Abstract
Objectives To assess the efficacy and cost effectiveness of a home safety programme and a home exercise programme to reduce falls and injuries in older people with low vision.
Design Randomised controlled trial.
Setting Dunedin and Auckland, New Zealand.
Participants 391 women and men aged ≥75 with visual acuity of 6/24 or worse who were living in the community; 92% (361 of 391) completed one year of follow-up.
Interventions Participants received a home safety assessment and modification programme delivered by an occupational therapist (n = 100), an exercise programme prescribed at home by a physiotherapist plus vitamin D supplementation (n = 97), both interventions (n = 98), or social visits (n = 96).
Main outcome measures Numbers of falls and injuries resulting from falls, costs of implementing the home safety programme.
Results Fewer falls occurred in the group randomised to the home safety programme but not in the exercise programme (incidence rate ratios 0.59 (95% confidence interval 0.42 to 0.83) and 1.15 (0.82 to 1.61), respectively). However, within the exercise programme, stricter adherence was associated with fewer falls (P = 0.001). A conservative analysis showed neither intervention was effective in reducing injuries from falls. Delivering the home safety programme cost $NZ650 (£234, 344 euros, $US432) (at 2004 prices) per fall prevented.
Conclusion The home safety programme reduced falls and was more cost effective than an exercise programme in this group of elderly people with poor vision. The Otago exercise programme with vitamin D supplementation was not effective in reducing falls or injuries in this group, possibly due to low levels of adherence.
Trial registration number ISRCTN15342873.
Introduction
Multiple factors contribute to most falls in older people.1,2 The first successful community trial, the landmark study by Tinetti and colleagues,3 and subsequent studies in specific populations, such as those presenting to an emergency department,4 have shown that multiple interventions can prevent falls. Many guide-lines now recommend such strategies.5-7
The problem with this approach is that not all components of multiple intervention programmes are effective.8 Also intervention programmes are not effective in certain population groups, such as those with dementia.9 Importantly, in selected populations, trials using single interventions such as strength and balance retraining10 and withdrawal of psychotropic drugs11 have been as successful as those using multiple interventions. As multiple intervention strategies in unselected older populations are not necessarily the best use of public money, the next research task has been to identify which interventions are most effective, and most cost effective, in selected populations.
People with visual impairment fall more frequently than those with normal sight.12 They may fail to see or over correct in stepping over environmental hazards and may have difficulty taking corrective action after a stumble. They may exercise less with consequent loss of strength and balance and may venture outside less, resulting in low vitamin D concentrations. We carried out a randomised controlled trial to investigate the effectiveness of two home based strategies to prevent falls in elderly people with impaired vision—a programme to address safety in the home environment and a programme of strength and balance retraining plus vitamin D supplements.
Methods
Participant recruitment
We used records from the Royal New Zealand Foundation of the Blind register (in Dunedin and Auckland), the University of Auckland optometry clinic, Dunedin and Auckland hospital low vision outpatient clinics, and a private ophthalmology practice to identify potential participants aged ≥75 years with poor vision who were living in the community. Poor vision was defined as visual acuity of 6/24 or worse in the better eye after the best possible correction. Foundation or clinic staff invited people who met the criteria to participate. We excluded those who could not walk around their own residence, who were receiving physiotherapy at the time of recruitment, or could not understand the trial requirements. Recruitment took place over a 12 month period beginning in October 2002.
Trial design
We used a 2×2 factorial design and one year of follow-up. To calculate the sample size we used the rate of falls in those aged ≥75 in the control groups in our four previous trials of the exercise programme and the 35% reduction in falls achieved,10 a power of 0.80, and a two sided significance of 0.05; we allowed for the Poisson type distribution of falls and a 20% dropout rate.
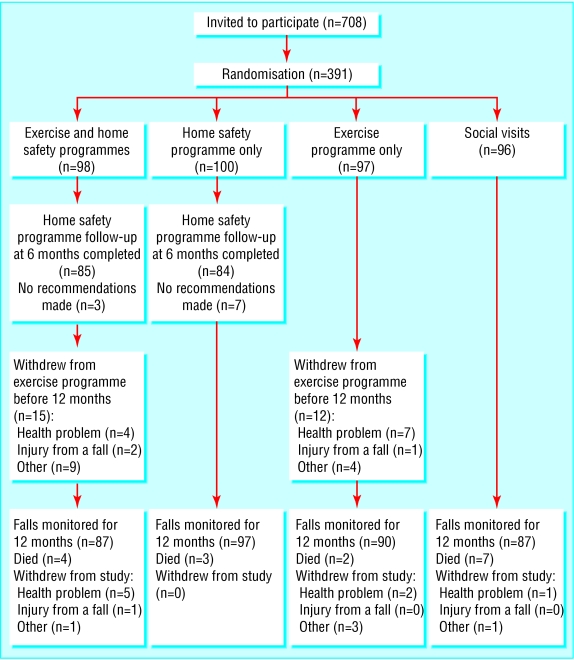
After we obtained written informed consent and an independent assessor completed baseline assessments (demographic, health, physical, and visual function) at the participant's home, we randomised 391 participants: 100 to the home safety assessment and modification programme, 97 to the exercise programme, 98 to both interventions, and 96 to social visits (see figure). A statistician developed the group allocation schedule using computer generated random numbers. The schedule was held by an independent person at a separate site and was accessed by a research administrator for the study, who telephoned after each baseline assessment was completed. The administrator then informed the occupational therapist, physiotherapist, or social visitor, who delivered the assigned intervention to that participant where possible within the next two weeks.
Figure 1.
Flow of participants through the trial
Interventions
The two occupational therapists and three physiotherapists delivering the interventions and the two independent assessors attended a two day training course.
Home safety programme
The home safety assessment and modification programme was specifically designed for people with severe visual impairments. The occupational therapist (one in each centre) visited the person at home and used a modified version of the Westmead home safety assessment checklist to identify hazards and to initiate discussion with the participant about any items, behaviour, or lack of equipment that could lead to falls.13 The therapist and participant agreed on which recommendations to implement. The occupational therapist listed these recommendations in a follow-up letter to the participant. She facilitated provision of equipment and payment from various usual sources depending on the price and type of the home modification. Referrals were made to the Royal New Zealand Foundation of the Blind as appropriate. A second home visit was needed to sign off the equipment installed by some providers.
The occupational therapist evaluated adherence to the home safety programme during a telephone interview six months after study entry. The participant reported whether each recommendation for home modifications and behaviour change had been acted on, partially acted on, or not carried out.
Exercise programme
The one year exercise intervention consisted of the Otago exercise programme (specific muscle strengthening and balance retraining exercises that progress in difficulty and a walking plan),14 modified for those with severe visual acuity loss, with vitamin D supplementation. The physiotherapist individually prescribed the exercises during five home visits at weeks one, two, four, and eight and a booster visit after six months. The degree of difficulty of the exercise and the number of 1, 2, and 3 kg ankle cuff weights used for muscle strengthening were increased at each visit as appropriate. Audiotapes of the exercises in four different levels of difficulty were available for those who could not see the exercise instruction sheets. Participants were expected to exercise at least three times a week (about 30 minutes a session) and to walk, if walking outside could be done safely, at least twice a week for a year. The physiotherapist delivered vitamin D tablets (two 1.25 mg calciferol tablets initially and then one monthly for one year) to those not already taking this supplement. For the months with no scheduled home visit the physiotherapist telephoned to encourage the person to maintain motivation and discuss any problems.
Adherence to the exercise programme was monitored for a year with monthly postcard calendars similar to those used to monitor falls. Peer group review of the physiotherapists was carried out twice each year to ensure quality control.
Social visits
Research staff made two home visits lasting an hour each during the first six months of the trial to participants who were not randomised to either the exercise or home safety programmes.
Measurement of vision
We measured distance high contrast and low contrast (10%) visual acuity using logMAR letter charts adapted from the Snellen criteria and designed to be used from 1-4 metres, a broad measure of peripheral field loss in four quadrants, and contrast sensitivity using the Melbourne edge test at 25 cm distance.15 Standard lighting was used and each eye was tested separately with participants given a free choice about wearing spectacles.
Falls and injuries
Falls were defined as “unintentionally coming to rest on the ground, floor, or other lower level.”16 Falls were monitored for one year for each person with participants using prepaid, addressed, tear-off monthly postcard calendars. The independent assessor in each centre telephoned participants to record the circumstances of the falls and any resulting injuries or use of resources. They remained blind to group allocation.
Fall events were classified as resulting in serious injury if the fall resulted in a fracture or admission to hospital with an injury or if stitches were required; “moderate” injury if bruising, sprains, cuts, abrasions, or reduction in physical function for at least three days resulted, or if the participant sought medical help; and no injury. The circumstances of serious injuries were confirmed from hospital and general practice records. The investigator classifying fall events remained blind to group allocation.
Economic evaluation
We used cost effectiveness analysis to enable comparisons of efficiency among different interventions to prevent falls. We planned to determine the cost effectiveness of each of the two programmes if it proved to be effective in reducing falls in this trial. Costs were considered from the societal perspective because of the broad nature of the problems caused by falls and were reported in New Zealand dollars at 2004 prices exclusive of government goods and services tax. We used the control participants (those not receiving the particular intervention) as the comparator. Cost effectiveness was measured as the incremental cost of delivering the programme per fall event prevented by the programme during the one year trial. One way sensitivity analyses were performed.
Costs of the home safety programme
We focused on the costs of implementing the home safety programme. Although there were costs associated with developing the programme, these were incurred before the trial and were not incremental to this programme. We did not include the research costs of evaluating the programme.
Programme implementation costs were obtained from trial records, from the participants, and from the financial records of the research group and other equipment funders, with actual costs when available. We did not include the costs of recruiting the occupational therapists because existing staff in an organisation may deliver the programme. We did not put a value on the time the participants spent with the occupational therapist or organising any home modifications; the opportunity cost in these cases was taken to be zero. We estimated overhead costs as 21.85% of observed resource use, the sector average reported for all hospital and health services in New Zealand for operating costs and overhead expenses.17 This was consistent with our previous cost effectiveness analyses.18,19
Calculation of cost effectiveness ratios
We measured cost effectiveness as the ratio ΔC:ΔE, where ΔC (incremental cost) was the change in resource use resulting from the home safety programme.20 This was taken as the total cost of implementing the programme in the home safety groups; the change in resource use for the control participants was conservatively valued at zero. We planned to include estimates for the costs of injuries as a result of falls in ΔC only if the number of injuries proved to be significantly different between the groups being compared.
We measured ΔE (incremental effect) as the difference between the number of falls in the control and home safety groups. We used the actual number of falls and also a standardised measure of falls per 100 person years. This measure takes into account the variable follow-up times for individuals in the trial.
Sensitivity analysis
We used one way sensitivity analyses, calculating cost effectiveness ratios using a range of estimates of cost items for implementing the home safety programme, to investigate robustness of the cost effectiveness ratios to different delivery and adherence scenarios.
We used the 125th centile of the total, the total, and the 75th centile of the total implementation costs to calculate the cost effectiveness ratios to account for the possibility of different cost conditions when replicating the programme in different settings. The major cost items were the salary and travel costs of the occupational therapist and the cost of equipment installed in the homes. We used the following scenarios: the 125th centile of the costs of home visits to give an indication of costs of delivering the programme in a more spread out community and four times the cost of the equipment installed to indicate costs if equipment proved to be more expensive or the adherence level was higher than in this trial. To estimate the cost effectiveness of the programme at different levels of effectiveness we used fall reductions at the upper and lower 95% confidence limits of efficacy found in the trial.
Time horizon
Assuming that participants maintain behaviour changes and any home modifications, the benefits of the home safety programme will extend past the time each person participated in the trial, but the extent of this benefit and longer term compliance rates are uncertain. We calculated cost effectiveness ratios for the duration of the trial only.
Statistical analysis
Data were analysed on an intention to treat basis with Stata Release 7 and SPSS 11. We have adhered to the principles outlined in the revised CONSORT statement for reporting randomised controlled trials,21 those for reporting factorial designs,22 and recommendations for reporting falls prevention intervention trials developed by the Prevention of Falls Network Europe (ProFaNE).23
We compared the number of falls in the intervention and control groups using negative binomial regression models.24 These models estimate the number of occurrences of an event when the event has Poisson variation with overdispersion, allow for investigation of the treatment and interaction effects, and adjust for the variable follow-up times of participants. We also used negative binomial regression models to test whether there was a difference between the fall rates inside and outside the home environment and to determine the fall rates at different levels of adherence to the exercise programme. We included all falls in our analyses—that is, until the participant died, withdrew from the trial, or completed 12 months.
Results
Trial participants and follow-up
The mean age of participants was 83.6 (SD 4.8) years, and ages ranged from 75 to 96 years. Table 1 shows the characteristics of participants at entry to the trial. The four groups seemed well balanced at baseline. The flow of participants through the trial is shown in the figure.
Table 1.
Demographic and health related characteristics of study participants at entry to trial. Values are numbers (percentages) unless stated otherwise
|
Separate intervention groups
|
Combined intervention groups
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Home safety + exercise programmes (n=98) | Home safety programme alone (n=100) | Exercise programme alone (n=97) | Social visits alone (n=96) | Home safety programme (n=198) | No home safety programme (n =193) | Exercise programme (n=195) | No exercise programme (n=196) | |
| Mean (SD) age (years) | 83.8 (4.7) | 83.1 (4.5) | 83.4 (4.9) | 84.0 (4.9) | 83.4 (4.6) | 83.7 (4.9) | 83.6 (4.8) | 83.5 (4.7) |
| Women | 62 (63) | 66 (66) | 72 (74) | 67 (70) | 128 (65) | 139 (72) | 134 (69) | 133 (68) |
| Distance high contrast visual acuity*: | ||||||||
| 4/≥16 to 4/≤32 | 21 (21) | 16 (16) | 17 (18) | 32 (33) | 37 (19) | 49 (25) | 38 (19) | 48 (24) |
| 4/>32 to 4/≤64 | 22 (22) | 20 (20) | 19 (20) | 16 (17) | 42 (21) | 35 (18) | 41 (21) | 36 (18) |
| 4/>64 to 4/≤128 | 32 (33) | 29 (29) | 26 (27) | 19 (20) | 61 (31) | 45 (23) | 58 (30) | 48 (24) |
| 4/>128 to 4/≤256 | 4 (4) | 18 (18) | 16 (16) | 13 (14) | 22 (11) | 29 (15) | 20 (10) | 31 (16) |
| 4/>256 or no sight | 19 (19) | 17 (17) | 19 (20) | 16 (17) | 36 (18) | 35 (18) | 38 (19) | 33 (17) |
| Low contrast (10%) visual acuity*: | ||||||||
| 4/≤128 | 7 (7) | 13 (13) | 15 (15) | 18 (19) | 20 (10) | 33 (17) | 22 (11) | 31 (16) |
| 4/>128 to 4/≤256 | 26 (27) | 19 (19) | 15 (15) | 17 (18) | 45 (23) | 32 (17) | 41 (21) | 36 (18) |
| 4/>256 to 4/≤512 | 18 (18) | 22 (22) | 20 (21) | 15 (16) | 40 (20) | 35 (18) | 38 (19) | 37 (19) |
| 4/>512 to 4/≤1024 | 18 (18) | 15 (15) | 19 (20) | 20 (21) | 33 (17) | 39 (20) | 37 (19) | 35 (18) |
| 4/>1024 or no sight | 29 (30) | 31 (31) | 28 (29) | 26 (27) | 60 (30) | 54 (28) | 57 (29) | 57 (29) |
| Mean (SD) Melbourne edge test score*† | 7.9 (4.5) | 7.8 (4.5) | 7.5 (4.7) | 8.2 (5.0) | 7.8 (4.5) | 7.8 (4.8) | 7.7 (4.6) | 8.0 (4.7) |
| Peripheral field loss (one eye) | 60 (61) | 42 (42) | 44 (45) | 54 (56) | 102 (52) | 98 (51) | 104 (53) | 96 (49) |
| Peripheral field loss (both eyes) | 35 (36) | 23 (23) | 32 (33) | 31 (32) | 58 (29) | 63 (33) | 67 (34) | 54 (28) |
| Eye problems (self reported): | ||||||||
| Age related macular degeneration | 79 (81) | 90 (90) | 87 (90) | 73 (76) | 169 (85) | 160 (83) | 166 (85) | 163 (83) |
| Cataract | 46 (47) | 45 (45) | 36 (37) | 41 (43) | 91 (46) | 77 (40) | 82 (42) | 86 (44) |
| Diabetic retinopathy | 2 (2) | 3 (3) | 3 (3) | 4 (4) | 5 (3) | 7 (4) | 5 (3) | 7 (4) |
| Glaucoma | 12 (12) | 14 (14) | 15 (15) | 17 (18) | 26 (13) | 32 (17) | 27 (14) | 31 (16) |
| Eye surgery | 47 (48) | 51 (51) | 37 (38) | 43 (45) | 98 (49) | 80 (41) | 84 (43) | 94 (48) |
| Fall(s) in previous year | 42 (43) | 45 (45) | 41 (42) | 48 (50) | 87 (44) | 89 (46) | 83 (43) | 93 (47) |
| History of stroke | 19 (19) | 21 (21) | 16 (16) | 15 (16) | 40 (20) | 31 (16) | 35 (18) | 36 (18) |
| Hip fracture | 3 (3) | 7 (7) | 7 (7) | 2 (2) | 10 (5) | 9 (5) | 10 (5) | 9 (5) |
| Knee and/or hip pain | 31 (32) | 26 (26) | 41 (42) | 30 (32) | 57 (29) | 71 (37) | 72 (37) | 56 (29) |
| Takes multivitamin/other vitamin D containing medication | 14 (14) | 20 (20) | 27 (28) | 15 (16) | 34 (17) | 42 (22) | 41 (21) | 35 (18) |
| Takes psychotropic medication | 15 (15) | 18 (18) | 16 (16) | 18 (19) | 33 (17) | 34 (18) | 31 (16) | 36 (18) |
| Mean (SD) No of medications | 5.4 (2.9) | 4.5 (3.1) | 5.4 (3.6) | 4.9 (2.8) | 4.9 (3.0) | 5.1 (3.2) | 5.4 (3.2) | 4.7 (3.0) |
| Lives alone | 53 (54) | 51 (51) | 56 (58) | 48 (50) | 104 (53) | 104 (54) | 109 (56) | 99 (51) |
| Registered with Royal New Zealand Foundation of the Blind | 93 (95) | 95 (95) | 89 (92) | 86 (90) | 188 (95) | 175 (91) | 182 (93) | 181 (92) |
| Received services from Royal New Zealand Foundation of the Blind | 73 (74) | 69 (69) | 70 (72) | 62 (65) | 142 (72) | 132 (68) | 143 (73) | 131 (67) |
| Home help: | ||||||||
| Cleaning | 60 (61) | 63 (63) | 60 (62) | 61 (64) | 123 (62) | 121 (63) | 120 (62) | 124 (63) |
| Personal care | 11 (11) | 11 (11) | 10 (10) | 8 (8) | 22 (11) | 18 (9) | 21 (11) | 19 (10) |
| Meals | 11 (11) | 12 (12) | 11 (11) | 10 (10) | 23 (12) | 21 (11) | 22 (11) | 22 (11) |
Values are for better eye with participants given free choice about wearing spectacles.
Scores range from 0 to 24, higher scores indicate better contrast sensitivity.
The occupational therapist completed a six month follow-up telephone call for 85% (169/198) of those in the home safety group. The reasons for not completing the six month follow-up were that no recommendations for change were made at the initial home visit for 10 (5%) participants, four refused the initial visit, three had died, eight had moved to long term care, and four were lost to follow-up. Ninety per cent of participants (152/169) reported complying partially or completely with one or more of the recommendations made by the occupational therapist. Recommendations included removing or changing loose floor mats, painting the edge of steps, reducing glare, installing grab bars and stair rails, removing clutter, and improving lighting.
Eighteen per cent of participants (36/195) in the exercise groups carried out their prescribed set of exercises three or more times a week for one year (one person exercised three times a week until withdrawing from the trial); 70 (36%) completed their exercises at least twice a week during their time in the trial. A total of 44% (85 of 195) walked at least twice a week during the year; twenty one (11%) did not walk outside at all as part of the programme. Of those prescribed vitamin D supplements at trial entry, 100/145 continued taking the tablets for a year.
Falls and fall related injuries
Table 2 shows the actual and standardised numbers of falls and the numbers of falls resulting in injuries during the trial. There was a significant interaction between the two interventions for falls (P = 0.016) therefore we present the pre-planned combined group comparisons plus appropriate single group comparisons (table 3).22 We have reported the more conservative results of the combined group comparisons as the main outcomes of the trial. With this approach, the number of falls resulting in severe and moderate injuries or falls requiring medical care did not differ between the intervention groups (tables 2 and 3).
Table 2.
Incidence of fall events and follow-up times
|
Separate intervention groups
|
Combined intervention groups
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Home safety + exercise programmes (n=98) | Home safety programme alone (n=100) | Exercise programme alone (n=97) | Social visits alone (n=96) | Home safety programme (n=198) | No home safety programme (n=193) | Exercise programme (n=195) | No exercise programme (n=196) | |
| No of falls | 108 | 64 | 120 | 151 | 172 | 271 | 228 | 215 |
| Falls per person year | 1.17 | 0.65 | 1.30 | 1.65 | 0.90 | 1.47 | 1.23 | 1.13 |
| No (% of group) with ≥1 fall(s) | 47 (48) | 36 (36) | 47 (48) | 59 (61) | 83 (42) | 106 (55) | 94 (48) | 95 (48) |
| No (% of group) with ≥2 falls | 24 (24) | 16 (16) | 27 (28) | 29 (30) | 40 (20) | 56 (29) | 51 (26) | 45 (23) |
| No of injurious falls: | ||||||||
| Any | 61 | 39 | 53 | 65 | 100 | 118 | 114 | 104 |
| Serious | 11 | 10 | 4 | 4 | 21 | 8 | 15 | 14 |
| Moderate | 50 | 29 | 49 | 61 | 79 | 110 | 99 | 90 |
| Injurious falls per person year: | ||||||||
| Any | 0.66 | 0.40 | 0.57 | 0.71 | 0.53 | 0.64 | 0.62 | 0.55 |
| Serious | 0.12 | 0.10 | 0.04 | 0.04 | 0.11 | 0.04 | 0.08 | 0.07 |
| Moderate | 0.54 | 0.30 | 0.53 | 0.67 | 0.42 | 0.60 | 0.54 | 0.48 |
| No (%) of falls for which medical care sought | 30 (28) | 19 (30) | 32 (27) | 32 (21) | 49 (28) | 64 (24) | 62 (27) | 51 (24) |
| Mean (SD) follow-up (months) | 11.30 (2.27) | 11.77 (1.29) | 11.46 (2.17) | 11.41 (2.08) | 11.54 (1.85) | 11.44 (2.12) | 11.38 (2.22) | 11.60 (1.73) |
| Total follow-up (person years) | 92.24 | 98.12 | 92.63 | 91.31 | 190.36 | 183.94 | 184.87 | 189.43 |
Table 3.
Incidence rate ratios for fall events for home safety and exercise programmes*
| Incidence rate ratio (95% CI) | |
|---|---|
| Effect on falls | |
| Home safety programme: | |
| All receiving home safety programme (n=198) v all not receiving home safety programme (n=193) | 0.59 (0.42 to 0.83) |
| Home safety programme only group (n=100) v social visits group (n=96) | 0.39 (0.24 to 0.62) |
| Exercise programme: | |
| All receiving exercise programme (n=195) v all not receiving exercise programme (n=196) | 1.15 (0.82 to 1.61) |
| Exercise programme only group (n=97) v social visits group (n=96) | 0.79 (0.48 to 1.28) |
| Effect on injurious falls | |
| Home safety programme: | |
| All receiving home safety programme (n=198) v all not receiving home safety programme (n=193) | 0.81 (0.56 to 1.16) |
| Home safety programme only group (n=100) v social visits group (n=96) | 0.56 (0.36 to 0.87) |
| Exercise programme: | |
| All receiving exercise programme (n=195) v all not receiving exercise programme (n=196) | 1.15 (0.80 to 1.65) |
| Exercise programme only group (n=97) v social visits group (n=96) | 0.82 (0.48 to 1.40) |
Interaction ratios for falls and injurious falls were 2.28 (1.17 to 4.45) and 2.05 (0.99 to 4.23), respectively.
Home safety programme
There were 41% fewer falls in the participants of the home safety programme compared with those who did not receive this programme (incidence rate ratio 0.59, 95% confidence interval 0.42 to 0.83). There was no significant difference in the reduction of falls at home compared with those away from the home environment (ratio of incidence rate ratios 0.60, 0.31 to 1.17). No adverse events were reported as a result of this intervention.
Exercise programme
There were 15% more falls during the trial for participants randomised to the exercise programme compared with those who did not receive this programme (incidence rate ratio 1.15, 0.82 to 1.61). There was one moderate injury but no falls while the person was exercising according to instructions.
As the fall rate was higher in the exercise programme groups, we tested whether the exercise programme was safe to deliver to this sample of older people by investigating the relation between falls and the number of exercise sessions completed during the trial. We found that higher levels of adherence were associated with lower fall rates. The rate of falls was 77% lower in those who exercised at least three times a week during their time in the trial compared with those exercising less than once a week (table 4).
Table 4.
Incidence of falls by level of adherence to home exercise sessions*
| <1 session/week (n=53) | 1 to <2 sessions/week (n=35) | 2 to <3 sessions/week (n=70) | ≥3 sessions/week (n=37) | |
|---|---|---|---|---|
| No of falls | 98 | 57 | 55 | 18 |
| Falls per person year | 2.16 | 1.69 | 0.80 | 0.49 |
| Incidence rate ratio (95% CI) | 1.00 | 0.79 (0.42 to 1.50) | 0.37 (0.23 to 0.60) | 0.23 (0.12 to 0.45) |
Based on 156 (52×3) exercise sessions in 12 months pro rata. This relation held after adjustment for age, sex, previous fall, and total number of medications.
Economic evaluation
As we did not find that the exercise programme was effective in reducing falls in this trial, we report only the cost effectiveness of the home safety programme.
Table 5 shows the costs of implementing the home safety programme. The programme cost $NZ64 337 to deliver to the 198 participants in the two centres, or $NZ325 (SD $NZ292) per person. Table 6 shows the cost effectiveness ratios we calculated to indicate the incremental cost of implementing the home safety programme per fall prevented and the results of the sensitivity analyses. The incremental cost per fall prevented was $NZ650. Estimates ranged from $NZ460 to $NZ1569 per fall prevented for the different cost scenarios.
Table 5.
Incremental costs ($NZ*) of implementing the home safety programme
| Cost item | Resource use | Unit cost | Total cost |
|---|---|---|---|
| Training costs | |||
| Occupational therapists: | |||
| Time | 15 hours each | 24.92 | 748 |
| Programme supervisor: | |||
| Time | 30 hours | 56.41 | 1692 |
| Travel | Flights, airport transfers | 1463 | |
| Accommodation | 4 nights | 150.00 | 600 |
| Transport to visit clients | 96 km | 0.62 | 60 |
| Materials | Manuals, photocopying, street maps | Variable | 268 |
| Recruitment | |||
| Clinic staff | Time | 7.50† | 953 |
| Staff at Royal New Zealand Foundation of the Blind | Time, telephone calls | 6.50/3.50‡ | 805 |
| Programme delivery | |||
| Occupational therapists§: | |||
| Time | 699 hours | 24.92 | 17 428 |
| Transport | 4369 km | 0.62 | 2709 |
| Practising certificates | 2 | 120.00 | 240 |
| Administration | Stationery, photocopying, stamps | 4.35 | 861 |
| Telephone calls, email, facsimiles | 783 calls | 0.20 | 157 |
| Services and equipment installed in homes:
|
|
|
|
| Funded by trial | Various¶ | Actual** | 6023 |
| Funded by client or family | Various¶ | Actual** | 2835 |
| Provided by Royal New Zealand Foundation of the Blind | Various¶ | Actual** | 1350 |
| Provided by other health agencies | Various¶ | Actual** | 14 460 |
| Provided by housing management | Various¶ | Actual** | 149 |
| Overhead costs†† | — | — | 11 537 |
| Total cost | — | — | $64 337 |
| Mean (SD) cost per participant | — | — | $325 ($292) |
| Cost per fall prevented | — | — | $650 |
Average exchange rate in 2004, $NZ1.00=£0.36, €0.53, and $US0.66.
$7.50 per participant.
$6.50 Dunedin, $3.50 Auckland per potential participant, pro rata allocated to intervention group.
Includes home visits and organising any modifications.
Rubber backed mats, contrast paint on edge of steps, shower stools, bathroom rails, shower matting, outdoor rails, walking canes, slippers, etc.
Actual costs used when available.
Office accommodation, financial and administration services, depreciation on equipment.
Table 6.
Cost effectiveness ratios and sensitivity analysis: incremental cost ($NZ*) per fall prevented for implementing home safety programme
| Cost scenario | Cost |
|---|---|
| Cost per fall prevented: | |
| Total cost of implementing programme | 650 |
| 125th centile total cost of programme | 812 |
| 75th centile total cost of programme | 487 |
| 125th centile cost of home visits | 716 |
| Equipment costs ×4 | 1566 |
| Falls reduced by 17% (upper 95% confidence limit) | 1569 |
| Falls reduced by 58% (lower 95% confidence limit) | 460 |
| Adjusted cost per fall prevented†: | |
| Total cost of implementing programme | 1129 |
| 125th centile total cost of programme | 1411 |
| 75th centile total cost of programme | 847 |
| 125th centile cost of home visits | 1243 |
| Equipment costs ×4 | 2720 |
| Falls reduced by 17% (upper 95% confidence limit) | 2725 |
| Falls reduced by 58% (lower 95% confidence limit) | 798 |
Average exchange rate in 2004, $NZ1.00=£0.36, €0.53, and $US0.66.
Calculated with fall events per 100 person years to adjust for variable follow-up time of individuals in trial.
Discussion
We have shown that in community based programmes for prevention of falls one size does not fit all. Just as an individual patient requires specific prevention treatments, different elderly populations require specifically selected programmes. Our results indicate that an organisation seeking to reduce falls in elderly people with severe visual impairment would do best by investing in a proved programme of home safety assessment and modification delivered by an occupational therapist.
Many falls result from trips and slips when the impaired balance of an elderly person prevents swift corrective action. Removal of environmental hazards has therefore seemed a logical measure to prevent falls. The problem with this approach has been that these hazards are so ubiquitous it is difficult to remove them all. Also such an approach does not address the underlying problem of poor balance. In two previous studies such an intervention was only partially successful.25,26 Only those who had a history of falls benefited and falls occurring outside were reduced to the same extent as falls within the home. Similarly in our study, falls inside and outside the home environment were reduced, suggesting that, despite the specific protocol, prevention results from the professional advice of the occupational therapist as well as the environmental changes.
The Otago exercise programme, previously shown to be of benefit in those aged ≥80,18,19,27 was not successful in this population. The fall rate was greater in the exercise group, albeit not significantly so, and we were concerned that the programme may be dangerous in those with visual impairment. The fall rate was highest in those with the lowest adherence to the programme and lowest in the group who exercised at least three times a week (table 3). This may be a frailer population than we have studied before and more participants were unable to participate fully in the strength and balance retraining. Adherence rates were considerably lower than in our previous trials.18,19,27
The home safety programme we adapted for older people with severe vision loss is currently the only successful falls prevention programme reported for this group, although earlier cataract removal was associated with fewer falls and fractures in elderly women on the waiting list for cataract surgery.28 Our home safety programme cost less per person to implement than the Otago exercise programme delivered to people aged ≥75 with normal sight ($NZ484 per person at 2004 prices).18 When we considered savings in hospital costs resulting from a reduction in serious injuries, however, the Otago exercise programme in the previous trial was more cost effective to deliver than the home safety programme in the current trial.18
Limitations of the study
We had not expected any interaction between the two interventions and have no convincing explanation for the fact that the home safety programme seemed less effective when the person was also receiving the exercise programme. It may simply be a chance effect. We feel that the conservative estimates for the combined group rate ratio are more likely to indicate the efficacy of the interventions (see table 3).
Participants were recruited through the Royal New Zealand Foundation of the Blind and through low vision clinics. They were not selected for their ability to participate in an exercise programme. A population screened through primary care for their ability to participate in an exercise programme may benefit.
Many of those who were registered with the Foundation of the Blind had already undertaken an orientation and mobility programme and this might have lessened the benefit from the home safety programme.
The duration of visual impairment varied considerably, as did the causes of blindness. There were too few participants to determine if particular groups, such as those who had lost their sight recently, benefited more from the home safety programme.
Future directions
Falls result in loss of confidence, injuries, admission to an institution, fractures, and death.6 They can be prevented at a cost. Careful targeting of the programme to specific population groups and avoidance of programmes in groups who will not benefit can reduce that cost. There is now sufficient evidence from trials to design community programmes to prevent falls so that the specific interventions are used only in the particular populations known to benefit.
What is already known on this topic
Older people with poor vision are at increased risk of falling
Home safety assessment and modification programmes can be effective in reducing falls in those who have fallen previously
A home based strength and balance retraining programme (the Otago exercise programme) is effective in reducing falls in older people with normal sight living in the community
What this study adds
Community based programmes for prevention of falls should be targeted at particular population groups
Older people with severe visual impairment can benefit from a specially developed programme of home safety assessment and modification
A home exercise programme was not effective in reducing falls in this sample with visual impairment, possibly due to lower levels of adherence
We thank the participants; research nurses Glynnis Clarke and Karen Hayman; physiotherapists Susan Kohut, Ineke Stol, and Stephanie Woodley; occupational therapists Wendy Hughes and Fiona Mains; administrator Liz Kiata; and statisticians Jo McKenzie, Sheila Williams, and Peter Herbison. We are grateful to the Royal New Zealand Foundation of the Blind and to the low vision clinic staff for their involvement in this trial. We thank Ross McCormick for supervision of staff.
Contributors: All authors contributed to the study or protocol design, or both, interpreted the data, and wrote the paper. AJC directed the project, interpreted the data, and wrote the paper. MCR managed the project and the data gathering, analysed and interpreted the data, and wrote the paper. MCR and NMK supervised the research staff. SJLaG developed the home safety programme. GFS, RJJ, and DMS advised on vision measures and recruited participants. LAH supervised the physiotherapists. AJC and MCR are guarantors.
Funding: Health Research Council of New Zealand.
Competing interests: None declared.
Ethical approval: Otago and Auckland ethics committees.
References
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988;319: 1701-7. [DOI] [PubMed] [Google Scholar]
- 2.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol Med Sci 1989;44: M112-7. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 1994;331: 821-7. [DOI] [PubMed] [Google Scholar]
- 4.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet 1999;353: 93-7. [DOI] [PubMed] [Google Scholar]
- 5.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev 2003;(4): CD000340. [DOI] [PubMed]
- 6.American Geriatrics Society, British Geriatrics Society, American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc 2001;49: 664-72. [PubMed] [Google Scholar]
- 7.NHS National Institute for Clinical Excellence. Falls: the assessment and prevention of falls in older people. Clinical Guideline 21, November 2004. www.nice.org.uk/CG021NICEguideline (accessed May 2005).
- 8.Tinetti ME, McAvay G, Claus E. Does multiple risk factor reduction explain the reduction in fall rate in the Yale FICSIT trial? Am J Epidemiol 1996;144: 389-99. [DOI] [PubMed] [Google Scholar]
- 9.Shaw FE, Bond J, Richardson DA, Dawson P, Steen IN, McKeith IG, et al. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. BMJ 2003;326: 73-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in elderly people by preventing falls: a meta-analysis of individual level data. J Am Geriatr Soc 2002;50: 905-11. [DOI] [PubMed] [Google Scholar]
- 11.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc 1999;47: 850-3. [DOI] [PubMed] [Google Scholar]
- 12.Lord SR, Dayhew J. Visual risk factors for falls in older people. J Am Geriatr Soc 2001;49: 508-15. [DOI] [PubMed] [Google Scholar]
- 13.Clemson L. Home fall hazards: a guide to identifying fall hazards in the homes of elderly people and an accompaniment to the assessment tool, the Westmead home safety assessment (WeHSA). West Brunswick, Victoria: Co-ordinates Publications, 1997.
- 14.Accident Compensation Corporation. Otago exercise programme to prevent falls in older adults. August 2003. www.acc.co.nz/injury-prevention/growing-and-living-safely (accessed May 2005).
- 15.Lord SR, Clark RD, Webster IW. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc 1991;39: 1194-200. [DOI] [PubMed] [Google Scholar]
- 16.Buchner DM, Hornbrook MC, Kutner NG, Tinetti ME, Ory MG, Mulrow CD, et al. Development of the common database for the FICSIT trials. J Am Geriatr Soc 1993;41: 297-308. [DOI] [PubMed] [Google Scholar]
- 17.Crown Company Monitoring Advisory Unit. Hospital and health services performance reporting measures. Quarter ended 30 September 1999. Wellington: The Treasury, 1999.
- 18.Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ 2001;322: 697-701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ 2001;322: 701-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drummond MF, O'Brien B, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 2nd ed. New York, NY: Oxford University Press, 1997.
- 21.Moher D, Schulz KF, Altman DG, Group C. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 2001;357: 1191-4. [PubMed] [Google Scholar]
- 22.McAlister FA, Straus SE, Sackett DL, Altman DG. Analysis and reporting of factorial trials: a systematic review. JAMA 2003;289: 2545-53. [DOI] [PubMed] [Google Scholar]
- 23.Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, on behalf of Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc 2005;53: 1618-22. [DOI] [PubMed] [Google Scholar]
- 24.Robertson MC, Campbell AJ, Herbison P. Statistical analysis of efficacy in falls prevention trials. J Gerontol Med Sci 2005;60A: 530-4. [DOI] [PubMed] [Google Scholar]
- 25.Cumming RG, Thomas M, Szonyi G, Salkeld G, O'Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc 1999;47: 1397-402. [DOI] [PubMed] [Google Scholar]
- 26.Nikolaus T, Bach M. Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized Falls-HIT trial. J Am Geriatr Soc 2003;51: 300-5. [DOI] [PubMed] [Google Scholar]
- 27.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315: 1065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harwood RH, Foss AJE, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol 2005;89: 53-9. [DOI] [PMC free article] [PubMed] [Google Scholar]