Abstract
Restoring elbow flexion is a priority in adults with complete brachial plexus palsy. If the nerve root is not avulsed, a graft can be placed between the existing root and the musculocutaneous nerve. The aim of this study was to evaluate the outcomes of using vascularized ulnar nerve grafts in this context. Our case series consisted of 17 male and 3 female patients (mean age of 31 years) presenting complete brachial plexus palsy after a motorcycle accident. A graft at the C5 or C6 root on the musculocutaneous nerve was done in all patients using a pedicled vascularized ulnar nerve to restore elbow flexion at a mean of 5 months after the accident. At a mean follow-up of more than 3 years, elbow flexion was graded as M4 in six patients and between M0 and M2 in the other 14 patients on the Medical Research Council scale. None of the patients had M3 strength. While the results of long grafts using a vascularized ulnar nerve are disappointing in this case series, they are consistent with previous publications. Encouraging results have only been reported with short grafts (<10 cm), which can rarely be used with supraclavicular lesions. For this reason, we currently prefer using a sural nerve graft or nerve transfer, when possible, to restore elbow flexion in adult patients with brachial plexus injuries.
Keywords: brachial plexus, nerve graft, vascularized ulnar nerve, allograft
Introduction
Restoring elbow flexion is a priority in adults with complete brachial plexus palsy. If the upper nerve roots are not avulsed, a graft can be used to restore flexion. 1 Currently, the preferred technique uses the sural nerve. 2 This long graft, however, does not have a feeder artery to ensure its survival with a high risk of central necrosis. 3 For this reason, vascularized nerve grafts have been introduced in 1976, by Taylor and Ham. They were the first to describe using vascularized grafts to improve the outcomes of long nerve grafts, aiming to reduce the likelihood of necrosis of the interposed nerve graft. 1 The aim of this study was to evaluate the outcomes of using pedicled vascularized ulnar nerve grafts to restore active elbow flexion in adults with complete brachial plexus palsy.
Materials and Methods
This retrospective case series consisted of 20 men who had complete brachial plexus palsy secondary to a motorcycle accident. The mean patient age was 31 years (15–60). The patients were operated a mean of 5 months (2–7) after the accident. All patients underwent a magnetic resonance imaging beforehand to confirm the upper cervical nerve roots were not avulsed.
With the patient under general anesthesia, the cervical area was explored to confirm the C5 or C6 nerve root was available for grafting. When a root was available, a vascularized ulnar nerve harvested from the ipsilateral arm was used a graft on the motor portion of the musculocutaneous nerve. The vascularized graft was 19 cm long, on average (14–20).
In two patients, since another root was available for grafting, a nonvascularized graft (the remaining ulnar nerve) was added between C6 and the median nerve trunk ( Fig. 1 ).
Fig. 1.
Intraoperative photos (right upper limb). —of distal suturing of a vascularized ulnar nerve graft (UNG) on the musculocutaneous nerve (MC) to restore elbow flexion. —of the transfer of 3 intercostal nerves (ICN) on the long head of triceps nerve (LHTN) to restore elbow extension. —of a nonvascularized ulnar nerve graft remnant (NVUN) being transferred on the median nerve (MN) to restore finger flexion.
The vascularized graft was turned around its vascular pedicle and slipped into a subcutaneous tunnel until the cervical region, where it is sutured to the target nerve root ( Fig. 2 ). Using a microscope, epiperineural suturing was done and supplemented by fibrin glue. The patient's arm was immobilized for 6 weeks; rehabilitation was initiated to mobilize the joints and reduce the risk of stiffness.
Fig. 2.

Schema of the vascularized ulnar nerve graft technique. The ulnar nerve is severed at the wrist and then turned around its pedicle, the distal part becomes proximal and is sutured to the root, and the proximal part becomes distal and is sutured to the musculocutaneous nerve.
Results
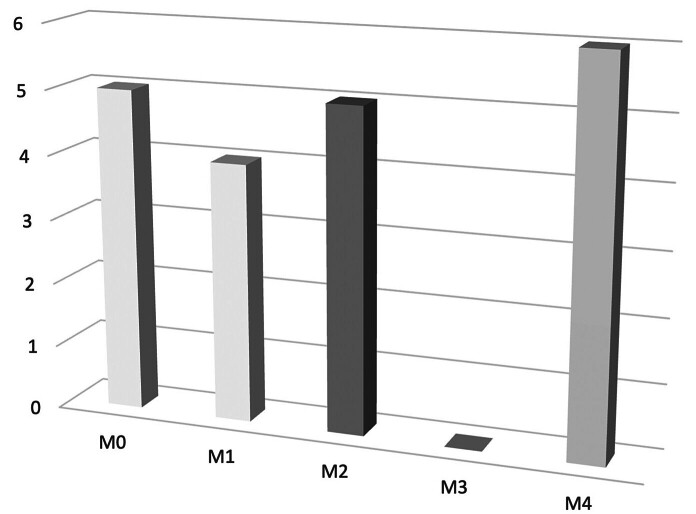
The mean follow-up was 38 months (16–120). Six patients recovered M4 elbow flexion strength on the Medical Research Council scale ( Fig. 3 ). Five patients had M2 strength, 4 had M1, and 5 had M0. None of the patients had M3 strength. On average, recovery of elbow strength took 17 months (10–22). None of the patients had persistent pain due to pseudo-Tinel sign sensations during percussion of the cervical area ( Table 1 ).
Fig. 3.
Graph of motor recovery after ulnar vascularized graft for elbow flexion (according the classification of British Medical Council: M0: No muscle activation; M1: Trace muscle activation, such as a twitch, without achieving full range of motion; M2: Muscle activation with gravity eliminated, achieving full range of motion; M3: Muscle activation against gravity, full range of motion; M4: Muscle activation against some resistance, full range of motion; M5: Muscle activation against examiner's full resistance, full range of motion.
Table 1. Patient data summary.
| Age (y) | Sex | Time before surgery (mo) | Ruptured roots |
Avulsed roots | Grafted root to MCN nerve | Vascularized ulnar nerve length (cm) | Elbow flexion (BMC scale) | Other procedures | |
|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 27 | M | 4 | C5C6 | C7T1 | C5 | 20 | M4 | SAN to SSN/ICN to LHTN |
| Patient 2 | 29 | M | 2 | C5T1 | C5 | 20 | M4 | Shoulder fusion/ICN to LHTN/ FL Transfer | |
| Patient 3 | 16 | M | 4 | C5C6 | C7T1 | C5 | 20 | M4 | SAN to SSN/ICN to LHTN |
| Patient 4 | 30 | M | 4 | C5C6 | C7T1 | C6 | 19 | M4 | SAN to SSN/ICN to LHTN |
| Patient 5 | 23 | M | 7 | C5C6 | C7T1 | C5 | 14 | M2 | SAN to SSN/ICN to LHTN |
| Patient 6 | 35 | M | 6 | C5T1 | C5 | 16 | M2 | C6 median (NVUN) (shoulder fusion refused) | |
| Patient 7 | 54 | F | 2 | C5C6 | C7T1 | C6 | 20 | M1 | SAN to SSN/ICN to LHTN |
| Patient 8 | 17 | M | 6 | C5C6 | C7T1 | C5 | 19 | M2 | C6 median (SG)/SSN grafting/ICN to LHTN |
| Patient 9 | 38 | M | 2 | C5C6 | C7T1 | C5 | 20 | M0 | Trapezius transfer/ICN to LHTN |
| Patient 10 | 60 | M | 6 | C5 | C6T1 | C5 | 17 | M0 | SAN to SSN |
| Patient 11 | 15 | M | 5 | C5C6C7 | C8T1 | C6 | 20 | M4 | C7 median/shoulder fusion/ICN to LHTN |
| Patient 12 | 35 | M | 3 | C5C6 | C7T1 | C5 | 19 | M1 | SAN to SSN/ICN to LHTN |
| Patient 13 | 18 | F | 3 | C5C6 | C7T1 | C5 | 20 | M2 | C6 median (SG)/shoulder fusion |
| Patient 14 | 35 | M | 5 | C5C6C7 | C8T1 | C5 | 19 | M4 | C6 median (SG)/shoulder fusion |
| Patient 15 | 32 | F | 5 | C5C6C7 | C8T1 | C5 | 20 | M1 | C6 median (SG)/shoulder fusion refused |
| Patient 16 | 27 | M | 6 | C5T1 | C5 | 19 | M0 | C6 median (SG)/shoulder fusion | |
| Patient 17 | 18 | M | 6 | C5C6C7 | C8T1 | C5 | 18 | M0 | C6 median (NVUN)/SSN recovery/ICN to LHTN |
| Patient 18 | 31 | M | 5 | C5T1 | C5 | 20 | M1 | Shoulder fusion | |
| Patient 19 | 19 | M | 5 | C5T1 | C5 | 19 | M2 | Shoulder fusion | |
| Patient 20 | 27 | M | 6 | C5C6 | C7T1 | C5 | 20 | M0 | SSN to SAN |
Abbreviations: F, female; FL, fascia lata; ICN intercostal nerve; LHTN, long head of the triceps nerve; M, male; MCN, musculocutaneous nerve; NVUN, nonvascularized ulnar nerve; SAN, spinal accessory nerve; SG, sural graft; SSN, suprascapular nerve.
Discussion
The results in terms of muscle strength are poor in our series, with only 30% of M4 results. These results are comparable with those reported in the literature. As a matter of fact, in a case series of eight patients with complete brachial plexus palsy, Bertelli et al. did a C5 root graft onto the musculocutaneous nerve using a vascularized ulnar graft. At more than 2 years' follow-up, six patients had achieved M2 strength only in their biceps. 4 The results reported by Birch et al. 5 appear better, likely because their grafts were shorter (14 cm) than ours since they were sutured onto secondary trunks (given that patients had a retroclavicular injury), which led to faster muscle reinnervation and therefore, better motor recovery. After placing a vascularized ulnar nerve graft between the C5 root and the median nerve, Chang et al. reported that 75% of their 25 patients had M3 finger flexion strength, 6 which is a poor functional result.
It is difficult to explain why the results with this technique are inadequate. The vascularization provided by the accompanying artery may not be sufficient to vascularize the entire nerve after its distal end is cut. Thrombosis after pedicle or artery manipulation is another potential explanation, as is spontaneous thrombosis of the extended artery after its distal end is cut. Questions about the suturing's effectiveness are natural when nerve surgery fails. However, the diameter of the ulnar nerve corresponds exactly to that of the torn nerve roots, making the graft and root anatomically compatible. Also, microsurgical suturing is done in a comfortable and reproducible anatomical environment. Lastly, the repairs are sufficiently permeable, since 13 of our patients had achieved M1 to M4 strength and nerve regrowth was occurring based on the Tinel sign, although it did not reach the motor end-plates for sufficient recovery to M3.
Our conclusion that the nerve root was graftable from a macro- and microscopic perspective can be brought into question and may be another reason for failure. Here again, several studies that did not confirm the nerve root was available for grafting based on trimmed nerve specimens examined by histopathology still reported satisfactory results with shorter grafts. Lastly, none of the well-known patient-specific factors that limit nerve regrowth, such as smoking were present in our case series. 7
The lack of a control group with conventional sural grafts is a limitation of our study. However, there are many published studies describing acceptable, but sometimes inconsistent results with this type of graft with no more than 55% of M3 to M4 active elbow flexion, 8 even though the use of a sural nerve remains the most commonly used technique for brachial plexus reconstruction in most international teams. 2
The 3-year follow-up period appears to be sufficient. In fact, motor recovery can take up to 2 years after this type of surgery. 5 The time elapsed between the accident, and the surgery impacts recovery. All the patients in our case series were operated within 5 months on average, a time frame in which the prognosis is best. 9 Chronic denervation of the ulnar nerve due to an initially complex brachial plexus injury can also explain the lower effectiveness of the denervated graft, 10 we believe this is the primary reason for these results.
Excessive regrowth related to graft vascularization and the magnitude of intraneural connections in the ulnar nerve may explain the worse results for this type of graft, as shown by Bertelli et al. 11 While the radial or sural nerve has been used as vascularized grafts they are currently not used for brachial plexus injuries. 12 13 Using a nonvascularized allograft has not yet been evaluated in adult brachial plexus injuries, although some authors have published encouraging results for the repair of injuries to the large peripheral nerve trunks. 14
Conclusion
While the principle is attractive from an intellectual point of view, the outcomes of using long vascularized ulnar nerve grafts do not yield consistently satisfactory results when used to restore elbow flexion in adults with complete brachial plexus palsy. We now use these graft only when a nerve transfer cannot be done, or the sural nerve cannot be used as a free graft. The use of a vascularized sural nerve for long grafts in the management of long grafts in brachial plexus palsy could be a suitable solution involving the use of a healthy nerve with sufficient vascularization to avoid graft necrosis. A clinical study should be proposed to confirm this hypothesis.
Footnotes
Conflict of Interest None declared.
References
- 1.Taylor G I, Ham F J. The free vascularized nerve graft. A further experimental and clinical application of microvascular techniques. Plast Reconstr Surg. 1976;57(04):413–426. [PubMed] [Google Scholar]
- 2.Čebron U, Mayer J A, Lu C, Daigeler A, Prahm C, Kolbenschlag J. Treatment trends of adult brachial plexus injury: a bibliometric analysis. Plast Reconstr Surg Glob Open. 2021;9(09):e3803. doi: 10.1097/GOX.0000000000003803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muangsanit P, Shipley R J, Phillips J B. Vascularization strategies for peripheral nerve tissue engineering. Anat Rec (Hoboken) 2018;301(10):1657–1667. doi: 10.1002/ar.23919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bertelli J A, Ghizoni M F. Results of c5 root grafting to the musculocutaneous nerve using pedicled, vascularized ulnar nerve grafts. J Hand Surg Am. 2009;34(10):1821–1826. doi: 10.1016/j.jhsa.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Birch R, Dunkerton M, Bonney G, Jamieson A M. Experience with the free vascularized ulnar nerve graft in repair of supraclavicular lesions of the brachial plexus. Clin Orthop Relat Res. 1988;(237):96–104. [PubMed] [Google Scholar]
- 6.Lin J A, Lu J C, Chang T Net al. Long-term outcome of 118 acute total brachial plexus injury patients using free vascularized ulnar nerve graft to innervate the median nerveJ Reconstr Microsurg2022 [DOI] [PubMed]
- 7.Goubier J, Teboul F. Elsevier; 2015. Grading of nerve injuries; p. 609. [Google Scholar]
- 8.Lanaras T I, Schaller H E, Sinis N. Brachial plexus lesions: 10 years of experience in a center for microsurgery in Germany. Microsurgery. 2009;29(02):87–94. doi: 10.1002/micr.20583. [DOI] [PubMed] [Google Scholar]
- 9.Birch R. Timing of surgical reconstruction for closed traumatic injury to the supraclavicular brachial plexus. J Hand Surg Eur Vol. 2015;40(06):562–567. doi: 10.1177/1753193414539865. [DOI] [PubMed] [Google Scholar]
- 10.Bertelli J ATM, Taleb M, Mira J C, Ghizoni M F. Functional recovery improvement is related to aberrant reinnervation trimming. A comparative study using fresh or predegenerated nerve grafts. Acta Neuropathol. 2006;111(06):601–609. doi: 10.1007/s00401-005-0005-0. [DOI] [PubMed] [Google Scholar]
- 11.Bertelli J AGM, Ghizoni M F. Concepts of nerve regeneration and repair applied to brachial plexus reconstruction. Microsurgery. 2006;26(04):230–244. doi: 10.1002/micr.20234. [DOI] [PubMed] [Google Scholar]
- 12.Doi K, Kuwata N, Kawakami F, Tamaru K, Kawai S. The free vascularized sural nerve graft. Microsurgery. 1984;5(04):175–184. doi: 10.1002/micr.1920050403. [DOI] [PubMed] [Google Scholar]
- 13.Shafi M, Hattori Y, Doi K. Surgical technique of harvesting vascularized superficial radial nerve graft. J Hand Surg Am. 2010;35(02):312–315. doi: 10.1016/j.jhsa.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 14.Peters B R, Wood M D, Hunter D A et al. Acellular nerve allografts in major peripheral nerve repairs: an analysis of cases presenting with limited recovery. Hand (N Y) 2023;18(02):312–315. doi: 10.1177/15589447211003175. [DOI] [PMC free article] [PubMed] [Google Scholar]