Case
A 73-year-old man with a history of hyperlipidemia, hypertension, and idiopathic small fiber neuropathy presented to our dermatology clinic after 5 months of a progressive, generalized, and pruritic rash (Fig 1). He first developed a rash 2 weeks after a course amoxicillin-clavulanate and was thus prescribed a 5-day course of oral prednisone for a presumed drug exanthem. His rash worsened despite prednisone, prompting him to present to a local emergency department where he was prescribed a 3-week prednisone taper. His rash worsened, and he was referred to a local dermatologist. A biopsy revealed a spongiotic dermatitis. He was diagnosed with atopic dermatitis and initiated on dupilumab as well as 1 week of empiric itraconazole for a potential superficial fungal infection. His rash worsened on dupilumab, after which he was transitioned to upadacitinib for presumed atopic dermatitis. Upon presentation to our dermatology clinic, physical examination was notable for diffuse, deeply erythematous, well-demarcated annular plaques with variable scale and occasional pustules. His scrotum was covered in thick grey scale. Examination did not reveal onychomycosis or tinea pedis.
Fig 1.
Rash at presentation consisting of diffuse, deeply erythematous, well-demarcated annular plaques with variable scale and occasional pustules at the leading edges.
What would you do next?
-
A.
Obtain antinuclear antibody titers
-
B.
Repeat punch biopsy for hematoxylin and eosin
-
C.
Skin scraping for light microscopy
-
D.
Initiate a course of oral terbinafine
-
E.
Obtain tissue cultures
What to do next?
Skin scraping for light microscopy.
Discussion
Skin scraping is a readily accessible and economical point-of-care diagnostic procedure allowing for diagnosis of superficial skin infections caused by parasites, fungi, or mites. In this case, mineral oil preparation revealed multiple ovoid Sarcoptes scabei and scybala (Fig 2), confirming the diagnosis of crusted scabies. potassium hydroxide preparation also revealed occasional fungal forms and hematoxylin & eosin of a contemporary biopsy identified foci of intracorneal pityrosporum.
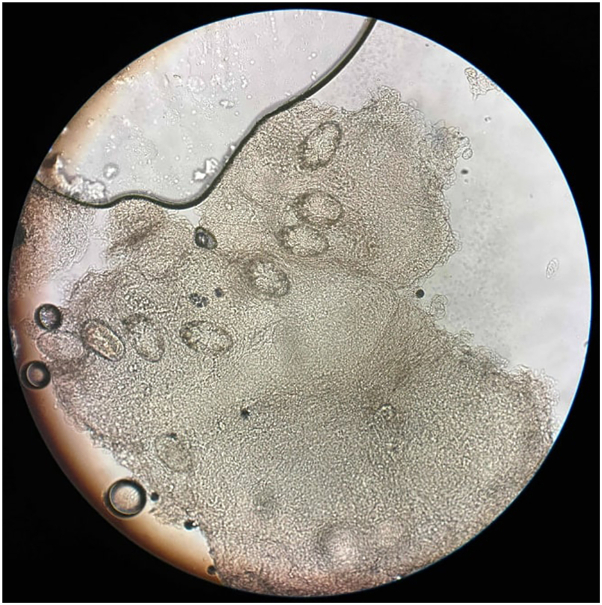
Fig 2.
Mineral oil preparation of skin scrapings revealed multiple S scabei ova and scybala. S scabei, Sarcoptes scabei.
Crusted scabies is a highly contagious scabies infestation that classically presents with thick, hyperkeratotic gray-white plaques teeming with mites that result in intractable pruritus. A high index of suspicion was warranted in this case given the extent of his rash, his debilitating itch, and his many ineffective immunosuppressive regimens.
Skin scrapings, a lynchpin diagnostic tool, have variable sensitivity (50% to 90%) in most cases of scabies but are more likely to yield mites from immunosuppressed patients or in crusted scabies.1 First-line treatment for classic scabies includes topical permethrin 5% cream and/or oral ivermectin 200 μg/kg.2, 3, 4 Permethrin is applied to the entire body from the neck down and left on for 8 to 14 hours, while ivermectin is administered as a single dose. Both permethrin and ivermectin therapy can be repeated after 1 to 2 weeks, and combination therapy is more effective than either agent alone.4 More aggressive therapy is required in crusted scabies. Permethrin is applied daily for 7 days and then twice weekly, with repeat doses of ivermectin on days 1, 2, 8, 9, and 15, with additional doses on days 22 and 29 for severe cases.5 Close personal contacts should also be examined and treated regardless of symptoms. HIV testing should be strongly considered in cases of crusted scabies.
The patient was advised to launder all clothing and bedding in hot water and high heat. Upadacitinib was discontinued, and he was treated as crusted scabies with repeated regimens of oral ivermectin and topical permethrin. In follow-up, the patient reported significant improvement in both his pruritus and rash.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: J.S.S. is supported by NIH grant K08AR084617.
Patient consent: The authors attest that they have obtained written consent from patient/s, their legal guardian/s or person/s with legal authority, for their photographs and medical information to be published in print and online and with the understanding that this information may be publicly available. Patient consent forms were not provided to the journal but are retained by the authors to be made available upon request.
IRB approval status: Not applicable.
References
- 1.Walter B., Heukelbach J., Fengler G., et al. Comparison of dermoscopy, skin scraping, and the adhesive tape test for the diagnosis of scabies in a resource-poor setting. Arch Dermatol. 2011;147:468–473. doi: 10.1001/archdermatol.2011.51. [DOI] [PubMed] [Google Scholar]
- 2.Usha V., Nair T.V.G. A comparative study of oral ivermectin and topical permethrin cream in the treatment of scabies. J Am Acad Dermatol. 2000;42(2):236–240. doi: 10.1016/s0190-9622(00)90131-2. [DOI] [PubMed] [Google Scholar]
- 3.Thadanipon K., Anothaisintawee T., Rattanasiri S., Thakkinstian A., Attia J. Efficacy and safety of antiscabietic agents: a systematic review and network meta-analysis of randomized controlled trials. J Am Acad Dermatol. 2019;80(5):1435–1444. doi: 10.1016/j.jaad.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Workowski K.A., Bachmann L.H., Chan P.A., et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1–187. doi: 10.15585/mmwr.rr7004a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Clinical care for scabies. 2022. https://www.cdc.gov/scabies/hcp/clinical-care/index.html