Abstract
Background
“Gummy smile” describes the aesthetically unappealing display of gums that extends more than 2 to 3 mm when individuals smile. The multifactorial etiology of the gummy smile leads to various surgical and nonsurgical treatment strategies, including orthodontic therapies, lip fillers, and primarily botulinum toxin as a nonsurgical treatment.
Objectives
In this paper, the authors present the preliminary report of a novel, minimally invasive, and non-neurotoxic treatment option for gummy smiles based on the insertion of smooth-surfaced resorbable polydioxanone threads along the vectors of the lip elevator muscles, offering long-lasting satisfactory aesthetic outcomes.
Methods
The proposed subcutaneous thread insertion technique utilizes 23 G, 38 mm cannulas with 14 smooth threads per cannula. Twenty-two female patients with subjectively distressing gummy smiles have been treated so far. The correction of gummy smiles is rapid and has been documented for up to 18 months, with the most protracted case lasting 20 months. The first cannula is positioned 1.5 cm from the labial commissure and 0.5 cm above it, following the vector of the orbicularis oris muscle from the modiolus to the upper white lip. The second cannula targets the levator labii superioris muscle vector, entering from the modiolus, and the third cannula follows the zygomaticus major and zygomaticus minor muscle vectors. The insertion points are the same for the first, second, and third cannula. The fourth cannula is inserted 2 cm from the insertion point of the first, second, and third cannulas toward the premasseteric area and the internal corner of the eye, crossing the third thread in a crossed pattern. Only the 2 threads along the levator labii superioris and orbicularis oris vectors were inserted in 1 of the 22 treated patients, who displayed no molar teeth exposure while smiling.
Results
No novel excessive gingival display has occurred in the 22 ambulatory patients treated so far for 9 to 12 months. In the patients treated so far, the mean distances between the diagnostic reference points decreased by 0.85 and 1.25 mm after 2 and 6 weeks, respectively, with negligible pain during the procedure and high satisfaction among all patients.
Conclusions
The proposed smooth thread technique could be a technically convenient and minimally invasive option for addressing disturbing gummy smile problems.
Level of Evidence: 4 (Therapeutic)

Regardless of cultural and ethnic nuances, an oval face with balanced features is the cornerstone of an attractive and youthful appearance. Symmetrical, harmonious smiles, with 1 to 2 mm of gingival exposure, have long complemented this universal aesthetic rule of beauty, with reports of restorative cosmetic dentistry procedures tracing back to ancient Egypt.1,2 The term “gummy smile” describes the unpleasant gingival display that exceeds 2 to 3 mm when the individual smiles. Synonymous terms such as “horse smile,” “gingival smile line,” or “high lip line” shed light on the multifactorial etiology of excessive gingival display (EGD), including skeletal, periodontal, muscular, and possibly combined etiologies.
The exposure of the maxillary anterior gingiva during a full smile (gingival smile line) demonstrates distinct sexual dimorphism, with a 96% prevalence in females. This observation primarily relates to anterior vertical maxillary excess or if the upper lip rises higher than expected when smiling.3
In clinical studies, a ruler or caliper is helpful for quickly measuring the gingival display. The landmarks from which to measure the diagnostic distance from the reference points RP1 to RP2 are the lowest margin of the upper lip, extending upwards to the midpoint of the gingival margin of the maxillary lateral or central incisor (RP1), and the gingival margin at the midportion of the gingival margin of the maxillary lateral or central incisor (RP2; Figure 1).4,5
Figure 1.
The reference points, RP1 and RP2, for linear gummy smile diagnosis and quantification. The image shows the maxillary lateral incisor as the basis for measurements. The distance from RP1 to the midpoint of the incisal edge of the maxillary lateral or central incisor (RP3) is occasionally recorded when RP1 falls below the gingival-dental margin. Reproduced from Diaspro et al, published in Aesthetic Surgery Journal, with permission from Oxford University Press.5
A Le Fort I osteotomy is the only option for correcting EGD when excessive maxillary vertical bony growth is the cause. In contrast, orthognathic surgery, gingivectomy, and surgical crown lengthening have only limited applications when EGD involves altered passive dental eruption, short clinical crowns, or periodontal disorders affecting the gingiva scaffold.4,6
Because the hypercontraction of the upper lip elevator muscles during smiling is the second determinant or co-determinant of EGD, botulinum toxin has unsurprisingly gained prominence among nonsurgical EGD treatments, including orthodontic therapies and lip fillers.4 The levator labii superioris alaeque nasi, levator labii superioris, and zygomaticus minor muscles receive blood from the terminal branches of the facial artery and the infraorbital branch of the maxillary artery. These muscles elevate the upper lip because of the action of the facial nerve's terminal buccal and zygomatic branches.2 Two units of botulinum toxin, injected 1 cm lateral to the ala of the nose on each side (the Yonsei points), are sufficient to target all 3 muscles while respecting local vascularity.1 Resorting to 2 injections per side, following facial animation and palpation to identify target points—at the convergence area of the levator labii superioris alaeque nasi and levator labii superioris, and where the levator labii superioris and zygomaticus minor approximate each other—may further enhance outcomes.2
The primary limitation of botulinum toxin is its relatively short-lasting effectiveness, with excellent outcomes persisting for no more than 12 weeks for gummy smiles measuring up to 4 mm. Aesthetic deterioration begins around the fifth month, and the condition soon reverts to baseline.4,7
Always focusing on reducing the neuromotor input to the hyper-contracted elevator muscles, one of the authors introduced a novel technique in 2018 to correct gummy smiles immediately. This technique can be used independently without resorting to neurotoxicity or as an ancillary option that complements more complex treatment strategies. The innovation involved extrinsic mechanical compression on the lateral fibers of the levator labii superioris alaeque nasi muscle, inhibiting the motility of the deep muscle fibers.5 A single 0.22 mL average bolus of hyaluronic acid (ranging from 0.2 to 0.3 mL) is sufficient to immediately reduce the elevation of the upper lip during smiling when injected without local anesthesia at constant pressure near the bony surface with a 30 G, 13 mm needle at the most cranial portion of the nasolabial fold (∼3 mm from the alar cartilage wing), perpendicular to the skin.5
Once again, the temporary effectiveness posed a problem because of the resorption of the hyaluronic acid bolus and the loss of compressive effect on the neuromotor input to the upper lip elevator muscles. Serendipity allowed for a departure from traditional strategies focused on neuromotor input.
In 2023, the corresponding author and a co-author observed that implanting smooth threads for the usual biorevitalization and rejuvenation purposes led to an unexpected outcome: rapid correction of the gummy smile's unsightly hypercontraction of the upper lips. Polydioxanone (PDO) smooth-surfaced absorbable threads inserted through cannulas into subcutaneous tissue layers lead to immediate volume enhancement and filling of depressions because of their physical filling effect and induced swelling and restoration of depleted soft tissue volumes because of long-lasting induced collagen and elastic fiber neosynthesis by tumor growth factor-β signaling.8-10
PDO threads, very flexible and biocompatible, are clinically tested polyester monofilaments of high tensile strength with no demonstrated allergic potential. Extrusion occurs only because of improper technique. The monofilaments are safely degraded by hydrolysis within ∼6 months after inducing local fibroblast proliferation, as demonstrated by histologically neocollagenesis, neosynthesis of connective tissue, and increased capillary volume.8-10
In rejuvenating procedures, smooth threads have an advantage: they minimize the risks of puffiness and unnatural contours associated with soft tissue filler injections. Subcutaneously inserted smooth threads also minimize vascular risks in anatomically dangerous areas. An example is the nasojugal area, in which the angular artery and vein cross superficially after emerging from the facial artery and vein.8,9
Following their observation, all authors agreed to shift the focus of smooth thread insertion from generic local rejuvenation to the direct correction of bothersome gummy smiles and to standardize the technique for inserting smooth threads.
This preliminary report presents the novel PDO thread technique as an example of nonsurgical, minimally invasive strategies for correcting gummy smiles without the need for neurotoxicity. Threads are inserted using a cannula and follow the paths of the lip elevator muscles. The correction of gummy smiles is rapid and has been documented to last up to 18 months, with the most protracted case lasting 20 months.
METHODS
This study was conducted between May 2023 and February 2025. The ambulatory-treated female patients who had sought specialist treatment for their gummy smile agreed to the video recording of their procedure and the possibility of anonymous publication of a manuscript describing the innovative thread treatment they underwent. All performed activities were within the accepted regulatory indications for ambulatory thread application, as stated in the patient information leaflet, and complied with the accepted regulatory requirements (ie, Articles 62 to 82 of the European Union Regulation MDR 2017/745 and Article 16 of Legislative Decree 137/2022). These considerations allow for waiving all formal preliminary IRB approval requirements.
The proposed subcutaneous thread insertion technique utilizes 23 G, 38 mm cannulas. Ideal candidates should not have undergone any previous treatments for their gummy smiles and must have no medical history that could interfere with the thread procedure. The technique, which requires a 2-member team consisting of an author and an assistant, has been standardized and tested without complications on 22 female patients with subjectively distressing gummy smiles but not on men. This gender selection happened by chance, likely because the prevalence of the condition is twice as high in women, and women tend to seek consultation more often than men. Each cannula contains 14 PDO smooth threads (V Lift Pro International, La Vila Joyosa, Alicante, Spain).
The first cannula is inserted subdermally, 1.5 cm from the labial commissure and 0.5 cm above it, following the vector of the orbicularis oris muscle from the modiolus to the upper white lip (Figure 2). All investigators used the same caliper to avoid biases and ensure maximum precision in all measurements (Figure 3).
Figure 2.
Details of the injection points of the first, second, and third smooth thread (1.5 cm from the commissure and 0.5 cm above it) and the fourth thread (2 cm from the first insertion point) with evidence of the injection vectors in the same 37-year-old female patient displayed in Videos 2 and 3.
Figure 3.
The operating table before the procedure: the 14-thread cannulas and a caliper for precise measurements.
Using the same subdermal technique and insertion point, the placement of the second cannula proceeds until it reaches the vector of the levator labii superioris muscle entering from the modiolus. The third cannula is also inserted subdermally at the same insertion point as the first and second ones, following the vectors of the zygomaticus major and zygomaticus minor muscles. The fourth cannula is inserted 2 cm from the insertion point of the first, second, and third cannulas toward the premasseteric area and the internal corner of the eye, crossing with the third thread in an X pattern. Video 1 details the topographical identification of the 2 injection points and the insertion vectors of smooth threads on the skin surface. Video 2 illustrates the injection technique after needle positioning.
The authors’ empirical experience suggests that the collagen network induced by the threads crossing is firmer and more stable than when the threads are inserted in parallel. This crossed insertion enhances the skin's resistance to the lifting force of muscles. No topical or infiltrative anesthesia is warranted unless required by the patient or the injector. In summary, there are only 2 insertion points for the 4 cannulas. Four cannulas, each with 14 threads, means 56 threads per hemiface, or eight 14-thread cannulas per patient, with an estimated cost for a complete 8-cannula treatment of approximately USD 130 in Latin America and USD 90 in Europe.
For more complete information, Figure 4 pictures the final orientations of the implanted threads against the background of the involved facial muscles. All insertion points steer clear of the “danger zone” identified by local vascular anatomy, specifically the angular artery, the superior labial and lateral nasal arteries, and the more distal infraorbital artery.1 Video 3 illustrates the procedure comprehensively, following the identification of the 2 injection points: from skin disinfection to the insertion of the 4 cannulas.
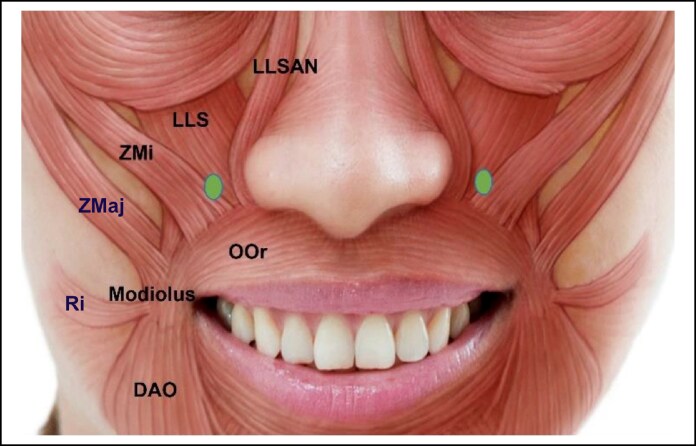
Figure 4.
Diagram showing the cannula insertion points and directions of inserted threads. The positions of the botulinum toxin's Yonsei points are shown for reference laterally to the nose pyramid. Reproduced from Hong under the terms of a Creative Commons Attribution (CC BY) license.1 DAO, depressor anguli oris; LLSAN, levator labii superioris alaeque nasi; LLS, levator labii superioris; OOr, orbicularis oris; Ri, risorius; ZMaj, zygomaticus major; ZMi, zygomaticus minor.
A minor but equally effective technical variation deviating from the standard 4-cannula protocol in 1 of the 22 patients treated so far involved inserting only 2 cannulas following the levator labii superioris and orbicularis oris vectors while omitting the zygomaticus major and zygomaticus minor muscle vectors. The patient displayed no exposure of molar teeth while smiling, indicating that the force exerted by the zygomatic muscles was not excessive. The lack of contractile elevation of the zygomatic muscles justified this deviation from the standardized technique for this patient. Standard recommendations following the procedure included avoiding makeup and physical exercise for 24 h and refraining from local massage for 2 weeks.
Two weeks after the procedure, the 22 treated patients completed a brief questionnaire to assess the pain experienced during the procedure using a 10-point Likert scale (0 = no pain; 10 = maximum pain). Additionally, the treated patients evaluated their satisfaction with the treatment experience and, although still at that precocious stage, their early impressions of the initial aesthetic benefits, assessed through the Global Aesthetic Improvement Scale (GAIS) patient subscale (5 scores: worse, no change, improved, much improved, and very much improved).
RESULTS
In the 22 ambulatory patients treated so far with the proposed thread technique (all patients were female; age range: 28-45 years, mean age: 37.3 years), the period with no or negligible reversal of the corrected EGD has ranged from 9 to 12 months. One patient experienced a transient hematoma at the insertion point, with no other complications reported. There has been no shift over time in all patients treated so far. Patients only experienced mild discomfort when gesticulating during the first week.
Correction of the gummy smile condition develops rapidly. Videos 4 and 5, taken in standardized conditions (posture, light), document that the baseline upper lip retraction appears less severe and disfiguring after 20 days in a 34-year-old female patient. In the patients treated so far, the mean decrease in the RP1 to RP2 distance was 0.85 mm after 2 weeks and progressed to 1.25 mm after 6 weeks. The mean pain experienced during the procedure was 1.82 out of a maximum of 10, whereas the GAIS patient score averaged 4.23 out of 5. None of the treated patients reported a complete loss of aesthetic benefits, even after 12 months.
Figures 5A, B and 6A, B depict pre- and posttreatment examples of the short-term correction 4 months after the standard 14-thread procedure in 2 patients aged 35 and 41, respectively. The lower eyelids do not appear to contract, as the cheekbones rise only modestly when smiling because of the reduced strength of the zygomatic major and minor muscles. The right commissure in the patient depicted in Figure 6B showed a more significant elevation, but the clinical significance of this asymmetry was negligible for her. The likely reason was a greater strength of the zygomatic muscles on that side. The author responsible for the patient (F.I.C.A.) added a cannula horizontally at the intersection of the other 2, hoping that this additional cannula would increase resistance to muscle traction and improve the baseline asymmetry and that was what happened.
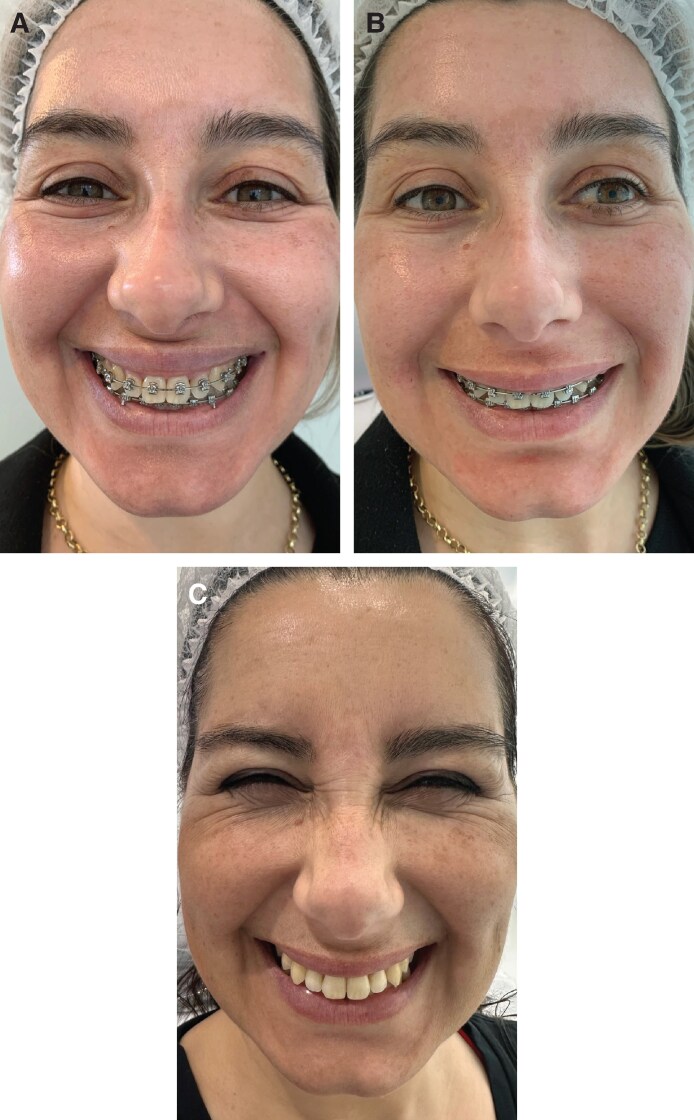
Figure 5.
(A) Pretreatment image of a 35-year-old female patient with upper lip retraction rising higher than expected when smiling, causing a baseline gummy smile. (B) The patient is shown 4 months after the 14-thread cannula procedure. (C) Partial reversion to baseline upper lip retraction with no retreatment is shown 18 months after the 14-thread cannula procedure.
Figure 6.
(A) Pretreatment image of a 41-year-old female patient with upper lip retraction rising higher than expected when smiling, causing a baseline gummy smile. (B) The patient is shown 4 months after the 14-thread cannula procedure. (C) Partial reversion to baseline upper lip retraction with no retreatment is shown 18 months after the 14-thread cannula procedure.
In Figures 5C and 6C, the patient images show that the upper lip has partially reverted to its baseline elevation in both patients after 18 months. The results are no longer the same ones shown in Figures 5B and 6B, yet the overall aesthetic outcomes remain satisfactory after 18 months. Although, as expected, the reversal rate over time is variable, and neither patient has required retreatment yet.
DISCUSSION
The outcomes of orthognathic surgery are permanent; however, these surgical procedures are costly and time-consuming. Additionally, they come with limitations and liabilities, including psychological resistance, relapses, and occlusion results that may be unbalanced or aesthetically unpleasant.11 Nonsurgical techniques for correcting EGD, such as botulinum toxin or the proposed thread technique, are quick and ambulatory, alleviate the fear of surgery, are affordable, and achieve success rates exceeding 95%. However, they require a solid understanding of the anatomy of mimic muscles and vascularity in the relevant areas, the upper lip, and the nasal ala.4,12
A dazzling smile results from the coordinated action of several muscles: the levator labii superioris alaeque nasi, zygomaticus minor and major, levator anguli oris, risorius, depressor anguli oris, depressor labii inferioris, mentalis, depressor septi nasi, and orbicularis oris.2 The levator labii superioris alaeque nasi muscle elevates and everts the upper lip in moderate gummy smiles, whereas the depressor septi nasi muscle pulls the nasal tip down. In severe gummy smiles, the levator labii superioris muscle and, to a lesser extent, the zygomaticus minor muscle also contribute to raising the upper lip.1,2 For thread insertion, the anatomy of the upper lip elevator muscles and the distribution of muscle vectors do not show significant bilateral asymmetries.12 Regarding gender differences, the authors cannot offer a hypothesis because they have treated no male individual so far.
Initially, the sole purpose of thread placement was to achieve a general biorevitalization and rejuvenating effect.8,9 Only microscopic investigations could reveal how the observed actions of muscle hypercontraction and upper lip elevation evolve; currently, the authors can only propose hypotheses. The threads modulate the mimic muscles to reduce activity. Is a mechanical action on the muscles responsible for the changes in muscle insertion to the subdermal layers through the septal fibers on the muscle surface? Another hypothesis suggests that the monofilament threads initially act as a mechanical barrier that counteracts the muscle force, followed by local neocollagenesis, resulting in firmer skin and increased mechanical resistance to muscle pull. Ethical concerns regarding biopsies and histology to unravel this riddle would be significant.
Although the case series has 2 significant biases (few treated patients so far, all female patients), the aesthetic benefits of the proposed thread technique seem to last longer than those of botulinum toxin. Negligible or no reversal of EGD correction is noticeable for at least 9 to 12 months and has been documented for 18 months in the first 2 treated patients, with only a slight return to baseline compared with the EGD effect of botulinum toxin, which lasts from 4 to 7 months.13,14 Depending on the botulinum toxin type and the gummy smile's baseline severity, the first signs of reversal may appear within 4 months if the EGD is <5 mm. Initial reversal can occur within 3 months if the EGD exceeds 5 mm. Furthermore, the unpredictable risk of developing high titers of antibodies to botulinum toxin from repeated injections should not be overlooked. This risk is notable, ranging from 0.5% to 1.5% per year, which may lead to partial or complete treatment failure.13,14 Moreover, compared with hyaluronic acid or botulinum toxin, the proposed technique of inserting PDO smooth threads reduces the risk of allergies.8,9 Additionally, it may enhance skin quality by increasing collagen neosynthesis.
Another possible bias in these preliminary observations may relate to the photographic documentation. The patients depicted in Figures 5 and 6 appear to smile less intensely in the follow-up photographs because eyelid wrinkles present in the baseline photographs are absent in the follow-up images. This difference is not an artifact of manipulation to minimize visual exposure of the gums at follow-up; the authors always ask their patients to smile as intensely as possible. Their idea is that the increased rigidity of the skin because of the inserted threads acts as a mechanical brake on the vigorous contraction of facial muscles and skin folding, resulting in less evident eyelid and nasal wrinkles, as well as wrinkles on the outer corner of the eye compared with the baseline photograph. The unintentional “bias” may persist in future treatments; however, it should not undermine the overall judgment on the outcomes and value of the authors’ thread technique.
The remarkable safety and absence of complications in facial areas with significant animation among the 22 patients treated so far also warrant discussion. The safety of thread placement strictly depends on identifying the correct insertion plane; skin dimpling, appreciable palpation, and visual appreciation of threads can occur with dermal thread placement. Beyond hematoma, other speculatively possible complications that were not observed include thread migration after insertion or thread extrusion, which could occur because of an incorrect insertion plane.
The critical risk mitigation strategy is attention while performing the procedure. The operators who performed the thread injections are highly skilled; however, the authors cannot dismiss the possibility that the proposed thread procedure may be less safe in the hands of less experienced practitioners, which would be a limitation of the technique. Although considered minimally invasive treatments, using threads in aesthetic medicine requires skills such as sound cannula handling and thorough knowledge of skin planes and anatomical landmarks. Insertion must be precise, because 1 portion of the threads is inside the cannula and the other outside. It is impossible to reverse or correct the orientation after insertion, unlike other injectable treatments, where correcting the plane before injection is always feasible. Master-level courses in aesthetic medicine can provide these skills if offered by reputable educational institutions that provide both theoretical and practical training and if taught by qualified trainers.
Concerning the satisfaction reported in the GAIS patient subscale forms filled out 2 weeks after the procedure, when postprocedural inflammation may not have resolved, the high scores reported carry only short-term anecdotal value and limited clinical significance. Nonetheless, the elevated GAIS scores indicate that the technique is well received and that initial outcomes are satisfactory. The authors plan to reassess the GAIS scores in all future patients after 1 year or 15 months.
CONCLUSIONS
Thanks to its safety and fewer injections, the proposed thread technique could offer a novel, technically convenient, minimally invasive, safe, and consistently effective treatment option for skilled injectors to tackle the gummy smile issue without directly affecting the neuromotor input to the overly active upper lip elevator muscles. In the future, a formal preliminary categorization of gummy smile patients according to the severity of gingival exposure could help personalize the number of injected cannulas.
Disclosures
The authors declare that they have no conflict of interest related to this article. No author received funds or other benefits for their research or manuscript and has no paid or unpaid relationships with industry manufacturers, publishers, or other companies in any way connected to the manuscript submission. Dr Cavallini received research grants as a member of R&D steering boards and as a lecturer and tutor in continuous medical education activities, primarily from Allergan (Irvine, CA) and Mastelli Srl (Sanremo, Italy). Similarly, Dr Raichi has received fees over the past year and a half from Mastelli Srl and other producers of fillers, aesthetic medicine, and plastic surgery products for his roles as an editor of educational materials and as a lecturer at continuous medical education events, as well as for sponsored educational meetings. Dr Carrasco Avilés, the corresponding author, and Dr Llorca Pérez have never received fees or other benefits for activities that could generate conflicts of interest.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1.Hong SO. Cosmetic treatment using botulinum toxin in the oral and maxillofacial area: a narrative review of esthetic techniques. Toxins (Basel). 2023;15:82. doi: 10.3390/toxins15020082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polo M. Botulinum toxin and smile design. Dent Clin North Am. 2022;66:419–429. doi: 10.1016/j.cden.2022.03.003 [DOI] [PubMed] [Google Scholar]
- 3.Peck S, Peck L, Kataja M. The gingival smile line. Angle Orthod. 1992;62:91–100; discussion 101-2. https://pubmed.ncbi.nlm.nih.gov/1626754/ [DOI] [PubMed] [Google Scholar]
- 4.Rajagopal A, Goyal M, Shukla S, Mittal N. To evaluate the effect and longevity of Botulinum toxin type A (Botox®) in the management of gummy smile—a longitudinal study up to 4 years follow-up. J Oral Biol Craniofac Res. 2021;11:219–224. doi: 10.1016/j.jobcr.2021.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diaspro A, Cavallini M, Piersini P, Sito G. Gummy smile treatment: proposal for a novel corrective technique and a review of the literature. Aesthet Surg J. 2018;38:1330–1338. doi: 10.1093/asj/sjy174 [DOI] [PubMed] [Google Scholar]
- 6.Schendel SA, Eisenfeld J, Bell WH, Epker BN, Mishelevich DJ. The long face syndrome: vertical maxillary excess. Am J Orthod. 1976;70:398–408. doi: 10.1016/0002-9416(76)90112-3 [DOI] [PubMed] [Google Scholar]
- 7.Zengiski ACS, Basso IB, Cavalcante-Leão BL, et al. Effect and longevity of botulinum toxin in the treatment of gummy smile: a meta-analysis and meta-regression. Clin Oral Investig. 2022;26:109–117. doi: 10.1007/s00784-021-04223-w [DOI] [PubMed] [Google Scholar]
- 8.Liao ZF, Yang W, Lin FC, Wang SW, Hong WJ, Luo SK. A case study: comprehensive approach for treating horizontal neck wrinkles using hyaluronic acid injections and thread-lifting. Aesthetic Plast Surg. 2023;47:765–771. doi: 10.1007/s00266-022-03071-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao Z-F, Yang W, Li X, Wang S-W, Liu F-C, Luo S-K. Infraorbital rejuvenation combined with thread-lifting and non-cross-linked hyaluronic acid injection: a retrospective, case-series study. Aesthetic Plast Surg. 2024;48:1589–1596. doi: 10.1007/s00266-023-03740-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim CM, Kim BY, Suh DH, et al. The efficacy of powdered polydioxanone in terms of collagen production compared with poly-l-lactic acid in a murine model. J Cosmet Dermatol. 2019;18:1893–1898. doi: 10.1111/jocd.12894 [DOI] [PubMed] [Google Scholar]
- 11.Sarver DM, Weissman SM. Long-term soft tissue response to LeFort I maxillary superior repositioning. Angle Orthod. 1991;61:267–276. https://pubmed.ncbi.nlm.nih.gov/1763837/ [DOI] [PubMed] [Google Scholar]
- 12.Hwang WS, Hur MS, Hu KS, et al. Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin. Angle Orthod. 2009;79:70–77. doi: 10.2319/091407-437.1 [DOI] [PubMed] [Google Scholar]
- 13.Naumann M, Carruthers A, Carruthers J, et al. Meta-analysis of neutralizing antibody conversion with onabotulinumtoxinA (BOTOX®) across multiple indications. Mov Disord. 2010;25:2211–2218. doi: 10.1002/mds.23254 [DOI] [PubMed] [Google Scholar]
- 14.Naumann M, Boo LM, Ackerman AH, Gallagher CJ. Immunogenicity of botulinum toxins. J Neural Transm (Vienna). 2013;120:275–290. doi: 10.1007/s00702-012-0893-9 [DOI] [PMC free article] [PubMed] [Google Scholar]