Abstract
Percutaneous repair is a safe and reliable method to restore continuity after acute Achilles tendon ruptures, with a lower incidence of wound complications than to open techniques. We describe a percutaneous ultrasound-guided surgical technique for acute Achilles tendon ruptures. Ultrasound guidance enables the tendon to be sutured without damaging the sural nerve or vessels. Following a cadaveric study in seven specimens, the technique was then used in 11 Achilles tendon tear patients. Ultrasound-guided repair of Achilles tendon ruptures is safe and reliable, and does not require skin incisions or a tourniquet. No re-ruptures nor sural nerve damage were recorded at the latest follow-up. Appropriately powered clinical studies are necessary to compare this closed technique with other percutaneous or minimally invasive techniques.
Keywords: Percutaneous, Ultrasound-guided, Achilles tendon, Tendon repair
Introduction
Acute Achilles tendon ruptures (ATR) as more frequent in men, with a male-to-female ratio ranging from 1.7:1 to 30:1 [1, 2].
Their management is controversial. Conservative treatment involves immobilization with a cast or brace, with a reported re-rupture rate of up to 17% and a significant loss of strength and power in the calf muscles [3]. Surgery can be performed using open, minimally invasive or percutaneous techniques, but it carries a risk of infection, wound healing complications, adhesions, and iatrogenic nerve injury [4–8].
Open surgery enables accurate juxtaposition of the tendon stumps, but can increase the rate of wound dehiscence and infection [9]. Minimally invasive approaches have emerged as viable alternatives for acute ATRs, potentially reducing the frequency of complications [10–12].
Percutaneous techniques increase the risk of sural nerve entrapment, with the possibility of saphenous neuritis ranging from 1.7–27% [4, 13–17].
Ultrasonography allows to identify small superficial nerves of the ankle and foot, including the sural nerve [18–20], and perform ultrasound-guided surgery of the ankle and foot (e.g., tarsal tunnel syndrome, Morton’s neuroma, Achilles tendon lengthening) [21–23].
The aim of our study was to evaluate the efficacy and safety of ultrasound-guided repair of the Achilles tendon in a completely closed procedure with no incision, stitches, or tourniquet [24]. We first studied the viability of the technique in cadaveric specimens, and later its outcome in ATR patients. The integrity of the sural nerve was checked using ultrasound during each step of the technique.
Materials and methods
Our prospective study was performed in accordance with the principles of the 1964 Declaration of Helsinki (2013 revision) and approved by the Research Ethics Committee of Hospital Beata María. All participants gave their informed consent to participate in the study and for their clinical and imaging data to be collected and analyzed. The specimens were provided by the Department of Anatomy of University Lasalle, Madrid, Spain. We used 7 fresh anatomical specimens (4 left and 3 right) including the knee, calf, ankle, and foot. All authors contributed to patient selection, procedure and application of scores.
All ultrasound scans were performed using an E-CUBE 15 equipped with an L8-17X multifrequency linear transducer (Alpinion Medical Systems, Bothell, WA, USA) and the Needle Vision Plus™ software package (Alpinion Medical Systems, Bothell, WA, USA).
The ultrasound-guided technique described below was performed on cadaveric specimens.
We then applied the ultrasound-guided technique to repair ATRs in 11 patients. Both in cadaveric specimens and in patients we used a straight needle kit (1.6 mm) and high-strength N°2 FiberWire® suture (Arthrex), although a high strength reabsorbable suture could equally be used [25].
Pre-clinical study: development of the surgical procedure
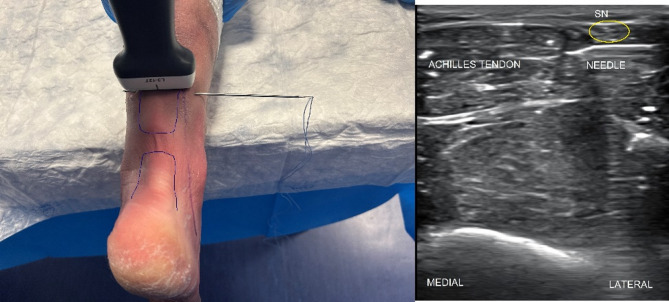
The cadaveric specimens were placed prone, and a complete percutaneous tenotomy of the Achilles tendon was performed 5 cm proximal to the insertion on the calcaneus, simulating a complete rupture. The sural nerve was then mapped throughout its course using ultrasound to accurately place the portals for surgery and prevent nerve entrapment or damage (Fig. 1).
Fig. 1.
Sural nerve mapping with US
No skin incisions were made. At the point where the proximal and distal sutures meet, minimal stretching of the skin was performed with the tip of forceps to avoid skin bridges between the stitches.
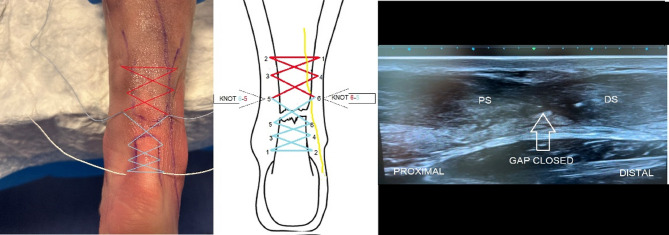
We used a symmetrical Bunnell-type suture configuration, starting 6–8 cm proximal to the ATR. The proximal suture ends at the proximal end of the tendon stump. Each medial-to-lateral or lateral-to-medial cross-suture was advanced approximately 2 cm (Figs. 2 and 3, and Fig. 4).
Fig. 2.
Ultrasound-guided passage of the needle and suture in the lateral area of the proximal stump with direct vision of the sural nerve
Fig. 3.
In the distal stump, passage of the needle and suture is usually medial to the nerve, as this runs from distal and lateral to proximal and medial
Fig. 4.
The ends of both the proximal and the distal sutures are tied in the lateral and medial aspects of the ruptured tendon. The approximation of the ends of the Achilles tendon is verified using ultrasound
The sural nerve usually runs from lateral, in the distal area, posterior to the fibular malleolus, lateral to the Achilles tendon, to medial in the medial third of the calf, crossing over the gastrocnemius tendon. Care is required to pass the suture without trapping the sural nerve. The first pass is normally deep to the nerve and, at some point distally, depending on the anatomy of the nerve, the suture is superficial to the tendon.
In the proximal stump, the needle and thread must be advanced carefully in the lateral area to avoid damaging or trapping the sural nerve. The procedure was performed under ultrasound guidance to avoid damaging the sural nerve and to ensure that the tendon was appropriately sutured (Fig. 2).
We repeated the procedure with another suture starting in the distal portion stump of the tendon and advancing proximally.
The distal ends of the suture were guided through the distal puncture of the proximal end suture to tie the proximal suture to the distal one. Reliable approximation of both ends of the tendon was thus achieved and verified with ultrasound.
We finished the Bunnell-type suture emerging at the point of the proximal ends of the suture (Fig. 4). Therefore, we did not need to enlarge the emergence points of the suture more than 1–2 mm if a skin bridge remains between the two stitches.
In addition, we achieved maximum tension when we tie the proximal and distal ends of 2 independent sutures by driving one suture to the point where the other one ends.
The ankle was kept in full plantar flexion while the sutures were tied (Fig. 4).
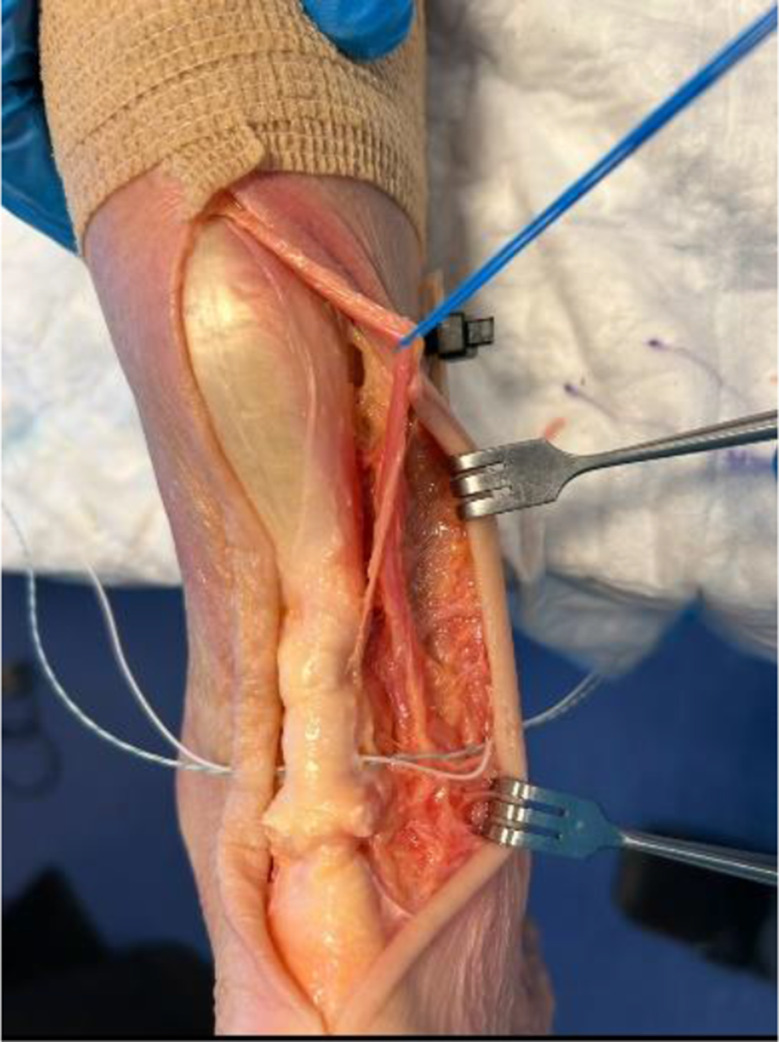
Postsurgical dissection enabled us to verify that the sural nerve was not damaged, and that full juxtaposition of the tendon stumps had been was achieved (Fig. 5).
Fig. 5.
Verification of the sural nerve via dissection of the specimen
Clinical study
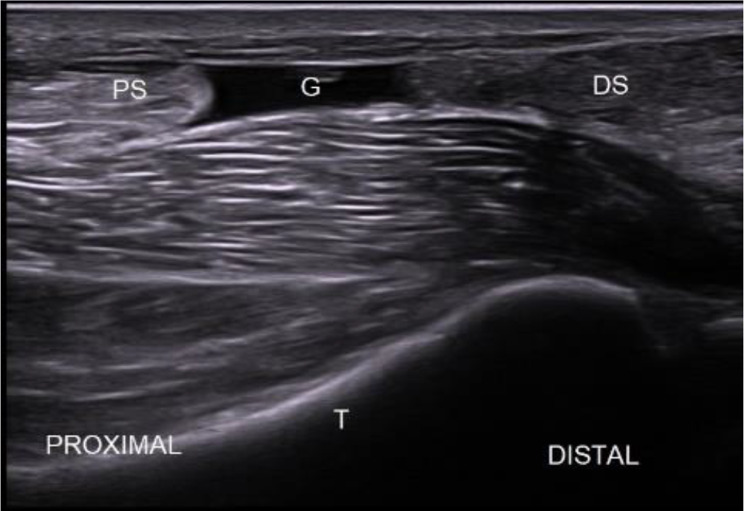
The clinical series comprised 11 patients (10 males and 1 female; mean age: 54 years (range 42 to 65) in whom the ATR was located by ultrasound and the sural nerve was carefully identified (Fig. 6). TThe time elapsed from the rupture of the Achilles tendon until the surgery was performed was 8.6 days (3–14). No patients had systemic diseases.
Fig. 6.
Achilles tendon tear: ultrasound image of acute Achilles tendon tear in the sagittal plane. G: gap (tendon lesion); PS: proximal stump; DS: distal stump; T: tibia
The skin was prepared in the usual fashion, obtaining a sterile field. Anesthesia involved sedation and local infiltration with 20 mL of local anesthetic (20 mL bupivacaine/adrenaline, 5 mg/mL + 0.005 mg/mL) in the puncture areas and tendon defects, approximately 4 to 6 cm proximal and distal to the tendon defect (Fig. 7). No tourniquet was used.
Fig. 7.
Bunnell-type criss-cross suture, knotting the proximal end with the distal end
At the end of the procedure, the patient was immobilized in a below knee cast, with maximum plantar flexion of the ankle.
Post‑operative protocol
Patients were discharged from the hospital on the same day. The full cast was kept in place for 3 weeks.
Patients walked using crutches without weight bearing for 3 weeks. The cast was removed at that stage, and an Aircast boot (XP Walker, DJO Ltd, Guilford, England, UK) with 3 heel wedges was appliied. Partial weight bearing with the Aircast boot was allowed at 4 weeks following the index procedure (one week after removal of the casr). The aptients were allowed to progressively increase their weight bearing status until full weight bearing was achieved 6 weeks after the percutaneous repair.
Nine weeks after surgery, and over the course of a further 2 weeks, patients were instructed to remove the orthosis for 1 to 4 h in the morning and again in the evening. At this stage, when not wearing the splint, patients bore their full weight on the operated leg and were instructed to wear a 15 mm heel wedge.
After complete removal of the Aircast boot, patients wore the heel wedge for a further month, by which time they had usually regained a fully plantigrade foot. Only at this stage (after approximately 12 weeks) were they permitted to begin eccentric exercises of the gastrocsoleus complex. At 5 months, patients were allowed to return to their normal activities, including running, when they felt confident to do so.
An early clinical examination was performed 2–3 weeks after the surgical procedure, and all patients underwent ultrasound assessment of the approximated stumps. The area innervated by the sural nerve was examined for tenderness, numbness, or any other complication. The Tinel test was performed along the entire course of the sural nerve.
Results
In the seven cadaver specimens, the sural nerve was intact, and the tendon ends were juxtaposed successfully: the technique was therefore considered safe.
In the 11 patients enrolled in the clinical study, the results of the sensory examination of the sural nerve were normal, and the Tinel sign was negative.
No complications, such as wounds, deep infections, or tendon re-rupture were detected after a minimum follow-up of 2 years (Fig. 8).
Fig. 8.

No complications, infection, or wounds
At 8 months, all patients were able to perform 10 single heel raises on the affected side(Fig. 9).
Fig. 9.

Single heel raises
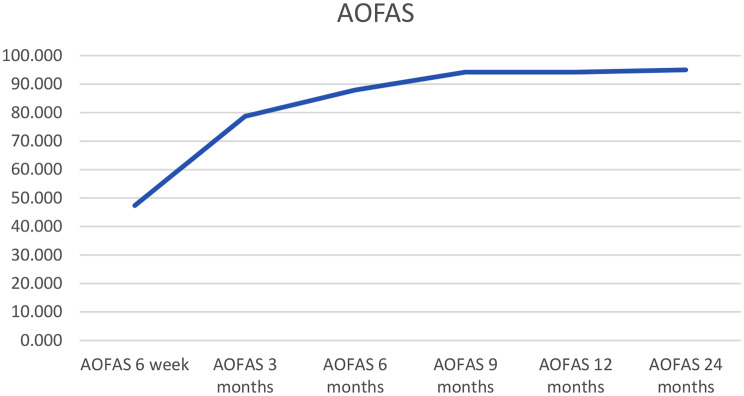
The AOFAS Ankle-Hindfoot Score increased significantly from 47.3 (range, 20–60) to 94.2 (range, 80–100) at 9 months, with no significant changes over the 2 years of follow-up (Fig. 10).
Fig. 10.
Progression of AOFAS over time
Patients recovered their level of sports activity, although some reported to be afraid that the tendon may rupture again during high-intensity activities. No such event occurred in any of our patients during the follow up period.
Discussion
The main finding of the present study is that ultrasound-guided repair of Achilles tendon ruptures is a safe and reliable surgical procedure that does not require scalpel incisions or a tourniquet. No re-ruptures nor sural nerve damage were recorded at the latest follow-up.
Ultrasound is at least as effective as magnetic resonance imaging in identifying the location of a tear and the gap between the torn ends of the tendon and distinguishing between partial and complete rupture [25, 26].
Achilles tendon surgery entails the risk of nerve damage and wound-related complications [27].
Minimally invasive approaches have emerged as a viable alternative for acute ATR, potentially reducing the rate of complications, the most important of which include infection and wound dehiscence [11, 12].
The percutaneous technique first described by Ma and Griffith in 1977 has since evolved, with no significant differences recorded for the risk of re-rupture between open and percutaneous surgery [28].
The risk of infection is lower with percutaneous surgery compared to open techniques [11, 12].
A significant risk of sural nerve injury has been observed with minimally invasive surgery, prompting to develop different suturing techniques to minimize the risk of damage to this nerve, reported in 4.5–27% of patients.
High-resolution ultrasound has proven reliable to assess the development of small-diameter nerves, such as the sural nerve and tibial nerve and distal branches such as the medial calcaneal branch [18, 20].
In 2003, Maffulli et al. reported placing a longitudinal suture parallel to the sural nerve, as in this way nerve injury is less likely. If it were to occur, it would most likely take the form of longitudinal neurotomy rather than transverse axonotmesis or neurotmesis, thus promoting regeneration and minimizing neuroma formation [3, 13].
Ultrasound-assisted surgery has been explored to minimize the risk of sural nerve damage. In 2014, Giannetti et al. combined ultrasound assistance with percutaneous Achilles tendon surgery and reported excellent results, with no damage to the sural nerve in the 13-month follow-up [29]. These authors used a scalpel to produce medial and lateral incisions and then introduced the needle [29]. Later, Paczesny et al. presented a study with 2 groups, one with percutaneous surgery without ultrasound and the other with ultrasound-assisted percutaneous surgery. They produced a 3 cm transverse incision at the level of the tendon gap to be able to suture the proximal stump with the distal stump [29, 30].
Ultrasound-guided surgery with the approach reported in the present work allows the surgical instruments and affected structures to be directly visible at all times during surgery. Moreover, the procedure is guided by continuous monitoring of each surgical step. No step requires to produce an actual surgical wound [21, 22, 31–33].
The risk of complications can be potentially eliminated by applying ultrasound-guided surgery, which enables continuous monitoring of the sural nerve, the vessel, the tendon, and the position of the suture. This approach optimizes all the potential advantages of percutaneous surgery.
Independent adequately powered comparative studies are required to establish the potential of this ultrasound-guided surgical modality.
Conclusions
Intraoperative use of high-resolution ultrasound can effectively minimize the risk of sural nerve injury during percutaneous Achilles tendon repair. Suturing the tendon in the fashion described enables greater tendon volume to be crossed without damaging the sural nerve or veins.
Author contributions
AI Performed surgeries, conceptualization, writing, revision, and supervision; MV Performed surgeries, conceptualization, writing, revision, and supervision; DF revision; JP revision; NM revision and supervision. All authors have read and agreed tothe published version of the manuscript.
Data availability
Data are available from the corresponding author upon reasonable request.
Declarations
Competing interests
Prof N. Maffulli is the Editor in Chief of the Journal of Orthopaedic Surgery and Research.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lemme NJ, Li NY, DeFroda SF, Kleiner J, Owens BD. Epidemiology of Achilles tendon ruptures in the united states: athletic and nonathletic injuries from 2012 to 2016. Orthop J Sports Med. 2018;6(11):2325967118808238. 10.1177/2325967118808238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guevara-Chávez FM, Caballero-Alvarado J, Zavaleta-Corvera C. Efficacy of surgical management versus Conservative management to decrease the incidence of re-rupture in adult patients with Achilles tendon rupture: A systematic review and meta-analysis. Muscles Ligaments Tendons J. 2024;14(1):54–66. 10.32098/mltj.01.2024.06. [Google Scholar]
- 3.Maffulli N, Sammaria G, Ziello S, Migliorini F, Oliva F. Percutaneous cruciate repair of ruptured Achilles tendon. J Orthop Surg Res. 2023;18(1):677. 10.1186/s13018-023-04167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carmont MR, Rossi R, Scheffler S, Mei-Dan O, Beaufils P. Percutaneous & mini invasive Achilles tendon repair. Sports Med Arthrosc Rehabilitation Therapy Technol. 2011;3(1):28. 10.1186/1758-2555-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webb JM, Bannister GC. Percutaneous repair of the ruptured tendo achillis. J Bone Joint Surg Br Volume. 1999;81–B(5):877–80. 10.1302/0301-620X.81B5.9784. [DOI] [PubMed] [Google Scholar]
- 6.Häggmark T, Liedberg H, Eriksson E, Wredmark T. Calf muscle atrophy and muscle function after non-operative vs operative treatment of Achilles tendon ruptures. Orthopedics. 1986;9(2):160–4. 10.3928/0147-7447-19860201-06. [DOI] [PubMed] [Google Scholar]
- 7.Carmont MR, Rossi R, Scheffler S, Mei-Dan O, Beaufils P. (2011). Percutaneous & mini invasive Achilles tendon repair. Sports Medicine, Arthroscopy, Rehabilitation, Therapy and Technology, 3(1), 28. 10.1186/1758-2555-3-28 [DOI] [PMC free article] [PubMed]
- 8.Venkateshaiah S, Reddy AGR, Srikantaiah VC. Transfer of the flexor hallucis longus tendon for neglected and degenerative tendo achillis rupture: A prospective clinical study. Muscles Ligaments Tendons J. 2023;13(2):243–51. 10.32098/mltj.02.2023.07. [Google Scholar]
- 9.Del Buono A, Volpin A, Maffulli N. Minimally invasive versus open surgery for acute Achilles tendon rupture: A systematic review. Br Med Bull. 2014;109(1):95–114. 10.1093/bmb/ldt029. [DOI] [PubMed] [Google Scholar]
- 10.Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: A multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg. 2010;92(17):2767–75. 10.2106/JBJS.I.01401. [DOI] [PubMed] [Google Scholar]
- 11.Metz R, Van Der Heijden GJMG, Verleisdonk EJMM, Kolfschoten N, Verhofstad MHJ, Van Der Werken C. Effect of complications after minimally invasive surgical repair of acute Achilles tendon ruptures: report on 211 cases. Am J Sports Med. 2011;39(4):744–9. 10.1177/0363546510392012. [DOI] [PubMed] [Google Scholar]
- 12.Maffulli N, D’Addona A, Maffulli GD, Gougoulias N, Oliva F. Delayed (14–30 days) percutaneous repair of Achilles tendon ruptures offers equally good results as compared with acute repair. Am J Sports Med. 2020;48(5):1134–41. 10.1177/0363546520908592. [DOI] [PubMed] [Google Scholar]
- 13.Carmont MR, Maffulli N. Modified percutaneous repair of ruptured Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):150–3. 10.1007/s00167-007-0411-z. [DOI] [PubMed] [Google Scholar]
- 14.Maffulli N, Longo UG, Spiezia F, Denaro V. Minimally invasive surgery for Achilles tendon pathologies. Open Access J Sports Med. 2010;1:95–103. 10.2147/oajsm.s7752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Majewski M, Rohrbach M, Czaja S, Ochsner P. Avoiding Sural nerve injuries during percutaneous Achilles tendon repair. Am J Sports Med. 2006;34(5):779–83. 10.1177/0363546505283266. [DOI] [PubMed] [Google Scholar]
- 16.Lim J, Dalal R, Waseem M. Percutaneous vs. open repair of the ruptured Achilles tendon - A prospective randomized controlled study. Foot Ankle Int. 2001;22(7):559–68. 10.1177/107110070102200705. [DOI] [PubMed] [Google Scholar]
- 17.Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture: immobilization versus functional postoperative treatment. Clin Orthop Relat Res. 1997;341:113–22. 10.1097/00003086-199708000-00018. [PubMed] [Google Scholar]
- 18.Ricci S, Moro L, Antonelli Incalzi R. Ultrasound imaging of the Sural nerve: ultrasound anatomy and rationale for investigation. Eur J Vasc Endovasc Surg. 2010;39(5):592–7. 10.1016/j.ejvs.2009.11.024. [DOI] [PubMed] [Google Scholar]
- 19.Hamada T, Toribatake Y, Okamoto S, Sakagoshi D, Ota T, Nishimura M. Positional relationship between the Achilles tendon and Sural nerve on ultrasound. J Med Ultrason. 2023;50(3):447–52. 10.1007/s10396-023-01312-z. [DOI] [PubMed] [Google Scholar]
- 20.Iborra A, Villanueva M, Barrett SL, Rodriguez-Collazo E, Sanz P. Anatomic delineation of tarsal tunnel innervation via ultrasonography. J Ultrasound Med. 2018;37(6):1353–9. 10.1002/jum.14499. [DOI] [PubMed] [Google Scholar]
- 21.Iborra Marcos Á, Villanueva Martínez M, Fahandezh-Saddi Díaz H. Needle-based gastrocnemius lengthening: a novel ultrasound-guided noninvasive technique. J Orthop Surg Res. 2022;17(1):291. 10.1186/s13018-022-03318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iborra A, Villanueva M, Sanz-Ruiz P. Results of ultrasound-guided release of tarsal tunnel syndrome: A review of 81 cases with a minimum follow-up of 18 months. J Orthop Surg Res. 2020;15(1):487. 10.1186/s13018-020-1559-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iborra-Marcos A, Villanueva-Martinez M, Barrett SL, Sanz-Ruiz P. Ultrasound-guided decompression of the intermetatarsal nerve for morton’s neuroma: A novel closed surgical technique. J Am Podiatr Med Assoc. 2020;110(6):480–6. 10.7547/19-033. [DOI] [PubMed] [Google Scholar]
- 24.Campillo-Recio D, Comas-Aguilar M, Ibáñez M, Maldonado-Sotoca Y, Albertí-Fitó G. Percutaneous Achilles tendon repair with absorbable suture: outcomes and complications. Revista Española De Cirugía Ortopédica Y Traumatología. 2023;67(2):98–105. 10.1016/j.recot.2022.08.009. [DOI] [PubMed] [Google Scholar]
- 25.Maffulli N, Dymond NP, Regine R. Surgical repair of ruptured Achilles tendon in sportsmen and sedentary patients: A longitudinal ultrasound assessment. Int J Sports Med. 1990;11(1):56–60. 10.1055/s-2007-1024767. [DOI] [PubMed] [Google Scholar]
- 26.Bergamin F, Civera M, Reinoso MR, Burgio V, Ruiz OG, Surace C. Worldwide incidence and surgical costs of tendon injuries: A systematic review and meta-analysis. Muscles Ligaments Tendons J. 2023;13(1):64. 10.32098/mltj.01.2023.05. [Google Scholar]
- 27.Park SH, Lee HS, Young KW, Seo SG. Treatment of acute Achilles tendon rupture. Clin Orthop Surg. 2020;12(1):1–8. 10.4055/cios.2020.12.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma GWC, Griffith TG. Percutaneous repair of acute closed ruptured Achilles tendon: a new technique. Clin Orthop Relat Res. 1977;128:55–8. [PubMed] [Google Scholar]
- 29.Giannetti S, Patricola AA, Stancati A, Santucci A. Intraoperative ultrasound assistance for percutaneous repair of the acute Achilles tendon rupture. Orthopedics. 2014;37(12):e1119–24. 10.3928/01477447-20141124-04. [DOI] [PubMed] [Google Scholar]
- 30.Paczesny Ł, Zabrzyński J, Domżalski M, et al. Mini-invasive, ultrasound guided repair of the Achilles tendon rupture—a pilot study. J Clin Med. 2021;10(11):2370. 10.3390/jcm10112370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iborra A, Villanueva M, Sanz-Ruiz P, Martin A, Noriega C. A novel closed technique for ultrasound-guided plantar fascia release with a needle: review of 107 cases with a minimum follow-up of 24 months. J Orthop Surg Res. 2021;16(1):243. 10.1186/s13018-021-02302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Villanueva M, Iborra Á, Fahandezh-Saddi H, Sanz-Ruiz P, Noriega C. Ultrasound-guided aponeurotomy and interphalangeal joint capsular release for treatment of dupuytren’s disease. J Hand Surgery: Eur Volume. 2022;47(7):720–6. 10.1177/17531934221083815. [DOI] [PubMed] [Google Scholar]
- 33.Villanueva M, Iborra Á, Ruiz MdelM, Sanz-Ruiz P. Proximal ultrasound-guided gastrocnemius recession: A new ultra-minimally invasive surgical technique. J Foot Ankle Surg. 2019;58(5):884–9. 10.1053/j.jfas.2018.12.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.