Abstract
Background
Nitrous oxide (N₂O) misuse has become increasingly prevalent among young adults in Vietnam, with growing reports of neurological complications.
Methods
We conducted a retrospective analysis of 35 patients with N₂O-induced neurotoxicity admitted to Bach Mai Hospital from 2022 to 2024.
Results
Patients were mostly female (65.7 %), median age 22, with students and office workers being the predominant occupations. Neurological symptoms included paresthesias (88.6 %), weakness (82.9 %), and unsteadiness (77.1 %). MRI revealed dorsal column lesions in 60 %. All patients received B12 therapy. Full recovery occurred in 91.4 %; 8.6 % had mild persistent symptoms.
Conclusions
N₂O misuse is an emerging threat in Vietnam. Despite favorable treatment outcomes, prevention through public education and policy is essential. Our findings contribute important local data to support future regulation and health promotion efforts.
Keywords: Nitrous oxide, Recreational drug use, Myeloneuropathy, Vitamin B12 deficiency, MRI dorsal column lesion, Public health policy, Vietnam
Highlights
-
•
First case series of nitrous oxide-induced myeloneuropathy in Vietnamese youth.
-
•
Majority of patients were students and office workers with high-dose daily exposure.
-
•
Neurological symptoms included paresthesia, weakness, and gait unsteadiness.
-
•
MRI revealed dorsal column lesions in 60 % of symptomatic patients.
-
•
Most patients recovered fully with timely vitamin B12 treatment.
1. Introduction
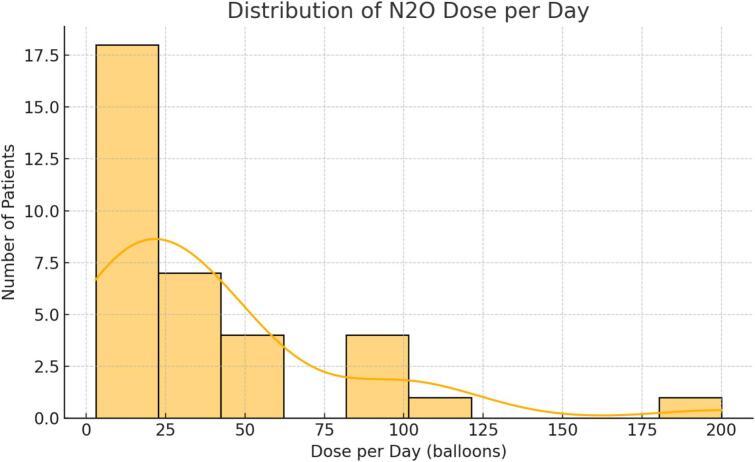
Nitrous oxide (N2O), also known as “laughing gas,” has historically been used for its anesthetic properties in medical and dental procedures. However, in recent years, its recreational use has surged globally, particularly among adolescents and young adults [1]. The appeal of N2O lies in its short-lived euphoria, easy availability, and misconception of being a “safe high” [2]. The growing trend of N2O misuse is especially notable in urban areas and among populations with access to nightlife, social media, and peer influence [3]. (See Fig. 1.) (See Table 1.)
Fig. 1.
Dose per day (balloons).
Table 1.
Demographic and clinical characteristics of patients (n = 35).
| Variable | Value |
|---|---|
| Age, median (IQR) | 22 (19–27) |
| Female sex (%) | 65.7 |
| Occupation: - Students - Office workers -Others |
33.4 31.4 35.2 |
| Duration of use (months) | 12 (6–36) |
| Daily dose >50 balloons | 34.3 % |
| Tingling | 88.6 % |
| Weakness | 82.9 % |
| Unsteady gait | 77.1 % |
| MRI dorsal lesion | 60 % |
| Full recovery | 91.4 % |
In Vietnam, the reports from poison control center and emergency department visits suggest a sharp increase in N2O intoxication cases, especially among students and young workers. However, epidemiological data remains sparse. The neurotoxicity of N2O stems from its interference with cobalamin (vitamin B12) metabolism, leading to functional B12 deficiency and resulting in demyelination, particularly of the dorsal spinal cord columns [4,5]. Clinically, this manifests as paresthesia, weakness, ataxia, and in severe cases, irreversible myelopathy [6,7].
A previous Vietnamese case series by Tuan et al. (2020) described 11 patients with nitrous oxide-induced subacute combined degeneration, providing initial insight into the clinical spectrum of N₂O neurotoxicity in Vietnam. However, their cohort was limited in size, and no demographic patterns or public health implications were discussed. While similar case series have been published from other Southeast Asian countries, the present report represents the most comprehensive Vietnamese dataset to date. As such, it provides not only clinical confirmation of dorsal column involvement and favorable response to B12 therapy, but also socio-occupational insights that may inform policy development and targeted education initiatives.
Despite the growing concern, few studies in Southeast Asia have described the clinical profile and usage patterns of N2O abusers. Existing literature mainly derives from Western countries, and cultural differences may affect both drug accessibility and treatment-seeking behavior [8]. Our study addresses this gap by analyzing a case series of 35 patients with confirmed N2O-associated neurological dysfunction in a Vietnamese young.
2. Methods
This retrospective study included 35 patients admitted to our Poison Control Center of at Bach Mai hospital in Hanoi, Vietnam, between January 2022 and March 2024. Patients were included if they had a history of recent N2O use and presented with neurological symptoms consistent with N2O-related neurotoxicity.
Data collected from medical records included age, sex, occupation, education level, duration and dose of N2O use, neurological symptoms (tingling, weakness, sensory loss, gait disturbances), MRI findings, and clinical outcome at discharge. MRI was performed in symptomatic patients. Outcome was categorized as full recovery or presence of sequelae.
Descriptive statistics were calculated using SPSS 27. Categorical variables were presented as percentages; continuous variables as medians with interquartile ranges.
3. Results
Among 35 patients, 23 (65.7 %) were female and the median age was 22 years (range: 15–46). Students (34.3 %) and office workers (31.4 %) were the most frequent occupations. Median use duration was 12 months (IQR: 6–36), and 34.3 % used >50 balloons/day.
Tingling or paresthesia was reported in 88.6 % of cases, muscle weakness in 82.9 %, and unsteady gait in 77.1 %. MRI was performed in 30 patients, with 21 (60 %) showing dorsal column lesions. All patients received vitamin B12 supplementation. At discharge, 32 patients (91.4 %) had recovered completely, while 3 (8.6 %) had persistent mild deficits.
Other occupations included service workers (e.g., baristas, delivery drivers) and unemployed individuals (collectively 35.2 %). Regarding education, 71.4 % had completed high school, 22.9 % had some college education, and 5.7 % had not completed secondary school.
The annual number of cases admitted for N₂O-related neurotoxicity increased over the study period: 7 in 2022, 13 in 2023, and 15 in the first quarter of 2024, suggesting a rising trend similar to other international reports. However, no official national data currently exists quantifying the prevalence or volume of nitrous oxide use in Vietnam, underscoring the need for population-level monitoring and surveillance.
4. Discussion
This case series builds on prior Southeast Asian studies documenting nitrous oxide-associated subacute combined degeneration [8], providing new insights specific to the Vietnamese context. With 35 patients over two years, this is the largest published cohort in Vietnam, reflecting both the rising incidence and sociocultural dynamics of N₂O use in this population. Patients were mostly young, female, and either students or white-collar workers—a trend that may reflect broader vulnerabilities in urban youth groups.
Our findings are broadly consistent with the earlier Vietnamese case series by Tuan et al. (Neurol Int, 2020), which documented N₂O-induced subacute combined degeneration in a smaller cohort of 11 patients [18]. While both studies observed common symptoms such as paresthesia and gait disturbance, our data provide a broader sociocultural context, highlighting occupation, education levels, and temporal trends, which were not emphasized previously. This reinforces the suggestion that N₂O abuse is spreading among urban youth, particularly students and lower-income service workers.
Unlike some European reports where usage is predominantly confined to nightlife settings, our cohort included patients with diverse usage environments, many reported solitary or home-based use. The lack of legal regulation and rising case numbers (from 7 in 2022 to 15 in the first quarter of 2024) suggest a growing problem. Regarding treatment, all patients received intramuscular hydroxocobalamin at a dose of 1000 μg daily for at least 7 days, followed by oral B12 supplementation. In 28 patients (80 %), symptoms improved significantly within 2 weeks. Follow-up was available in 29 cases (82.9 %), conducted via telephone or outpatient visits within 1–3 months post-discharge. Among them, 4 patients (13.8 %) reported intermittent residual symptoms such as numbness or fatigue. Three patients (8.6 %) admitted to reusing N₂O within 3 months, highlighting the need for better counseling and addiction support services.
Our findings are consistent with global reports on nitrous oxide (N₂O) abuse among youth, particularly in urban environments. In the UK, nearly 38 % of young adults aged 16–24 had reported using N₂O at least once, often unaware of its neurotoxicity [1]. Similarly, studies from the Netherlands and other European countries have highlighted increasing cases of N₂O-induced myeloneuropathy, especially among nightlife participants [2,9]. In China, Lin et al. documented a case series of N₂O-induced subacute combined degeneration, involving a slightly older demographic and often private use settings [8]. Compared to these settings, our cohort in Vietnam represents a notably younger population (median age: 22) with high representation among students and office workers. This reflects an early onset of recreational substance use, often influenced by peer groups and social trends [3].
The widespread misuse of N₂O in Vietnam can be attributed to several interrelated socio-cultural factors. First, a lack of clear legal regulation surrounding N₂O production, sale, and consumption allows easy access, particularly in urban nightlife settings. In contrast, the UK has already implemented restrictions under the Psychoactive Substances Act 2016, though misuse persists [17]. Second, health education programs on drug abuse remain limited in Vietnamese schools and universities. Most of our patients lacked awareness of the neurological consequences of N₂O use—a finding mirrored in international literature [3,6]. Misconceptions of N₂O as a “harmless” or “legal high” contribute to delayed presentation and diagnosis [2,4,5].
From a pathophysiological standpoint, the observed neurological deficits are largely due to oxidative inactivation of vitamin B12, resulting in demyelination of the spinal cord and peripheral nerves [4,5,13]. This mechanism explains the high rates of paresthesia, weakness, and gait disturbances observed in our study and others [6,7,11,12]. MRI findings, especially T2-weighted hyperintensity of the dorsal columns are consistent with subacute combined degeneration [14]. Our MRI data (60 % with dorsal column lesions) aligns closely with case series from Asia and Europe [8,14].
Importantly, most patients in our study responded well to high-dose vitamin B12 therapy, in agreement with existing case reports and reviews suggesting good recovery if treatment is timely [15,16]. However, 8.6 % had residual deficits, emphasizing the need for early intervention and public education.
Moving forward, multilevel interventions are urgently required. We recommend integrating drug education into secondary and tertiary school curricula, focusing on both legal and health risks. Educational materials should address the biochemical basis of N₂O-induced neurotoxicity, reinforcing that symptoms are not benign [6,13]. Furthermore, screening tools targeting high-risk groups, such as nightlife patrons or young adults with frequent use, should be implemented within community and clinical settings [10].
Finally, Our findings may serve as a valuable local foundation for initiating regulatory and public health responses. We echo prior calls for legal regulation of nitrous oxide sales and distribution, as implemented in other countries [17], and we stress the importance of integrating nitrous oxide education into school and university curricula. Tailored prevention programs could significantly reduce neurotoxicity burden among Vietnamese youth. A national surveillance and reporting system is also urgently needed to track trends and evaluate interventions over time.
4.1. Limitations
Limitations of this study include its retrospective nature and reliance on self-reported data for N₂O use and follow-up. Moreover, due to the absence of centralized surveillance data on N₂O consumption in Vietnam, we could not correlate our findings with national trends. Future prospective studies and government monitoring systems are necessary.
5. Conclusions
Recreational N2O use among Vietnamese youth is associated with a high risk of neurological complications. Despite generally favorable outcomes with treatment, prevention remains the key strategy. Public health authorities should prioritize awareness and regulatory measures to address this growing problem.
Authors contribution
-
•
Nguyen Dang Duc: Principal investigator, drafted and finalized the manuscript, corresponding author.
-
•
Nguyen Hong Anh Lam: Designed the study methodology, collected and entered data.
-
•
Dang Bach Nguyen: Performed data analysis and contributed to manuscript editing.
CRediT authorship contribution statement
Duc Nguyen Dang: Writing – review & editing, Writing – original draft, Supervision. Anh Lam Nguyen Hong: Investigation, Formal analysis. Bach Nguyen Dang: Software.
Informed consent
Written informed consent was obtained from all participants or their legal guardians prior to data collection and publication.
Ethical approval
This study was approved by the Ethics Committee of Bach Mai Hospital, Hanoi, Vietnam. All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Funding
This study received no external funding.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgments
The authors thank the clinical staff at the Poison Control Center, Bach Mai Hospital, for their assistance in patient care and data retrieval.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Kaar S.J., Ferris J., Waldron J., Devaney M., Ramsey J., Winstock A.R. Up: the rise of nitrous oxide abuse. an international survey of contemporary nitrous oxide use. J. Psychopharmacol. 2016 doi: 10.1177/0269881116632375. [DOI] [PubMed] [Google Scholar]
- 2.van Amsterdam J., Nabben T., van den Brink W. Recreational nitrous oxide use: prevalence and risks. Regul. Toxicol. Pharmacol. 2015 doi: 10.1016/j.yrtph.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Ehirim E.M., Naughton D.P., Petróczi A. No laughing matter: presence, consumption trends, drug awareness, and perceptions of “legal highs” on a UK university campus. J. Psychoactive Drugs. 2014 doi: 10.3389/fpsyt.2017.00312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Layzer R.B. Myeloneuropathy after prolonged exposure to nitrous oxide. Lancet. 1978 doi: 10.1016/s0140-6736(78)92101-3. [DOI] [PubMed] [Google Scholar]
- 5.Flippo T.S., Holder W.D., Jr. Neurologic degeneration associated with nitrous oxide anesthesia in patients with vitamin B12 deficiency. Arch. Surg. 1993 doi: 10.1001/archsurg.1993.01420240099018. [DOI] [PubMed] [Google Scholar]
- 6.Garakani A., Jaffe R.J., Savla D., Welch A.K., Protin C.A., Bryson E.O., McDowell D.M. Neurologic, psychiatric, and other medical manifestations of nitrous oxide abuse: a systematic review of the case literature. Am. J. Addict. 2016 doi: 10.1111/ajad.12372. [DOI] [PubMed] [Google Scholar]
- 7.Thompson A.G., Leite M.I., Lunn M.P., Bennett D.L. Whippits, nitrous oxide and the dangers of legal highs. Pract. Neurol. 2015 doi: 10.1136/practneurol-2014-001071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin R.J., Lin S.L., Wang C.H., Hsieh Y.C. Subacute combined degeneration of the spinal cord caused by nitrous oxide intoxication: a case series. Kaohsiung J. Med. Sci. 2020 [Google Scholar]
- 9.van Amsterdam J., Nabben T., van den Brink W. Recreational use of nitrous oxide: prevalence and risks. Regul. Toxicol. Pharmacol. 2015 doi: 10.1016/j.yrtph.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Garakani A., Welch A.K., Jaffe R.J. Neuropsychiatric and medical consequences of nitrous oxide abuse. Psychiatr. Clin. North Am. 2018 [Google Scholar]
- 11.Sedhom R., Shweikeh F., Ibrahim D. Nitrous oxide-induced myelopathy: a case report and review of the literature. Case Rep. Neurol. Med. 2019 [Google Scholar]
- 12.Richardson P.G. Peripheral neuropathy following nitrous oxide abuse. Emerg. Med. J. 2010 doi: 10.1111/j.1742-6723.2009.01262.x. [DOI] [PubMed] [Google Scholar]
- 13.Flippo T.S., Holder W.D. Neurologic degeneration associated with nitrous oxide. Arch. Surg. 1993 doi: 10.1001/archsurg.1993.01420240099018. [DOI] [PubMed] [Google Scholar]
- 14.Malhotra H.S., Gupta P., Prabhu H., et al. MRI findings in nitrous oxide-induced subacute combined degeneration. Neurol. India. 2016 [Google Scholar]
- 15.Jiang Y., Chen L., Ye Y., Wang L. Subacute combined degeneration due to nitrous oxide intoxication: a case report. Medicine (Baltimore) 2019 [Google Scholar]
- 16.Nogue E., Clavel M., Mégarbane B. Reversible myelopathy following nitrous oxide abuse. Clin. Toxicol. (Phila.) 2014 [Google Scholar]
- 17.UK Home Office . 2018. Review of the Psychoactive Substances Act 2016. [Google Scholar]
- 18.Tuan N.D., et al. Subacute combined degeneration due to nitrous oxide abuse: a case series from Vietnam. Neurol. Int. 2020;12(2):134–138. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.