Abstract
Introduction
There are few studies evaluating the outcomes associated with transurethral resection of the prostate (TURP) in extremely elderly men. Our objective was to assess the safety and efficacy of this procedure in this special population.
Methods
As part of an ethically approved study, retrospective review was carried out of all patients ≥ 85 years who underwent TURP between 2014 and 2023 at a tertiary centre. Data was collected on demographics including frailty status, operative data and complications. Treatment success was defined as catheter free status.
Results
Over the study period, 194 patients (median age 87 years, IQR 86–89) underwent TURP, with a median follow-up of 6 years (IQR 3.5–8). The majority (68%) were ASA 3. 28% received home nursing assistance or were nursing home residents at the time of surgery. Median CCI score was 2 (IQR 1–3). 66% used anticoagulant medication. 97% received spinal anaesthesia and median operative time was 63 min (IQR 39–88). The intra-operative complication rate was 2.6%. The 30-day complication rate was 30% (Clavien-Dindo (CD) 1–2: 24%, ≥ CD 3: 5.7%). Among those with a catheter preoperatively (62%, n = 120), 84% had achieved spontaneous voiding (n = 101) at three month follow up. Overall, 93% were still alive at 1 year post surgery. The cumulative reoperation rate during study follow up was 7.2% at 1 year, 10.9% at 3 years, and 11.5% at 5 years.
Conclusion
Treatment success for TURP in extremely elderly men (≥ 85 years) is high, but the associated morbidity burden warrants the need for an individualised approach when considering men in this special population who are potential candidates for surgery.
Keywords: BPH, Elderly, Surgery, Complications
Introduction
Benign prostatic obstruction (BPO) is a common condition in older men, frequently leading to lower urinary tract symptoms (LUTS), acute urinary retention (AUR), and, in many cases, long-term catheter dependence [1]. With global life expectancy steadily increasing, the number of men aged ≥ 85 years presenting with symptomatic BPO is rising, which arguably poses new management challenges for urologists [2–4].
Transurethral resection of the prostate (TURP) remains the reference intervention for the surgical management of BPO [5]. While efficacy and morbidity profiles are well established in the general adult population, relatively few studies have examined outcomes specifically in the “extreme elderly”, i.e. men aged ≥ 85 years. Moreover, it is often the case that studies on these methods exclude the very elderly or include them only as a small subgroup [6]. However, it is a demographic that is becoming increasingly visible in clinical practice and a conservative approach may often be preferred due to concerns about frailty, anesthetic risk, and postoperative complications. Frailty, in particular, has been associated with adverse functional outcomes following TURP [7]. However, a non-surgical approach must be weighed against the substantial morbidity and reduced quality of life associated with long-term catheterization, including reduced mobility, urinary tract infections, hematuria, and significant psychological burden [8].
In addition to LUTS and AUR, many elderly men with BPO experience recurrent macroscopic hematuria, often exacerbated by anticoagulant use [9]. Others develop recurrent bladder stones that cannot be definitively treated without addressing the underlying obstruction [10]. These factors can further contribute to patient morbidity [11].
The lack of evidence provides limited guidance to clinicians when assessing elderly patients with BPO and determining their suitability for surgery. In particular, it remains limited regarding how common preoperative characteristics—such as catheter dependency, anticoagulation use or, frailty status affect outcomes in men aged ≥ 85 [12].
The present study aims to address this knowledge gap by conducting a retrospective cohort study evaluating the safety, effectiveness, and postoperative outcomes of TURP in men aged ≥ 85 years. Specifically, we examine catheter-free rates, complication profiles, and one-year survival, and explore predictors of surgical success.
Methods
Study design, ethics and patient selection
We conducted a retrospective cohort study of male patients aged ≥ 85 years who underwent transurethral resection of the prostate (TURP) between 2014 and 2023 at a referral center for BPO surgery in Western Norway. During the study period, TURP was the only endoscopic treatment available, and minimally invasive surgical therapies (MISTs) were not in clinical use locally. The study was approved by the Regional Committee for Medical and Health Research Ethics (REK-no: 739374) and was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and its subsequent amendments. In compliance with the requirements set forth by the ethics committee, a negative (passive) informed consent process was employed: participants were informed about the study in writing and were included unless they explicitly declined participation. Data collection proceeded unless patients actively declined (n = 2) within four weeks. No external funding was obtained.
Data collection and outcome definitions
Medical records of included patients were reviewed, and variables collected included age, American Society of Anesthesiologists (ASA) physical status classification, Charlson Comorbidity Index (CCI), catheter status, use of anticoagulant or antiplatelet medication, type of anesthesia, and operative details and mortality status. In lieu of formal frailty assessments, frailty status was inferred from care dependency, defined as receipt of formal home care assistance or nursing home residency. The primary outcome of interest was postoperative complications within 30 days, classified according to the Clavien–Dindo (CD) system. A secondary outcome was treatment success, defined as catheter-free status at 3-month follow-up.
Pre-operative assessments
Standard pre-operative assessments included physical examination, uroflowmetry, and cystoscopy. In those with a history of bladder outlet obstruction surgery, cystoscopy confirmed recurrent obstruction. Prostate volume was most commonly assessed by transrectal ultrasound; however, alternative imaging modalities, such as magnetic resonance imaging, were also used when available. Urodynamic studies were not routinely performed.
Surgical technique and catheter care
All procedures were performed using a standardized bipolar resection technique with the TURis system (Olympus Medical Systems, Tokyo, Japan), in accordance with institutional protocols. Operations were carried out either by experienced urologists specializing in endoscopic management of BPO or by residents under direct supervision. Catheters placed intraoperatively were removed before hospital discharge.
Perioperative antithrombotic management
Perioperative antithrombotic management followed national recommendations [13]. Direct oral anticoagulants were withheld for 2 days, clopidogrel/ticagrelor for 5 days, and warfarin until INR < 1.6. Aspirin was discontinued only when used for primary prophylaxis. Bridging was considered in high-risk cases after consultation with a hematologist and/or cardiologist. Antithrombotic agents were restarted once the surgeon deemed the urine sufficiently clear.
Statistical analysis
Logistic regression analyses were performed to identify predictors of complications and treatment failure for patients that were catheter dependent pre-operatively. Kaplan–Meier survival curves were generated to compare mortality against estimated data for men with same age from Norwegian reference population [14]. All statistical analyses were conducted using R (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
We included 194 TURP procedures performed in patients aged ≥ 85 years with a median follow up of 6 years (IQR 3.5–8). The preoperative and intraoperative characteristics are summarized in Table 1. The median age was 87 years (IQR 86–89). Most patients were classified as ASA III (68%, n = 131), and the median CCI score was 2 (IQR 1–3). A total of 28% (n = 55) received formal care assistance at home care or were nursing home residents. Anticoagulant or antiplatelet therapy was used by 66% (n = 128). Preoperative catheterization was present in 62% (n = 120). Baseline prostate volume was available for 144 patients (74%), with a median of 58 mL (IQR 35–90).
Table 1.
Summary of demographics
| Total number of patients | 194 |
|---|---|
| Total number of TURP procedures | 194 |
| Median age (IQR) | 87 years (86—89) |
| ASA grade | |
| 1 | 1 (0.5%) |
| 2 | 54 (28%) |
| 3 | 131 (68%) |
| 4 | 8 (4.1%) |
| Median pre-operative hemaglobin (IQR) |
13.5 g/dL (IQR 12.4–14-4) |
| Median CCI (IQR) | 2 (1–3) |
| Living status: | |
| Lives at home without public assistance | 139 (72%) |
| Lives at home with home nursing care | 51 (26%) |
| Nursing home residence | 4 (2.1%) |
| Catheter status | |
| None | 74 (38%) |
| Indwelling catheter | 63 (33%) |
| Clean intermittent catheterization | 50 (26%) |
| Suprapubic catheter | 7 (3.6%) |
| Anticoagulant/platelet inhibitor use | 128 (66%) |
| Previous BPO surgery | 44 (23%) |
| Previous bladder stone surgery | 7 (3.6%) |
| Median preoperative PSA (IQR) | 5.2 (2.0–10.4) |
| Median prostate volume (IQR) (n = 144) | 58 ml (35–90) |
| Preoperative urine culture (n = 173): | |
| No growth | 104 (60%) |
| Growth in urine culture | 69 (40%) |
TURP = transurethral resection of the prostate
IQR = interquartile range
ASA = American Society of Anesthesiologists
CCI = Charlson Comorbidity Index
BPO = benign prostatic obstruction
LUTS = lower urinary tract symptoms
UTI = urinary tract infection
PSA = prostate specific antigen
Among patients without a catheter prior to TURP (n = 74), the main indications for surgery were persistent LUTS (n = 62, 84%), recurrent urinary tract infection (n = 10, 14%), and hematuria (n = 2, 3%). In the overall cohort (n = 194), 131 patients (67.5%) received some form of medical therapy prior to surgery, while 63 patients (32.5%) had not received any. The most common regimen was combination therapy with an α-blocker and 5-ARI (n = 98, 50.5%), followed by α-blocker monotherapy (n = 19, 9.8%) and 5-alpha reductase inhibitor monotherapy (n = 14, 7.2%).
Intraoperative and perioperative data
Spinal anesthesia was used in 97% of procedures (Table 2). The median operative time was 63 min (IQR 39–88), and the median resected tissue weight was 26 g (IQR 13–45). Intraoperative complications occurred in 2.6% and consisted of bleeding from the prostate (1%), bleeding related to suprapubic drainage (0.5%), angina pectoris (0.5%), and inadvertent resection of the ureteral orifice (0.5%). The transfusion rate was 5.7%. The median decrease in hemoglobin on postoperative day 1 was 1.1 g/dL (IQR 0.6–1.7). The median hospital stay was 1 day (IQR 1–2).
Table 2.
Operative data
| Anesthesia type | |
|---|---|
| General anesthesia | 6 (3.1%) |
| Spinal | 188 (97%) |
| Median operative time (minutes) (IQR) | 63 (39—88) |
| Median resected weight (gram) (IQR) | 26 (13—45) |
| Operator experience | |
| Consultant urologist | 116 (60%) |
| Resident | 78 (40%) |
| Median hospital stay (days) (IQR) | 1 (1—2) |
| Median change in hemoglobin (g/dL) (IQR) | 1.1 (0.6 – 1.7) |
IQR = interquartile range
Complications
Postoperative complications within 30 days occurred in 30% (Table 3). Most were CD 1–2 (24%) while CD ≥ 3 complications occurred in 5.7%. One mortality was recorded and consisted of in hospital cardiac arrest at 24 h postoperatively. There was one death, which resulted from an in-hospital cardiac arrest 24 h postoperatively.
Table 3.
Summary of complications
| Early postoperative complications within 30 days | Management | CD | |
|---|---|---|---|
| Urinary retention | Catheter | II | 10 (5.2%) |
| Urinary tract infection | Oral antibiotics | II | 15 (7.7%) |
| Urinary sepsis | IV antibiotics + vasopressors | IV | 1 (0.5%) |
| Hematuria | Irrigation catheter ± transfusion | II | 14 (7.2%) |
| Hematuria | Cystoscopic clot evacuation (sedation/local) | IIIa | 3 (1.5%) |
| Hematuria | Cystoscopic clot evacuation (spinal anesthesia) | IIIb | 1 (0.5%) |
| Non–ST–Elevation myocardial infarction* | LMWH + DAPT | II | 1 (0.5%) |
| Non–ST–Elevation myocardial infarction* | LMWH + DAPT + chest tube (local) | IIIa | 1 (0.5%) |
| Atrioventricular block | Observation + beta-blocker withdrawal | I | 1 (0.5%) |
| Atrioventricular block | Pacemaker (local) | IIIa | 1 (0.5%) |
| ST–Elevation myocardial infarction* | PCI (local) | IIIa | 1 (0.5%) |
| Transient ischemic attack | DAPT (dipyridamole + ASA/clopidogrel) | II | 2 (1.0%) |
| Concussion after fall | Observation + wound suturing (local) | IIIa | 1 (0.5%) |
| Acute psychiatric episode | Psychiatric pharmacotherapy | II | 1 (0.5%) |
| Cerebral infarction * | Thrombolysis | II | 1 (0.5%) |
| Acute renal failure | IV fluid therapy | II | 2 (1.0%) |
| Bleeding gastric ulcer | Endoscopic hemostasis + transfusion | IIIa | 1 (0.5%) |
| Death (cardiac arrest) | – | V | 1 (0.5%) |
| Complication rate | |||
| CD I-II | 47 (24%) | ||
| CD ≥ III | 11 (5.7%) | ||
| Overall | 58 (30%) |
*Note that these cases did not require ICU admission
CD = Clavien–Dindo
IV = Intravenous
LMWH = Low molecular weight heparin
DAPT = Dual antiplatelet therapy
PCI = Percutaneous coronary intervention
ASA = Acetylsalicylic acid
On logistic regression no significant predictors were identified for postoperative complications. On logistic regression, no significant predictors of postoperative complications were identified. Variables tested included age, ASA score, operative time, resection weight, and preoperative catheter status.
Functional outcomes
At 3-month follow-up, 90% (n = 173) of patients were catheter-free; none required reoperation within this period to achieve catheter-free status. Among patients with an indwelling catheter preoperatively (62%, n = 120), 84% (n = 101) achieved spontaneous voiding. In this subgroup, lower resection weight was the only significant predictor of treatment failure (OR 0.94, 95% CI 0.90–0.99, p = 0.01), whereas age, ASA score, and operative time were not significant predictors. Paired comparisons among patients without a preoperative catheter (n = 74) demonstrated significant improvements following TURP. Qmax increased from a preoperative median of 8 ml/s (IQR 6–11) to a postoperative median of 14 ml/s (IQR 10–21) (p < 0.001). Similarly, PVR was significantly reduced, from a preoperative median of 90 ml (IQR 40–138) to a postoperative median of 22 ml (IQR 0–67) (p < 0.001, Wilcoxon signed-rank test).
Among men who were catheter free, the reported urinary incontinence rate was 6.9% (n = 12).
Long-term outcomes
The median overall time to reoperation was 8.8 months (IQR 5.8–19.8). The cumulative reoperation rate during study follow-up was 7.2% at 1 year, 10.9% at 3 years, and 11.5% at 5 years (Fig. 1, Table 4). Reoperations consisted of re-TURP (4.1%, n = 8), bladder neck incision (5.7%, n = 11), cystolitholopaxy (1.0%, n = 2), and internal urethrotomy (0.5%, n = 1). One-year survival was 93%. This was not worse than the expected survival for men of the same age in the general Norwegian population (Fig. 2).
Fig. 1.

Cumulative rate of reoperation
Table 4.
Follow up data
| Catheter status | |
|---|---|
| Catheter free | 173 (90%) |
| Indwelling catheter | 8 (4.2%) |
| Clean intermittent catheterization | 12 (6.2%) |
| Histology | |
| Benign | 129 (67%) |
| Malignant | 63 (33%) |
| Mortality status: | |
| Death within 30 days | 1 (0.5%) |
| Death within 1 year | 13 (6.7%) |
| Elective surgical retreatment during study follow up | 22 (11%) |
Fig. 2.
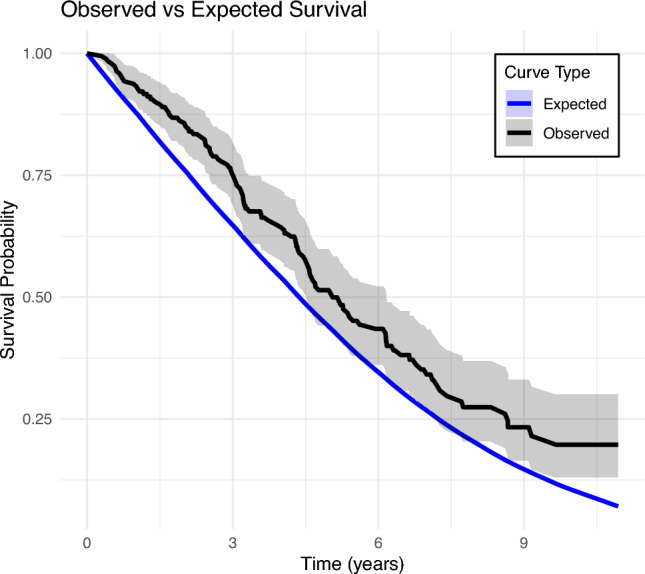
Overall survival of study sample compared to expected survival for Norwegian reference population
Discussion
This study confirms that TURP is an effective treatment option for bladder outlet obstruction in the extremely elderly. Catheter-free status was achieved in the vast majority of patients, and the rate of major complications (Clavien–Dindo ≥ 3) was low. Overall, these results support the premise that chronological age alone should not preclude patients from BPO surgery. These findings are consistent with a multicenter study by Lotterstätter et al., who similarly found TURP to be effective in selected patients aged ≥ 85 years [15]. In their study, the authors only identified polypharmacy to be a risk factor for failure to void spontaneously.
These favorable outcomes are consistent with those reported in a recent Holmium Laser Enucleation of the Prostate (HoLEP) series from Klein et al. [16]. Similarly, in a multicenter study by Priola et al., which included 731 patients with a median age of 82 years undergoing endoscopic enucleation, the major complication rate was low at 2.2% [17]. In addition, in a large study of 981 patients stratified by age 75 years and above versus below 75 years, Giulioni et al., found that functional outcomes were comparable at 1 year follow-up [18]. Photoselective Vaporization of the Prostate (PVP) is also a potential alternative and could offer advantages proposed for patients on anticoagulation or with an elevated anesthetic risk [19]. In a study by Macdonald et al., 57 octogenarians underwent PVP, with 91% classified as ASA III and 7% as ASA IV [20]. The overall complication rate was 10.5% and 93% were catheter free at one year follow up.
The rate of cumulative reoperations plateaued after 3 years. This could be interpreted in several ways. It could infer that most reoperations are necessitated early on and/or that if a patient reaches this time point, their outcomes are durable. Alternatively, the rate could artificially flatten beyond this time period as patients may become too frail to be considered eligible for repeat surgery and a conservative method is adopted accordingly. It is also noteworthy that the one-year survival in our cohort was 93%, similar to a matched age group based on national demographic data [21]. This most likely reflects selection bias and is a common finding in such studies in elderly populations. Outcome data including survival data on those who were denied surgery based on a high-risk profile would be valuable. Nonetheless, our findings support offering definitive treatment to appropriately selected patients in this age group. It also supports avoiding rigid age-based criteria in favor of a more nuanced, holistic assessment of the patient. Ideally, this should involve a multidisciplinary approach, incorporating surgical, anesthesiological, and geriatric evaluation, with the aim of minimizing intra-, peri-, and postoperative complications. While ASA and CCI scores are helpful, the integration of established geriatric tools—such as gait speed, cognitive status, and polypharmacy burden can further refine surgical risk stratification [22, 23].
MISTs are also a therapeutic alternative although data in the ≥ 85 age group are more limited. Furthermore, access to newer surgical modalities remains limited in smaller nations such as Norway. According to national registry data, in 2023 TURP constituted over 90% of BPO procedures performed, laser enucleation accounted for 1.1%, and the remainder were simple prostatectomies conducted via either open or robotic approaches [24]. MISTs only became available in Western Norway after the conclusion of the study period. Accordingly, the findings presented here reflect outcomes from a context in which TURP was the sole endoscopic treatment option.
MISTs that have been developed for the treatment of BPO include transperineal laser ablation (TPLA), iTind, Rezūm, and urolift [25–28]. Many of these such as TPLA can also be performed under local anaesthesia [29]. Destefanis et al., reported outcomes of TPLA in high-risk surgical patients, demonstrating significant improvements in both prostate volume reduction and IPSS scores [30]. Data on MIST outcomes in catheter-dependent cohorts and in the very elderly remain limited, and available studies suggest lower rates of achieving catheter-free status in patients with a long-term catheter patients [31, 32].
The overall reoperation rate of 11% in our cohort is higher than the pooled 5 year retreatment rate of 7.7% reported by He et al. in their systematic review of TURP outcomes, although still lower than the corresponding rate reported for prostate artery embolization (23.8%) [33]. This discrepancy could reflect differences in patient selection, follow-up duration, or reoperation definitions across studies. This could include for example if the definition for reoperation only refers to repeat TURP. Surgeons may also adopt a more conservative approach in higher-risk patients, performing more limited resections and thereby increasing the likelihood of recurrent obstruction. Furthermore, factors common in this age group, such as prolonged preoperative catheterisation, comorbidities like diabetes, and reduced vascular supply, may predispose to fibrosis and the development of complications such as bladder neck contracture.
Similar to the study by Macdonald et al., a small proportion of patients in our cohort (n = 8, 4.1%) had a high comorbidity burden (ASA IV) [20]. Although such patients carry significant perioperative risk, they were cognitively intact, expressed strong wishes to be free of a catheter, and were carefully counselled before surgery. For these individuals, the potential benefits included avoidance of chronic catheter-related complications, preservation of independence, and the possibility of improving quality of life despite limited life expectancy [34, 35].
Strengths and limitations
This study is limited by its retrospective, single-center design and lack of baseline prostate volume in all patients. While catheter-free status is a pragmatic endpoint, subjective outcomes such as IPSS were not available. As such, reliable conclusions cannot be drawn regarding the impact of TURP on patients’ quality of life, sexual function or broader patient related outcomes. The cohort consisted only of patients deemed fit for surgery, which may introduce selection bias. This likely contributed to the high one-year survival rate. Accordingly, the findings may not be fully generalizable to the broader population of very elderly men with LUTS or urinary retention. Frailty was not formally assessed using a standardized instrument, which limits the precision of frailty assessment. Use of validated tools such as the Clinical Frailty Scale (CFS) or G-8 Geriatric Screening Tool would have provided a more robust evaluation of frailty, which represents a multidimensional and complex phenotype [36, 37].
Despite these limitations, the study provides real-world reference data in a growing demographic for which evidence remains scarce. Future studies should prospectively validate frailty-based risk models, and the development of a dedicated clinical decision tool could aid preoperative counseling in this special population. This could be complemented by qualitative research exploring to what extent relief from catheter dependence may improve quality of life, particularly when patients weigh this potential benefit against the risks of surgery. Comparative trials between TURP and alternative surgical approaches in men ≥ 85 years are warranted, and parallel health-economic analyses may clarify the cost-effectiveness of TURP compared with long-term catheterization.
Conclusion
TURP in men aged ≥ 85 years is effective, including in catheter-dependent patients, and is associated with a low rate of serious adverse events. Chronological age alone should not be regarded as a contraindication; rather, surgical decisions should be made in the context of an individual patient’s comorbidity profile and functional status.
Author contributions
PJJ conceived the project. All authors planned the project and methodology. SB collected data. SB, PJJ, CB and CAM performed analysis. All authors contributed to manuscript writing, reviewed it and approved the final version.
Funding
Open access funding provided by University of Bergen (incl Haukeland University Hospital). Not applicable.
Data availability
. Available upon reasonable request to the corresponding author.
Declarations
Conflicts of interest
PJJ has received funding from the Norwegian Institute of Urology to research surgical outcomes in the elderly population.
Human ethics and consent to participate
The study was approved by the Regional Committee for Medical and Health Research Ethics (REK-no: 739374), and was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and its subsequent amendments. In compliance with the requirements set forth by the ethics committee, a negative (passive) informed consent process was employed: participants were informed about the study in writing and were included unless they explicitly declined participation.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gravas S, Cornu JN, Gacci M (2023) EAU guidelines on the management of non-neurogenic male lower urinary tract symptoms. Eur Urol 84(2):207–222 [DOI] [PubMed] [Google Scholar]
- 2.Ye Z, Wang J, Xiao Y, Luo J, Xu L, Chen Z (2024) Global burden of benign prostatic hyperplasia in males aged 60–90 years from 1990 to 2019: results from the global burden of disease study 2019. BMC Urol 24(1):193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steel N, Bauer-Staeb CMM, Ford JA, Abbafati C, Abdalla MA, Abdelkader A et al (2025) Changing life expectancy in European countries 1990–2021: a subanalysis of causes and risk factors from the Global Burden of Disease Study 2021. Lancet Public Health 10(3):e172–e188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collaborators GBDF (2024) Burden of disease scenarios for 204 countries and territories, 2022–2050: a forecasting analysis for the Global Burden of Disease Study 2021. Lancet 403(10440):2204–2256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agrawal MS, Mishra DK (2022) Transurethral resection of prostate. J Endourol 36(S2):S-29-S−34 [DOI] [PubMed] [Google Scholar]
- 6.Juliebo-Jones P, Baug S, Tzelves L, Beisland C (2025) Ageing patients, missing evidence: the need for more research in the elderly. World J Urol 43(1):303 [DOI] [PubMed] [Google Scholar]
- 7.Ren X, Wang J, Wang Z, Yin Y, Li X, Tian Y et al (2023) Frailty as a risk marker of adverse lower urinary symptom outcomes in patients with benign prostatic hyperplasia undergoing transurethral resection of prostate. Front Med 10:1185539 [Google Scholar]
- 8.Wiedemann A, Gedding C, Heese M, Stein J, Manseck A, Kirschner-Hermanns R (2022) Quality of life for wearers of a suprapubic or transurethral bladder catheter as lifelong permanent care. Urologe A 61(1):18–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elmansy H, Hodhod A, Fathy M, Violette PD, Elshafei A, Zakaria AS et al (2023) Emergency holmium laser enucleation of the prostate (HoLEP): a novel approach in the management of refractory hematuria for patients with benign prostatic hyperplasia (BPH): a single-institution experience. World J Urol 41(3):805–811 [DOI] [PubMed] [Google Scholar]
- 10.Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al (2023) EAU Guidelines on Urolithiasis
- 11.Maresca G, Mc Clinton S, Swami S, El-Mokadem I, Donaldson JF (2022) Do men with bladder stones benefit from treatment of benign prostatic obstruction? BJU Int 130(5):619–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lotterstätter M, Seklehner S, Wimpissinger F (2022) Transurethral resection of the prostate in 85+ patients: a retrospective, multicentre study. World J Urol 40:3015–3020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SVELIC O, Om L, RELIS O. Seponering av platehemmere og antikoagulantia før kirurgi.
- 14.Statistics OfN. Mortality Statistics (2023) [Available from: https://www.nomisweb.co.uk.
- 16.Klein C, Anract J, Pinar U (2025) Comparative study of HoLEP in elderly patients with indwelling catheters: a retrospective dual-center study. World J Urol 43:75 [DOI] [PubMed] [Google Scholar]
- 17.Pirola GM, Castellani D, Naselli A, Fong KY, Biligere S, Dellabella M et al (2025) Endoscopic enucleation of the prostate in men aged 80 years and older. Outcomes from a global, large, and multicenter series using different energy sources and techniques. World J Urol 43(1):344 [DOI] [PubMed] [Google Scholar]
- 18.Giulioni C, Talle M, Papaveri A, Mengoni F, Orciani R, Pandolfo SD et al (2025) The implementation of trifecta score to assess the quality of holmium laser enucleation of the prostate in elderly patients: an analysis of perioperative and functional outcomes and the impact of age. J Clin Med. 10.3390/jcm14103410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruszat R, Wyler S, Forster T, Reich O, Stief CG, Gasser TC et al (2007) Safety and effectiveness of photoselective vaporization of the prostate (PVP) in patients on ongoing oral anticoagulation. Eur Urol 51(4):1031–1038 (discussion 8-41) [DOI] [PubMed] [Google Scholar]
- 20.MacDonald A, Fathy M, Nikoufar P, Hodhod A, Hadi RA, Vangala SK et al (2023) Safety and clinical outcomes of GreenLight laser prostatectomy in octogenarians. Can Urol Assoc J 18(3):E65 [Google Scholar]
- 21.Statistics N. Life expectancy – remaining years for males and females at selected ages. Statbank Table 05375. 2025.
- 22.Aceto P, Bassi P, Sollazzi L, Racioppi M, Fortunato G, Di Gianfrancesco L et al (2021) Implementation of frailty preoperative assessment to predict outcome in patients undergoing urological surgery: a systematic review and meta-analysis. BJU Int. 10.1111/bju.15314 [DOI] [PubMed] [Google Scholar]
- 23.Yajima S, Masuda H (2024) The significance of G8 and other geriatric assessments in urologic cancer management: a comprehensive review. Int J Urol 31(6):607–615 [DOI] [PubMed] [Google Scholar]
- 24.Juliebo-Jones P, Roth I, Moen CA, Gjengsto P, Beisland C (2025) National trends in medication prescriptions for male lower urinary tract symptoms and erectile dysfunction: findings from the Norwegian prescription database. Eur Urol Open Sci 75:89–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones P, Siena G, Hameed BZ, Somani BK (2021) Emerging data on the safety and efficacy of transurethral water vapour therapy for benign prostatic hyperplasia. Res Rep Urol. 10.2147/RRU.S273686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ray A, Morgan H, Wilkes A, Carter K, Carolan-Rees G (2016) The urolift system for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: a NICE medical technology guidance. Appl Health Econ Health Policy 14(5):515–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tzelves L, Nagasubramanian S, Pinitas A, Juliebø-Jones P, Madaan S, Sienna G et al (2023) Transperineal laser ablation as a new minimally invasive surgical therapy for benign prostatic hyperplasia: a systematic review of existing literature. Ther Adv Urol 15:17562872231198634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Godard L, Trivedi H, Narang G, Forbes CM (2025) Device profile of the iTind temporary implantable nitinol device for benign prostatic hyperplasia. Expert Review of Medical Devices (just-accepted)
- 29.Polverino P, Lo Re M, Saladino M, Pecoraro A, Moscardi L, Rivetti A et al (2024) Could transperineal interstitial laser ablation of the prostate be the right option for highly-comorbid patients with lower urinary tract symptoms due to benign prostatic obstruction? A preliminary single-center experience focusing on functional and safety outcomes. Minerva Urol Nefrol 76(5):646–649 [Google Scholar]
- 30.Destefanis P, Sibona M, Vitiello F, Vercelli E, Micai L, Montefusco G et al (2024) Trans - perineal laser ablation of the prostate in high surgical risk patients affected by severe lower urinary tract symptoms related to benign prostatic obstruction. Prostate Cancer Prostatic Dis 27(4):693–699 [DOI] [PubMed] [Google Scholar]
- 31.Sandhu JS, Bixler BR, Dahm P, Goueli R, Kirkby E, Stoffel JT et al (2024) Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia (BPH): AUA guideline amendment 2023. J Urol 211(1):11–19 [DOI] [PubMed] [Google Scholar]
- 32.Alcina EL, Arjona MF, Guzman EF, Zuazu JR, Jochamowitz IS (2025) Expert consensus on Rezum: indications, surgical technique and postoperative care. BJUI Compass 6(2):e491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.He W, Ding T, Niu Z, Hao C, Li C, Xu Z et al (2023) Reoperation after surgical treatment for benign prostatic hyperplasia: a systematic review. Front Endocrinol (Lausanne) 14:1287212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Godfrey H (2008) Living with a long-term urinary catheter: older people’s experiences. J Adv Nurs 62(2):180–190 [DOI] [PubMed] [Google Scholar]
- 35.Murphy C, Cowan A, Moore K, Fader M (2018) Managing long term indwelling urinary catheters. BMJ 363:k3711 [DOI] [PubMed] [Google Scholar]
- 36.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bellera CA, Rainfray M, Mathoulin-Pelissier S, Mertens C, Delva F, Fonck M et al (2012) Screening older cancer patients: first evaluation of the G-8 geriatric screening tool. Ann Oncol 23(8):2166–2172 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
. Available upon reasonable request to the corresponding author.


