Abstract
Three drug-dependent mutants of human rhinovirus 16 (HRV16) were characterized by sequence analyses of spontaneous mutant isolates and were genetically reconstructed from a parental cDNA plasmid. These mutants formed plaques in the presence but not in the absence of the selecting antiviral drug, WIN 52035, which binds to the capsid of wild-type virus and inhibits its attachment to the host cell. The drug-dependent phenotype of each mutant was caused by a single amino acid substitution in the VP1 coat protein. The three independent mutations conferring drug dependence are M1103T, T1208A, and V1210A. Single-step growth experiments involving rescue of one of the three mutants (V1210A) by delayed drug addition suggested (i) that the drug dependence lesion is at the stage of virus assembly and (ii) that one or more components of the viral assembly pool decay in the absence of drug. RNA accumulation and infectivity were unaffected by the absence of drug in all three mutants, suggesting that the labile assembly component is coat protein.
Human rhinoviruses (HRV) are the single most important causative agents of common colds in humans. They cause one-third to one-half of all acute respiratory disease (11, 13, 18). HRV16, a major-group serotype that utilizes ICAM-1 (intercellular adhesion molecule-1) on the host cells as its cellular receptor (17, 45), is a good model for clinical studies since it reproducibly causes cold symptoms in human volunteers (4, 6, 28). For example, HRV16 has been used as a model for studying the transmission of colds (12, 33) and the exacerbation of asthma (4, 5, 28). It is also ideal for structural and genetic studies since its crystal structure (19, 37) and cDNA are available.
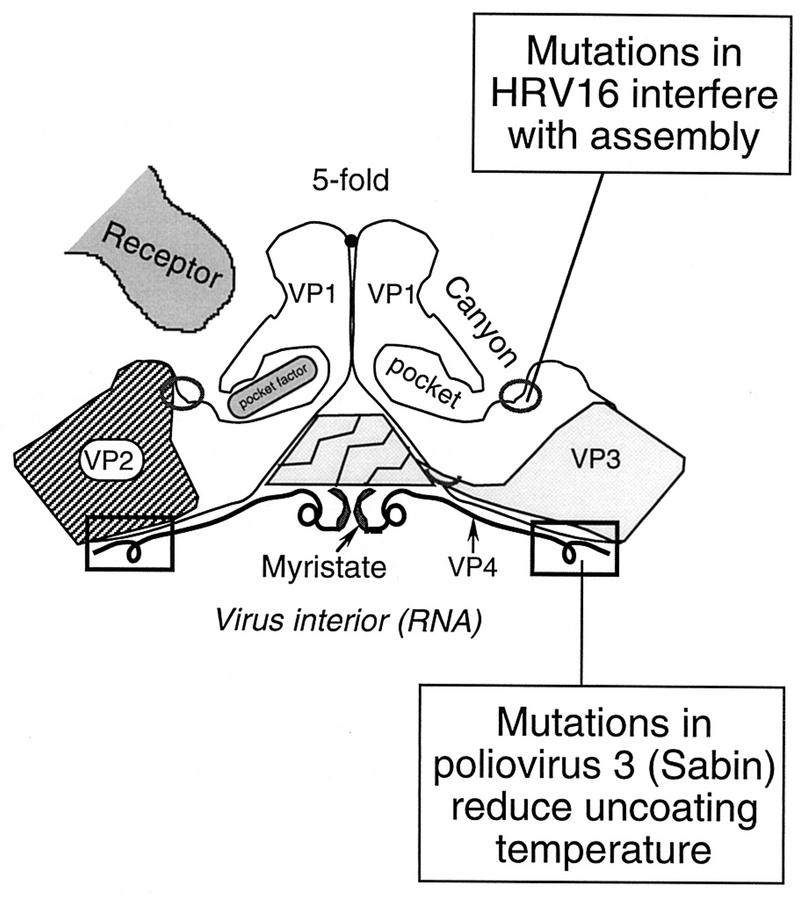
Rhinoviruses are members of the family Picornaviridae, which also includes poliovirus, encephalomyocarditis virus, and foot-and-mouth disease virus. These viruses are small nonenveloped icosahedral particles containing one single-stranded message-sense genomic RNA. The capsid is made up of 60 copies each of four polypeptides (VP1, VP2, VP3, and VP4) which are symmetrically organized into promoters, pentamers, and icosahedral shells (40). Surrounding each fivefold icosahedral vertex of the virus particle there is a canyonlike depression on the virion surface, which is mostly contributed by the structure of the VP1 peptides and is the binding site for cellular receptor (9, 10, 39, 44). The VP4 peptides lie at the inner surface of the capsid and are in contact with the genomic RNA (15, 22, 39, 40). The structure of VP1 within each protomer also harbors a pocket, which lies just beneath the canyon floor and has a pore leading to the surface of the particle. Some electron density, called pocket factor, has been observed by crystallography in the pockets of some human picornaviruses such as HRV16, HRV1A, and poliovirus types 1 and 3 (15, 22, 23, 37). The chemical identity and biological function of pocket factor are not known.
Human rhinoviruses, like other picornaviruses, multiply in the cytoplasm of their host cells. The infection cycle includes attachment, uncoating, RNA and protein synthesis, virion assembly, and exit from cells. The initial cellular attachment step is mediated by recognition and binding of receptors via the canyon. The virus particle then undergoes several conformational changes resulting in penetration of the membrane and release of the genomic RNA into the cell (uncoating). The uncoated RNA serves as the message for viral protein translation and as the template for minus-strand RNA synthesis. Capsid proteins and plus-strand RNA accumulate in the cell and assemble through multiple steps into noninfective 150S provirions, which then mature (by cleavage of VP0 to VP4 plus VP2) into infective 150S virions and exit the host cell upon cell lysis.
Capsid-binding drugs, such as the WIN drugs (after Sterling-Winthrop Pharmaceuticals Research Division), are currently the most promising antiviral agents against human rhinoviruses and human enteroviruses (3, 14, 31, 34). They are small hydrophobic molecules that inhibit virus infectivity by blocking its attachment to cells (as in HRV14 or HRV16) or uncoating (as in HRV1A, HRV2, or poliovirus 3) (16, 35, 41, 47). Crystallographic studies have shown that these drugs bind in the VP1 pocket underneath the canyon and that drug binding elevates the pocket roof on the canyon floor of HRV14 (43) but does not deform the canyon floor of HRV16 (37). This finding suggests that proper seating of cellular receptor requires deformation of the canyon floor downward (37). Control of the canyon floor has now become the working model for explaining how WIN drugs block attachment. In addition, affecting rearrangement of the capsid proteins offers a model for explaining the block of uncoating.
Drug-resistant mutants provide tools for studying picornavirus capsid functions. Mapping drug resistance mutations has been proposed as a way of identifying regions within the viral coat protein that are critical for cellular attachment or uncoating (21). Previous studies in our lab have revealed two phenotypic classes of picornavirus drug-resistant mutants: drug-dependent and nondependent (20, 35). Drug-dependent mutants form plaques in the presence of drug but not in its absence, while nondependent mutants form plaques with approximately equal levels of efficiency in the presence and absence of drug. Drug-dependent mutants are particularly useful tools for dissecting the picornavirus infection mechanism because the capsid-binding drugs, as experimental reagents, play a positive role in their life cycle.
We report here the search for and characterization of HRV16 mutants that are dependent on WIN 52035 for plaque formation. The same drug was previously used for selection and analyses of HRV14 drug-resistant mutants (41).
MATERIALS AND METHODS
Cells, virus, and drugs.
HeLa cells, free of mycoplasma (25), were passaged in suspension culture in medium B as described previously (32). HRV16 stock has been described elsewhere (26). WIN 52035-2 (referred to as WIN 52035), WIN 52084(S) (referred to as WIN 52084), WIN 51711, and WIN 56291 were gifts from G. Diana at the former Sterling-Winthrop Pharmaceuticals Research Division (34, 37). R61837 (manufactured by Janssen Pharmaceuticals) was a gift from M. G. Rossmann, Purdue University, West Lafayette, Ind. (2).
Each drug was dissolved in dimethyl sulfoxide (DMSO) to 10 mg/ml and kept as stock, which was diluted before use at least 1,000 times in medium or PBS4A (phosphate-buffered saline [PBS] with 0.4% bovine serum albumin [BSA]). Up to 0.1% DMSO in the medium had no apparent effect on the growth properties of HeLa cells either in suspension or in monolayer culture (41).
Virus amplification and purification.
Virus was propagated at 35°C in HeLa cell suspension or cell monolayers as described previously (26, 42). HeLa cells were infected at room temperature for 1 h with a multiplicity of infection (MOI) of 10 to 15 PFU per cell. Infected cell suspensions were diluted 10-fold to 4 × 106 cells/ml in prewarmed medium B and incubated at 35°C for 7 to 8 h. The cells were then pelleted and resuspended in PBS at the initial volume. Infected cell monolayers were overlaid with 2 ml of medium A, incubated at 35°C until a cytopathic effect was observed (after 30 to 40 h), and then scraped from dishes. Virus was released from cells by three cycles of freezing and thawing and then harvested as the supernatant after centrifugation to pellet cell debris.
For purification on sucrose gradients, virus was released from cells either as described above or by lysing the cells with 0.5% Nonidet P-40. The lysate was supplemented with 1% sarcosyl and 0.1% 2-mercaptoethanol and was then subjected to centrifugation through a 1-ml 30% sucrose cushion in a Beckman SW41 rotor (40,000 rpm, 16°C, 130 min). Pelleted virus was resuspended in PBS with 0.01% BSA and subjected to centrifugation on a 7.5 to 45% sucrose gradient (Beckman SW41 rotor, 40,000 rpm, 16°C, 100 min). The gradient fraction(s) containing the most concentrated virus band was collected and stored at −70°C.
Radiolabeling and sucrose gradient sedimentation of virus.
HeLa cell suspensions (4 × 107 cells/ml) in PBS or PBS4A were infected with virus (MOI of 10 to 15) at room temperature for 1 h. The infected cells were diluted 10-fold in prewarmed medium B lacking all amino acids except l-glutamine and incubated at 35°C with gentle shaking. [35S]methionine was added to cell suspension (20 μCi/ml) at 4 to 4.5 h after infection. Virus was harvested after 7 to 8 h and pelleted through a 1-ml 30% sucrose cushion. The viral pellet was resuspended in PBS4A and sedimented on a 7.5 to 45% sucrose gradient as described above. The gradient was fractionated (0.4 ml per fraction) from top to bottom. Sample radioactivity was determined by liquid scintillation counting.
Plaque assay.
The procedure was described by Heinz et al. (20). HeLa monolayers were prepared by plating 2.5 × 106 cells (suspended in 5 ml of medium A with serum) in each 60-mm-diameter dish and then incubating them at 37°C for 12 h. Virus samples diluted in PBS4A were pipetted onto PBS-washed monolayers and were allowed to incubate at room temperature for 1 h. The infected monolayers were overlaid first with 2.5 ml of 0.8% agar in medium P6 (42) and then with 2.5 ml of medium P6 containing 0.8% BSA, 4 mM glutamine, 4 mM oxaloacetate, 2 mM pyruvate, and 11.2 mM d-glucose. Plaques were allowed to develop at 35°C for 50 to 60 h and then visualized by crystal violet staining.
Dose-response curve.
Virus was propagated in HeLa cells with an MOI of 0.1 to 0.5 PFU per cell to minimize the presence of pseudovirions (mutant genome with wild-type capsid) in the stock, which results in an underestimation of mutant frequency. A series of WIN 52035 stocks in DMSO were diluted 1,000 times in PBS4A, agar overlay, or nutrient overlay to prepare three sets of working solutions; each set contained a series of specified concentrations of the drug. Virus was diluted serially in PBS4A containing drug at each concentration and DMSO at the same concentration (0.1% or less). DMSO minus drug was the negative-drug control. Plaque assays were performed as described above. For each monolayer, the agar and nutrient overlays contained the same concentration of drug as the initial inoculum in PBS4A.
Mutant selection and amplification.
The strategy of selecting drug-resistant mutants was described by Heinz et al. (20). Plaque-purified wild-type virus was plated on HeLa cell monolayers in the presence of 2 μg of WIN 52035 per ml to select for resistant plaques. These plaques were visualized by live staining with 0.01% neutral red at 35°C for 2 h. Representative individual plaques were isolated with Pasteur pipettes; each isolate was stored in 0.5 ml of PBS4A in the presence of drug. Each mutant isolate was replated both in the presence and in the absence of 2 μg of WIN 52035 per ml to determine whether it was drug dependent or nondependent.
The mutant isolates were first amplified on HeLa monolayers in the presence of drug, further plaque purified once or twice to remove contaminating wild-type virus, and propagated in HeLa cell suspensions. The mutant stocks, whose titers ranged from 5 × 108 to 5 × 109 PFU/ml, were stored in PBS at −70°C.
Single-step growth curves.
The procedure was described by Shepard et al. (41). Virus was diluted in PBS4A. HeLa cells were washed with and resuspended in PBS. Virus (10 to 15 PFU/cell) was mixed with HeLa cells (4 × 107 cells/ml) in a 15-ml polypropylene tube and incubated at room temperature for 1 h with gentle shaking. The infected cells were then pelleted, washed with PBS (or PBS4A) to remove unattached virus, resuspended (to 4 × 106 cells/ml) in prewarmed (35°C) medium B, and incubated at 35°C with shaking. Samples were taken from infected cell suspensions at intervals, supplemented to 50 mM with HEPES buffer (pH 7.4), and frozen immediately in a dry ice-ethanol bath. Virus was released from cells by the freeze-thaw method and harvested as the supernatant after clarifying centrifugation. Infectivity was determined by plaque assay. A final WIN 52035 concentration of 2 μg/ml was used where needed.
Viral and cellular RNA preparations.
The acid guanidinium thiocyanate and phenol-chloroform method (7) was modified and described below. A sample of the virus preparation or infected HeLa cells was dissolved in solution D (4 M guanidine thiocyanate, 25 mM sodium citrate [pH 7.0], 0.5% sarcosyl, 0.5% 2-mercaptoethanol). It was incubated on ice for 15 min with 0.1 volume of 2 M sodium acetate (pH 4.0), 1 volume of water-saturated phenol, and 0.2 volume of (24:1) chloroform-isoamyl alcohol and then subjected to centrifugation in a microcentrifuge (at 14,000 rpm for 20 min). The upper (aqueous) phase contained RNA, which was precipitated by incubation with 1 volume of isopropanol at −20°C for 2 h or longer and then pelleted by centrifugation. For further purification, the RNA pellet was resuspended in solution D and reprecipitated with an equal volume of isopropanol. For removal of residual guanidine thiocyanate, the RNA was resuspended in diethylpyrocarbonate-treated water and then precipitated by addition of 0.1 volume of 2 M sodium acetate (pH 4.0) and 1.1 volume of isopropanol. Purified RNA was stored in diethylpyrocarbonate-treated water at −20°C.
RNA and DNA sequencing.
Viral RNA was sequenced by primer extension as described by Air (1). Avian myeloblastosis virus reverse transcriptase was purchased from Promega Inc., Madison, Wis. A set of 21 minus-strand primers (18 to 20 nucleotides) complementary to the viral genomic sequence and covering the coat genes (26) was synthesized at the Biotechnology Center of the University of Wisconsin. The RNA sample was mixed with a specific primer, boiled for 1 min, and then cooled gradually to facilitate annealing. Primer extension was then carried out at 42°C for 30 min in the presence of 5 μCi of [α-35S]dATP and 3 U of reverse transcriptase per reaction, and with a deoxynucleoside triphosphate/dideoxynucleoside triphosphate ratio of 5, 6, 4, or 7 in the respective A, C, G, or T reaction. Each reaction product was mixed with FDE (95% formamide, 20 mM EDTA, 0.05% bromophenol blue, and 0.05% xylene cyanol FF), boiled for 3 min, and electrophoresed on 4.8% polyacrylamide gels, which were then fixed, dried, and autoradiographed.
Double-stranded DNA sequencing by the dideoxynucleotide method was performed with a Sequenase kit (United States Biochemical Corp.) according to the manufacturer’s instructions.
Site-directed mutagenesis.
A full-length HRV16 cDNA plasmid that produces highly infectious RNA transcripts was constructed (24a). Overlapping fragments of the full-length cDNA were subcloned for use as mutagenesis cassettes. Subclones pR16-1AB (containing the HpaI/NdeI fragment), pR16-1C (NdeI/AvrII), and pR16-1D (AvrII/ClaI) collectively covered the entire viral coat gene.
The method of site-directed mutagenesis was described elsewhere (24, 25). Negative-sense, uracil-rich, and single-stranded DNA of each subclone was prepared with the Escherichia coli dut ung mutant strain (CJ236) and M13 helper phage. Positive-sense mutagenic primers (18 to 20 nucleotides) were synthesized as described above. Each primer was phosphorylated at its 5′ end with T4 polynucleotide kinase and then annealed to its complementary single-stranded DNA plasmid containing the desired genomic site for the mutation. The mutagenic strand was synthesized with T4 DNA polymerase, circularized with T4 DNA ligase, and then used to transform competent E. coli DH5α cells. Plasmids containing the desired mutation(s) were identified by dideoxy sequencing. The mutation was then introduced through subcloning into a full-length viral cDNA plasmid by replacing a fragment of the full-length wild-type cDNA plasmid with the corresponding mutated fragment.
Transfection.
The DEAE-dextran-facilitated transfection procedure was described elsewhere (25). Viral RNA preparation or RNA transcripts from viral cDNAs was diluted in HEPES-buffered saline containing 200 μg of DEAE-dextran per ml. HeLa cell monolayers were washed with HEPES-buffered saline. The RNA dilution was pipetted onto prewashed monolayers and incubated at room temperature for 1 h. The cell monolayers were washed with PBS to remove the DEAE-dextran, overlaid as for plaque assay, and incubated at 35°C for plaque formation.
For production of virus, the transfected cell monolayers were incubated in medium A at 35°C until cytopathic effect was observed (after 40 to 50 h). Virus was harvested from cells scraped from dishes as described above.
RESULTS
Effect of drug concentration on plating efficiency.
The inhibitory effect of WIN 52035 appeared at about 0.1 μg/ml (Fig. 1). At higher concentrations, the plaque titer decreased about 104-fold, leveling off at about 1 μg/ml (plateau). The relative plaquing efficiency within the plateau, 10−4, was consistent with the high mutation rate (10−4 to 10−5) that is typically found in RNA viruses. The dropoff at drug concentrations above 4 μg/ml was accompanied by paler staining of the cell monolayers, suggesting a toxic effect of the drug on HeLa cells. That the plateau consists largely of drug-resistant mutants was confirmed by replating representative plaque isolates both in the presence and in the absence of drug.
FIG. 1.
Plating efficiency of HRV16 in various concentrations of WIN 52035. Plaque-purified virus stock, amplified at 0.5 PFU per cell, was serially diluted in PBS4A containing WIN 52035 at the indicated concentrations, and these samples were incubated at room temperature for 1 h. Virus in PBS4A containing the same concentration of DMSO, minus drug, was used as a control. Viral dilutions were then pipetted onto HeLa cell monolayers and left at room temperature for 1 h. Monolayers were overlaid with agar and medium P6, which contained drug of the same concentration as the previous incubation. Plaques were allowed to develop at 35°C for 60 h under 5% CO2. The relative plaquing efficiency is the ratio of plaque titer obtained in the presence of drug to that obtained in the absence of drug. (The relative plaquing efficiency at each drug concentration is the mean of results from four to six different dishes in one experiment, and the error bar is the standard deviation.)
Strategy for isolating drug-dependent mutants.
The isolation procedure involved two experimental steps. (i) A collection of 118 drug-resistant isolates was selected by plating a panel of 20 independent plaque-purified wild-type HRV16 stocks on HeLa cell monolayers in the presence of 2 μg of WIN 52035 per ml. (ii) Each isolate was then replated in the presence or absence of the drug to screen for drug-dependent mutants, i.e., those forming plaques with higher efficiency in the presence of drug than in its absence. Nine of the 118 isolates were drug dependent (Table 1). The remaining isolates were nondependent, that is, formed plaques with the same efficiency in the presence or absence of drug.
TABLE 1.
Selection of WIN 52035-dependent mutants of HRV16
| Isolate no. | Relative plaquing efficiencya
|
||
|---|---|---|---|
| 1st plaquing | 2nd plaquing | 3rd plaquing | |
| 1 | 23 | 220 | 1,300 |
| 2 | 6 | 70 | 3,200 |
| 3 | 29 | 1,800 | 5,000 |
| 4 | 44 | 8,000 | 10,000 |
| 5 | 280 | 290 | 850 |
| 6 | 70 | 2,500 | 6,000 |
| 7 | 210 | 11,000 | 5,000 |
| 8 | 110 | 3,200 | 10,000 |
| 9 | 17 | 110 | 6,000 |
Defined as the plaque titer in the presence of 2 μg of WIN 52035 per ml divided by that in the absence of the drug.
The enhancing effect of WIN 52035 on relative plaquing efficiency of the initial drug-dependent isolates varied from 6- to 280-fold (Table 1, column 2). After the second and third rounds of plaque purification (columns 3 and 4), the plaquing efficiencies trended upward toward 104, except for isolates 1 and 5, which were subsequently shown to harbor different mutations. Further plaque purification no longer increased the plaquing efficiencies (not shown). This progressive enhancing effect of drug with serial plaquings can be attributed to progressive elimination of contaminating wild-type virus. Thus, one or two additional rounds of replaquing were necessary to purify the mutant isolates for sequence analyses and biological characterization. Residual plaques that appeared in the absence of drug (at a frequency on the order of 10−4) after removal of wild-type virus probably represent true revertants.
Identification of the mutations conferring drug dependence and reconstruction of mutants with cDNA.
Candidate mutations were identified in each of the nine drug-dependent isolates after the viral coat genes were fully or partially sequenced. These mutations were then individually introduced into a cDNA plasmid of the parental genotype to verify whether each mutation confers drug dependence. A total of three mutations were confirmed in this way; each independently confers drug dependence by causing a single amino acid substitution in the VP1 capsid protein: M1103T (in isolate 1), T1208A (in isolate 5), and V1210A (in the other seven isolates) (Table 2). A fourth mutation, E3081Q (in isolates 3 and 4, which were originally from the same plaque-purified virus stock), was identified but proved by site-directed mutagenesis to confer the wild-type phenotype. Thus, we believe that it is a random mutation unrelated to drug dependence. For subsequent studies of the three drug-dependent mutants, the viruses derived from cDNA constructs were used since cDNAs provided defined genotypes.
TABLE 2.
Mutations in VP1 that confer drug dependence
| Amino acid substitutiona | Codon mutation | Isolate no.b |
|---|---|---|
| V1210A | GUC→GCC | 2, 3,c 4,c 6, 7, 8, 9 |
| T1208A | ACU→GCU | 5 |
| M1103T | AUG→ACG | 1 |
The flanking letters represent the amino acid residues in the wild-type and mutant viruses, respectively; the first digit represents the capsid peptide (i.e., 1 for VP1); and the subsequent three digits represent the residues numbered 1 to 285 from the amino end.
See Table 1.
Harbors an additional mutation (E3081Q) which subsequently proved unrelated to drug dependence by site-directed mutagenesis.
Dose response of mutant V1210A to WIN 52035 and four other drugs.
To study the precise concentration of WIN 52035 required for the rescue of the drug-dependent mutants, we analyzed the plaque-forming ability of mutant V1210A in the presence of various concentrations of WIN 52035. A detectable rescue of V1210A plaque formation by WIN 52035 was achieved above 0.1 μg/ml (Fig. 2), the same concentration at which the drug began to inhibit plaque formation of wild-type HRV16 (Fig. 1). Moreover, this drug reached maximal rescuing effect on V1210A plaque formation at about 1 μg/ml (Fig. 2), the same concentration at which the drug reached maximal inhibition of plaque formation of the wild-type virus (Fig. 1). This result suggests that the drug, despite its opposite effects on mutant and wild-type viruses, binds to their VP1 pockets with similar affinities.
FIG. 2.

Plating efficiency of mutant V1210A in the presence of five capsid-binding drugs (structures indicated at the bottom). Virus was serially diluted in PBS4A containing the indicated drug concentrations, and these samples were incubated at room temperature for 1 h to allow drug binding by the virus capsid. As a control, similar samples of virus were diluted into PBS4A containing DMSO, minus drug. Dilutions (0.2 ml) were then pipetted onto HeLa cell monolayers and left at room temperature for 1 h to allow for viral attachment. Monolayers were overlaid with agar in medium P6, containing the same drug at the same concentration as the previous incubation. Plaques were allowed to develop at 35°C for 60 h under 5% CO2. The relative plaquing efficiency is the ratio of virus titer in the presence of the drug to that in the absence of the drug.
Mutant V1210A infectivity could also be rescued by three of the other four drugs tested. R61837 was even more potent than WIN 52035, requiring only about 0.1 μg/ml for a maximal rescue (Fig. 2). Plaque formation declined at R61837 concentrations exceeding 1 μg/ml possibly because of residual interference with attachment or uncoating by the drug. WIN 51711 and WIN 52084 were somewhat less active, requiring about 4 μg/ml for complete rescue. WIN 56291 failed to rescue V1210A plaque formation. Rather, it demonstrated a slight inhibitory effect at concentrations above 0.1 μg/ml.
Evidence that drug-dependent mutants attach normally but are defective in assembly in the absence of drug.
To identify the step(s) at which drug-dependent mutants require WIN 52035, single-step growth experiments were carried out with progressively delayed addition of drug to the infected cell cultures. Each of the three mutants was allowed to attach to HeLa cells in the absence of drug at room temperature (23 to 25°C). The infected cells were divided into several aliquots, resuspended in prewarmed medium, and allowed to grow at 35°C. The drug was added to the cell suspensions at 0, 3, 5, and 7 h after transfer of samples to 35°C (Fig. 3).
FIG. 3.
Single-step growth experiments demonstrating the rescue of three drug-dependent mutant viruses by delayed drug addition. (A and B) Mutant V1210A; (C) mutant M1103T; (D) mutant T1208A. Panel B shows a more detailed time course for the rescue of V1210A (drug added at 5 h postinfection). In all experiments, virus was allowed to attach to HeLa cells (MOI of 15) in the absence of drug at room temperature for 1 h. The infected cells were then pelleted, washed with PBS to remove unattached virus, divided into several aliquots, resuspended in prewarmed medium, and then allowed to incubate at 35°C. WIN 52035 (final concentration, 2 μg/ml) was added to the samples at the times indicated by arrows. Samples were taken from each culture at the indicated times and frozen and thawed three times to release virus. Infectivity was determined by plaque assay on HeLa cells in the presence of 2 μg of WIN 52035 per ml.
In the absence of added drug, mutant V1210A eclipsed during the first few hours at 35°C but showed no evidence of multiplication (Fig. 3A). When the drug was added at 0 h, the mutant multiplied normally, reaching peak titers at 5 to 6 h. Its multiplication profile, including infectivity yield, was similar to that of wild-type virus (not shown). Delaying drug addition for 3 h had little, if any, effect on the final yield of virus. Thus, the drug was not required for attachment or uncoating of V1210A, although the slower eclipse rate of the mutant in the presence of drug suggested a slight inhibitory effect on its uncoating rate. Delaying drug addition 5 to 7 h progressively reduced the final yield of virus, suggesting that the pool of mutant assembly subunits in the cell decays in the absence of drug.
Notably, the infectivity of V1210A appeared very quickly after drug addition. A more detailed time course of the rescue confirmed that its infectivity increased markedly without a noticeable time lag, even after times as short as 5 min (Fig. 3B). The rapidity with which virions are assembled following drug addition suggests that addition of drug triggers assembly from an accumulated pool of preformed subunits, whose flow into virions after synthesis normally requires 0.5 h (40).
The growth curve of another drug-dependent mutant, M1103T, and its response to delayed drug addition were similar to those of mutant V1210A (Fig. 3C). However the third mutant, T1208A, behaved rather differently. In the absence of drug, it multiplied to some extent although its final yield was about 100-fold lower than when drug was present (Fig. 3D). For each of the three drug-dependent mutants, addition of WIN 52035 as late as 5 h after the start of the growth cycle rescued 30 to 40% of the full infection yield. These results suggest that all three mutants are defective in virion assembly.
Evidence that accumulation and integrity of mutant RNA are not affected by the absence of drug.
To investigate whether RNA of the drug-dependent mutants is the unstable component of the viral assembly pool in the absence of drug, total RNA was isolated from samples of infected cell cultures in a set of single-step growth experiments. The amount of infective viral RNA was determined by transfecting HeLa cell monolayers with the total RNA sample and by counting plaques developed in the presence of WIN 52035.
The rise of V1210A infective RNA during the first few hours in the growth cycle demonstrated no significant differences between the presence and absence of WIN 52035 (Fig. 4). Synthesis of infective RNA by mutant V1210A was similar or slightly less than that by wild-type virus. Moreover, both mutant and wild-type RNAs remained infective in the absence of drug even after their synthesis was complete. Thus, drug was not required for synthesis of mutant RNA, nor was it required for protection of RNA infectivity. Studies of the other two drug-dependent mutants, M1103T and T1208A, gave the same results (data not shown).
FIG. 4.
Single-step growth experiments demonstrating the accumulation of viral infective RNA in the presence or absence of WIN 52035. Wild-type or V1210A virus (MOI of 15) was mixed with HeLa cells (4 × 107 cells per ml) in PBS, in the absence of drug, and allowed to incubate at room temperature for 1 h. Duplicate V1210A-infected cell suspensions were prepared. After 1 h, each of the three cell suspensions was washed with PBS to remove unattached virus. After the wash, one of the V1210A-infected suspensions was resuspended in prewarmed medium B containing 2 μg of WIN 52035 per ml, while the other V1210A-infected suspension and the wild-type virus-infected suspension were resuspended separately in the same medium without the drug. Then the three cell suspension cultures were allowed to incubate at 35°C. Samples were taken from each suspension culture at the indicated times postinfection, and the total RNA in each sample was isolated by the guanidinium thiocyanate-phenol method. The amount of infective viral RNA in each sample was determined by transfecting HeLa cell monolayers with the respective total RNA preparation and by scoring plaques that were allowed to develop in the presence of 2 μg of WIN 52035 per ml.
Evidence that mutant V1210A requires WIN 52035 for virion assembly.
To investigate whether the absence of progeny infectivity (Fig. 3A) was due to failure to form virions by mutant V1210A in the absence of drug, the virus was propagated in HeLa cells in the presence of [35S]methionine with or without drug. Extracts from the radiolabeled cells were sedimented through 30% sucrose cushions. The pellets were then resuspended and sedimented on 7.5 to 45% sucrose gradients to display 150S virus particles (virions and provirions).
As seen in Fig. 5, mutant V1210A formed 150S particles in the presence of WIN 52035 but not in its absence. Thus, the assembly defect of drug-dependent mutant V1210A is at a step(s) prior to the formation of 150S provirions. A smaller peak sedimented in about the position expected for 80S empty shells but lacked radioactive capsid proteins when examined by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (data not shown).
FIG. 5.
Response of V1210A virion formation to WIN 52035 and WIN 56291. Virus (MOI of 15) and HeLa cells (4 × 106 cells per ml) were mixed in PBS, in the absence of drug, allowed to incubate at room temperature for 1 h, diluted 10 times (to 4 × 106 cells per ml) in prewarmed medium BL (26), divided into three aliquots, and then allowed to incubate at 35°C. PBS was used instead of virus sample in the mock infection control. At 1 h postinfection, WIN 52035 (final concentration, 2 μg/ml), WIN 56291 (final concentration, 2 μg/ml), or no drug was added to each of the three virus-infected cultures. No drug was added to the mock-infected culture. At 4 h postinfection, 170 μCi of radiolabeled [35S]methionine was added to each of the four cultures. At 7.5 h postinfection, virus was harvested from each culture by the freeze-thaw method and sedimented through a 1-ml 30% sucrose cushion in a Beckman SW41 rotor (40,000 rpm, 16°C, 135 min). Each pellet was resuspended in 300 μl of PBS (containing 0.01% BSA) and subjected to centrifugation on a 7.5 to 45% sucrose gradient in a Beckman SW41 rotor (40,000 rpm, 16°C, 100 min). Each gradient was fractionated (0.4 ml per fraction), and the radioactivity in a 50-μl sample of each fraction was determined by liquid scintillation counting.
Evidence that WIN 56291 supports assembly of mutant V1210A virions.
As shown earlier, WIN 56291 did not rescue the infectivity of mutant V1210A (Fig. 2). However, it did support assembly of 150S mutant particles (Fig. 5). That these 150S particles were infective was shown by demonstrating that they formed plaques when plated in the presence of WIN 52035. However, the specific infectivity of the particles rescued with WIN 56291 was only about 5% of that of particles rescued with WIN 52035 (data not shown). Since WIN 56291 is known to bind to HRV16 with higher affinity than WIN 52035 (37), this lower infectivity may have resulted from incomplete release of drug from virus before plating.
Virion location of drug dependence mutations.
Computer imaging of the X-ray coordinates of HRV16 showed that two of the three amino acids substituted in drug-dependent mutants V1210A and M1103T are located on the surface of the canyon that surrounds the fivefold axis of each pentameric subunit of the icosahedral shell (Fig. 6A). In addition, the two wild-type residues (V1210 and M1103) appear to make contact with residues Y3183 (Fig. 6B) and Q1161 (Fig. 6C), respectively, of neighboring subunits (protomers) within one pentamer. The third drug dependence mutation, T1208A (not shown in Fig. 6), is located near the surface of the canyon and close to the V1210A mutation.
FIG. 6.

Computer representation of HRV16 showing that two of the three drug dependence mutations are exposed on the virion surface. The protein shell contains 60 subunits (protomers) organized as 12 pentamers. (A) For clarity, only one pentamer is shown (in stereo projection). Both mutated residues are shown in red (V1210A and M1103T). The green patches in the canyon region identify the foot print for the cellular receptor ICAM-1 (36). One promoter is highlighted (gray) to show that both residues are located at a protomer-protomer interface. (B) Protomer-protomer interface showing how residue V1210 within the gray protomer contacts residue Y3183 within its neighboring protomer (yellow). (C) Stereo projection of a protomer-protomer interface showing how residue M1103 within one protomer (gray) makes contact with residue Q1161 within a neighboring protomer (yellow). In panels B and C, the surfaces of the contacting residues are depicted as meshes. (Crystallographic coordinates were provided by M. G. Rossmann. Projections were made by using the computer program GRASP.)
The drug-dependent phenotype of V1210A is independent of ICAM-1.
The position of drug dependence mutations near the canyon floor, and the observation that drug binding to the pocket affects binding of ICAM-1 to the canyon (37), raised the possibility that the assembly defect is related to defective interaction of mutant subunits or nascent provirions with ICAM-1. For example, abnormal binding of ICAM-1 to mutant subunits might prevent their assembly in the absence of drug. Alternatively, failure of mutant 150S particles to accumulate in the absence of drug might be ascribed to formation of transient provirions, which are then immediately disassembled if they bind ICAM-1.
To investigate whether ICAM-1 plays a role in assembly, murine L cells, which do not encode ICAM-1 and are not susceptible to rhinovirus infection, were transfected with samples of V1210A RNA and then incubated at 35°C for 10 h in the presence or absence of WIN 52035. Infectivity that arose from these transfected L-cell samples was measured by plaque assay on HeLa cell monolayers in the presence of WIN 52035. The results showed that the same amount of transfecting viral RNA, which produced in L cells about 50 PFU in the presence of drug, produced no plaques in its absence. Thus, the drug-dependent phenotype of V1210A is unrelated to the presence of ICAM-1 in the host cells.
However, the ability of HRV16 to multiply in L cells is notable. It has been generally assumed that L cells are unable to support rhinovirus replication because mice are known to be insusceptible to rhinovirus infection and because a different rhinovirus serotype (HRV2) was reported to be unable to multiply in these cells (46). We have preliminary data suggesting that wild-type HRV16 also replicates when transfected into L cells (not shown).
DISCUSSION
We report here the isolation and characterization of three HRV16 mutants which require, for plaque formation, a capsid-binding drug which prevents attachment of the wild-type parental virus. These mutants were initially isolated in two steps: first, mutants were selected for the ability to form plaques in the presence of WIN 52035, requiring that they overcome the attachment block. Second, these drug-resistant isolates were screened for drug-dependent mutants, i.e., those with decreased plating efficiency in the absence of drug. Such mutants should require drug either for attachment or for some other viral function.
All three drug-dependent mutants described here required drug in the late stage of their growth cycle (Fig. 3). Moreover, RNA synthesis, stability, and transfection efficiency, a rigorous measure of functional integrity, were unaffected by the absence of drug (Fig. 4). At least one of these mutants (V1210A) required drug for 150S virion formation (Fig. 5), and its mature virions retained the ability to bind drug (data not shown). We have also shown (Fig. 3) that externally added drug was not required for attachment or uncoating by any of the three mutants. However, since stocks of these drug-dependent mutants required drug for propagation, the presence of residual drug in purified mutant virions is not rigorously ruled out.
Location of drug dependence mutations is influenced by the mechanism of drug action upon wild-type virus.
Nine of 118 drug-resistant isolates proved to be drug dependent. Sequence analyses revealed that some of these nine isolates had identical mutations so that the total number of distinct mutations conferring drug dependence was reduced to three. Each of the three mutations was shown by site-directed mutagenesis of cDNA to confer the drug-dependent phenotype. All three drug-dependent mutations were located at or near the virion surface, in the same vicinity as mutations in several different families of poliovirus mutants with altered stability and cell entry (10, 15, 29, 38). These latter mutations have been thoroughly reviewed by Chow et al. (8).
The locations of drug dependence mutations in HRV16 differ markedly from those reported for drug-dependent mutants of poliovirus 3 (Fig. 7). The different locations most likely reflect the different action of capsid-binding drugs on the two viruses. In the case of poliovirus, for example, the drug interferes with uncoating, while in HRV16 it interferes with attachment to receptor. Accordingly, the location of polioviral drug dependence mutations in a region on the inner side of the capsid (36) reflects the importance of this region in uncoating, a transition involving major rearrangements in the capsid protein, finally resulting in release of genomic RNA (34).
FIG. 7.
Cutaway view of a picornavirus pentamer illustrating the location of amino acid substitutions that confer drug dependence in HRV16 and P3/Sabin. The mutations in HRV16 are on the outside the capsid, near the south wall of the canyon, and affect assembly. The mutations in poliovirus 3 map to a region on the internal side of the capsid and destabilize the virus particle (36).
The mechanism by which the parental viruses are blocked by capsid-binding drugs also influences the phenotypes of drug-dependent mutants. In the case of poliovirus, where the drug blocks uncoating, drug dependence mutations greatly reduce the uncoating transition temperature so that the mutants uncoat spontaneously, even in the absence of receptor, unless drug is present (35). The drug-dependence mutations in HRV16, on the other hand, had a small effect on its physiological uncoating behavior (data not shown). Rather, they caused a defect in virion assembly, which is probably an accidental consequence of these mutations.
Locations of drug dependence mutations are consistent with defects in virion assembly.
Computer graphic analyses of the X-ray coordinates of HRV16 (19) have shown that all three drug dependence mutations reside at or near a protomer-protomer interface (Fig. 6). Thus, it is likely that the assembly defect of these mutants is caused by abnormal protomer-protomer interaction. With this model, occupancy of drug in the binding pockets would correct a surface deformation at the mutant protomer-protomer contact, resulting in the rescue of assembly. Elsewhere (27a) we will provide evidence that one of the mutants is blocked at the step where pentamers are assembled into shells (27).
All three drug dependence mutations in HRV16 are replacements with amino acids whose side chains are smaller (Table 2). Consistent with this trend, another engineered mutant T1208G is also drug dependent, in a manner similar to that of T1208A (data not shown). This finding suggests that the presence of drug in the capsid compensates for the reduction of side chain size in each mutant.
Evidence that the drug-dependent assembly defect of HRV16 is probably not an artifact of virion instability.
It has been previously shown that the drug-dependent phenotype of poliovirus 3 Sabin strain (P3/Sabin) is linked to virion instability (35). This does not necessarily preclude the possibility that the protein subunits of this poliovirus mutant are also partially defective in assembly in the absence of drug. Indeed, the virus yield in the drug-dependent mutants of P3/Sabin are all 10-fold lower than in their wild-type parent.
That the phenotype of drug-dependent HRV16 mutants is due primarily to an assembly defect, rather than to virion instability, is suggested by the rapid appearance of infectious virus which occurred in the growth of the dependent HRV16 mutants after addition of drug (Fig. 3), making it highly likely that an assembly intermediate is synthesized in the absence of drug but is unable to assemble until drug is added. Decay in virus yield with delayed addition of drug could be explained by instability of the unassembled mutant subunits.
All three mutants were stable at physiological temperature (35°C) in the absence of added drug (data not shown). This finding supports our conclusion that the dependence mutations affect assembly, not virion stability. However, the possible presence of drug molecules retained in the capsid after propagation in drug-supplemented medium has not yet been excluded, because there is no way to produce mutants in the absence of drug. The simplest interpretation is that HRV16 virions never form in the absence of drug.
Does pocket factor play a role in assembly?
Capsid-binding drugs are inhibitory analogs of pocket factor (43). The observations that particular drugs repair the assembly defect of drug-dependent HRV16 as reported here and that they modulate uncoating of type 3 poliovirions (35) are compatible with suggestions that natural pocket factors play a role in picornavirus infection (15, 19, 23, 30, 37). While drug-dependent mutants represent tempting models for gaining further insights into the role(s) of pocket factor, studies with natural pocket factors are probably the only reliable way of accomplishing this goal.
ACKNOWLEDGMENTS
We thank Jean-Yves Sgro for invaluable assistance in computer graphics, Michael Rossmann for providing R61837 and the X-ray coordinates of HRV16, Guy Diana and Mark McKinlay for providing the WIN drugs, and Max Nibert and Ann Palmenberg for helpful discussions of this work.
This work was supported by National Institutes of Health grant AI31960 to R.R.R. and by the Lucille P. Markey charitable trust (grant 92-24).
REFERENCES
- 1.Air G M. Nucleotide sequence coding for the “signal peptide” and N terminus of the hemagglutinin from an Asian (H2N2) strain of influenza virus. Virology. 1979;97:468–472. doi: 10.1016/0042-6822(79)90358-1. [DOI] [PubMed] [Google Scholar]
- 2.Al-Nakib W, Higgins P G, Barrow G I, Tyrrell D A, Andries K, Vanden Bussche G, Taylor N, Janssen P A. Suppression of colds in human volunteers challenged with rhinovirus by a new synthetic drug ( R61837) Antimicrob Agents Chemother. 1989;33:522–525. doi: 10.1128/aac.33.4.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andries K. Anti-picornaviral agents. In: Jeffries D J, DeClercq E, editors. Antiviral chemotherapy. New York, N.Y: John Wiley & Sons; 1995. pp. 287–319. [Google Scholar]
- 4.Bush R K, Busse W, Flaherty D, Warshauer D, Dick E C, Reed C E. Effects of experimental rhinovirus 16 infection on airways and leukocyte function in normal subjects. J Allergy Clin Immunol. 1978;61:80–87. doi: 10.1016/0091-6749(78)90229-4. [DOI] [PubMed] [Google Scholar]
- 5.Busse W W, Anderson C L, Dick E C, Warshauer D. Reduced granulocyte response to isoproterenol, histamine, and prostaglandin E1 after in vitro incubation with rhinovirus 16. Am Rev Respir Dis. 1980;122:641–646. doi: 10.1164/arrd.1980.122.4.641. [DOI] [PubMed] [Google Scholar]
- 6.Calhoun W J, Swenson C A, Dick E C, Schwartz L B, Lemanske R F, Jr, Busse W W. Experimental rhinovirus 16 infection potentiates histamine release after antigen bronchoprovocation in allergic subjects. Am Rev Respir Dis. 1991;144:1267–1273. doi: 10.1164/ajrccm/144.6.1267. [DOI] [PubMed] [Google Scholar]
- 7.Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156–159. doi: 10.1006/abio.1987.9999. [DOI] [PubMed] [Google Scholar]
- 8.Chow M, Basavappa R, Hogle J M. The role of conformational transitions in poliovirus pathogenesis. In: Chiu W, Burnett R M, Garcea R L, editors. Structural biology of viruses. New York, N.Y: Oxford University Press; 1997. pp. 157–186. [Google Scholar]
- 9.Colonno R J, Condra J H, Mizutani S, Callahan P L, Davis M-E, Murcko M A. Evidence for the direct involvement of the rhinovirus canyon in receptor binding. Proc Natl Acad Sci USA. 1988;85:5449–5453. doi: 10.1073/pnas.85.15.5449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colston E, Racaniello V R. Soluble receptor-resistant poliovirus mutants identify surface and internal capsid residues that control interaction with the cell receptor. EMBO J. 1994;13:5855–5862. doi: 10.1002/j.1460-2075.1994.tb06930.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Couch R B. Rhinoviruses. In: Fields B N, Knipe D M, Chanock R M, et al., editors. Virology. 2nd ed. New York, N.Y: Raven Press; 1990. pp. 607–629. [Google Scholar]
- 12.D’Alessio D J, Peterson J A, Dick C R, Dick E C. Transmission of experimental rhinovirus colds in volunteer married couples. J Infect Dis. 1976;133:28–36. doi: 10.1093/infdis/133.1.28. [DOI] [PubMed] [Google Scholar]
- 13.Dick E C, Inhorn S L. Rhinoviruses. In: Feigin R D, Cherry J D, editors. Textbook of pediatric infection diseases. 3rd ed. Philadelphia, Pa: W. B. Saunders Co.; 1992. pp. 1507–1532. [Google Scholar]
- 14.Eggers H J. Selective inhibition of uncoating of echovirus 12 by rhodanine. Virology. 1977;78:241–252. doi: 10.1016/0042-6822(77)90095-2. [DOI] [PubMed] [Google Scholar]
- 15.Filman D J, Syed R, Chow M, Macadam A J, Minor P D, Hogle J M. Structural factors that control conformational transitions and serotype specificity in type 3 poliovirus. EMBO J. 1989;8:1567–1579. doi: 10.1002/j.1460-2075.1989.tb03541.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fox M P, Otto M J, McKinlay M A. The prevention of rhinovirus and poliovirus uncoating by WIN 51711: a new antiviral drug. Antimicrob Agents Chemother. 1986;30:110–116. doi: 10.1128/aac.30.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greve J M, Davis G, Meyer A M, Forte C P, Yost S C, Marlor C W, Kamarck M E, McClelland A. The major human rhinovirus receptor is ICAM-1. Cell. 1989;56:839–847. doi: 10.1016/0092-8674(89)90688-0. [DOI] [PubMed] [Google Scholar]
- 18.Gwaltney J M., Jr . Rhinoviruses. In: Evans A S, editor. Viral infection of humans. 3rd ed. New York, N.Y: Plenum Press; 1989. pp. 593–615. [Google Scholar]
- 19.Hadfield A T, Lee W-M, Zhao R, Oliveira M A, Minor I, Rueckert R R, Rossmann M G. The refined structure of human rhinovirus 16 at 2.15 A resolution: implications for the viral life cycle. Structure. 1997;5:427–441. doi: 10.1016/s0969-2126(97)00199-8. [DOI] [PubMed] [Google Scholar]
- 20.Heinz B A, Rueckert R R, Shepard D A, Dutko F J, McKinlay M A, Fancher M, Rossmann M G, Badger J, Smith T J. Genetic and molecular analyses of spontaneous mutants of human rhinovirus 14 that are resistant to an antiviral compound. J Virol. 1989;63:2476–2485. doi: 10.1128/jvi.63.6.2476-2485.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heinz B A, Shepard D A, Rueckert R R. Escape mutants analysis of a drug-binding site can be used to map functions in the rhinovirus capsid. In: Laver G, Air G, editors. Use of X-ray crystallography in the design of antiviral agents. New York, N.Y: Academic Press; 1990. pp. 173–186. [Google Scholar]
- 22.Hogle J M, Chow M, Filman D J. Three-dimensional structure of poliovirus at 2.9 A resolution. Science. 1985;229:1358–1365. doi: 10.1126/science.2994218. [DOI] [PubMed] [Google Scholar]
- 23.Kim S, Smith T J, Chapman M S, Rossmann M G, Pevear D C, Dutko F J, Felock P J, Diana G D, McKinlay M A. Crystal structure of human rhinovirus serotype 1A (HRV1A) J Mol Biol. 1989;210:91–111. doi: 10.1016/0022-2836(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 24.Kunkel T A, Roberts J D, Zakour R A. Rapid and efficient site-directed mutagenesis without phenotypic selection. Methods Enzymol. 1987;154:367–382. doi: 10.1016/0076-6879(87)54085-x. [DOI] [PubMed] [Google Scholar]
- 24a.Lee, W.-M. Unpublished data.
- 25.Lee W-M, Monroe S S, Rueckert R R. Role of maturation cleavage in infectivity of picornaviruses: activation of an infectosome. J Virol. 1993;67:2110–2122. doi: 10.1128/jvi.67.4.2110-2122.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee W-M, Wang W, Rueckert R R. Complete sequence of the RNA genome of human rhinovirus 16, a clinically useful common cold virus belonging to the ICAM-1 receptor group. Virus Genes. 1994;9:177–181. doi: 10.1007/BF01702661. [DOI] [PubMed] [Google Scholar]
- 27.Lee W-M, Wang W, Rueckert R R. Scientific Program & Abstracts of the American Society for Virology 15th Annual Meeting. London, Ontario, Canada: University of Western Ontario; 1996. Is pocket factor required to activate assembly of picornaviral capsids? p. 144. [Google Scholar]
- 27a.Lee, W.-M., et al. Unpublished data.
- 28.Lemanske R F, Jr, Dick E C, Swenson C A, Vrtis R F, Busse W W. Rhinovirus upper respiratory infection increases airway hyperreactivity and late asthmatic reactions. J Clin Invest. 1989;83:1–10. doi: 10.1172/JCI113843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macadam A J, Arnold C, Howlett J, John A, Marsden S, Taffs F, Reeve P, Hamada N, Wareham K, Almond J, et al. Reversion of the attenuated and temperature-sensitive phenotypes of the Sabin type 3 strain of poliovirus in vaccinees. Virology. 1989;172:408–414. doi: 10.1016/0042-6822(89)90183-9. [DOI] [PubMed] [Google Scholar]
- 30.Macadam A J, Ferguson G, Arnold C, Minor P D. An assembly defect as a result of an attenuating mutation in the capsid proteins of the poliovirus type 3 vaccine strain. J Virol. 1991;65:5225–5231. doi: 10.1128/jvi.65.10.5225-5231.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McKinlay M A, Dutko F J, Pevear D C, Woods M G, Diana G D, Rossmann M G. Rational design of antipicornavirus agents. In: Brinton M A, Heinz F X, editors. New aspects of positive-strand RNA viruses. Washington, D.C: American Society for Microbiology; 1990. pp. 366–372. [Google Scholar]
- 32.Medappa K C, McLean C, Rueckert R R. On the structure of rhinovirus 1A. Virology. 1971;44:259–270. doi: 10.1016/0042-6822(71)90258-3. [DOI] [PubMed] [Google Scholar]
- 33.Meschievitz C K, Schultz S B, Dick E C. A model for obtaining predictable natural transmission of rhinoviruses in human volunteers. J Infect Dis. 1984;150:195–201. doi: 10.1093/infdis/150.2.195. [DOI] [PubMed] [Google Scholar]
- 34.Mosser A G, Rueckert R R. Capsid-binding agents. In: Richman D D, editor. Antiviral drug resistance. Chichester, England: John Wiley & Sons Ltd.; 1996. pp. 13–40. [Google Scholar]
- 35.Mosser A G, Rueckert R R. WIN 51711-dependent mutants of poliovirus type 3: evidence that virions decay after release from cells unless drug is present. J Virol. 1993;67:1246–1254. doi: 10.1128/jvi.67.3.1246-1254.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mosser A G, Sgro J-Y, Rueckert R R. Distribution of drug resistant mutations in type 3 poliovirus identifies three regions involved in uncoating functions. J Virol. 1994;68:8193–8201. doi: 10.1128/jvi.68.12.8193-8201.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oliveira M A, Zhao R, Lee W-M, Kremer M J, Minor I, Rueckert R R, Diana G D, Pevear D C, Dukto F J, McKinlay M A, Rossmann M G. The structure of human rhinovirus 16. Structure. 1993;1:51–68. doi: 10.1016/0969-2126(93)90008-5. [DOI] [PubMed] [Google Scholar]
- 38.Racaniello V R. Early events in poliovirus infection. Virus-cell interactions. Proc Natl Acad Sci USA. 1996;93:11378–11381. doi: 10.1073/pnas.93.21.11378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rossmann M G, Arnold E, Erickson J W, Frankenberger E A, Griffith J P, Hecht H-J, Johnson J E, Kamer G, Luo M, Mosser A G, Rueckert R R, Sherry B, Vriend G. Structure of a human common cold virus and functional relationship to other picornaviruses. Nature. 1985;317:145–153. doi: 10.1038/317145a0. [DOI] [PubMed] [Google Scholar]
- 40.Rueckert R R. Picornavirus structure and multiplication. In: Fields B N, Knipe D M, Howley P M, et al., editors. Virology. 3rd ed. New York, N.Y: Raven Press, Ltd.; 1996. pp. 609–654. [Google Scholar]
- 41.Shepard D A, Heinz B A, Rueckert R R. WIN 52035-2 inhibits both attachment and eclipse of human rhinovirus 14. J Virol. 1993;67:2245–2254. doi: 10.1128/jvi.67.4.2245-2254.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sherry B, Rueckert R. Evidence for at least two dominant neutralization antigens on human rhinovirus 14. J Virol. 1985;53:137–143. doi: 10.1128/jvi.53.1.137-143.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith T J, Kremer M J, Luo M, Vriend G, Arnold E, Kamer G, Rossman M G, McKinlay M A, Diana G D, Otto M J. The site of attachment in human rhinovirus 14 for antiviral agents that inhibit uncoating. Science. 1986;233:1286–1293. doi: 10.1126/science.3018924. [DOI] [PubMed] [Google Scholar]
- 44.Smith T J, Olsen M H, Cheng R H, Chase E S, Baker T S. Structure of a human rhinovirus-bivalently bound antibody complex: implications for viral neutralization and antibody flexibility. Proc Natl Acad Sci USA. 1993;90:7015–7018. doi: 10.1073/pnas.90.15.7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Staunton D E, Merluzzi V J, Rothlein R, Barton R, Marlin S D, Springer T A. A cell adhesion molecule, ICAM-1, is the major surface receptor for rhinoviruses. Cell. 1989;56:849–853. doi: 10.1016/0092-8674(89)90689-2. [DOI] [PubMed] [Google Scholar]
- 46.Yin F H, Lomax N B. Host range mutants of human rhinovirus in which nonstructural proteins are altered. J Virol. 1983;48:410–418. doi: 10.1128/jvi.48.2.410-418.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zeichhardt H, Otto M J, McKinlay M A, Willingmann P, Habermehl K-O. Inhibition of poliovirus uncoating by disoxaril. Virology. 1987;160:281–285. doi: 10.1016/0042-6822(87)90075-4. [DOI] [PubMed] [Google Scholar]