Abstract
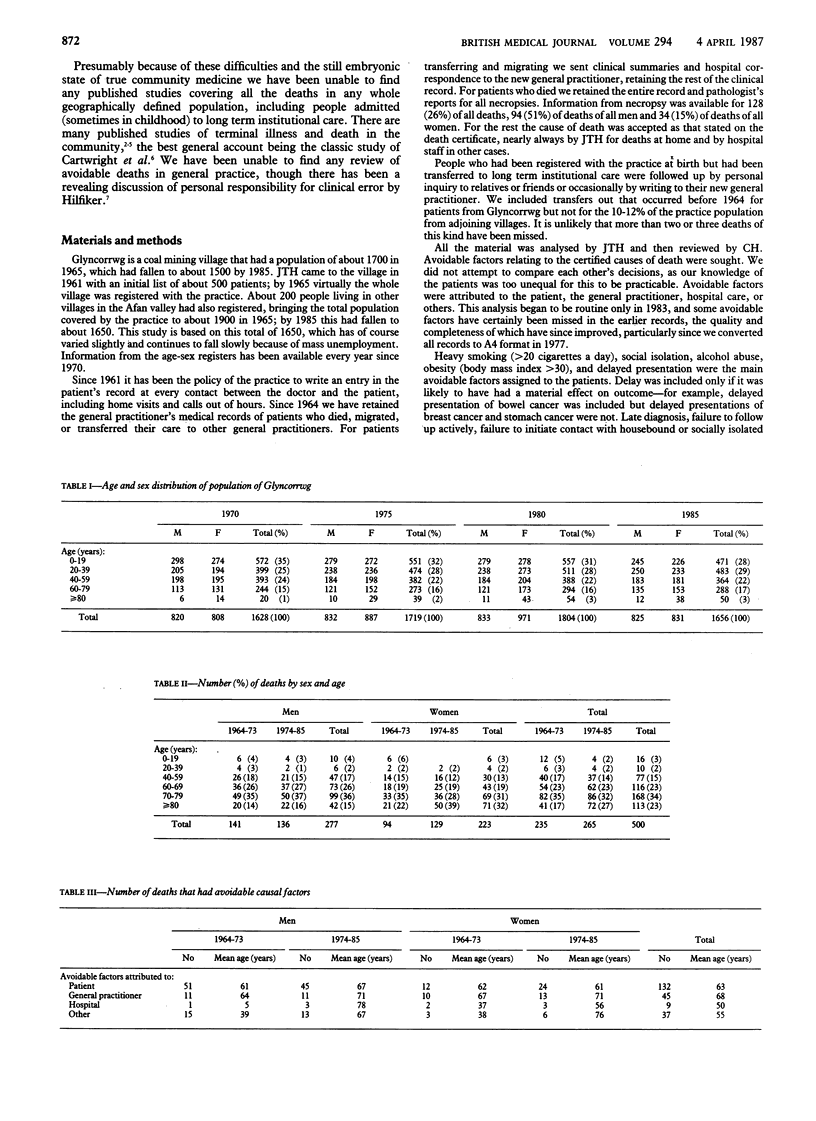
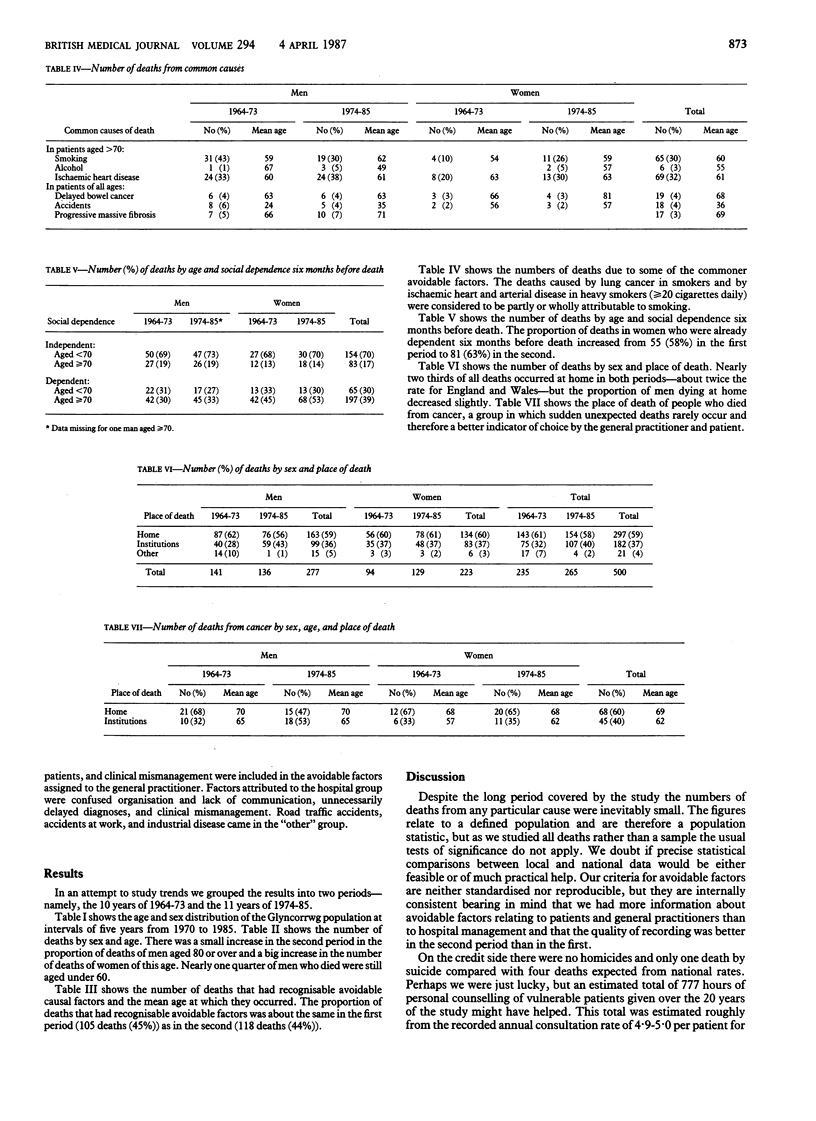
General practitioners' medical records of a geographically defined population of about 1600-1800 have been retained since 1964. Details of care by general practitioners and hospital correspondence were available for 500 deaths (277 men, 223 women) from 1964 to 1985, including deaths at home, at work, in the street, in short term and long term institutional care, and within six months of release from institutional care. The periods 1964-73 and 1974-85 were compared. The proportion of men aged greater than or equal to 80 who died increased from 20 (14%) in 1964-73 to 22 (16%) in 1974-85, but the proportion of women aged greater than or equal to 80 who died increased from 21 (23%) to 50 (39%). Of all deaths, 223 (45%) were thought to have had avoidable causal factors, of which 132 (59%) were attributed to patients, 45 (20%) to the general practitioner, 9 (4%) to hospitals, and 37 (17%) to others. The number of deaths related to smoking decreased from 31 (43%) in men aged less than 70 to 19 (30%) but in women aged less than 70 increased from 4 (10%) to 11 (26%). The proportion of deaths in women who were already dependent six months before death increased from 55 (58%) to 81 (63%) but in men remained constant at 64 (46%) in the first period and 62 (46%) in the second. Nearly two thirds of all deaths occurred at home in both periods--about twice the proportion for England and Wales--but the proportion of men dying at home decreased from 87 (62%) to 76 (56%). A critical analysis of deaths in whole populations by primary care teams can identify changes that are needed both in the work and organisation of the team and in the behaviour of the population itself.
Full text
PDF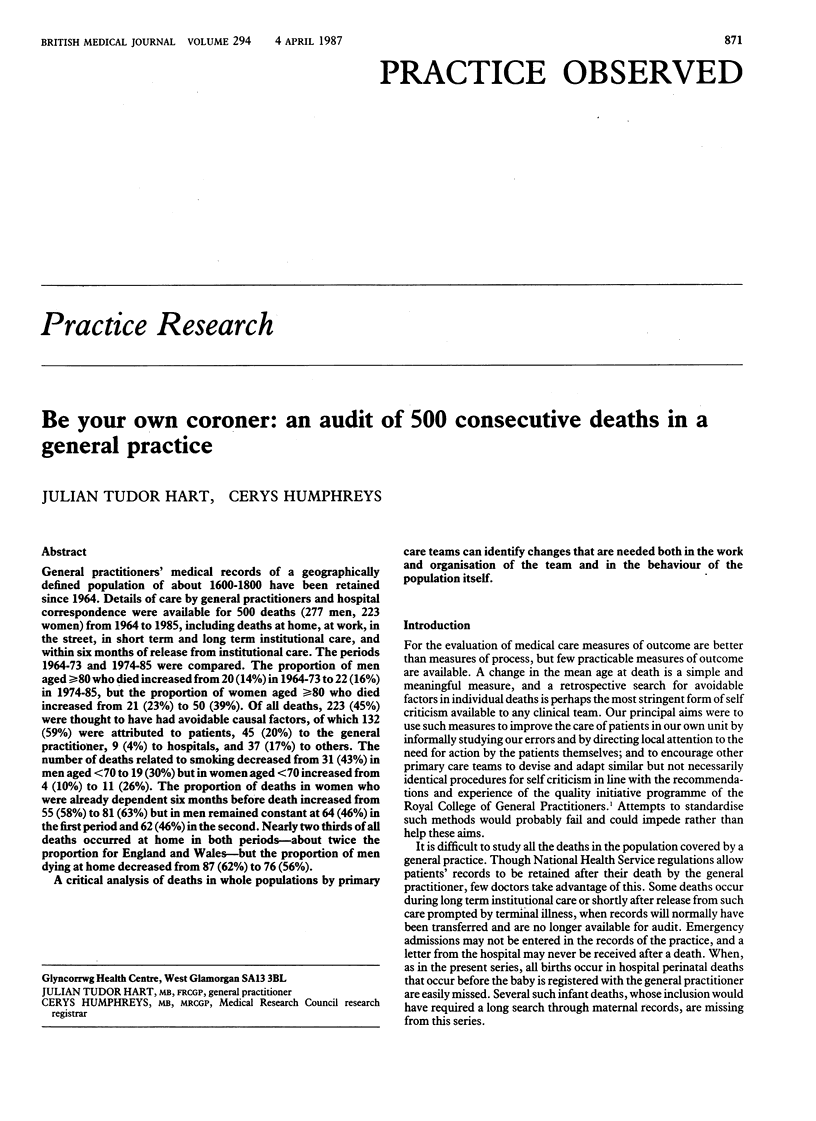

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Byfield P. E., Stratton J. A., Small R. Letter: Lymphocyte response after radiotherapy. Lancet. 1974 Feb 23;1(7852):309–309. doi: 10.1016/s0140-6736(74)92611-7. [DOI] [PubMed] [Google Scholar]
- Caldwell J. R. One hundred deaths in practice. A study of terminal care. J R Coll Gen Pract. 1971 Aug;21(109):460–468. [PMC free article] [PubMed] [Google Scholar]
- Forsythe K. "The ultimate diagnosis". Ulster Med J. 1971;40(1):1–13. [PMC free article] [PubMed] [Google Scholar]
- Hardcastle J. D., Armitage N. C. Early diagnosis of colorectal cancer: a review. J R Soc Med. 1984 Aug;77(8):673–676. doi: 10.1177/014107688407700812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B. Fatal illness in general practice. J R Coll Gen Pract. 1976 Apr;26(165):303–307. [PMC free article] [PubMed] [Google Scholar]
- MacAdam D. B. Delay in diagnosis of symptomatic colorectal cancer. Lancet. 1979 Mar 3;1(8114):489–490. [PubMed] [Google Scholar]
- Parkes C. M. Home or hospital? Terminal care as seen by surviving spouses. J R Coll Gen Pract. 1978 Jan;28(186):19–30. [PMC free article] [PubMed] [Google Scholar]


