Abstract
Background
Patients with nonshockable out-of-hospital cardiac arrest (OHCA) have poor outcomes compared with those with shockable rhythm. The optimal strategy for advanced airway management (AAM) for these patients remains controversial. This study aimed to compare outcomes between prehospital endotracheal intubation (ETI) and supraglottic airway (SGA) for adults with witnessed and nonshockable OHCA.
Methods
We compared the outcomes according to airway management using a nationwide, population-based Japanese registry (All-Japan Utstein Registry) between 2005 and 2021. The study population included adults with witnessed, nontraumatic, nonshockable OHCA who received prehospital AAM by emergency medical service (EMS) personnel. The outcomes were return of spontaneous circulation (ROSC), 1-month overall survival, and 1-month survival with a favorable neurological outcome, defined as a Cerebral Performance Category score of 1 or 2. To adjust for confounding factors between the ETI and SGA groups, we used propensity score analysis with inverse probability of treatment weighting (IPTW) and performed a sensitivity analysis using overlap weighting.
Results
A total of 147,088 patients were included: 30,797 (20.9%) received ETI and 116,291 (79.1%) received SGA. After IPTW adjustment, patients receiving ETI had significantly higher rates of ROSC (19.3% vs. 11.1%; odds ratio [OR] 1.51; 95% confidence interval [CI] 1.48–1.54), 1-month survival (6.4% vs. 4.5%, OR 1.44; 95%CI 1.40–1.49), and 1-month survival with favorable neurological outcomes (1.0% vs. 1.0%, OR 1.11; 95%CI 1.04–1.20) than those receiving SGA. The sensitivity analysis confirmed robust associations for ROSC (OR 1.53; 95%CI 1.45–1.61) and 1-month survival (OR 1.48; 95%CI 1.36–1.60), but the association with favorable neurological outcome was not statistically significant (OR 1.11; 95%CI 0.93–1.34).
Conclusion
In this Japanese nationwide Utstein registry cohort study with IPTW adjustment, for adult witnessed OHCA patients with initial nonshockable rhythm, prehospital ETI was associated with significantly higher rates of ROSC and 1-month survival, compared to prehospital SGA. These findings suggest that ETI, when performed by EMS personnel, has the potential to improve outcomes in these patients with OHCA.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12873-025-01341-6.
Keywords: Out-of-hospital cardiac arrest, Nonshockable rhythm, Advanced airway management, Endotracheal intubation, Supraglottic airway, Prehospital, Emergency medical services
Introduction
Out-of-hospital cardiac arrest (OHCA) is a major public health burden worldwide. In 2010, Berdowski et al. reported that emergency medical service (EMS) treated OHCA occurred in 87.4, 96.5, 65.4, and 108.9 cases per 100,000 person-years in Europe, North America, Asia, and Australia, respectively [1]. A recent report has indicated that OHCA occurred in 143,507 adult patients and had a high incidence, occurring in 88.8 patients per 100,000 person-years annually in the United States [2]. Moreover, most adult patients with OHCA had an initial nonshockable rhythm (74.4%), and approximately 52.2% had an initial asystole rhythm [2].
Despite intensive efforts by the EMS over many years, adult patients with OHCA have a low survival rate to hospital discharge (9.3%) [2]. The outcomes of patients with OHCA treated by EMS vary according to the initial cardiac rhythm [2–5]. Patients with an initial nonshockable rhythm (pulseless electrical activity or asystole) have worse survival rates to hospital discharge than those with an initial shockable rhythm (ventricular fibrillation or pulseless ventricular tachycardia) [2–5]. The initial nonshockable rhythm is independently associated with worse outcomes in patients with OHCA [6]. The database of the United States indicated that the survival rates to hospital discharge were 26.6% and 5.7% in shockable and nonshockable rhythms, respectively [2]. A systematic review and meta-analysis revealed that the survival rates to hospital discharge or at 30 days were 20% and 6% in shockable and nonshockable rhythms, respectively, even among patients with EMS-witnessed OHCA [7]. Therefore, improving outcomes in OHCA with nonshockable rhythms is a major challenge worldwide.
Advanced airway management (AAM) and epinephrine administration can be performed simultaneously while continuing high-quality cardiopulmonary resuscitation (CPR) in the prehospital situation [8]. Globally, guidelines recommend AAM for OHCA during CPR [9–11]; however, the survival benefits of management are still controversial in OHCA. Although some studies have reported survival benefits regarding prehospital AAM, others have reported poor outcomes [12–17]. Actually, AAM can provide optimal oxygenation and airway protection in the early stages of CPR [18]. In contrast, positive pressure ventilation and technical errors in AAM can result in a reduction in the quality of chest compression and worsen OHCA outcomes [19, 20]. Based on the constructive controversy, AAM has been the focus of clinical research and device development in recent years, with the potential to complement existing strategies for patients with OHCA treated EMS.
AAM commonly consists of manual maneuvers with a bag-valve-mask (BVM), endotracheal intubation (ETI), and supraglottic airway (SGA) [21]. In addition, SGA devices include the laryngeal tube (LT), laryngeal mask, i-Gel, and combi-tube [22, 23]. ETI has long been considered the gold standard of AAM for patients with OHCA in most countries [24]. However, reports of ETI-related complications, including unrecognized esophageal intubation, iatrogenic hyperventilation, and aspiration pneumonia, have increased [25–27]. In addition, EMS personnel require proper training and competence in performing ETI [28]. Compared with ETI, SGA insertion is rapid, simple, and requires less training and has been gradually used despite its complications [22, 23].
In Japan, specially trained EMS personnel have been permitted to use ETI since 2004, which has gradually increased nationwide, and received instructions and training on the use [29]. In the cohort study conducted in Osaka Prefecture, Japan, in 2011, no difference in the outcome from witnessed OHCA was noted between ETI and SGA regardless of the initial rhythm [30]. In this current study, using the All-Japan Utstein Registry from 2005 to 2021, we evaluated the outcomes of witnessed adult patients with nonshockable OHCA according to AAM types (ETI versus SGA).
Methods
Study design and settings
This retrospective cohort study used data from the All-Japan Utstein Registry, as previously described [31]. In Japan, this registry is a prospective, population-based, nationwide registry of OHCA in which data are recorded with the internationally standardized Utstein template [32]. The cohort study was approved by the Wakayama Medical University Ethics Committee (Approval no. 4196, approved on July 16, 2024) and the Meiji University of Integrative Medicine Ethics Committee (Approval no. 2024-043, approved on January 30, 2025), and was performed in accordance with the Declaration of Helsinki. Due to the retrospective nature of the study and the use of publicly available de-identified data, the Wakayama Medical University Ethics Committee and the Meiji University of Integrative Medicine Ethics Committee waived the need of obtaining informed consent. This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines [33]. Data are available through the submission of a proposal and completion of a data usage agreement with the Fire and Disaster Management Agency of Japan.
Study participants
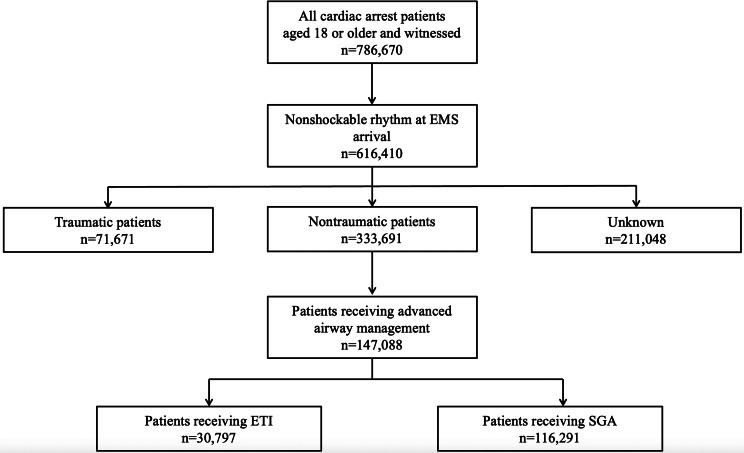
This retrospective cohort study enrolled 786,670 patients, aged ≥ 18 years who suffered from witnessed OHCA, recorded in the Utstein Registry between January 1, 2005, and December 31, 2021. Among them, data on 616,410 patients with an initial nonshockable rhythm at EMS arrival were extracted. Then, 282,719 patients with traumatic or unknown causes were excluded, and 333,691 patients with nontraumatic causes were selected (Fig. 1). To mitigate the impact of treatment bias and potential confounding in the direct comparisons between patients who underwent ETI and those who underwent SGA, we excluded patients who did not receive prehospital AAM, and 147,088 were included in the primary analysis.
Fig. 1.
Flowchart of the study population
Study variables
The following variables were analyzed: age, sex, origin of arrest, place of occurrence, witness status, presence and type of bystander CPR, bystander automated external defibrillator (AED) use, first documented rhythm on EMS personnel arrival, interventions of EMS personnel (defibrillation, types of AAM, and epinephrine administration), and the time from collapse to arrival of EMS [31, 32]. The All-Japan Utstein Registry records SGA use with information on device type, including laryngeal tube and laryngeal mask airway. Information on the i-Gel is incorporated into the category of laryngeal mask. However, the registry does not capture whether ETI was performed using video or direct laryngoscopy. Moreover, the datasets included outcome measures, such as the return of spontaneous circulation (ROSC), 1-month overall survival, and 1-month survival with favorable neurological outcomes. Neurological outcomes were evaluated according to the Glasgow Cerebral Performance Categories (CPC) scale. Patients with CPC 1 or 2 were considered to have favorable neurological outcomes [31].
EMS system in Japan
The EMS personnel are highly trained in all aspects of prehospital emergency care and treat cardiac arrest based on the Japanese CPR guidelines [34]. EMS teams are not allowed to terminate resuscitation in the field unless postmortem signs such as rigor mortis or lividity are evident. In particular, certified personnel with advanced training are allowed to insert an intravenous line, administer adrenaline, and conduct ETI for patients with OHCA. With online medical guidance by a physician, they are permitted to perform these emergency life-saving technicians. Moreover, medical control is established as a regionally structured protocol for these technicians. During the COVID-19 pandemic, infection control notices were issued in Japan; however, there were no changes to the protocol regarding the selection of AAM methods.
In accordance with international recommendations, adrenaline administration for nonshockable OHCA is indicated without delay, and this practice is also followed in Japan [34]. However, Japan’s EMS protocol limits intravenous access attempts to a maximum of two. Consequently, vascular access is not always achieved before hospital arrival, preventing epinephrine administration in some cases.
Exposure and outcome measures
The main exposure was prehospital ETI or SGA by EMS personnel. The primary study outcome was 1-month survival with favorable neurological outcomes. The secondary outcomes were 1-month overall survival and ROSC.
Statistical analyses
In this analysis, 147,088 patients receiving AAM were divided into two subcohorts: ETI and SGA. Continuous variables are reported as means, and categorical variables are reported as counts and proportions. Standardized mean differences were calculated to determine differences in baseline patient characteristics.
Inverse probability of treatment weights (IPTW), which were calculated from the propensity score (PS) for ETI, was used to adjust for confounding factors. IPTW analysis was applied to the multiply imputed datasets using the within-imputation method [35], wherein PS estimation and weighted outcome modeling were conducted separately for each dataset and subsequently combined using standard methods. PS was estimated through conditional logistic regression on the covariates. These covariates included age, sex, bystander CPR, initial rhythm, administration of epinephrine, and the time from collapse to EMS arrival, consistent with the variables listed in Table 1. To evaluate the ability of the model to predict ETI, the C-statistic was calculated as the area under the receiver operating characteristic curve. To evaluate the balance of the baseline covariates between the two groups, absolute standardized differences were computed, with a threshold of < 25% considered acceptable [36]. Following the generation of the IPTW cohorts, weighted logistic regression analyses were conducted to compare the outcomes between the ETI and SGA groups: logistic regression analyses were performed for binary outcomes. OR and standard errors were calculated using Rubin’s rules [37].
Table 1.
Demographic and clinical characteristics of all patients and propensity-score inverse probability of treatment weighted patients
| Before Weighting | After Weighting | |||||
|---|---|---|---|---|---|---|
| ETI (N = 30,797) | SGA (N = 116,291) | SMD | ETI (N = 28,285) | SGA (N = 115,529) | SMD | |
| Age, median, year | 79.9 | 77.1 | 0.061 | 78.0 | 77.6 | 0.012 |
| Sex, female, N (%) | 13,664 (46) | 48,373 (43) | 0.215 | 13,539 (44) | 49,058 (43) | 0.026 |
| Implementation of bystander CPR, N (%) | 14,578 (41) | 63,068 (47) | -0.115 | 13,263 (46) | 51,503 (45) | 0.013 |
| Asystole as initial rhythm on EMS arrival, N (%) | 17,534 (57) | 59,860 (51) | 0.112 | 16,871 (54) | 61,568 (52) | 0.053 |
| Administration of Epinephrine, N (%) | 16,291 (54) | 59,145 (50) | 0.098 | 13,155 (43) | 61,637 (53) | -0.203 |
| Collapse-EMS arrival, median, (seconds) | 799.6 | 757.8 | 0.038 | 800.0 | 760.0 | 0.036 |
| EMS arrival-AAM, median, (seconds) | 600.0 | 540.0 | ||||
Characteristics of the included patients in the cohort data. Data are presented as N (%) or median (interquartile range)
Abbreviation: CPR: cardiopulmonary resuscitation; EMS: emergency medical service; ETI: endotracheal intubation; N: number; SMD: Standardized mean difference; SGA: supraglottic airway
By stratifying patients into two groups based on the year, the subgroup analysis was performed to investigate whether the effect of ETI interacted with the outcomes. Weighted logistic regression analyses for the outcomes were performed using identical covariates.
For the sensitivity analysis, overlap weighting of the PS was applied as an alternative to IPTW to balance the baseline characteristics [38, 39]. The overlap weighting estimate represents the average treatment effect within the overlap population, comprising patients with a realistic likelihood of receiving either treatment. This method ensures an exact balance in the mean of all measured covariates [39].
All statistical analyses and data visualization were performed using R statistical software version 4.1.0 (The R Foundation for Statistical Computing, Vienna, Austria) and Stata/MP 16.0 (StataCorp, College Station, TX, USA). All p-values were two-sided, with p < 0.05 considered significant.
Results
In this study, 147,088 eligible patients who were treated with AAM by ESM personnel were analyzed and categorized into two distinct groups: 30,797 patients (20.9%) with ETI (ETI group) and 116,291 patients (79.1%) with SGA (SGA group). The mean ages of the ETI and SGA groups were 79.9 and 77.1 years, and female patients were 13,664 (46%) and 48,373 (43%), respectively. Moreover, we focused on the year of AAM implementation for patients with OHCA. Before matching, the mean time between EMS arrival and AAM was 1,200 s in the early (2005–2012) years and 626 s in the later (2013–2021) years (p < 0.001). Patients with OHCA in the ETI group were unlikely to receive bystander CPR and were likely to be female and receive epinephrine administration. Table 1 shows the patient demographics and clinical characteristics before and after the IPTW. The C-statistic was 0.605 in the PS models. The IPTW indicated that the patient distributions were well-balanced between the groups. Among the covariates used from the cohort, missing values ranged from 5.7 to 23.8% (Supplemental Table 1).
After imputing the missing data, the outcomes by the type of advanced airway are shown in Table 2. The proportions of the ROSC in the ETI and SGA groups were 19.3% and 11.1%, respectively. The proportions of 1-month survival of the ETI and SGA groups were 6.4% and 4.5%, respectively. The proportions of 1-month survival with favorable neurological outcomes in the ETI and SGA groups were 1.0% and 1.0%, respectively. The ETI group exhibited significantly higher rates of ROSC (OR, 1.51; 95% CI, 1.48–1.54), 1-month overall survival (OR, 1.44; 95% CI, 1.40–1.49), and 1-month survival with favorable neurological outcomes (OR, 1.11; 95% CI, 1.04–1.20). Table 3 indicates the results of the sensitivity analysis. The overlap weighting of the PS confirmed the relationship of ETI with ROSC (OR, 1.53; 95% CI, 1.45–1.61) and 1-month overall survival (OR, 1.48; 95% CI, 1.36–1.60). The relationship between the ETI group with 1-month survival and favorable neurological outcomes was not significant (OR, 1.11; 95% CI, 0.93–1.34).
Table 2.
Outcomes among endotracheal intubation versus supraglottic airway after propensity-score inverse probability of treatment weighted logistic regression analyses
| Overall (N = 147,088) | ETI (N = 30,797) | SGA (N = 116,291) | Odds ratio (95%CI) (IPW)* | |
|---|---|---|---|---|
| ROSC, N (%) | 18,895 (12.8) | 5,931 (19.3) | 12,964 (11.1) | 1.51 (1.48–1.54) |
| One-month Survival, N (%) | 7,238 (4.9) | 1,986 (6.4) | 5,252 (4.5) | 1.44 (1.40–1.49) |
| CPC score 1 or 2, N (%) | 1,508 (1.0) | 307 (1.0) | 1,201 (1.0) | 1.11 (1.04–1.20) |
Data are presented as N (%)
Abbreviations: CI: confidence interval; CPC: cerebral performance category; ETI: endotracheal intubation; ROSC: return of spontaneous circulation, SGA: supraglottic airway, IPW: inverse probability weighting. * IPW analysis was performed to balance the potential confounders
Table 3.
Outcomes among endotracheal intubation versus supraglottic airway after sensitivity analysis
| Odds ratio (95% confidence interval) | |
|---|---|
| ROSC | 1.53 (1.45–1.61) |
| One-month Survival | 1.48 (1.36–1.60) |
| CPC score 1 or 2 | 1.11 (0.93–1.34) |
Abbreviations: CPC: cerebral performance category; ROSC: return of spontaneous circulation
As for the year group, the differences in the effects of ETI on the outcomes were observed between the early (2005–2012) and later (2013–2021) years (Table 4). In the early years, although a significantly higher ROSC rate was observed (OR, 1.26; 95% CI, 1.21–1.30), no significant differences were detected in 1-month overall survival (OR, 1.03; 95% CI, 0.98–1.08) or 1‐month survival with favorable neurological outcomes (OR, 1.00; 95% CI, 0.91–1.10). Meanwhile, in the later years, the ETI group exhibited better outcomes consistent with the primary analyses for ROSC (OR, 1.54; 95% CI, 1.50–1.59), 1‐month overall survival (OR, 1.62; 95% CI, 1.55–1.70), and 1‐month survival with favorable neurological outcomes (OR, 1.17; 95% CI, 1.05–1.31).
Table 4.
Outcomes according to the year of advanced airway management implementation
| Odds ratio (95% confidence interval) | ||
|---|---|---|
| 2005–2012 years | 2013–2021 years | |
| ROSC | 1.26 (1.21–1.30) | 1.54 (1.50–1.59) |
| One-month Survival | 1.03 (0.98–1.08) | 1.62 (1.55–1.70) |
| CPC score 1 or 2 | 1.00 (0.91–1.10) | 1.17 (1.05–1.31) |
Abbreviations: CPC: cerebral performance category; ROSC: return of spontaneous circulation
Discussion
This observational study using the All-Japan Utstein Registry focused on adult patients with witnessed nontraumatic OHCAs and nonshockable rhythms on EMS arrival and assessed the difference between ETI and SGA outcomes. Patients with OHCA receiving ETI in the prehospital setting exhibited favorable outcomes than those receiving SGA.
In 2011, a prospective Utstein-style population cohort database conducted in Osaka, Japan, showed that these devices were not significant predictors of OHCA outcomes regardless of the initial rhythms [30]. Two multicenter randomized control trials (RCTs) of AAM for OHCA did not indicate a difference in the survival and neurological outcomes between ETI and SGA [23, 40]. An RCT by Wang et al. revealed that the initial LT insertion improved the 72-h survival compared with the initial ETI among adults with OHCA [22]. In two reports of systematic review and network meta-analysis, ETI did not contribute to improving survival to discharge compared with other devices for AAM [41, 42]. Furthermore, the subanalysis of the Target Temperature Management-2 trial showed that the choice of airway device, including ETI and SGA, was not independently associated with the outcomes of adult patients with OHCA [43]. In this study, the positive effect of ETI for OHCA did not align with these reports but may be due to focusing on some variables such as witnessed and initial nonshockable rhythm in the prehospital setting.
Some studies, including a meta-analysis, have indicated that compared with SGA, ETI is positively associated with outcomes among adults with OHCA [21, 44]. The ROC PRIMED study, a prospective clinical trial conducted in the North America, revealed the superiority of ETI over SGA in adult and nontraumatic OHCAs [21]. At that time, the Ministry of Health, Labour and Welfare issued a directive stating that ETI should be performed only in cases where SGA was ineffective or where ETI was expected to provide superior airway management [45]. As a result, patients who underwent ETI in the early period may have included those in whom SGA was not feasible or who had already experienced failed SGA attempts, introducing potential selection bias against ETI. More than 10 years have passed since this report of the Osaka registry, and prehospital medical care in Japan has changed. In our country, specially trained and certified EMS personnel have been permitted to perform ETI under medical direction, although the regional protocol varies [46, 47], and the number has been increasing. Early and increased performance of AAM including ETI and SGA at the prefecture level improved neurologically favorable survival following OHCA [46, 47]. Notably, even in the PS matching for OHCA, AAM was associated with favorable outcomes among patients with nonshockable rhythms [48]. However, SGA was preferred because of the low ETI success rate in these studies. In the RCT by Wang et al., the rate of unsuccessful first insertion was significantly higher in the ETI group (44.1%) than in the LT group (11.8%) [22]. For OHCAs receiving ETI attempts, the cumulative success rates for the first three attempts were 69.9%, 84.9%, and 89.9%, respectively, and the overall success rate was 91.8% after three attempts [49]. In this study, during prehospital CPR, conducting ETI improved the outcomes of nonshockable OHCA regardless of the timing and attempt. Moreover, high PaO2 and PaCO2 ≤ 45 mmHg by ETI were associated with favorable outcomes following OHCA [50, 51]. Therefore, the higher success of ETI by EMS personnel is needed for adequate training and practice, as in previous reports [52, 53].
For patients with OHCA, the use of a video laryngoscope for ETI during CPR was associated with better neurological outcomes than with a direct laryngoscope [54]. In addition, an observational study in Hiroshima (Japan) and the meta-analysis have recently shown that the video laryngoscope was associated with first-pass success for patients with OHCA; however, no differences in survival outcomes were found between the two approaches [55, 56]. The improvement in portability and price reduction led to the worldwide use of video laryngoscopy to assist ETI and promote effectiveness and safety. Therefore, the use of video laryngoscopy for OHCA is suggested to offer a promising option. Indeed, our subanalyses indicated that the ETI group in the later years shortened the mean time between EMS arrival and AAM and improved favorable outcomes compared with that in the early years. The improvement in outcomes observed in the later years may reflect not only enhanced EMS training systems but also the increasing adoption of video laryngoscopy, which has been reported to improve first-pass success during CPR [55, 56]. Unfortunately, the registry does not include data on laryngoscopy type, so stratified analyses could not be performed. The wide dissemination of video laryngoscopy for each team of Japanese EMS is important to increase the success rate of ETI and the survival rate of patients with OHCA.
In our study, the relatively low rate (54% in the ETI group and 50% in the SGA group) of epinephrine administration in the nonshockable OHCA is likely attributable to procedural constraints within Japan’s EMS system, where intravenous access attempts are limited to two per patient. Moreover, in Japan, vascular access placed by EMS personnel is not permitted via intraosseous route [31]. This can result in failed vascular access before hospital arrival, even when epinephrine is indicated. Similarly, a population-based study from the Osaka Utstein Registry reported that intravenous access was attempted in 42.0% of non-ventricular fibrillation cohort and succeeded in 45.7% of attempts (ventricular fibrillation cohort: 51.2% attempted; 53.5% successful among attempts) [57]. These findings should be interpreted in the context of Japan’s unique EMS system, which differs from those of other countries.
The interval in our study from EMS arrival to AAM attempt (median times: 600 s for ETI and 540 s for SGA) appears relatively longer than in a previous study, which reported the time from arrival to AAM as approximately 8 min for ETI and 6.5 min for SGA [30]. That study was conducted using the Osaka Utstein Registry database, reflecting Japan’s major metropolitan areas with a well-developed EMS system, whereas our study employed a nationwide database that also included rural regions. In addition, delays in AAM may have occurred in some cases due to EMS resource constraints and regional protocols that prioritize uninterrupted chest compressions [31]. These factors, inherent to Japan’s EMS system, likely contributed to the longer time to AAM observed in our study and should be considered when comparing our findings with those from other EMS systems. Importantly, prior research has suggested that survival outcomes may be adversely affected when the time to advanced airway exceeds 15 min [13]. Given that the median interval in our study was considerably shorter than this threshold, it is unlikely that the observed delay substantially altered our results. Nevertheless, our findings may not be directly generalizable to EMS systems operating under different regulatory and training frameworks, and extrapolation should be made with caution.
Limitations
This observational cohort study has several limitations. First, this study did not compare adults receiving AAM with those receiving BVM. Although previous studies have shown that BVM was associated with favorable outcomes compared with AAM, including ETI and SGA [15], the comparison between AAM and BVM is now controversial. The current 2024 AHA guidelines recommend both BVM and AAM for adult OHCA in the prehospital setting [58]. In this study, the effect of ETI relative to SGA for them was evaluated. Second, the choice of AAM techniques varied according to the local medical direction and EMS experience in Japan. Therefore, selection bias may occur in the AAM implementation content between regions. Third, the exact confounding variables could not be clarified because our database lacks detailed information such as intubation attempt counts, success rates, or complications. Moreover, whether ETI was performed using video or direct laryngoscopy were not recorded, limiting further device-specific analyses. This information could have potentially affected the outcomes. Fourth, the dataset analyzed did not include information regarding in-hospital interventions, such as induced targeted temperature management, extracorporeal CPR, percutaneous coronary intervention, and administration of some drugs [59]. These interventions may have contributed to the outcomes observed, but prior evidence suggests that excluding such patients does not materially change the associations [60].
Future registry iterations should incorporate such variables to enable a more comprehensive evaluation of the continuum of care from prehospital to in-hospital settings.
Conclusion
For adults with witnessed nontraumatic OHCA, the ETI strategy was positively associated with outcomes in nonshockable rhythms on EMS arrival. In Japan, improving training and protocols so that ETI can be performed accurately and quickly may improve outcomes for OHCA with nonshockable rhythms. Future studies on global cohort and RCT are required to address the impact of ETI for such patients.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Enago (www.enago.jp) for their assistance with English language editing.
Abbreviations
- OHCA
Out-of-Hospital Cardiac Arrest
- EMS
Emergency Medical Service
- AAM
Advanced Airway Management
- CPR
Cardiopulmonary Resuscitation
- BVM
Bag-Valve-Mask
- ETI
Endotracheal Intubation
- SGA
Supraglottic Airway
- LT
Laryngeal Tube
- AED
Automated External Defibrillator
- ROSC
Return of Spontaneous Circulation
- CPC
Cerebral Performance Categories
- IPTW
Inverse probability of treatment weights
- PS
Propensity score
- RCT
Randomized control trial
Author contributions
MN, AK, and ST contributed to study conception and design, and drafted the manuscript; MN, MU, AK and ST collected the data; AK, KK, TN, RH, SI, and MH contributed to methodology development; MN, MU, AK, and ST analyzed and interpreted the data; KK, TN, RH, SI, and MH provided supervision, critically reviewed the manuscript, and gave final approval. All the authors reviewed and approved the final version of the manuscript.
Funding
This work was supported by the JSPS KAKENHI (grant number: 23K07865) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan and 2023 Wakayama Medical University Special Grant-in-Aid for Research Projects (grant number: K23TS03).
Data availability
The datasets used and analyzed in this study are available from the corresponding author (Shinobu Tamura, stamura@wakayama-med.ac.jp) upon reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Wakayama Medical University Ethics Committee (Approval no. 4196, approved on July 16, 2024) and the Meiji University of Integrative Medicine Ethics Committee (Approval no. 2024-043, approved on January 30, 2025). The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. The requirement for informed consent was waived due to the retrospective design of the study and the use of use of publicly available de-identified data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Berdowski J, Berg RA, Tijssen JGP, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–87. 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Martin SS, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL et al. Heart disease and stroke statistics: A report of US and global data from the American Heart Association. Circulation. 2024;149:e347–e913. 10.1161/CIR.0000000000001209. [DOI] [PMC free article] [PubMed]
- 3.Liu N, Liu M, Chen X, Ning Y, Lee JW, Siddiqui FJ, et al. Development and validation of an interpretable prehospital return of spontaneous circulation (P-ROSC) score for patients with out-of-hospital cardiac arrest using machine learning: A retrospective study. EClinicalmedicine. 2022;48:101422. 10.1016/j.eclinm.2022.101422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grunau B, Reynolds JC, Scheuermeyer FX, Stenstrom R, Pennington S, Cheung C, et al. Comparing the prognosis of those with initial shockable and non-shockable rhythms with increasing durations of CPR: informing minimum durations of resuscitation. Resuscitation. 2016;101:50–6. 10.1016/j.resuscitation.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 5.Ishii J, Nishikimi M, Ohshimo S, Shime N. The current discussion regarding end-of-life care for patients with out-of-hospital cardiac arrest with initial non-shockable rhythm: A narrative review. Med (Kaunas). 2024;60:533. 10.3390/medicina60040533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 7.Gowens P, Smith K, Clegg G, Williams B, Nehme Z. Global variation in the incidence and outcome of emergency medical services witnessed out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2022;175:120–32. 10.1016/j.resuscitation.2022.03.026. [DOI] [PubMed] [Google Scholar]
- 8.Carlson JN, Colella MR, Daya MR, De Maio J, Nawrocki V, Nikolla P. Prehospital cardiac arrest airway management: an NAEMSP position statement and resource document. Prehosp Emerg Care. 2022;26(sup1):54–63. 10.1080/10903127.2021.1971349. [DOI] [PubMed] [Google Scholar]
- 9.Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–468. 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 10.Kiguchi T, Okubo M, Nishiyama C, Maconochie I, Ong MEH, Kern KB, et al. Out-of-hospital cardiac arrest across the world: first report from the international liaison committee on resuscitation (ILCOR). Resuscitation. 2020;152:39–49. 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 11.Semeraro F, Greif R, Böttiger BW, Burkart R, Cimpoesu D, Georgiou M, et al. Guidelines. European resuscitation Council guidelines 2021: systems saving lives. Resuscitation. 2021;161:80–97. 10.1016/j.resuscitation.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Shimizu K, Wakasugi M, Kawagishi T, Hatano T, Fuchigami T, Okudera H. Effect of advanced airway management by paramedics during out-of-hospital cardiac arrest on chest compression fraction and return of spontaneous circulation. Open Access Emerg Med. 2021;13:305–10. 10.2147/OAEM.S319385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okubo M, Komukai S, Izawa J, Gibo K, Kiyohara K, Matsuyama T, et al. Timing of prehospital advanced airway management for adult patients with out-of-hospital cardiac arrest: A nationwide cohort study in Japan. J Am Heart Assoc. 2021;10:e021679. 10.1161/JAHA.121.021679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMullan J, Gerecht R, Bonomo J, Robb R, McNally B, Donnelly J, et al. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation. 2014;85:617–22. 10.1016/j.resuscitation.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Hasegawa K, Hiraide A, Chang Y, Brown DF. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309:257–66. 10.1001/jama.2012.187612. [DOI] [PubMed] [Google Scholar]
- 16.Hanif MA, Kaji AH, Niemann JT. Advanced airway management does not improve outcome of out-of-hospital cardiac arrest. Acad Emerg Med. 2010;17:926–31. 10.1111/j.1553-2712.2010.00829.x. [DOI] [PubMed] [Google Scholar]
- 17.Oh YS, Ahn KO, Shin SD, Kagino K, Nishiuchi T, Ma M, et al. Variability in the effects of prehospital advanced airway management on outcomes of patients with out-of-hospital cardiac arrest. Clin Exp Emerg Med. 2020;7:95–106. 10.15441/ceem.19.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang HE, Simeone SJ, Weaver MD, Callaway CW. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Ann Emerg Med. 2009;54:645–e6521. 10.1016/j.annemergmed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 19.Benoit JL, Prince DK, Wang HE. Mechanisms linking advanced airway management and cardiac arrest outcomes. Resuscitation. 2015;93:124–7. 10.1016/j.resuscitation.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Studnek JR, Thestrup L, Vandeventer S, Ward SR, Staley K, Garvey L, et al. The association between prehospital endotracheal intubation attempts and survival to hospital discharge among out-of-hospital cardiac arrest patients. Acad Emerg Med. 2010;17:918–25. 10.1111/j.1553-2712.2010.00827.x. [DOI] [PubMed] [Google Scholar]
- 21.Andersen LW, Granfeldt A. Pragmatic airway management in out-of-hospital cardiac arrest. JAMA. 2018;320:761–3. 10.1001/jama.2018.10824. [DOI] [PubMed] [Google Scholar]
- 22.Wang HE, Schmicker RH, Daya MR, Stephens SW, Idris AH, Carlson JN, et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2018;320:769–78. 10.1001/jama.2018.7044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benger JR, Kirby K, Black S, Brett SJ, Clout M, Lazaroo MJ, et al. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac arrest on functional outcome: the AIRWAYS-2 randomized clinical trial. JAMA. 2018;320:779–91. 10.1001/jama.2018.11597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, et al. European resuscitation Council guidelines 2021: adult advanced life support. Resuscitation. 2021;161:115–51. 10.1016/j.resuscitation.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 2008;34:1835–42. 10.1007/s00134-008-1205-6. [DOI] [PubMed] [Google Scholar]
- 26.Aufderheide TP, Lurie KG. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32:S345–51. 10.1097/01.ccm.0000134335.46859.09. [DOI] [PubMed] [Google Scholar]
- 27.Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32–7. 10.1067/mem.2001.112098. [DOI] [PubMed] [Google Scholar]
- 28.Kunkes T, Makled B, Norfleet J, Schwaitzberg S, Cavuoto L. Understanding the cognitive demands, skills, and assessment approaches for endotracheal intubation: cognitive task analysis. JMIR Perioper Med. 2022;5:e34522. 10.2196/34522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tanigawa K, Shigematsu A. Choice of airway devices for 12,020 cases of nontraumatic cardiac arrest in Japan. Prehosp Emerg Care. 1998;2:96–100. 10.1080/10903129808958850. [DOI] [PubMed] [Google Scholar]
- 30.Kajino K, Iwami T, Kitamura T, Daya M, Ong ME, Nishiuchi T, et al. Comparison of supraglottic airway versus endotracheal intubation for the pre-hospital treatment of out-of-hospital cardiac arrest. Crit Care. 2011;15(R236). 10.1186/cc10483. [DOI] [PMC free article] [PubMed]
- 31.Kubo A, Hiraide A, Shinozaki T, Shibata N, Miyamoto K, Tamura S, et al. Impact of epinephrine on neurological outcomes in out-of-hospital cardiac arrest after automated external defibrillator use in Japan. Sci Rep. 2025;15:274. 10.1038/s41598-024-84950-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, International Liaison Committee on Resuscitation (American Heart Association. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385–97. 10.1161/01.CIR.0000147236.85306.15 [DOI] [PubMed]
- 33.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7. 10.1016/S0140-6736(07)61602-X. (2007). [DOI] [PubMed] [Google Scholar]
- 34.Japan Resuscitation Council. JRC guidelines for resuscitation 2020 (Tokyo: Igaku-Shoin. 2021) [in Japanese], Available from: https://www.jrc-cpr.org/jrc-guideline-2020/
- 35.Granger E, Sergeant JC, Lunt M. Avoiding pitfalls when combining multiple imputation and propensity scores. Stat Med. 2019;38:5120–32. 10.1002/sim.8355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25:1–21. 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10:585–98. 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 38.Li F, Thomas LE, Li F. Addressing extreme propensity scores via the overlap weights. Am J Epidemiol. 2019;188:250–7. 10.1093/aje/kwy201. [DOI] [PubMed] [Google Scholar]
- 39.Thomas LE, Li F, Pencina MJ. Overlap weighting: A propensity score method that mimics attributes of a randomized clinical trial. JAMA. 2020;323:2417–8. 10.1001/jama.2020.7819. [DOI] [PubMed] [Google Scholar]
- 40.Lee AF, Chien YC, Lee BC, Yang WS, Wang YC, Lin HY, et al. Effect of placement of a supraglottic airway device vs endotracheal intubation on return of spontaneous circulation in adults with out-of-hospital cardiac arrest in taipei, taiwan: A cluster randomized clinical trial. JAMA Netw Open. 2022;5:e2148871. 10.1001/jamanetworkopen.2021.48871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.White L, Melhuish T, Holyoak R, Ryan T, Kempton H, Vlok R. Advanced airway management in out of hospital cardiac arrest: A systematic review and meta-analysis. Am J Emerg Med. 2018;36:2298–306. 10.1016/j.ajem.2018.09.045. [DOI] [PubMed] [Google Scholar]
- 42.Lou J, Tian S, Kang X, Lian H, Liu H, Zhang W, et al. Airway management in out-of-hospital cardiac arrest: A systematic review and network meta-analysis. Am J Emerg Med. 2023;65:130–8. 10.1016/j.ajem.2022.12.029. [DOI] [PubMed] [Google Scholar]
- 43.Battaglini D, Schiavetti I, Ball L, Jakobsen JC, Lilja G, Friberg H, et al. Association between early airway intervention in the prehospital setting and outcomes in out of hospital cardiac arrest patients: A post-hoc analysis of the target temperature Management-2 (TTM2) trial. Resuscitation. 2024;203:110390. 10.1016/j.resuscitation.2024.110390. [DOI] [PubMed] [Google Scholar]
- 44.Benoit JL, Gerecht RB, Steuerwald MT, McMullan JT. Endotracheal intubation versus supraglottic airway placement in out-of-hospital cardiac arrest: A meta-analysis. Resuscitation. 2015;93:20–6. 10.1016/j.resuscitation.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 45.Nakahara S, Nagao T, Nishi R, Sakamoto T. Task-shift model in Pre-hospital care and standardized nationwide data collection in japan: improved outcomes for Out-of-hospital cardiac arrest patients. JMA J. 2021;4:8–16. 10.31662/jmaj.2020-0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nakagawa K, Sagisaka R, Morioka D, Tanaka S, Takyu H, Tanaka H. The association of delayed advanced airway management and neurological outcome after out-of-hospital cardiac arrest in Japan. Am J Emerg Med. 2022;62:89–95. 10.1016/j.ajem.2022.10.010. [DOI] [PubMed] [Google Scholar]
- 47.Onoe A, Kajino K, Daya MR, Nakamura F, Nakajima M, Kishimoto M, et al. Improved neurologically favourable survival after OHCA is associated with increased pre-hospital advanced airway management at the Prefecture level in Japan. Sci Rep. 2022;12:20498. 10.1038/s41598-022-25124-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Izawa J, Komukai S, Gibo K, Okubo M, Kiyohara K, Nishiyama C, et al. Pre-hospital advanced airway management for adults with out-of-hospital cardiac arrest: nationwide cohort study. BMJ. 2019;364:l430. 10.1136/bmj.l430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang HE, Yealy DM. How many attempts are required to accomplish out-of-hospital endotracheal intubation? Acad Emerg Med. 2006;13:372–7. 10.1197/j.aem.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 50.Spindelboeck W, Schindler O, Moser A, Hausler F, Wallner S, Strasser C, et al. Increasing arterial oxygen partial pressure during cardiopulmonary resuscitation is associated with improved rates of hospital admission. Resuscitation. 2013;84:770–5. 10.1016/j.resuscitation.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 51.Nakayama R, Bunya N, Uemura S, Sawamoto K, Narimatsu E. Prehospital advanced airway management and ventilation for out-of-hospital cardiac arrest with prehospital return of spontaneous circulation: A prospective observational cohort study in Japan. Prehosp Emerg Care. 2024;28:470–7. 10.1080/10903127.2023.2260479. [DOI] [PubMed] [Google Scholar]
- 52.Dyson K, Bray J, Smith K, Bernard S, Finn J. A systematic review of the effect of emergency medical service practitioners’ experience and exposure to out-of-hospital cardiac arrest on patient survival and procedural performance. Resuscitation. 2014;85:1134–41. 10.1016/j.resuscitation.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 53.Murphy DL, Bulger NE, Harrington BM, Skerchak JA, Counts CR, Latimer AJ, et al. Fewer tracheal intubation attempts are associated with improved neurologically intact survival following out-of-hospital cardiac arrest. Resuscitation. 2021;167:289–96. 10.1016/j.resuscitation.2021.07.001. [DOI] [PubMed] [Google Scholar]
- 54.Risse J, Fischer M, Meggiolaro KM, Fariq-Spiegel K, Pabst D, Manegold R, et al. Effect of video laryngoscopy for non-trauma out-of-hospital cardiac arrest on clinical outcome: A registry-based analysis. Resuscitation. 2023;185:109688. 10.1016/j.resuscitation.2021.07.001. [DOI] [PubMed] [Google Scholar]
- 55.Santou N, Ueta H, Nakagawa K, Hata K, Kusunoki S, Sadamori T, et al. A comparative study of video laryngoscope vs macintosh laryngoscope for prehospital tracheal intubation in hiroshima, Japan. Resusc Plus. 2023;13:100340. 10.1016/j.resplu.2022.100340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chien YT, Ong JR, Tam KW, Loh EW. Video laryngoscopy and direct laryngoscopy for cardiac arrest: A meta-analysis of clinical studies and trials. Am J Emerg Med. 2023;73:116–24. 10.1016/j.ajem.2023.08.028. [DOI] [PubMed] [Google Scholar]
- 57.Fujii T, Kitamura T, Kajino K, Kiyohara K, Nishiyama C, Nishiuchi T, et al. Prehospital intravenous access for survival from out-of-hospital cardiac arrest: propensity score matched analyses from a population-based cohort study in osaka, Japan. BMJ Open. 2017;7:e015055. 10.1136/bmjopen-2016-015055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Greif R, Bray JE, Djärv T, Drennan IR, Liley HG, Ng KC, et al. 2024 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Resuscitation. 2024;205:110414. 10.1016/j.resuscitation.2024.110414. [DOI] [PubMed] [Google Scholar]
- 59.Chalkias A, Adamos G, Mentzelopoulos SD. General critical care, temperature control, and end-of-life decision making in patients resuscitated from cardiac arrest. J Clin Med. 2023;12:4118. 10.3390/jcm12124118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jabre P, Penaloza A, Pinero D, Duchateau FX, Borron SW, Javaudin F, et al. Effect of Bag-Mask ventilation vs endotracheal intubation during cardiopulmonary resuscitation on neurological outcome after Out-of-Hospital cardiorespiratory arrest: A randomized clinical trial. JAMA. 2018;319:779–87. 10.1001/jama.2018.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed in this study are available from the corresponding author (Shinobu Tamura, stamura@wakayama-med.ac.jp) upon reasonable request.