Abstract
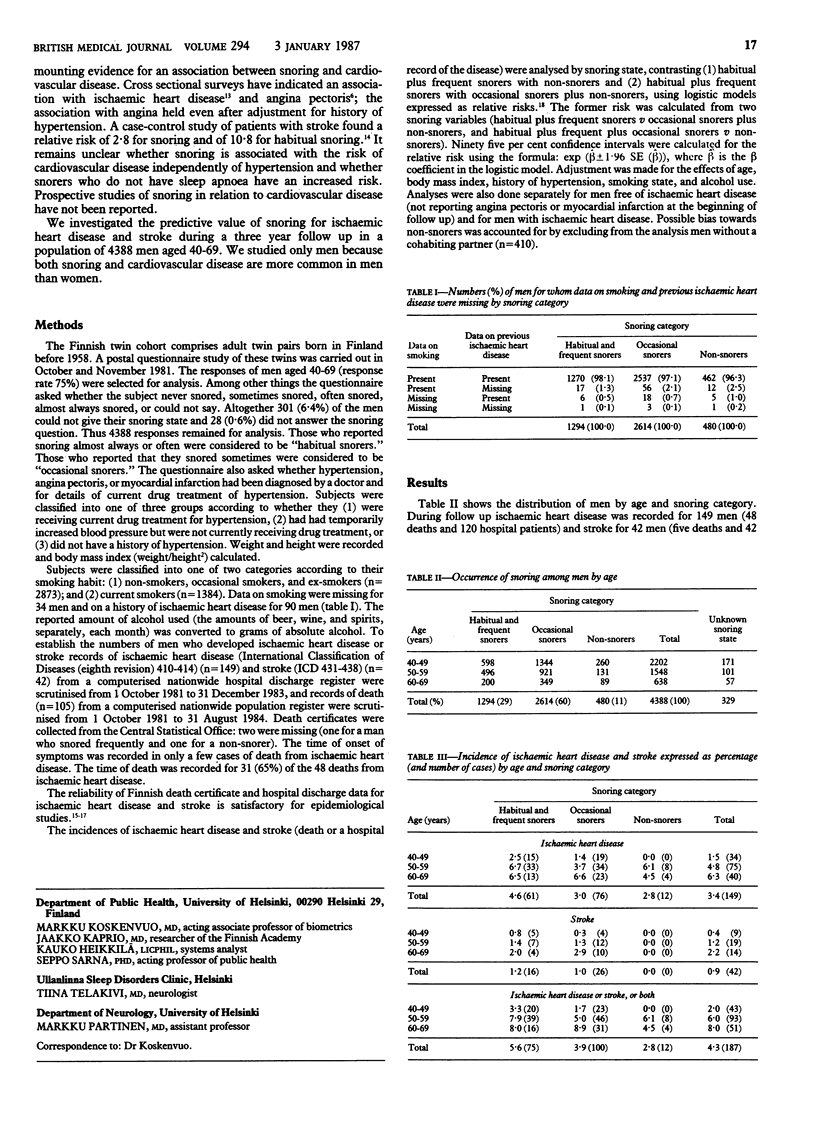
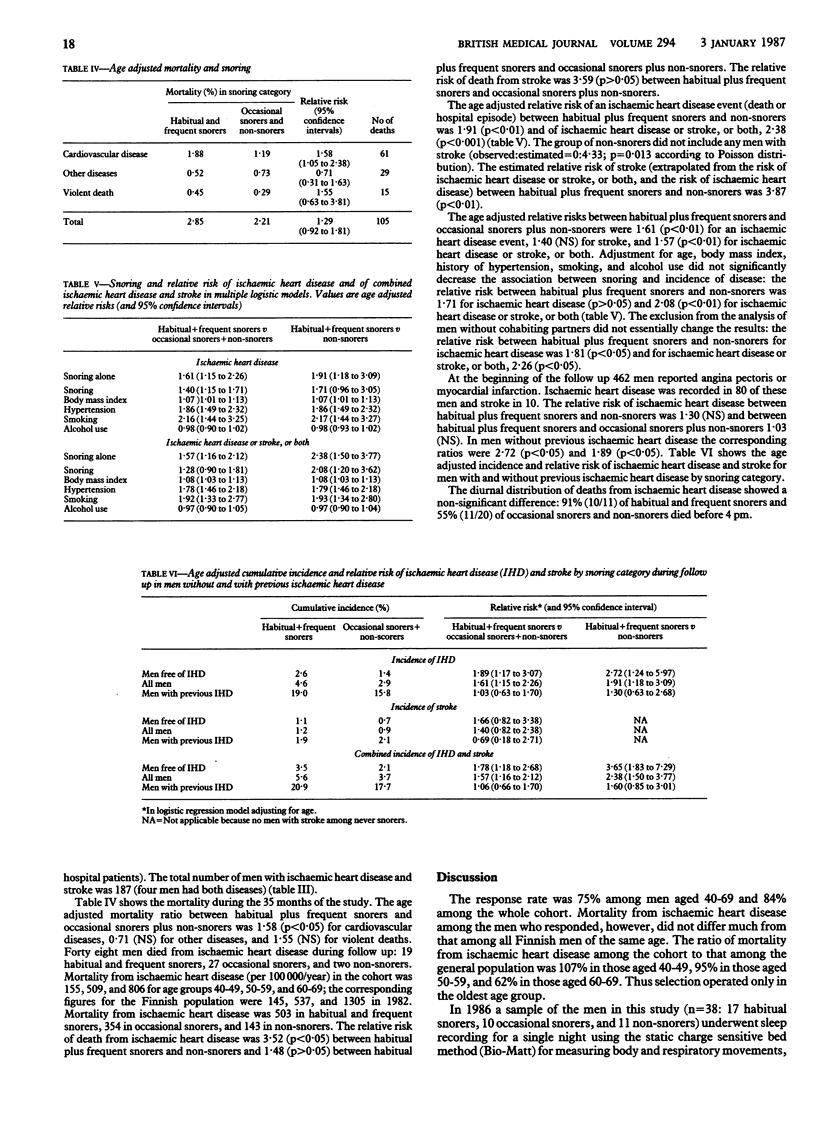
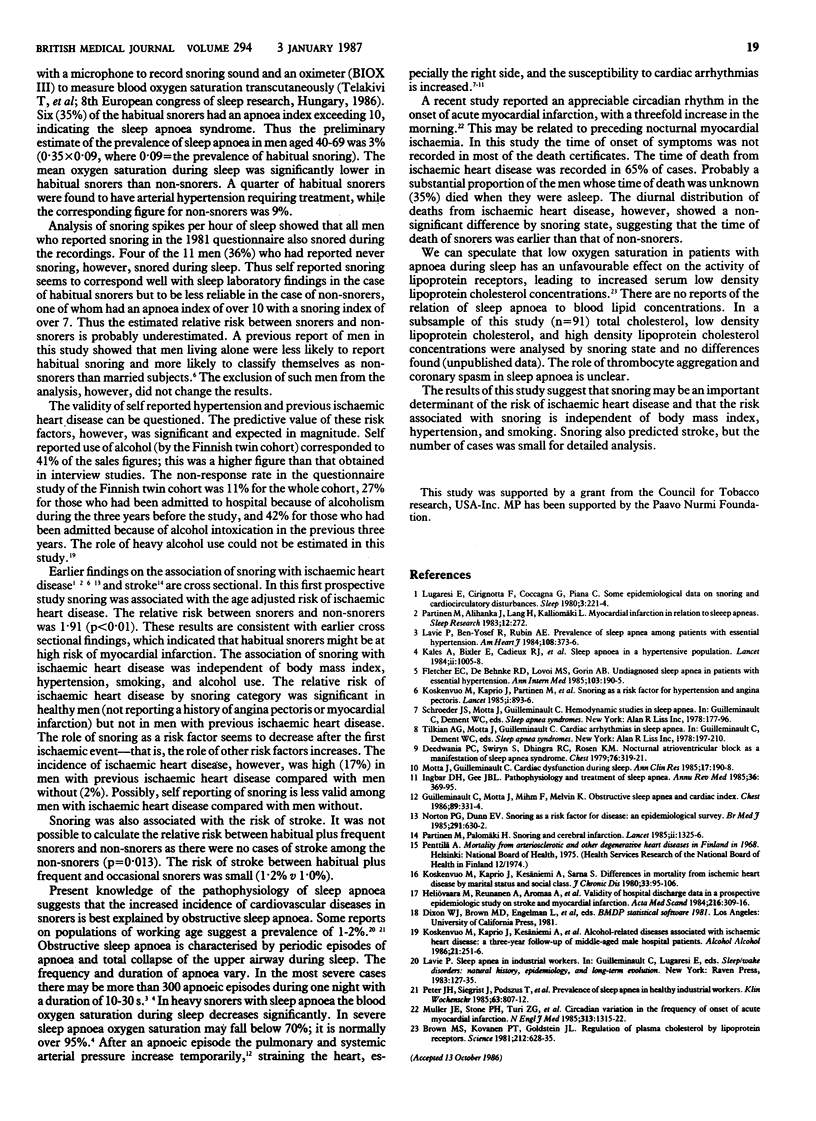
The association of snoring with ischaemic heart disease and stroke was studied prospectively in 4388 men aged 40-69. The men were asked, in a questionnaire sent to them, whether they snored habitually, frequently, occasionally, or never. Hospital records and death certificates were checked for the next three years to establish how many of the men developed ischaemic heart disease or stroke: the numbers were 149 and 42, respectively. Three categories of snoring were used for analysis: habitual and frequent snorers (n = 1294), occasional snorers (n = 2614), and non-snorers (n = 480). The age adjusted relative risk of ischaemic heart disease between habitual plus frequent snorers and non-snorers was 1.91 (p less than 0.01) and for ischaemic heart disease or stroke, or both, 2.38 (p less than 0.001). There were no cases of stroke among the non-snorers. Adjustment for age, body mass index, history of hypertension, smoking, and alcohol use did not significantly decrease the relative risks, which were 1.71 (p greater than 0.05) for ischaemic heart disease and 2.08 (p less than 0.01) for ischaemic heart disease and stroke combined. At the beginning of follow up in 1981, 462 men reported a history of angina pectoris or myocardial infarction. For them the relative risk of ischaemic heart disease between habitual plus frequent snorers and non-snorers was 1.30 (NS); for men without previous ischaemic heart disease 2.72 (p less than 0.05). Snoring seems to be a potential determinant of risk of ischaemic heart disease and stroke.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown M. S., Kovanen P. T., Goldstein J. L. Regulation of plasma cholesterol by lipoprotein receptors. Science. 1981 May 8;212(4495):628–635. doi: 10.1126/science.6261329. [DOI] [PubMed] [Google Scholar]
- Deedwania P. C., Swiryn S., Dhingra R. C., Rosen K. M. Nocturnal atrioventricular block as a manifestation of sleep apnea syndrome. Chest. 1979 Sep;76(3):319–321. doi: 10.1378/chest.76.3.319. [DOI] [PubMed] [Google Scholar]
- Fletcher E. C., DeBehnke R. D., Lovoi M. S., Gorin A. B. Undiagnosed sleep apnea in patients with essential hypertension. Ann Intern Med. 1985 Aug;103(2):190–195. doi: 10.7326/0003-4819-103-2-190. [DOI] [PubMed] [Google Scholar]
- Heliövaara M., Reunanen A., Aromaa A., Knekt P., Aho K., Suhonen O. Validity of hospital discharge data in a prospective epidemiological study on stroke and myocardial infarction. Acta Med Scand. 1984;216(3):309–315. doi: 10.1111/j.0954-6820.1984.tb03809.x. [DOI] [PubMed] [Google Scholar]
- Ingbar D. H., Gee J. B. Pathophysiology and treatment of sleep apnea. Annu Rev Med. 1985;36:369–395. doi: 10.1146/annurev.me.36.020185.002101. [DOI] [PubMed] [Google Scholar]
- Kales A., Bixler E. O., Cadieux R. J., Schneck D. W., Shaw L. C., 3rd, Locke T. W., Vela-Bueno A., Soldatos C. R. Sleep apnoea in a hypertensive population. Lancet. 1984 Nov 3;2(8410):1005–1008. doi: 10.1016/s0140-6736(84)91107-3. [DOI] [PubMed] [Google Scholar]
- Koskenvuo M., Kaprio J., Kesaniemi A., Poikolainen K. Alcohol-related diseases associated with ischaemic heart disease: a three-year follow-up of middle-aged male hospital patients. Alcohol Alcohol. 1986;21(3):251–256. [PubMed] [Google Scholar]
- Koskenvuo M., Kaprio J., Kesäniemi A., Sarna S. Differences in mortality from ischemic heart disease by marital status and social class. J Chronic Dis. 1980;33(2):95–106. doi: 10.1016/0021-9681(80)90033-8. [DOI] [PubMed] [Google Scholar]
- Koskenvuo M., Kaprio J., Partinen M., Langinvainio H., Sarna S., Heikkilä K. Snoring as a risk factor for hypertension and angina pectoris. Lancet. 1985 Apr 20;1(8434):893–896. doi: 10.1016/s0140-6736(85)91672-1. [DOI] [PubMed] [Google Scholar]
- Lavie P., Ben-Yosef R., Rubin A. E. Prevalence of sleep apnea syndrome among patients with essential hypertension. Am Heart J. 1984 Aug;108(2):373–376. doi: 10.1016/0002-8703(84)90628-8. [DOI] [PubMed] [Google Scholar]
- Lugaresi E., Cirignotta F., Coccagna G., Piana C. Some epidemiological data on snoring and cardiocirculatory disturbances. Sleep. 1980;3(3-4):221–224. doi: 10.1093/sleep/3.3-4.221. [DOI] [PubMed] [Google Scholar]
- Motta J., Guilleminault C. Cardiac dysfunction during sleep. Ann Clin Res. 1985;17(5):190–198. [PubMed] [Google Scholar]
- Muller J. E., Stone P. H., Turi Z. G., Rutherford J. D., Czeisler C. A., Parker C., Poole W. K., Passamani E., Roberts R., Robertson T. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985 Nov 21;313(21):1315–1322. doi: 10.1056/NEJM198511213132103. [DOI] [PubMed] [Google Scholar]
- Norton P. G., Dunn E. V. Snoring as a risk factor for disease: an epidemiological survey. Br Med J (Clin Res Ed) 1985 Sep 7;291(6496):630–632. doi: 10.1136/bmj.291.6496.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partinen M., Palomäki H. Snoring and cerebral infarction. Lancet. 1985 Dec 14;2(8468):1325–1326. doi: 10.1016/s0140-6736(85)92625-x. [DOI] [PubMed] [Google Scholar]
- Peter J. H., Siegrist J., Podszus T., Mayer J., Selzer K., von Wichert P. Prevalence of sleep apnea in healthy industrial workers. Klin Wochenschr. 1985 Sep 2;63(17):807–811. doi: 10.1007/BF01732285. [DOI] [PubMed] [Google Scholar]



