Abstract
The aim of this study was to compare outcomes between anteverting proximal femoral osteotomy (APFO) and anteverting periacetabular osteotomy (APAO) for femoroacetabular impingement syndrome (FAIS) due to combined acetabular retroversion (ARV) and femoral retrotorsion (FRT). We also compared these outcomes with hip arthroscopy (HA) for FAIS without ARV or FRT. Twelve patients with ARV and FRT underwent either APAO (six) or APFO (six) at two centres. A control group of 24 patients underwent HA for FAIS without version abnormality. Outcome measures included various hip scores, time to radiological bony union, complications, and conversion to hip arthroplasty. At the 2-year follow-up, no AFPO or APAO hips required arthroplasty. Patient-reported outcome scores showed no significant difference between the APAO and APFO groups: Non-Arthritic Hips Scores (NAHS) (APAO: median 72, range 52–78; APFO: 76, 52–80, P = .76), International Hip Outcome Tool 12 (iHOT-12) (APAO: 64, 48–70 vs. APFO: 55, 46–72, P = .57), EuroQol 5 Dimension Visual Analogue Scale (APAO: 72, 57–78 vs. APFO: 75, 49–80 P = .78), and University of California Los Angeles Score (APAO: 7, 4–8 vs. APFO: 6, 4–9 P = .43). APAO patients achieved radiological union faster (10.2 weeks: 6.6–19.3 vs. 19.2 weeks: 12–23, P = .05). Aside from metalwork removal, one AFPO patient required revision intramedullary nail to induce union. Compared to AFPO or APAO, HA patients (NAHS: 86.7, 72.1–94.1; iHOT-12: 73.1, 63.2–88.1) had better outcome scores (P < .05). Both APFO and APAO can achieve good outcomes and short-term survivorship for combined ARV and FRT, although function may be inferior to HA in patients without rotational abnormalities.
Introduction
The understanding of the causes of femoroacetabular impingement (FAI) has evolved since it was originally described as a conflict between the femoral head–neck junction and acetabulum, typically arising from cam- or pincer-type deformity [1]. Rotational abnormalities of the acetabulum and proximal femur affect a hip’s range of motion due to premature contact between the pelvis and femur [2, 3]. Furthermore, they amplify the impingement effect of cam- and focal pincer-type deformity [4, 5] and are a cause of coxarthrosis [6].
Acetabular retroversion (ARV)—described by Reynolds et al. [7]—is prevalent in ∼12% of patients presenting to a young adult hip clinic [8]. It may be treated by arthroscopic rim trimming [9, 10] or anteverting periacetabular osteotomy (APAO) [11]. Femoral retrotorsion (FRT) is prevalent in ∼22% of patients presenting to a young adult hip clinic [8]. It is classically treated with an anteverting proximal femoral osteotomy (APFO); it was first described by Tönnis and Heinecke [12] and has good outcomes [13, 14]. Arthroscopic cam-resection is a minimally invasive alternative to APFO, improving the head-neck offset and range of motion, while providing an opportunity to address chondrolabral injury . However, it is progressively less effective with more severe FRT [15].
Patients with combined ARV and FRT make up a minority (4%) of patients presenting to a young adult hip clinic; however, their morphology puts them at increased risk of symptomatic FAI [8]. It is, however, currently unknown whether this combined deformity is most effectively managed by APAO or APFO.
The aim of this study was to determine whether there was a difference in morbidity, joint preservation rates, and postoperative patient-reported outcome measures (PROMs) for two cohorts of patients with combined ARV and FRT, with one group undergoing a minimally invasive APAO and another undergoing APFO. We also compared these patients to a control cohort of patients with a diagnosis of FAI without rotational abnormality treated through hip arthroscopy (HA).
Materials and methods
This is an institutionally approved retrospective study from two tertiary referral centres for Young Adult Hip Pathology between 2013 and 2016. It included patients with FAI who were refractory to nonoperative management (weight loss, physiotherapy, and activity modifications). Clinical assessment included measurement of lower limb rotational profile. Radiographic assessment consisted of a standardized supine anteroposterior (AP) pelvic radiograph. A dedicated low-dose limited CT rotational profile assessment (CTRPA) of the pelvis, hip, and knee joints was undertaken for those in whom a rotational abnormality was suspected [16]. In the first centre, a single high-volume PAO surgeon (J.D.W.) performs >150 PAOs a year, and APAO is the preferred procedure for managing combined ARV and FRT. In the second centre, two highly experienced hip preservation surgeons (TA and T.P.) prefer APFO. The control patients were selected from one surgeon’s (AJA) practice at the second centre. They had no discernible rotational malalignment on clinical examination and therefore did not undergo CT imaging. Patients for whom malrotation is suspected typically undergo a dedicated low-dose limited CTRPA. Patients with coxarthrosis (Tönnis grade > 1) or hip dysplasia (lateral centre edge angle, LCEA < 24°) were excluded. Patients with combined ARV and FRT were offered either APAO or APFO according to local practice.
Across the two centres, 11 patients (five males and six females; 12 hips) had combined ARV and FRT who had undergone surgery. The mean age was 24.5 years (SD 3.7), and the two cohorts were equivalent for age (P > .05) and sex distribution (P > .05). Twenty-four control patients were identified from the second centre’s institutional database, comprising age-matched six males and 18 females undergoing HA between 2014 and 2016, in a 1:2 ratio; this resulted in 24 hips who had undergone HA for symptomatic FAI without a rotational abnormality.
For all cases, the LCEA and Acetabular Index (AI) were measured on the plain AP radiograph, and hip dysplasia was identified as a lateral centre-edge angle of <22°. The use of CT for assessing femoral version has been validated by Botser et al. [17], and our protocols used the same technique of obtaining images through the hip including femoral neck and at the distal femoral condyles. Femoral version was measured using the technique described by Murphy et al. [18]. Acetabular version was assessed through the identification of radiographic markers of ARV (crossover sign, ischial spine sign, and posterior wall sign) on the plain AP pelvis radiograph as described by Jamali et al. [19], and then this was confirmed by measuring both the cranial and central version as described by Reynolds et al. [7] and Tönnis and Heinecke [6], respectively. Measurements were recorded independently by two of the authors (P.H. and S.S.) and were confirmed by a third author (AJA) when there was a discrepancy.
The minimally invasive surgical technique for APAO has been described by Khan et al. [20] and is performed via a modified Smith–Petersen approach with fluoroscopic guidance, and the acetabular fragment is fixed with three long 4.5-mm screws introduced from the iliac crest. Patients were advised to partially weight bear with 20 kg on the operated side postoperatively for the first 6 weeks before progressing to full weight-bearing over the following 6 weeks.
APFO was carried out under fluoroscopic guidance just below the level of the lesser trochanter and fixed with a Dynamic Hip Screw (DePuy Synthes, USA) (one patient), LCP Proximal Femoral Plate (DePuy Synthes) (two patients), or TFN-advanced short femoral nail (DePuy Synthes, USA) (three patients) using a previously described technique [13]. The change in fixation device for APFO was driven by the operating centre’s belief that the cephalomedullary screw of an intramedullary device may preserve bone stock within the femoral head and neck and may allow for better control of the rotational correction and easier identification of the correction intra-operatively. In the surgeon’s (A.J.A.) experience, it was noted that the plate devices often occluded a view of the osteotomy site once the plate was applied for fixation, and guide-pins interfered with plate fixation. A change to intramedullary fixation enabled optimal control during rotational correction and an unobstructed view of the osteotomy site; however, disadvantages include potential injury to peritrochanteric soft tissue structures. Patients undergoing APFO after intramedullary nail were advised to toe-touch weight bear on the operated side for the first 2 weeks, progressing to full weight-bearing as able thereafter.
HA for FAI was performed using a standardized supine technique with a traction table, and the hip accessed through two anterolateral and mid-anterior portals. Labral pathology was addressed through either repair or debridement as appropriate, and the cam- and/or pincer-type deformity was corrected by femoral osteochondroplasty and/or acetabular rim trim, respectively. Postoperatively, patients were advised to fully weight bear and were commenced on an established post-HA physiotherapy protocol.
Postoperative PROMs were recorded prospectively in all the groups. The Non-Arthritic Hips Scores (NAHS) [21], International Hip Outcome Tool 12 (iHOT-12) [22], EuroQol 5 Dimension Visual Analogue Scale (EQ5D-VAS) [23], and the University of California Los Angeles (UCLA) Score [24] were collected in patients undergoing APAO or APFO; the NAHS and iHOT-12 were collected patients who underwent HA. Surgical complications as per Clavien–Dindo [25] at the final follow-up are classified as follows: Grade 1 denotes any deviation from the normal postoperative course without the need for pharmacological, radiological, or surgical intervention. Grades 2–5 ranges from complications that requiring pharmacological intervention, blood transfusion, surgical/radiological/endoscopic intervention, to those resulting in organ dysfunction, and mortality. The incidence of reoperation or conversion to hip arthroplasty was also collected at the final follow-up. Bony union was assessed on femoral radiographs using the modified Radiological Union of Tibial Fractures (mRUST) score [26], which was routinely calculated at 2-, 6-, 12-, and 24-week follow-up and at all subsequent clinical consultations. An mRUST score of >12 denoted radiographic femoral union. Union of the periacetabular osteotomy was determined subjectively by the operating surgeon (J.D.W.) from an AP Pelvis radiograph at the same follow-up timepoints. Radiographic findings were correlated with the absence of local pain on weight-bearing to confirm clinical bony union. Patients were followed up for an average of 26 months (range 16–53).
Statistical analysis was carried out using Microsoft Excel (Microsoft, One Microsoft Way, Redmond, WA, USA). The Shapiro–Wilk test was used to assess normality, and subsequently the chi-squared test used to compare categorical variables, and the t-test used to detect differences in the outcome measurements between the two groups. A P-value of <.05 was considered statistically significant.
Results
The patient demographics and radiological measurements are reported in Table 1. At a mean follow-up of 2 years, no hips within the osteotomy or arthroscopy groups had undergone arthroplasty.
Table 1.
Radiographic values of patients undergoing osteotomy or HA.
| APFO | APAO | HA | P-value | |
|---|---|---|---|---|
| Mean age (SD) | 24.5 (3.7) | 24.8 (5.6) | 39 (14.6) | .003 |
| Sex | Four males and two females | Two males and four females | Six males and 18 females | .062 |
| Mean lateral centre-edge angle (SD) | 36.3 (4.5) | 33.7 (3.8) | 35.7 (4.2) | .322 |
| Mean AI (SD) | 7.5 | 3.7 | 7.6 | .055 |
| Mean femoral version (SD, range) | −0.9 (3.1, −5 to 3 | 4.3 (5.7, −2 to 11) | N/A | .099 |
| Mean cranial acetabular version, (SD, range) | −6.3 (8.0, −19 to 0 | −4.7 (4.8, −10 to 3) | N/A | .221 |
| Mean crossover ratio (SD, range) | 0.26 (0.15, 0–0.4) | 0.29 (0.16, 0–0.5) | N/A | .221 |
| Presence of crossover sign, ischial spine sign, and posterior wall sign (number/total number of patients) | 6/6, 6/6, and 4/6 | 5/6, 5/6, and 5/6 | N/A | N/A |
| Mean McKibbin index (SD) | 13.4 (11.2) | 15.1 (12.1) | N/A | .327 |
We found no statistical difference in the outcome scores between the APFO and APAO groups. Specifically, there was no statistical difference in patient-reported outcome scores between the two osteotomy groups: NAHS (APAO: median 72, range 52–78; APFO: 76, 52–80, P = .76), iHOT-12 (APAO: 64, 48–70 vs. APFO: 55, 46–72, P = .57), EQ5D-VAS (APAO: 72, 57–78 vs. APFO: 75, 49–80, P = .78), and UCLA (APAO: 7, 4–8 vs. APFO: 6, 4–9, P = .43) (Figure 1). However, the outcome scores in the HA group (NAHS 86.7, 72.1–94.1; iHOT-12 73.1, 63.2–88.1) were statistically significantly higher than those in both osteotomy groups (NAHS, P = .02 and iHOT-12, P = .04) (Figure 1).
Figure 1.
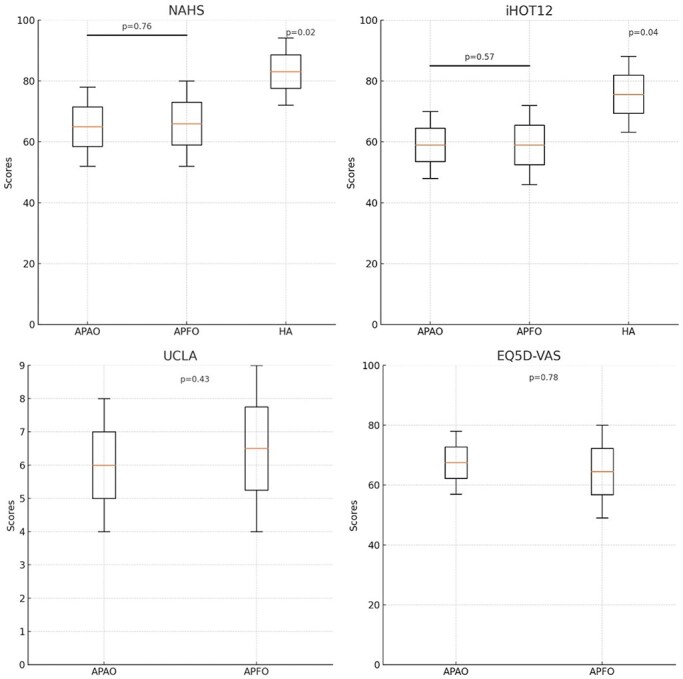
Patient-reported outcome measures of patients undergoing APFO, APAO, or HA.
All patients had achieved bony union at the time of the final follow-up. The median time taken for union for the APAO group was 10 weeks (range 6.6–19.3), and that for the AFPO group was 19 weeks (range 11.9–35.9) (P = .053); thus, there was a trend for the APAO group to achieve radiological union more quickly than the APFO group, but this was not statistically significant.
Complications were experienced in both osteotomy groups. In the APFO group, there were no Grade 1 complications, and two Grade 3 complications: one patient required dynamization of the nail before union was confirmed radiologically, and the other required removal of the compression plate as it caused discomfort when laying in the lateral position. In the APAO group, there were no Grade 1 complications and two Grade 2 complications: two patients underwent steroid injections to the psoas sheath to address psoas tendon irritation with complete relief. Six APAO hips underwent routine removal of screws as per local protocol with no adverse effects, and these were classed as Grade 3 complications as per Clavien–Dindo [25].
Discussion
The optimal management of combined ARV with FRT is yet to be determined. This study demonstrated that there was no difference in functional outcome whether the combined deformity was addressed through either acetabular or femoral osteotomy.
Compared to HA for FAI without rotational deformity (the control group), patients undergoing APAO or APFO achieved greater postoperative function—evidenced by significantly higher NAHS and iHOT-12 scores. Both APAO and APFO cohorts had two patients who continued to experience some pain postoperatively despite adequate improvement in rotational profile confirmed on postoperative multiplanar imaging. Preoperative scores would have demonstrated whether there had been an objective symptomatic improvement, and further investigation is required to determine the cause of persistent pain, such as symptomatic labral pathology. There is a dearth of evidence for validated PROMs’ thresholds for significant clinical benefit for managing rotational deformities with pelvic or femoral osteotomies. However, when evaluating postoperative PROMs with the patient acceptable symptom state previously reported for HA patients (iHOT-12 >62), 7 of the 11 included patients achieved this threshold [27]. Furthermore, the median postoperative NAHS for 62 patients undergoing APAO for isolated ARV at the same surgical centre was 76.7 (SD 17.9) [28]. Albeit without formal statistical comparison, this is higher than that reported in this study of patients undergoing APOA for combined acetabular and femoral retroversion (median 72, range 52–78). This underlines the complex nature of patients with rotational abnormalities, and our results highlight the importance of setting appropriate expectations and shared decision-making with patients. Finally, there may be a role for hip concurrent or subsequent HA to address labral pathology, although this is outside the scope of this study.
While patients with ARV underwent APAO using a consistent surgical technique [20], no optimal fixation device existed for APFO, and there was significant variation in technique within this cohort. Contemporary femoral osteotomy devices utilize an intra-medullary blade which may obviate the need for a lateral femoral incision [29], while contemporary intra-medullary femoral nails allow for active compression at the osteotomy site [30]. This is the authors’ current preferred technique, and future studies may demonstrate reduced pain and optimized bony union as a result.
Limitations to this study include the small sample size. Patients with combined femoral and ARV represent a minority of patients presenting with lower limb rotational deformity [8]. Both our units are high-volume young adult hip specialist tertiary referral centres within the UK, and yet only 11 patients with this particular deformity were identified and treated with an osteotomy over a 5-year period. The equivalence in outcomes between APAO and APFO may therefore be due to an underpowered sample. A larger sample size may also have revealed differences in femoral torsion between the APAO and APFO groups, which would also influence decision-making in clinical practice. Secondly, preoperative PROMs were not available. We therefore elected to compare APAO and APFO with HA for FAI as a relevant benchmark. Third, bony union was measured using radiographs rather than CT to reduce radiation exposure, and while the mRUST score allows some objectivity to assess femoral healing, APAO healing was qualitatively judged. Finally, this study did not investigate the impact of tibial torsion on FAI—external tibial torsion can also amplify the effect of ARV and FRT [31] and is an avenue for future study.
Conclusion
This small study demonstrates that patients with symptomatic FAI secondary to combined ARV and FRT can be successfully treated with either anteverting acetabular or femoral osteotomy according to surgeon expertise and preference. Patients can expect good clinical outcomes from rotational osteotomies, although these may be inferior to patients with cam- or pincer-type FAI without rotational deformity treated with HA.
Contributor Information
Kartik Logishetty, Young Adult Hip Unit, University College London Hospitals NHS Foundation Trust, 235 Euston Road, London NW1 2BU, United Kingdom; Department of Trauma and Orthopaedic, Royal Berkshire NHS Foundation Trust, London Road, Reading RG1 5AN, United Kingdom; MSk Lab, Imperial College London, Sir Michael Uren Hub, 86 Wood Lane, London W12 0BZ, United Kingdom.
Paul Haggis, Department of Trauma and Orthopaedics, Royal Cornwall Hospitals NHS Trust, Treliske, Truro TR1 3LJ, United Kingdom.
Saif Salih, Department of Trauma and Orthopaedics, Northern General Hospital, Herries Rd, Sheffield S5 7AU, United Kingdom.
George Grammatopoulos, Department of Orthopaedic Surgery, Ottawa Hospital, 251 Smyth Road, Ottawa, ON K1H 8L6, Canada.
Tom Pollard, Department of Trauma and Orthopaedic, Royal Berkshire NHS Foundation Trust, London Road, Reading RG1 5AN, United Kingdom; Reading Orthopaedic Centre, Circle Reading Hospital, 100 Drake Way, Reading, London RG2 0NE, United Kingdom.
Johan D Witt, Young Adult Hip Unit, University College London Hospitals NHS Foundation Trust, 235 Euston Road, London NW1 2BU, United Kingdom.
Antonio J Andrade, Young Adult Hip Unit, University College London Hospitals NHS Foundation Trust, 235 Euston Road, London NW1 2BU, United Kingdom; Reading Orthopaedic Centre, Circle Reading Hospital, 100 Drake Way, Reading, London RG2 0NE, United Kingdom.
Conflict of interest:
None declared.
Funding
None declared.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Ganz R, Parvizi J, Beck M et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;417:112–20. [DOI] [PubMed] [Google Scholar]
- 2. Shin J, Adeyemi TF, Hobson T et al. The bipolar hip: how acetabular and femoral pathomorphology affects hip motion in femoral acetabular impingement syndrome. Arthroscopy 2020;36:1864–71. [DOI] [PubMed] [Google Scholar]
- 3. Chadayammuri V, Garabekyan T, Bedi A et al. Passive hip range of motion predicts femoral torsion and acetabular version. JBJS 2016;98:127–34. [DOI] [PubMed] [Google Scholar]
- 4. Kraeutler MJ, Chadayammuri V, Garabekyan T et al. Femoral version abnormalities significantly outweigh effect of cam impingement on hip internal rotation. JBJS 2018;100:205–10. [DOI] [PubMed] [Google Scholar]
- 5. Lerch TD, Boschung A, Todorski IA et al. Femoroacetabular impingement patients with decreased femoral version have different impingement locations and intra-and extraarticular anterior subspine FAI on 3D-CT-based impingement simulation: implications for hip arthroscopy. Am J Sports Med 2019;47:3120–32. [DOI] [PubMed] [Google Scholar]
- 6. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 1999;81:1747–70. [DOI] [PubMed] [Google Scholar]
- 7. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br 1999;81:281–8. [DOI] [PubMed] [Google Scholar]
- 8. Lerch TD, Todorski IA, Steppacher SD et al. Prevalence of femoral and acetabular version abnormalities in patients with symptomatic hip disease: a controlled study of 538 hips. Am J Sports Med 2018;46:122–34. [DOI] [PubMed] [Google Scholar]
- 9. Maldonado DR, Chen JW, Kyin C et al. Hips with acetabular retroversion can be safely treated with advanced arthroscopic techniques without anteverting periacetabular osteotomy: midterm outcomes with propensity-matched control group. Am J Sports Med 2020;48:1636–46. [DOI] [PubMed] [Google Scholar]
- 10. Alter TD, Knapik DM, Lambers F et al. Outcomes for the arthroscopic treatment of femoroacetabular impingement syndrome with acetabular retroversion: a 3D computed tomography analysis. Am J Sports Med 2022;50:2155–64. [DOI] [PubMed] [Google Scholar]
- 11. Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am 2003;85:278–86. [DOI] [PubMed] [Google Scholar]
- 12. Tönnis D, Heinecke A. Diminished femoral antetorsion syndrome: a cause of pain and osteoarthritis. J Pediatr Orthop 1991;11:419–31. [DOI] [PubMed] [Google Scholar]
- 13. Buly RL, Sosa BR, Poultsides LA et al. Femoral derotation osteotomy in adults for version abnormalities. J Am Acad Orthop Surg 2018;26:e416–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mastel M, El-Bakoury A, Parkar A et al. Outcomes of femoral de-rotation osteotomy for treatment of femoroacetabular impingement in adults with decreased femoral anteversion. J Hip Preservation Surg 2020;7:755–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fabricant PD, Fields KG, Taylor SA et al. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. JBJS 2015;97:537–43. [DOI] [PubMed] [Google Scholar]
- 16. Henckel J, Richards R, Lozhkin K et al. Very low-dose computed tomography for planning and outcome measurement in knee replacement: the imperial knee protocol. J Bone Joint Surg Br Vol 2006;88:1513–8. [DOI] [PubMed] [Google Scholar]
- 17. Botser IB, Ozoude GC, Martin DE et al. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy 2012;28:619–27. [DOI] [PubMed] [Google Scholar]
- 18. Murphy SB, Simon SR, Kijewski PK et al. Femoral anteversion. JBJS 1987;69:1169–76. [PubMed] [Google Scholar]
- 19. Jamali AA, Mladenov K, Meyer DC et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross‐over‐sign”. J Orthop Res 2007;25:758–65. [DOI] [PubMed] [Google Scholar]
- 20. Khan O, Malviya A, Subramanian P et al. Minimally invasive periacetabular osteotomy using a modified Smith-Petersen approach: technique and early outcomes. Bone Joint J 2017;99:22–8. [DOI] [PubMed] [Google Scholar]
- 21. Christensen CP, Althausen PL, Mittleman MA et al. The nonarthritic hip score: reliable and validated. Clin Orthopaed Related Res(1976–2007) 2003;406:75–83. [DOI] [PubMed] [Google Scholar]
- 22. Griffin DR, Parsons N, Mohtadi NG et al. , Multicenter Arthroscopy of the Hip Outcomes Research Network . A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy 2012;28:611–8. [DOI] [PubMed] [Google Scholar]
- 23. Oppe M, Devlin NJ, van Hout B et al. A program of methodological research to arrive at the new international EQ-5D-5L valuation protocol. Value Health 2014;17:445–53. [DOI] [PubMed] [Google Scholar]
- 24. Zahiri CA, Schmalzried TP, Szuszczewicz ES et al. Assessing activity in joint replacement patients. J Arthroplasty 1998;13:890–5. [DOI] [PubMed] [Google Scholar]
- 25. Clavien PA, Barkun J, De Oliveira ML et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187–96. [DOI] [PubMed] [Google Scholar]
- 26. Plumarom Y, Wilkinson BG, Willey MC et al. Sensitivity and specificity of modified RUST score using clinical and radiographic findings as a gold standard. Bone Jt Open 2021;2:796–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nwachukwu BU, Chang B, Beck EC et al. How should we define clinically significant outcome improvement on the iHOT-12? HSS J 2019;15:103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Verhaegen J, Salih S, Thiagarajah S et al. Is a periacetabular osteotomy as efficacious in retroversion as it is in dysplasia?: The role of femoral anteversion on outcome. Bone Joint Open 2021;2:757–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Matsuda DK, Gupta N, Martin HD. Closed intramedullary derotational osteotomy and hip arthroscopy for cam femoroacetabular impingement from femoral retroversion. Arthrosc Tech 2014;3:e83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ruecker AH, Rupprecht M, Gruber M et al. The treatment of intertrochanteric fractures: results using an intramedullary nail with integrated cephalocervical screws and linear compression. J of Orthop Trauma 2009;23:22–30. [DOI] [PubMed] [Google Scholar]
- 31. Goriainov V, Farook M, Vanhegan I et al. Tibial derotation osteotomies are effective in improving pain and function and avoiding hip arthroscopy in patients with hip pain—a short-term follow-up. J Hip Preservation Surg 2023;10:173–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


