead as “alien limb,” and this term was presented along with other previously described instances of “alien hand” [14]. “Alien limb” then also became popular, with now 198 articles that have used this term being listed in PubMed.
In 1991 the Italian investigators Della Sala and colleagues recommended the alternate term “anarchic hand” because the earlier “alien hand” description by Brion and Jedynak was ambiguous. Della Sala et al. advocated their term because the patients with involuntary, seemingly purposeful action by one hand nonetheless did not deny self-ownership of it [15]. As of now the PubMed registry lists 28 articles that have used the term “anarchic hand.”
However, despite the recommendation by Della Sala et al., “alien hand” is the term that remains more often used for seemingly purposeful behavior by one hand, not consciously instigated by the patient, and with the patient’s impression that an outside entity controlled the limb. Other terms have been used for the same general behavior, including “wayward hand,” “capricious hand,” and “Dr. Strangelove hand” (the last coined for the undesired, seemingly purposeful right hand actions by the title character of the 1964 Stanley Kubrick film). “Alien leg” or “alien foot” also have been rarely described. In many instances the terms “alien hand” and “alien limb” were used interchangeably in the same article. These two terms thus have become synonymous with each other.
The Three Alien Hand Subtypes, and Related Subtypes
Although alien hand patients have shown diverse involuntary movements, three main disease subtypes have been proposed [16], which have conveniently organized these findings to facilitate identifying disabling behavioral patterns. These subtypes not only differ from each other clinically, but they are also associated with different anatomical areas of brain injury, located in different sites along the cerebral midline rostral-caudal axis. Feinberg et al. defined the first two in 1992 and recognized preliminary evidence for a third kind of alien hand [17].
-
i)
The frontal alien hand involves disinhibited grasping and squeezing objects within reaching distance and usually in view. Involuntary gripping of bedclothes can also occur [18, 19]. Often it is difficult for the patient, and even the examiner, to free the hand from the object. The alien hand behavior can be so extreme as risking self-injury, for example in one instance by reaching for a burning napkin, which had to be restricted by the patient’s other hand [20]. Damage to the contralateral medial frontal cortex is most often associated.
-
ii)
The callosal alien hand entails actions that are more complex than grasping or groping. This kind of alien hand can reverse actions voluntarily initiated with the other hand, such as turning the page of a book vs. closing the book by the other hand. Yet in other instances, the alien hand may perform a task unrelated to the actions done by the hand that was under cognizant control. For example, while one patient intentionally shaved himself, his other hand unzipped his jacket for no clear reason [21]. In addition, the hand may wildly misspell or omit letters when writing [5, 10, 15]. As with the frontal alien hand, the callosal alien hand can also risk self-injury, as for example the hand reaching for a hot pot while the patient is distracted by a different task [22] or the hand attempting to control the steering wheel in an erratic manner while the patient was safely controlling the car with the other hand [23]. As implied by the name, this form of hand follows injury to the corpus callosum or medial cortex adjacent to the callosum, generally farther back than the medial frontal cortex that is involved with frontal alien hand.
-
iii)
The posterior alien hand refers to a range of involuntary limb movements of purposeful appearance that include a substantial deficit in somesthesis. Late in the 20th century, well after the other forms of alien hand had been described, Levine and Rinn proposed a third alien hand kind in 1986 when they observed a patient who was hospitalized for an acute posterior cerebral artery territory infarction [24]. The features included poor contralateral cutaneous sensation of the arm, its movements interrupted by pauses, marked ataxic movements during voluntary reaching, and self-aimed involuntary movements. These latter movements could be potentially injurious, including pinching her other arm and knocking off her eyeglasses. The movements were aggravated by emotional upset, reduced during physical rehabilitation. The patient perceived her movements as if controlled by another entity, and she talked to the hand to try to control its movements.
In 1998 Ay et al. observed similar behaviors in another patient who had posterior cerebral infarction, including self-injurious movements [25]. They termed this “sensory alien hand.” Bundick and Spinella in 2000 described yet another similar patient, following posterior cerebral artery infarction, who had spontaneous levitation of the arm [26]. They termed the illness “posterior alien hand.”
As of now, “posterior alien hand” or limb have been reported in 16 articles in PubMed, most recently in 2024. One instance of “PCA [posterior cerebral artery] alien limb syndrome” was also reported. In contrast, six publications on “sensory alien hand” or limb have appeared, two of which were comments on prior articles, the last one in 2012. Consequently, “posterior alien hand” or limb have become the preferred terms for this behavioral pattern.
-
iv)
Mixed, multivariant, or combined alien hand. Many instances have been reported of multiple forms of alien hand within the same patient [27–37]. These findings thus demonstrate that although the various alien hand subtypes are characterized by cerebral injury in distinct different regions, in some cases focal cerebral injury can provoke multiple forms of alien hand, perhaps from more extensive injury.
-
v)
Bilateral alien hand has been occasionally noticed despite intact limb control at other times in the patient [38–46].
-
vi)
Alien leg or foot have been occasionally reported [45, 47–52]. These behaviors have included the discrepancy between the patient’s intended movement and the leg’s performance, involuntary foot tapping, or forcing the foot downward unwittingly while driving.
Aspects of Alien Hand Behavior, Seldom Reviewed
The following observations are presented here because they are rarely addressed in reviews. They are pertinent to consider possible mechanisms for alien hand and can extend one’s awareness for the scope of the disorder.
-
i)
Self-injury. Many studies have reported self-injury or risk of self-injury by the alien hand [15, 20, 24, 25, 48, 53–68]. Behaviors included self-slapping, choking, scratching the eye, reaching for scissors involuntarily, trying to drink from a too-hot cup, or battling for control of a steering wheel while driving.
-
ii)
Sleep. Many remarkable reports have indicated alien hand activity while the patients were sleeping or preparing to sleep [26, 55–57, 60–62, 65, 70–74]. These activities included self-directed groping, slapping, or choking, roving movements under the bedclothes, or arm levitation. The actions often awoke the patients.
-
iii)
Sexual behavior. Several case reports have indicated public self-scratching the genitals, lifting the skirt of a passerby, or touching a woman’s breasts or buttocks [15, 42, 67, 75–78]. The patients indicated that they had not willed these actions and were embarrassed.
-
iv)
Freezing of movement. Unintended interruption or impaired initiation of limb movement have often been reported in alien hand [3, 21, 29, 34, 45, 47, 48, 65, 78, 79].
-
v)
Freezing of decision. Persons with alien hand can show or complain with difficulty with decision making. Liepmann’s 1900 patient repeatedly picked up but then put down test blocks for no clear reason [5]. The case 2 patient reported by Akelaitis in 1944 showed the same behavior when attempting to buy bread [9]. Some patients complained of inability to decide between two opposing actions [52], even after resolution of intermanual conflict [80]. Another patient, who returned to work, found difficulty with decision making [81].
-
vi)
Alien communicative behavior. In some instances, alien hand patients uttered incorrect words repeatedly, to their frustration, or contradicted themselves or other individuals in their speech or gestures. Case 1 studied by Akelaitis felt compelled to contradict everything that was said to her by her mother [9]. Gasquoine’s patient complained of the inability to suppress speaking aloud some of his thoughts [42]. The case 3 patient studied by Nishikawa et al. was frustrated by stating the opposite of what she had intended to say [65]. Two other patients frequently self-contradicted verbally after corpus callosal surgery [82, 83]. A split-brain patient, upon saying the incorrect the name of a presented color, shook his head, and then changed his answer [84]. A patient following bilateral paracallosal infarcts pointed to the incorrect answer on a facial recognition test, while the other hand pointed to the correct answer [67]. A patient with callosal trauma was plagued by “conflicting thoughts” [85]. After a callosal infarction, a patient denied having seen a stimulus in his left visual field, but at the same time nodded [86].
Etiology and Epidemiology
Alien hand is reported most often following stroke or corticobasal degeneration [87]. One study found that alien hand could occur in 3% of patients with corpus callosum infarction [88]. Less often it has been noted to follow corpus callosum surgery, traumatic brain injury, subarachnoid hemorrhage, Creutzfeldt-Jakob disease, hereditary diffuse leukoencephalopathy, brain herniation, post-brain tumor excision, Parry-Romberg syndrome (progressive hemifacial atrophy), or Marchiafava-Bignami disease (cerebral atrophy from alcoholism). Even though corpus callosum agenesis, the congenital failure to develop the largest interhemispheric commissure, has only rarely been reported to occur with alien hand [48], one patient with corpus callosum agenesis was reported to have alien hand that resolved after discontinuing carbidopa/levodopa that had been prescribed to control tremor [89].
Alien hand is overwhelmingly described in adults. In a few instances alien hand has been reported in children [68, 90–92], as young as at age 9 years [93].
Natural Course
Following acute brain injury, alien hand tends to appear after a delay of days to weeks afterward (e.g [80, 94]). However, in one case alien hand appeared within minutes after a cerebral infarction had developed during recovery from bronchoscopy [29]. In contrast, in a young child, seven years elapsed after a stroke before alien hand appeared [68]. Recovery after acute brain injury generally occurs under a year (e.g [34, 80, 95]). In one case the alien hand resolved within hours of onset after a stroke [96]. Less often, the disturbance can persist for years after brain injury (e.g [43, 51, 54, 97]). The natural course of alien hand that occurs in neurodegenerative disease, such as corticobasal syndrome or Alzheimer disease, is not discussed in the literature.
Treatment
Owing to the rarity of alien hand, randomized treatment trials have not occurred. Treatment outcomes have instead been reported in single cases or small case series [16]. Conventional neurological rehabilitation efforts have been challenging and generally not successful [35, 98]. Mirror box training (where the patient looks at the mirror reflection of the good arm that practices motor tasks and superimposed over the impaired arm) has been associated with improvement [99], but without comparison to treatment as usual or other treatments. Redirecting attention from the hand that has repetitive grasping has had conflicting results [100, 101].
Hypothesized Mechanisms for Alien Hand
The rare occurrence of alien hand has prevented developing and testing theories for its etiology. Based on (1) associated clinical findings and (2) basic laboratory primate research, different pathophysiological mechanisms for the three kinds of alien hand are generally recognized. Frontal alien hand, commonly resulting from medial frontal lobe injury, has been considered to result from the physiological disinhibition of the ipsilateral parietal cortex, which is oriented to explore the surrounding space [102]. Callosal alien hand is generally thought to emerge from the loss of interhemispheric neural communication following injury to the brain’s largest commissure, the corpus callosum [17]. Consequently, this injury can divide consciousness, in effect, producing two independently functioning units that each entails comprehensive mechanisms for planning and directing movement, perception, and contemplation [103]. These two separate units may thus combat for control of the body and the surrounding environment. However, in general, only one cerebral hemisphere, more often the left hemisphere, has substantial verbal expression ability and mediates inner speech [104]. As a result, the patient may be unable to express insight on the decision making that is done by the other, “silent” hemisphere. The observations of alien communicative behavior, referred to above, are consistent with this mechanism. Posterior alien hand is widely thought to result from the disruption of somatosensory processing of cutaneous input coming from the contralateral limb. With reduction of this input, the affected hand may drift in space involuntarily, causing levitation [57].
There remain many other aspects of alien hand that are not explained, including the occasional self-attack of the hand owner’s body, impulsive and even dangerous maneuvers (e.g., wrestling for control of the steering wheel between the hands while the patient is driving), and the sudden interruption of the course of limb movement or the inability to initiate movement, despite the patient’s verbalized intent for doing so. The posterior alien hand entails more than drifting of the limb without somatosensory input to the brain, and yet the complex actions in the posterior alien hand subtype are not readily explained by deficient cutaneous sensitivity.
Cousins of Alien Hand
Alien hand stands out among the varieties of neurological symptoms and involuntary deficits that can follow brain illness in the awake individual. However, there is a large range of other involuntary, complex disturbances that can follow brain illness and resemble voluntary behavior. These also command clinical attention, but which are not referred to as alien hand. This may occur in part because the patients did not report the impression of an alternative entity taking control. There also has not been systematic evaluation for whether the patients had thought that they felt alienation. In some alien hand cases, alienation was also not described [61, 105]. These other disturbances are summarized in Table 1. Except for misoplegia, associated movement, and limb synkinesis, these behaviors reflect the environment’s apparently commandeering the patient’s actions, and in this manner similar to frontal and callosal alien hand.
Table 1.
Summary of spontaneous behaviors following brain illness not reported as alien behavior
| Behavior | Description | References |
|---|---|---|
| Misoplegia | Self-criticism and personification of an immobile limb, even physically punishing it | [106, 107] |
| Associated movement | Elbow flexion in an otherwise plegic arm, following yawning or cutaneous stimulation of the other arm | [108] |
| Limb synkinesis or synkinesia | Voluntary movement by one limb causes involuntary duplicated movement by another limb | [109] |
| Agonistic dyspraxia | Impaired hand involuntarily performs the action that was requested for the other hand | [110, 111] |
| Avoiding response | Fingers fan out or a limb withdraws upon presentation of a near stimulus | [40, 112–115] |
| Imitation or imitative behavior or echopraxia | Compulsive copying of another person’s action | [116] |
| Utilization behavior | Compulsive using a tool within reaching distance | [117] |
| Environmental dependency syndrome | Compulsive adopting an authoritative role appropriate for a professional or recreational setting, e.g., doctor’s office | [118–120] |
|
Functional neurological disorder |
Limb hyperkinesis or immobility provoked by formal examination or self-attention | [121] |
| Rooting | Turning the lips toward a stimulus when touched on the side of the mouth or presenting a visual stimulus near the face | [122] |
| Forced hyperphasia | Logorrhea prompted by a key word in conversation | [123] |
| Response-to-next-patient-stimulation | Automatically obeying instructions directed at a neighboring patient | [124] |
| Hyperlexia | Compulsive reading aloud material encountered in the environment | [125] |
Latest Progress in Alien Hand Research
This review summarizes research on the involuntary actions of the patients and not the failure to perceive self-ownership of one’s limb, the two behaviors that were recognized by Brion and Jedynak’s seminal research as part of the “sign of the foreign hand” [10]. This survey is directed at only actions because (1) current alien hand research emphasizes motor disturbances, rather than the somatosensory or perceptual impairments, and (2) these deficits are more likely to impair self-care. For research on the failure of bodily self-ownership, instead one can use the terms either “somatoparaphrenia” or “asomatognosia,” which are widely used [126]. The generally impaired awareness of one’s body or its parts can be formally assessed with a questionnaire to further research on impaired body self-ownership [127]. These efforts may help to disambiguate the term “alien hand.”
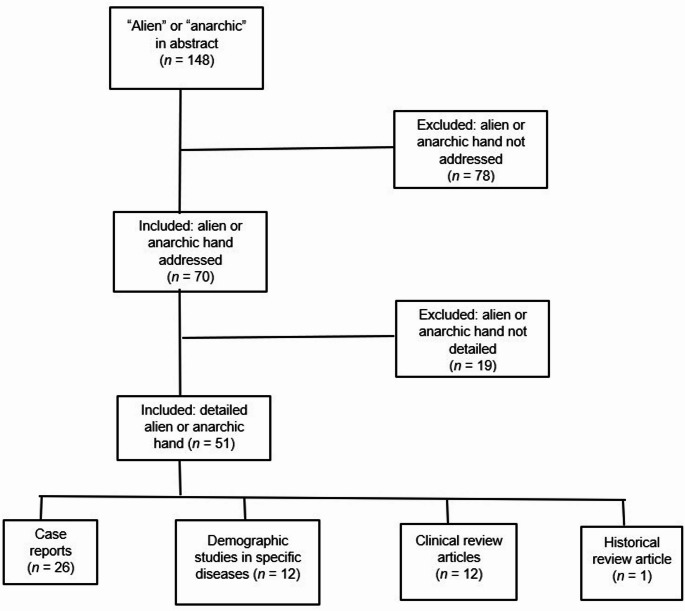
The author searched PubMed for articles that were published from 2020 to July 2025 whose abstracts included “alien” or “anarchic,” in any language. This yielded 148 articles (Fig. 1). The articles were carefully reviewed. Articles that did not describe an alien neurological disorder of any sort (e.g., “alien species,” “alien particles,” “anarchic urbanization”) were removed, which left 70 articles. Inspecting these articles led to removing those that mentioned alien or anarchic hand without describing pertinent clinical phenomena; this left 51 articles. These remaining articles then were categorized as either case reports (n = 26), epidemiological studies of specific neurological disorders that included alien or anarchic hand (n = 12), clinical reviews of alien or anarchic hand (n = 12), or a historic review of alien hand (n = 1). Outcomes of the literature review are summarized below.
Fig. 1.
PubMed search results for articles on either “alien hand’” or “anarchic hand,” 2020–2025
Results
Many of the case reports or series did not appreciably add to the knowledge from the literature. Several articles also reported outcomes from different kinds of neurological rehabilitation or medication. However, because these were case reports of a rare illness, they did not establish treatment efficacy and were unable to conduct randomized controlled trials.
On the other hand, this period saw an increase in experimental neuroimaging studies in alien hand, in particular, the use of diffusion tensor imaging [36, 95, 128, 129]. These studies add to the previous few reports, which find that the white matter structural changes in alien hand extend considerably beyond the boundaries of the focal changes that are visible in standard structural brain MRI. An improved understanding of the extent of structural brain injury in alien hand could improve modeling how structural damage can cause this disorder. In a different approach, a study of alien hand in persons with corticobasal syndrome (n = 16) found atrophy in cortical areas that were physiologically connected to the precuneus (based on functional maps that had been developed from healthy control subjects), unlike corticobasal syndrome patients without alien hand (n = 25) [130]. These findings accord with a prior study of stroke patients with alien hand, whose lesions were also physiologically connected with the precuneus [131]. These findings suggest that the precuneus is physiologically involved with disturbances in sensing self-agency in individuals who have involuntary limb movement disorders.
Other notable findings or patterns from this period:
Epidemiological studies: From 157 patients with corpus callosum infarction evaluated over 11 years at a single site, five had alien hand, thus an incidence of 3% [88]. In a second series, among 15 patients who had undergone corpus callosotomy to control refractory seizures, three had persisting callosal alien hand [81]. These individuals were exceptional because they were left-handed, and clinical testing established that both of their hemispheres participated in language, with more language ability in the left hemisphere (test results were not provided). The alien hand in each case was on the left. The results suggest that the condition can persist because the right hemisphere lacks the controlling input from the left hemisphere’s language mechanism that would otherwise restrict the right hemisphere’s operating the contralateral hand. It does not appear that the right hemisphere’s language ability in these patients alone could override contralateral alien hand. This special situation may arise because the patient’s dominant hand was the left hand.
Longitudinal studies: Exceptionally long periods between the onset of alien hand and diagnosing the underlying disease have occurred in a couple of reports. In the first case, the patient’s sole presenting symptom was callosal alien hand, without abnormalities on brain imaging apart from corpus callosum thinning [132]. The alien hand symptoms then resolved. Further work-up was not implemented until two years later, when the patient developed memory impairment, parkinsonian signs, and advanced cerebral atrophy. Genetic testing confirmed adult-onset leukoencephalopathy with axonal spheroids. In the second case, the patient presented with a cerebral infarction in the territory of the right middle cerebral artery and unilateral spatial and motor neglect [133]. These disturbances resolved after two months, but which were replaced by intermanual conflict. The latter condition faded after four months. A third case was exceptional because alien hand preceded the onset of hemiparesis, rather than the opposite sequence, which more often occurs when hemiparesis is associated with alien hand [73].
Developing a self-report assessment. To facilitate identifying patients with alien hand, Lewis-Smith et al. assembled a 13-item inventory by which to query patients for occurrence of this condition [134]. This included asking about mirror limb movements, limb levitation, touching objects within reaching distance without intending, and impaired sensing self-agency of movements. This appears to be the first publication of a comprehensive self-report battery to screen participants for alien hand studies.
A taxonomy for alien (or anarchic) hand behaviors. Pacella et al. have proposed the distinguishing and distinct phenomena of alien hand (though they use the term “anarchic hand”): apparently purposeful movements, non-purposeful movements that can include limb levitation and self-grabbing, “uncontrolled” bilateral involuntary movements that can include intermanual conflict and diagonistic dyspraxia, miscellaneous behaviors that include lack of response to command, and personification of the hand or sense of an extracorporeal entity guiding the movements [95]. This system may benefit future alien hand research to improve comparing studies to each other.
Unresolved developing a gold standard for diagnosing alien hand. For some investigators, the term “alien hand” requires the patient’s inability to recognize self-ownership of the hand, regardless of the patterns of movement disturbance [63, 95]. This insistence stems from the original research by Brion and Jedynak [10], who found several patients’ failure to recognize self-ownership of the hand after brain injury and coined the term “la main étrangère,” which later became re-titled as “alien hand.” Nonetheless, other investigators use the term “alien hand” or “alien limb” to refer to apparently goal-oriented involuntary limb movement without referring to absent self-ownership of the hand (e.g [72, 128]). In addition, “alien hand” or “alien limb” are often reported without commenting whether the patient had complained of sensing an alien presence guiding the hand, while indicating the involuntary, apparent goal-directed limb behavior (e.g [80, 100, 132, 135]).
Evidence for physiological interhemispheric disconnection after complete corpus callosotomy. While not a study of alien hand and did not report this disturbance, a recent paper found that patients who had undergone complete corpus callosotomy had absent interhemispheric synchronization of resting fMRI activity [136]. This observation supports that following callosotomy, the patients’ cerebral hemispheres can function independently from each other. This in turn supports understanding callosal alien hand behavior: the hemisphere that operates the contralateral, alien hand is without inhibition from the other hemisphere, because callosotomy blocks interhemispheric neural communication. Conflicting of actions initiated by each hemisphere, independently from each other, can thus be disabling.
Conclusions
The field of alien hand research is vibrant, with a steady output of about 12 peer-reviewed articles annually. This is remarkable for a rare neurological disorder. The illness continues to command neurological interest, which may lend insight for how impaired voluntary behavior can be caused by acquired brain injury and assist with managing this illness. However, the rare incidence of the illness impedes developing randomized controlled treatment trials. Consequently, treatment outcomes are anecdotal. Progress will remain slow.
Alien hand does not usually follow immediately after acute brain injury. Instead, usually several days or weeks elapse before the condition appears. This suggests that alien hand results from a slow, maladaptive physiological process during brain injury recovery, most likely because of neuroplastic cerebral reorganization. Such reorganization may well also support alien hand recovery under one year. Although the various forms of alien hand are associated with damage to specific brain regions, the rarity of the illness implies that lesion localization is not sufficient to account for its occurrence and characteristics. Of importance is that alien hand (1) only rarely occurs in children despite focal brain injury, and (2) almost never occurs in individuals with congenital corpus callosum agenesis. These observations suggest that brain development or maturation can influence alien hand.
Although alien hand is most often considered to be a disorder of active limb movement, many patients also demonstrate, paradoxically, paroxysmal motor or cognitive inactivity. The cause for this is not understood. Similarly, many other features of alien hand, summarized here, are not understood from reviewing the lesion characteristics or co-occurring signs, particularly self-injury, sexual behavior, occurrence during sleep, and communication disturbances. Another mystery is why alien hand is intermittent, while at other times the hand can comply with planned or requested movement. Still another unexplained aspect of callosal alien hand is the origination of diagonism (mutually opposite actions) and intermanual conflict (manual self-fighting to control self-care). These observations suggest that structural or physiological isolation of the cerebral hemispheres from each other can promote automatic oppositional or unwanted actions with the alien hand. This may not result from the “silent” hemisphere’s carefully and independently evaluating the patient’s needs, but rather from a reflexive state, in which the silent hemisphere impulsively reacts to the movements that are initiated by the other hemisphere and behaving at times inimical to the patient’s professed goals. The right cerebral hemisphere may be disposed to impulsive and rapid actions, as indicated by the several published observations that the alien left hand could launch into performing an action that was requested for the right hand before it could react [21, 52, 137]. This behavioral pattern accords with the many behaviors that are shown in Table 1, in which apparently autonomous manual behavior could be driven by features of the environment rather than careful decision making by the patient.
The large array of involuntary limb movements in Table 1 occurs without the patient’s reporting a foreign entity taking control of actions. Similarly, some alien hand case reports have not documented whether the patient had sensed alien control. These observations warrant systematic evaluation for whether these patients with behaviors in Table 1 truly consider these activities to be guided by an outside entity, or in contrast whether alien hand is a special condition in which the perception of self-agency can be dissociated from seemingly purposeful movements.
Different investigators prefer the terms “alien hand” vs. “anarchic hand” to describe seemingly purposeful limb actions for which the patient does not sense agency. Because “alien hand” is used more often, this term likely will remain the prevailing term.
Key References
- Pacella V, Bertagnoli S, Danese R, Bulgarelli C, Gobbetto V, Ricciardi GK, et al. Anarchy in the brain: behavioural and neuroanatomical core of the anarchic hand syndrome. Cortex 2025;182:181-94. https://doi.org/10.1016/j.cortex.2024.10.017.
- Identifies five key behavioral patterns of alien or anarchic hand.
- Lewis-Smith DJ, Wolpe N, Ghosh BCP, Rowe JB. Alien limb in the corticobasal syndrome: phenomenological characteristics and relationship to apraxia. J Neurol 2020;267:1147-1157. https://doi.org/10.1007/s00415-019-09672-8.
- Provides a checklist of behaviors that distinguish alien hand, to be used when querying patients who may have the disorder, to support investigation.
- Santander T, Bekir S, Paul T, et al. Full inter-hemispheric integration sustained by a fraction of posterior callosal fibers. bioRxiv 2025. https://doi.org/10.1101/2025.02.14.638327.
- Quantitative neuroimaging study of patients following corpus callosotomy, demonstrating physiological isolation of the cerebral hemispheres from each other.
Acknowledgements
Supported by a grant from the Heersink School of Medicine, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Author Contributions
V.W.M. wrote the manuscript text and prepared the figure.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights
All reported studies/experiments with humans performed by the author have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jackson JH. Case of large cerebral tumour without optic neuritis and with left hemiplegia and imperception. Roy Lond Ophthalmol Hosp Rep. 1876;8:434–44. [Google Scholar]
- 2.Dejerine J. Sur un cas de cécité verbale avec agraphie suivi d’autopsie. Mémoires De La Société De Biol. 1891;3:197–201. [in French]. [Google Scholar]
- 3.Van Vleuten CF. Linksseitige motorische Apraxie. Ein beitrag zur physiologie des Balkens. Z Psychiatr. 1907;64:203–39. [in German].
- 4.Goldstein K. Zur Lehre von der motorischen Apraxie. J Psychol Neurol. 1908;11:169–87. [Google Scholar]
- 5.Liepmann H. Das Krankheitsbild der Apraxie (motorischen Asymbolie). Auf Grund eines Falles von einseitiger Apraxie. Monatsschr Psychiatr Neurol. 1900;8:15–44. 102 – 32, 182 – 97 [in German]. [Google Scholar]
- 6.Steinthal H. Abriss der Sprachwissenschaft. Berlin: Ferd. Dümmler’s Verlagsbuchhandlung; 1871 [in German].
- 7.Van Wagenen WP, Herren RY. Surgical division of commissural pathways in the corpus callosum. Arch Neurol Psychiatry. 1940;44:740–59. [Google Scholar]
- 8.Smith KU, Akelaitis AJ. Studies on the corpus callosum. I. Laterality in behavior and bilateral motor organization in man before and after section of the corpus callosum. Arch Neurol Psychiatry. 1942;47:519–43. [Google Scholar]
- 9.Akelaitis AJ. Studies on the corpus callosum. IV. Diagonistic dyspraxia in epileptics following partial and complete section of the corpus callosum. Am J Psychiatry. 1944;101:594–9. [Google Scholar]
- 10.Brion S, Jedynak CP. Troubles du transfert interhemispherique (callosal disconnection). A propos de trois observations de tumeurs du corps calleux. Le signe de la main ètrangère. Rev Neurol (Paris). 1972;126:257–66. [in French]. [PubMed]
- 11.Bogen JE. The callosal syndrome. In: Heilman KM, Valenstein E, editors. Clinical neuropsychology. New York: Oxford; 1979. pp. 308–59. [Google Scholar]
- 12.Goldberg G, Mayer NG, Toglia JU. Medial frontal cortex infarction and the alien hand sign. Arch Neurol. 1981;38:683–6. 10.1001/archneur.1981.00510110043004. [DOI] [PubMed] [Google Scholar]
- 13.Brown JW. Frontal lobe syndromes [review]. Handb Clin Neurol. 1985;45:23–41. [Google Scholar]
- 14.Riley DE, Lang AE, Lewis A, Resch L, Ashby P, Hornykiewicz O, et al. Cortical-basal ganglionic degeneration. Neurology. 1990;40:1203–12. 10.1212/wnl.40.8.1203. [DOI] [PubMed] [Google Scholar]
- 15.Della Sala S, Marchetti C, Spinnler H. Right-sided anarchic (alien) hand: a longitudinal study. Neuropsychologia. 1991;29:1113–27. 10.1016/0028-3932(91)90081-i. [DOI] [PubMed] [Google Scholar]
- 16.Sarva H, Deik A, Severt WL. Pathophysiology and treatment of alien hand syndrome [review]. Tremor Other Hyperkinet Mov. 2014;4:241. 10.7916/D8VX0F48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feinberg TE, Schindler RJ, Flanagan NG, Haber LD. Two alien hand syndromes [review]. Neurology. 1992;42:19–24. 10.1212/wnl.42.1.19. [DOI] [PubMed] [Google Scholar]
- 18.Wilson SAK, Walshe FMR. The phenomenon of tonic innervation and its relation to motor apraxia. Brain. 1914;37:199–246. [Google Scholar]
- 19.Uchiyama S, Yoshino K, Ohka T, Uchiyama C. The alien hand sign associated with left anterior cerebral artery occlusion. Neurol Med. 1983;18:396–9. [Google Scholar]
- 20.Goldberg G, Bloom KK. The alien hand sign. Localization, lateralization and recovery. Am J Phys Med Rehabil. 1990;69:228–38. 10.1097/00002060-199010000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Tanaka Y, Yoshida A, Kawahata N, Hashimoto R, Obayashi T. Diagonistic dyspraxia. Clinical characteristics, responsible lesion and possible unerlying mechanism. Brain. 1996;119:859–73. 10.1093/brain/119.3.859. [DOI] [PubMed] [Google Scholar]
- 22.Gottlieb D, Robb K, Day B. Mirror movements in the alien hand syndrome. Am J Phys Med Rehabil. 1992;71:297–300. 10.1097/00002060-199210000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Leiguarda R, Starkstein S, Nogués M, Berthier M, Arbelaiz R. Paroxysmal alien hand syndrome. J Neurol Neurosurg Psychiatry. 1993;56(7):788–92. 10.1136/jnnp.56.7.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levine DN, Rinn WE. Opticosensory ataxia and alien hand syndrome after posterior cerebral artery territory infarction. Neurology. 1986;36:1094–7. 10.1212/wnl.36.8.1094. [DOI] [PubMed] [Google Scholar]
- 25.Ay H, Buonanno FS, Price BH, Le DA, Koroshetz WJ. Sensory alien hand syndrome: case report and review of the literature. J Neurol Neurosurg Psychiatry. 1998;65(3):366–9. 10.1136/jnnp.65.3.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bundick T, Spinella M. Subjective experience, involuntary movement, and posterior alien hand syndrome. J Neurol Neurosurg Psychiatry. 2000;68:83–5. 10.1136/jnnp.68.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan JL, Liu AB. Anatomical correlates of alien hand syndromes. Neuropsychiatry Neuropsychol Behav Neurol. 1999;12:149–55. [PubMed] [Google Scholar]
- 28.Lin JH, Kwan SY, Wu D. Mixed alien hand syndrome coexisting with left-sided extinction secondary to a left corpus callosal lesion: a case report. Mov Disord. 2007;22:248–51. 10.1002/mds.21241. [DOI] [PubMed] [Google Scholar]
- 29.Kloesel B, Czarnecki K, Muir JJ, Keller AS. Sequelae of a left-sided parietal stroke: posterior alien hand syndrome. Neurocase. 2010;16:488–93. 10.1080/13554794.2010.497154. [DOI] [PubMed] [Google Scholar]
- 30.Yuan JL, Wang SK, Guo XJ, Hu WL. Acute infarct of the corpus callosum presenting as alien hand syndrome: evidence of diffusion weighted imaging and magnetic resonance angiography. BMC Neurol. 2011;11:142. 10.1186/1471-2377-11-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Debray SBE, Demeestre J. Alien hand syndrome. Neurology. 2018;91:527. 10.1212/WNL.0000000000006172. [DOI] [PubMed] [Google Scholar]
- 32.Qu K, Gan L, Jiang W, Yu P, Dong M. Case report: good prognosis of mixed alien hand syndrome by verbal-cue rehabilitation exercise. Front Neurol. 2021;12:718706. 10.3389/fneur.2021.718706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matsuyama T, Hayashi K, Sato M, Suzuki A, Nakaya Y, Miura T, et al. Verbal-cue rehabilitation exercises are effective for the mixed callosal-frontal variant of alien hand syndrome following stroke. Cureus. 2024;16:e68564. 10.7759/cureus.68564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zainudin MF, Soo KF, Yin KN. Callosal disconnection syndrome manifesting as mixed frontal-callosal-posterior alien hand syndrome following extensive corpus callosum infarct. F1000 Res. 2024;12:529. 10.12688/f1000research.133838.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alvarez A, Weaver M, Alvarez G. Rehabilitation of alien hand syndrome complicated by contralateral limb apraxia. Am J Phys Med Rehabil. 2020;99:e122–4. 10.1097/PHM.0000000000001401. [DOI] [PubMed] [Google Scholar]
- 36.Pacella V, Ricciardi GK, Bonadiman S, Verzini E, Faraoni F, Scandola M, et al. The role of white matter disconnection in the symptoms relating to the anarchic hand syndrome: a single case study. Brain Sci. 2021;11: 632. 10.3390/brainsci11050632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sarkar P, Ray BK, Mukherjee D, Pandit A, Ghosh R, Benito-Leon J, et al. Alien limb phenomenon after diffuse corpus callosum ischemic stroke. Neurohospitalist. 2022;12(2):295–300. 10.1177/19418744211067033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Calmus A, Boyer F, Delmer F, Coulon JM, Tanguy MA, Étienne JC. Diagnostic positif d’une dyspraxie diagonistique et d’une main capricieuse: à propos d’un cas [abstract]. Ann Réadapt Méd Phys. 2005;48:425. [in French]. [Google Scholar]
- 39.Mark VW, Mc Alaster R, Laser KL. Bilateral alien hand [abstract]. Neurology. 1991;41(Suppl1):302. [Google Scholar]
- 40.FitzGerald DB, Drago V, Jeong Y, Chang YL, White KD, Heilman KM. Asymmetrical alien hands in corticobasal degeneration. Mov Disord. 2007;22:581–4. 10.1002/mds.21337. [DOI] [PubMed] [Google Scholar]
- 41.Ruggeri M, Biagioli C, Ricci M, Gerace C, Blundo C. Progressive aphasia, apraxia of speech and agraphia in corticobasal degeneration: a 12-case series clinical and neuropsychological descriptive study. Int J Lang Commun Disord. 2020;55:867–74. 10.1111/1460-6984.12559. [DOI] [PubMed] [Google Scholar]
- 42.Gasquoine PG. Bilateral alien hand signs following destruction of the medial frontal cortices. Neuropsychiatry Neuropsychol Behav Neurol. 1993;6:49–53. [Google Scholar]
- 43.Cantagallo A, Boldrini P. Bilateral anarchic hand in a single case report. J Neurol Rehabil. 1997;11:233–7. [Google Scholar]
- 44.McNabb AW, Carroll WM, Mastaglia FL. Alien hand and loss of bimanual coordination after dominant anterior cerebral artery territory infarction. J Neurol Neurosurg Psychiatry. 1988;51(2):218–22. 10.1136/jnnp.51.2.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shao J, Bai R, Duan G, Guan Y, Cui L, Deng H. Intermittent alien hand syndrome caused by Marchiafava-Bignami disease: a case report. Medicine (Baltimore). 2019;98:e16891. 10.1097/MD.0000000000016891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Riddoch MJ, Edwards MG, Humphreys GW, West R, Heafield T. Visual affordances direct action: neuropsychological evidence from manual interference. Cogn Neuropsychol. 1998;15:645–83. 10.1080/026432998381041. [DOI] [PubMed] [Google Scholar]
- 47.Chan JL, Chen RS, Ng KK. Leg manifestations in alien hand syndrome. J Formos Med Assoc. 1996;95:342–6. [PubMed] [Google Scholar]
- 48.Ridley B, Beltramone M, Wirsich J, Le Troter A, Tramoni E, Aubert S, et al. Alien hand, restless brain: salience network and interhemispheric connectivity disruption parallel emergence and extinction of diagonistic dyspraxia. Front Hum Neurosci. 2016;10: 307. 10.3389/fnhum.2016.00307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Haeri G, Saeedi Y, Haji Akhoundi F, Shoeibi A, Aghavali S, Emamikhah M, et al. Alien leg syndrome in two cases of corticobasal syndrome [letter]. Can J Neurol Sci. 2021;48:579–81. 10.1017/cjn.2020.238. [DOI] [PubMed] [Google Scholar]
- 50.Olszewska DA, McCarthy A, Murray B, Magennis B, Connolly S, Lynch T. A wolf in sheep’s clothing: an alien leg in corticobasal syndrome. Tremor Other Hyperkinet Mov. 2017;7:455. 10.7916/D86D5ZT8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Della Sala S, Marchetti C, Spinnler H. The anarchic hand: a fronto-mesial sign. In: Boller F, Grafman J, editors. Handbook of neuropsychology. Volume 9. Amsterdam: Elsevier; 1994. pp. 233–55. [Google Scholar]
- 52.Brainin M, Seiser A, Matz K. The mirror world of motor inhibition: the alien hand syndrome in chronic stroke. J Neurol Neurosurg Psychiatry. 2008;79:246–52. 10.1136/jnnp.2007.116046. [DOI] [PubMed] [Google Scholar]
- 53.Caplan LR. Top of the basilar syndrome. Neurology. 1980;30:72–9. 10.1212/wnl.30.1.72 [DOI] [PubMed] [Google Scholar]
- 54.Banks G, Short P, Martinez AJ, Latchaw R, Ratcliff G, Boller F. The alien hand syndrome. Clinical and postmortem findings. Arch Neurol. 1989;46:456–9. 10.1001/archneur.1989.00520400116030. [DOI] [PubMed] [Google Scholar]
- 55.Geschwind DH, Iacoboni M, Mega MS, Zaidel DW, Cloughesy T, Zaidel E. Alien hand syndrome: interhemispheric motor disconnection to a lesion in the midbody of the corpus callosum. Neurology. 1995;45:802–8. 10.1212/wnl.45.4.802 [DOI] [PubMed] [Google Scholar]
- 56.Nicholas JJ, Wichner MH, Gorelick PB, Ramsey MM. Naturalization of the alien hand: case report. Arch Phys Med Rehabil. 1998;79:113–4. 10.1016/s0003-9993(98)90218-0. [DOI] [PubMed]
- 57.Marey-Lopez J, Rubio-Nazabal E, Alonso-Magdalena L, Lopez-Facal S. Posterior alien hand syndrome after a right thalamic infarct. J Neurol Neurosurg Psychiatry. 2002;73:447–9. 10.1136/jnnp.73.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pack BC, Diamond KJS, Gale PT. Posterior-variant alien hand syndrome: clinical features and response to rehabilitation. Disabil Rehabil. 2002;24:817–8. 10.1080/09638280210142202. [DOI] [PubMed] [Google Scholar]
- 59.Ortega-Albás JJ, de Entrambasaguas M, Montoya FJ, Serrano AL, Geffner D. Sleep disorder in alien hand syndrome. Sleep Med. 2003;4:247–9. 10.1016/s1389-9457(02)00236-8. [DOI] [PubMed] [Google Scholar]
- 60.Terazzi E, Mittino D, Monaco F. Posterior alien hand in a left-handed person. BMJ Case Rep. 2010; 2010:bcr1020103401. 10.1136/bcr.10.2010.3401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Le K, Zhang C, Greisman L. Alien hand—a rare presentation of stroke. J Community Hosp Intern Med Perspect. 2020;10:149–50. 10.1080/20009666.2020.1756610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Russo M, Carrarini C, Dono F, Di Stefano V, De Angelis MV, Onofrj M, et al. Posterior variant of alien limb syndrome with sudden clinical onset as self-hitting associated with thalamic stroke. Case Rep Neurol. 2020;12:35–9. 10.1159/000503857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Murdoch M, Hill J, Barber M. Strangled by Dr Strangelove? Anarchic hand following a posterior cerebral artery territory ischemic stroke. Age Ageing. 2021;50:263–4. 10.1093/ageing/afaa129 [DOI] [PubMed] [Google Scholar]
- 64.Kikkert MA, Ribbers GM, Koudstaal PJ. Alien hand syndrome in stroke: a report of 2 cases and review of the literature. Arch Phys Med Rehabil. 2006;87:728–32. 10.1016/j.apmr.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 65.Nishikawa T, Okuda J, Mizuta I, Ohno K, Jamshidi J, Tokunaga H, et al. Conflict of intentions due to callosal disconnection. J Neurol Neurosurg Psychiatry. 2001;71:462–71. 10.1136/jnnp.71.4.462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Faber R, Azad A, Reinsvold R. A case of the corpus callosum and alien hand syndrome from a discrete paracallosal lesion. Neurocase. 2010;16:281–5. 10.1080/13554790903456217. [DOI] [PubMed] [Google Scholar]
- 67.Hendry MA, Holliday SL. Alien hand syndrome: diagnosis of disconnection through behavioral observations and bimanual testing [abstract]. Arch Clin Neuropsychol. 1996;11:399–400. [Google Scholar]
- 68.Soman T, Steeves TD, Lang AE. Alien hand syndrome and dystonia in a pediatric patient [letter]. Mov Disord. 2009;24:1557–9. 10.1002/mds.22620. [DOI] [PubMed] [Google Scholar]
- 69.Dolado AM, Castrillo C, Urra DG, de Seijas EV. Alien hand sign or alien hand syndrome? [Letter]. J Neurol Neurosurg Psychiatry. 1995;59:100–1. 10.1136/jnnp.59.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ventura MG, Goldman S, Hildebrand J. Alien hand syndrome without a corpus callosum lesion. J Neurol Neurosurg Psychiatry. 1995;58(6):735–7. 10.1136/jnnp.58.6.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Giovannetti T, Buxbaum LJ, Biran I, Chatterjee A. Reduced endogenous control in alien hand syndrome: evidence from naturalistic action. Neuropsychologia. 2005;43:75–88. 10.1016/j.neuropsychologia.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 72.Higgins K, Gandelman S, Menko J. Alien hand syndrome: an atypical presentation of acute left parietal stroke in a community emergency department. Am J Emerg Med. 2024;82:214.e1-.e3. 10.1016/j.ajem.2024.06.027. [DOI] [PubMed]
- 73.Rashwan G, Elagha S, Aldaham T, Thomas L. Alien hand unveiled in a patient with right middle cerebral artery stroke. Cureus. 2024;16:e52552. 10.7759/cureus.52552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ong Hai BJ, Odderson IR. Involuntary masturbation as a manifestation of stroke-related alien hand syndrome. Am J Phys Med Rehabil. 2000;79:395–8. 10.1097/00002060-200007000-00012. [DOI] [PubMed] [Google Scholar]
- 75.Bejot Y, Caillier M, Osseby GV, Didi R, Ben Salem D, Moreau T, et al. Involuntary masturbation and hemiballismus after bilateral anterior cerebral artery infarction. Clin Neurol Neurosurg. 2008;110:190–3. 10.1016/j.clineuro.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 76.Cantagallo A, Spinazzola L, Rabuffetti M, Della Sala S. Verbal commands help the execution of endogenous movements in anarchic hand. Neuropsychol Rehabil. 2010;20:406–22. 10.1080/09602010903345298. [DOI] [PubMed] [Google Scholar]
- 77.Amalnath SD, Subramanian R, Dutta TK. The alien hand sign. Ann Indian Acad Neurol. 2013;16:9–11. 10.4103/0972-2327.107671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Barbizet J, Degos JD, Lejeune A, Leroy A. Syndrome de dysconnexion inter-hémiphèrique avec dyspraxie diagonstique au cours d’une maladie de Marchiafava-Bignami. Rev Neurol (Paris). 1978;134:781–9. [PubMed] [Google Scholar]
- 79.Rohde S, Weidauer S, Lanfermann H, Zanella F. Posterior alien hand syndrome: case report. Neuroradiology. 2002;44:921–3. 10.1007/s00234-002-0839-2. [DOI] [PubMed] [Google Scholar]
- 80.Kouassi LK, Essoin-De Souza ANT, Beuseize RAM, Abbé SA. Late detection of corpus callosum infarction in a 55-year-old: insights from alien hand syndrome. Am J Case Rep. 2025;26:e947514. 10.12659/AJCR.947514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Helmstaedter C, Solymosi L, Kurthen M, Momjian S, Schaller K. Dr. Strangelove demystified: disconnection of hand and language dominance explains alien-hand syndrome after corpus callosotomy. Seizure. 2021;86:147–51. 10.1016/j.seizure.2021.02.013 [DOI] [PubMed] [Google Scholar]
- 82.Poncet M, Chérif AA, Choux M, Boudouresques J, Lhermitte F. Étude neuropsychologique d’un syndrome de déconnexion calleuse totale avec hémianopsie latérale homonyme droite. Rev Neurol (Paris). 1978;134:633–53. [PubMed] [Google Scholar]
- 83.Mark VW. Verbal diagonistic behavior in a commissurotomized subject [abstract]. J Clin Exp Neuropsychol. 1990;12:96. [Google Scholar]
- 84.Gazzaniga MS. The bisected brain. New York: Appleton-Century-Crofts; 1970. [Google Scholar]
- 85.Plas J, Brion F, Jeanneau A, Chevalier JF, Dussaux P, Brion S. Les contradictions d’origine calleuse. Comportement psychiatrique contradictoire après lésion traumatique de la partie antérieure du corps calleux. Rev Neurol (Paris). 1999;155:569–74. [in French]. [PubMed] [Google Scholar]
- 86.Lausberg H, Davis M, Rothenhäusler A. Hemispheric specialization in spontaneous gesticulation in a patient with callosal disconnection. Neuropsychologia. 2000;38:1654–63. 10.1016/s0028-3932(00)00071-3. [DOI] [PubMed] [Google Scholar]
- 87.Graff-Radford J, Rubin MN, Jones JT, Aksamit AJ, Ahlskog JE, Knopman DS, et al. The alien limb phenomenon. J Neurol. 2013;260:1880–8. 10.1007/s00415-013-6898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ma Y, Liu Y, Yan X, Ouyang Y. Alien hand syndrome, a rare presentation of corpus callosum and cingulate infarction. J Neurol Sci. 2023;452: 120739. 10.1016/j.jns.2023.120739. [DOI] [PubMed] [Google Scholar]
- 89.Krause M, Shou J, Joy S, Torres-Russotto D. Alien limb syndrome induced by a dopamine agonist in a patient with parkinsonism and agenesis of the corpus callosum [letter]. Parkinsonism Relat Disord. 2017;39:91–2. 10.1016/j.parkreldis.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 90.Boesebeck F, Ebner A. Paroxysmal alien limb phenomena due to epileptic seizures and electrical cortical stimulation. Neurology. 2004;63:1725–7. 10.1212/01.wnl.0000143064.81746.e9. [DOI] [PubMed] [Google Scholar]
- 91.Basu AP, Taylor PN, Lowther E, Forsyth EO, Blamire AM, Forsyth RJ. Structural connectivity in a paediatric case of anarchic hand syndrome. BMC Neurol. 2015;15:234. 10.1186/s12883-015-0477-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Haq IU, Malaty IA, Okun MS, Jacobson CE, Fernandez HH, Rodriguez RR. Clonazepam and botulinum toxin for the treatment of alien limb phenomenon. Neurologist. 2010;16:106–8. 10.1097/NRL.0b013e3181a0d670. [DOI] [PubMed] [Google Scholar]
- 93.Takenouchi T, Solomon GE. Alien hand syndrome in Parry-Romberg syndrome. Pediatr Neurol. 2010;42:280–2. 10.1016/j.pediatrneurol.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 94.Lawson McLean AC, Lobsien E, Leinisch E, Lobsien D. Alien hand syndrome in ruptured aneurysms: case report and review of the literature. Neuroradiology. 2022;64:2091–4. 10.1007/s00234-022-03025-5. [DOI] [PubMed] [Google Scholar]
- 95.Pacella V, Bertagnoli S, Danese R, Bulgarelli C, Gobbetto V, Ricciardi GK, et al. Anarchy in the brain: behavioural and neuroanatomical core of the anarchic hand syndrome. Cortex. 2025;182:181–94. 10.1016/j.cortex.2024.10.017. [DOI] [PubMed] [Google Scholar]
- 96.Liu HC, Apramian A, Liu A. A case of transient alien hand syndrome from a very small ischemic stroke. Clin Case Rep. 2020;8:2204–7. 10.1002/ccr3.3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ferguson SM, Rayport M, Corrie WS. Neuropsychiatric observations on behavioral consequences of corpus callosum section for seizure control. In: Reeves AG, editor. Epilepsy and the corpus callosum. New York: Plenum; 1985. pp. 501–14. [Google Scholar]
- 98.Nowak DA, Bösl K, Lüdemann-Podubecka J, Gdynia HJ, Ponfick M. Recovery and outcome of frontal alien hand syndrome after anterior cerebral artery stroke. J Neurol Sci. 2014;338:203–6. 10.1016/j.jns.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 99.Stevens R, Svenningsen ALV, Olesen C, Middelhede R. Rehabilitering af alienhåndsyndrom. Ugeskr Læger. 2025;187:V10240672. [in Danish]. 10.61409/V10240672 [DOI] [PubMed] [Google Scholar]
- 100.Bru I, Verhamme L, de Neve P, Maebe H. Rehabilitation of a patient with alien hand syndrome: a case report of a 61-year old man. J Rehabil Med. 2021;4: 1000050. 10.2340/20030711-1000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nowak DA, Engel A, Leutbecher M, Zeller C. Alien limb phenomenon following posterior cerebral artery stroke: a distinct clinical entity. J Neurol. 2020;267:95–9. 10.1007/s00415-019-09543-2. [DOI] [PubMed] [Google Scholar]
- 102.Mesulam MM. Frontal cortex and behavior [editorial]. Ann Neurol. 1986;19:320–5. 10.1002/ana.410190403. [DOI] [PubMed] [Google Scholar]
- 103.Volz LJ, Gazzaniga MS. Interaction in isolation: 50 years of insights from split-brain research [review]. Brain. 2017;140:2051–60. 10.1093/brain/awx139. [DOI] [PubMed] [Google Scholar]
- 104.Alderson-Day B, Fernyhough C. Inner speech: development, cognitive functions, phenomenology, and neurobiology [review]. Psychol Bull. 2015;141:931–65. 10.1037/bul0000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lin GL, Yu XQ, Cai HY, Zhou RY, Li XT, Zhang X, et al. Case report: reversible alien hand syndrome caused by cerebral infarction. Front Hum Neurosci. 2025;19:1551539. 10.3389/fnhum.2025.1551539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Critchley M. Misoplegia, or hatred of hemiplegia. Mt Sinai J Med. 1974;41:82–7. [PubMed] [Google Scholar]
- 107.Delgado MG, Bogousslavsky J. Misoplegia [review]. Front Neurol Neurosci. 2018;41:23–7. 10.1159/000475689. [DOI] [PubMed] [Google Scholar]
- 108.Blin O, Rascol O, Azulay JP, Serratrice G, Nieoullon A. A single report of hemiplegic arm stretching related to yawning: further investigation using apomorphine administration. J Neurol Sci. 1994;126:225–7. 10.1016/0022-510x(94)90278-x. [DOI] [PubMed] [Google Scholar]
- 109.Kojović M, Bhatia KP. Bringing order to higher order motor disorders [review]. J Neurol. 2019;266:797–805. 10.1007/s00415-018-8974-9. [DOI] [PubMed] [Google Scholar]
- 110.Aboitiz F, Carrasco X, Schröter C, Zaidel D, Zaidel E, Lavados M. The alien hand syndrome: classification of forms reported and discussion of a new condition. Neurol Sci. 2003;24:252–7. 10.1007/s10072-003-0149-4. [DOI] [PubMed] [Google Scholar]
- 111.Lavados M, Carrasco X, Peña M, Zaidel E, Zaidel D, Aboitiz F. A new sign of callosal disconnection syndrome: agonistic dyspraxia. A case study. Neurocase. 2002;8:480–3. 10.1076/neur.8.5.480.16178. [DOI] [PubMed] [Google Scholar]
- 112.Castaigne P, Laplane D, Degos JD, Augustin P. Comportement tonique d’évitement d’origine sous-corticale. Rev Neurol (Paris). 1971;124:166–8. [in French]. [PubMed] [Google Scholar]
- 113.Laplane D, Meininger V, Bancaud J, Talairach J, Broglin D. Contribution a l’étude anatomo-clinique des phénomènes d’évitement. Rev Neurol (Paris). 1979;135:775–87. [PubMed] [Google Scholar]
- 114.Denny-Brown D. The nature of apraxia. J Nerv Ment Dis. 1958;126:9–32. [DOI] [PubMed] [Google Scholar]
- 115.Lechevalier B, Andersson JC, Morin P. Hemispheric Disconnection syndrome with a ‘crossed avoiding’ reaction in a case of Marchiafava-Bignami disease. J Neurol Neurosurg Psychiatry. 1977;40:483–97. 10.1136/jnnp.40.5.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dankinas D, Melynyte S, Siurkute A, Dapsys K. Pathological imitative behavior and response preparation in schizophrenia. Arch Clin Neuropsychol. 2017;32:533–40. 10.1093/arclin/acx034. [DOI] [PubMed] [Google Scholar]
- 117.Iaccarino L, Chieffi S, Iavarone A. Utilization behavior: what is known and what has to be known? [Review]. Behav Neurol. 2014;2014:297128. 10.1155/2014/297128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lhermitte F. Human autonomy and the frontal lobes. Part II: patient behavior in complex and social situations: the environmental dependency syndrome. Ann Neurol. 1986;19:335–43. 10.1002/ana.410190405. [DOI] [PubMed] [Google Scholar]
- 119.Eslinger PJ, Warner GC, Grattan LM, Easton JD. Frontal lobe utilization behavior associated with paramedian thalamic infarction. Neurology. 1991;41:450–2. 10.1212/wnl.41.3.450. [DOI] [PubMed] [Google Scholar]
- 120.Hoffmann MW, Bill PLA. The environmental dependency syndrome, imitation behaviour and utilisation behaviour as presenting symptoms of bilateral frontal lobe infarction due to Moyamoya disease. S Afr Med J. 1992;81:271–3. [PubMed] [Google Scholar]
- 121.Mark VW. Functional neurological disorder: extending the diagnosis to other disorders, and proposing an alternate disease term—Attentionally-modifiable disorder. NeuroRehabilitation. 2022;50:179–207. 10.3233/NRE-228003. [DOI] [PubMed] [Google Scholar]
- 122.Schott JM, Rossor MN. The grasp and other primitive reflexes [review]. J Neurol Neurosurg Psychiatry. 2003;74: 558 – 60. 10.1136/jnnp.74.5.558 [DOI] [PMC free article] [PubMed]
- 123.Beschin N, Catani M, Della Sala S, Compulsive hyperphasia. Cortex. 2022;153:143–5. 10.1016/j.cortex.2022.05.003. [DOI] [PubMed] [Google Scholar]
- 124.Bogousslavsky J, Regli F. Response-to-next-patient-stimulation: a right hemisphere syndrome. Neurology. 1988;38:1225–7. 10.1212/wnl.38.8.1225. [DOI] [PubMed] [Google Scholar]
- 125.Vuilleumier P, Staub F, Assal G. Sniffing behaviour, or recognizing a lily by smell, but not recognizing a sock on sight. Cortex. 1997;33:571–7. 10.1016/s0010-9452(08)70238-7. [DOI] [PubMed] [Google Scholar]
- 126.Vallar G. Body schema and body image as internal representations of the body, and their disorders. An historical review. J Neuropsychol. 2025;19(Suppl 1):8–25. 10.1111/jnp.12389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Konik S, Beaud V, Fellrath J, Martinelli I, Guanziroli E, Molteni F, et al. Evaluation of upper limb perception after stroke with the new affected limb perception questionnaire (ALPQ): a study protocol. BMC Neurol. 2024;24:196. 10.1186/s12883-024-03648-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sugawara K, Takeuchi T, Harada K, Taki M, Fujimura I, Kogami Y, et al. Self-restraint in a patient with alien hand syndrome following cerebral infarction involving the anterior cerebral artery territory. Front Neurol. 2023;14:1203450. 10.3389/fneur.2023.1203450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Park J, Tae WS, Lee S, Pyun SB. White matter tract involvement in anarchic hand syndrome following stroke: diffusion tensor imaging study. Behav Brain Res. 2025;485: 115529. 10.1016/j.bbr.2025.115529. [DOI] [PubMed] [Google Scholar]
- 130.Tetreault AM, Phan T, Petersen KJ, Claassen DO, Neth BJ, Graff-Radford J, et al. Network localization of alien limb in patients with corticobasal syndrome. Ann Neurol. 2020;88:1118–31. 10.1002/ana.25901. [DOI] [PubMed] [Google Scholar]
- 131.Darby RR, Joutsa J, Burke MJ, Fox MD. Lesion network localization of free will. Proc Natl Acad Sci U S A. 2018;115:10792–7. 10.1073/pnas.1814117115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chung B, Kim M, Kim S, Kang H. A case of adult-onset leukoencephalopathy with axonal spheroids and pigmented glia presenting with alien hand syndrome [letter]. eNeurolSci. 2022;30:100441. 10.1016/j.ensci.2022.100441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wan Yusoff WR, Hanafi MH, Ibrahim AH, Kassim NK, Suhaimi A. Unilateral neglect or alien hand syndrome? A diagnostic challenge. J Taibah Univ Med Sci. 2021;16:288–91. 10.1016/j.jtumed.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lewis-Smith DJ, Wolpe N, Ghosh BCP, Rowe JB. Alien limb in the corticobasal syndrome: phenomenological characteristics and relationship to apraxia. J Neurol. 2020;267:1147–57. 10.1007/s00415-019-09672-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zalyalova ZA, Munasipova SE. Lobno-visochnaya dementsiya s kortikobazal’nym sindromom. Zh Nevrol Psikhiatr Im S S Korsakova. 2022;122:107–14 [in Russian]. 10.17116/jnevro2022122021107 [DOI] [PubMed]
- 136.Santander T, Bekir S, Paul T, Simonson JM, Wiemer VM, Skinner HE et al. Full inter-hemispheric integration sustained by a fraction of posterior callosal fibers. bioRxiv. 2025. 10.1101/2025.02.14.638327
- 137.Fisher CM. Symmetrical mirror movements and left ideomotor apraxia. Trans Am Neurol Assoc. 1963;88:214–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.