Abstract
Background and aim
Strong and effective stewardship is a fundamental function of health systems. However, rehabilitation services often receive insufficient attention due to the limited priority assigned to them by governments and health systems. In many countries—particularly low- and middle-income nations—this neglect has resulted in fragmented and poorly coordinated rehabilitation services across various sectors, with inconsistent service delivery influenced by the internal policies of individual institutions. This study investigates the broader barriers to rehabilitation services, analyzes their implications for stewardship, and proposes solutions to improve governance and system coordination.
Method
In this scoping review of studies conducted in Iran and globally, we identified factors and strategies for effective stewardship of rehabilitation services using Arksey and O’Malley’s framework. Searches were performed in English databases (PubMed, Web of Science, and Scopus) and Persian databases (SID and Magiran), as well as the Google Scholar search engine, utilizing relevant English keywords and their Persian equivalents. Data were analyzed through a qualitative methodology employing directed content analysis. Additionally, Veillard et al.‘s Health System Stewardship Framework was utilized to identify and analyze the challenges and solutions implemented in other countries.
Findings
From a total of 38 published articles on rehabilitation services, six themes, eight sub-themes, 81 challenges, and 74 solutions were identified. The challenges included the ineffectiveness of the fragmented rehabilitation structure and stewardship, the absence of a comprehensive plan, and inadequate coordination and communication. Proposed solutions from these studies included establishing a central regulatory and governance body; developing rehabilitation services that recognize rehabilitation as a population-based strategy for health and well-being across a wide range of health conditions throughout the continuum of care and throughout life; and creating databases to track individuals with disabilities and the rehabilitation services provided to them.
Conclusion
Effective stewardship of integrated rehabilitation services necessitates service continuity, coordinated policymaking, and active stakeholder engagement. A cohesive governance structure, bolstered by a robust information system, is crucial for evidence-based decision-making. Aligning policies with operational plans fosters collaboration and improves service efficiency.
Keywords: Stewardship, Governance, Rehabilitation services, Scoping review
Introduction
Rehabilitation is a vital service for individuals with diverse health conditions, aimed at improving functionality and reducing disability. It empowers individuals to manage their conditions and adapt to daily life, thereby enhancing their participation in education, employment, and community activities. Rehabilitation provides substantial health, social, and economic benefits by promoting independence and overall well-being [1].
The increasing prevalence of non-communicable diseases (NCDs) and an aging population have made rehabilitation more essential than ever [2]. As access to healthcare interventions expands, the need for rehabilitation becomes critical to optimize their effectiveness. However, the global demand for rehabilitation services significantly exceeds their availability, resulting in a substantial unmet need that hinders the achievement of key health and development objectives, including the Sustainable Development Goals (SDGs). Specifically, SDG Goal 3 aims to ensure healthy lives and well-being for all, which necessitates comprehensive services, including rehabilitation, as part of Universal Health Coverage (UHC) [1, 3].
In many low- and middle-income countries, the unmet need for rehabilitation services is particularly acute. The lack of prioritization by health ministries, coupled with escalating health challenges such as aging populations, rising rates of NCDs, and increasing disability prevalence, exacerbates this issue [4]. According to the World Health Organization (WHO), over one billion people, or 15.6% of the global population, live with disabilities, with the majority residing in low- and middle-income countries. This trend is expected to continue, highlighting the urgent need for improved rehabilitation services worldwide [5].
To address this challenge, it is essential to strengthen the functions of health systems, as outlined by the WHO in its 2000 report. These functions—service provision, resource generation, financing, and stewardship—are vital for developing an integrated system that ensures the delivery of quality services, including rehabilitation [6]. Among these functions, stewardship is particularly critical. It not only influences the other functions but also plays a central role in achieving the broader goals of health systems, such as equitable access to rehabilitation services. Stewardship emphasizes the government’s responsibility to manage health resources and systems in an ethical, fair, and economically efficient manner, ensuring that the growing demand for rehabilitation services can be met effectively and sustainably [7].
The capacity of stakeholders—particularly health ministries—to oversee and manage rehabilitation directly influences the implementation of strategic rehabilitation programs. Persistent weaknesses in governance and stewardship capacity throughout the program’s duration jeopardize its outcomes. Effective governance, resource management, and operational oversight are critical for achieving the objectives of strategic programs. Consequently, enhancing governance and stewardship capacity within rehabilitation systems should be prioritized [2, 8]. Strong stewardship of rehabilitation services necessitates coordination among multiple actors at the levels of policymaking, financing, service delivery, and monitoring.
Internationally, various models for the provision of rehabilitation services have been explored. However, evidence indicates that weak stewardship and governance continue to be the primary obstacles to equitable access to rehabilitation services in certain countries [9, 10]. However, evidence indicates that inadequate stewardship and governance continue to be the primary barriers to equitable access to rehabilitation services in certain countries [11]. For instance, in Iran, the lack of clear management of rehabilitation services has disrupted teamwork within these programs [12] Additionally, due to limited attention and weak stewardship—particularly in low- and middle-income countries—rehabilitation services have experienced inadequate funding and restricted access. Consequently, rehabilitation is often perceived as a luxury rather than an essential component of healthcare [1, 13].
The lack of coordination and integration of rehabilitation services across institutions has led to fragmented service delivery, driven more by internal organizational policies than by patient needs. In this context, integration refers to a systematic approach that enhances service delivery, ensuring that individuals receive a continuum of care throughout the health system [14]. This study aims to examine the broader barriers to effective rehabilitation services, analyze their implications for stewardship, and propose solutions to strengthen governance and coordination for improved service delivery.
Method
The present research was conducted through a scoping review of studies carried out in Iran and globally to identify factors and strategies for effective stewardship of rehabilitation services. This study utilized Arksey and O’Malley’s framework, which was published in 2005 and is the first methodological framework designed to guide scoping reviews. The framework consists of six steps: identifying the research question; identifying relevant studies; study selection; charting the data; collating, summarizing, and reporting the results; and consultation [15].
Eligibility criteria
All studies related to the stewardship of rehabilitation services published in Persian and English between 2000 and 2023 were included. Studies published after 2023, those written in languages other than English or Persian, documents without available full text, and theses (due to lack of access) were excluded.
Information sources
Following this framework, several Persian and English databases were searched from 2000 to 2023. Articles on rehabilitation services published in PubMed (Medline), Web of Science, Scopus, SID, and Magiran were identified based on a specific set of inclusion and exclusion criteria. Additionally, the Google Scholar search engine was utilized to locate further relevant papers.
Search
Keywords such as “rehabilitation,” “therapy,” “stewardship,” “leadership and “Governance AND policy” and their Persian equivalents, were utilized to search the databases. The reference lists of the retrieved articles were also manually examined for additional relevant papers. If other pertinent keywords were identified during the text searches, the search strategy was adjusted accordingly. Furthermore, Google Scholar alerts were established for relevant search terms, ensuring that researchers received daily updates on pertinent articles and that no relevant studies were overlooked. The results were updated at the conclusion of the study prior to drafting the report. Only studies with accessible full texts were included in the review; therefore, efforts were made to obtain access to specific articles by contacting the authors via email. The search strategy is detailed in Table 1.
Table 1.
Database search strategy
| Search Strategy | N | |
|---|---|---|
| PubMed | (((“rehab*”[Title/Abstract] OR “rehabilitation”[MeSH Terms]) AND (“stewardship*”[Title/Abstract] OR “governance“[Title/Abstract] OR “governing”[Title/Abstract] OR “leadership”[Title/Abstract] OR “policy”[Title/Abstract] OR “policies”[Title/Abstract] OR “politics”[Title/Abstract] OR “health policy”[MeSH Terms] OR “policy making”[MeSH Terms])) NOT (“Antimicrobial Stewardship“[MeSH Terms] OR “antifung*”[All Fields] OR “antibio*”[All Fields] OR “antimicrob*”[All Fields] OR “pharma*”[All Fields])) AND (english[Filter]) Filters: Books and Documents, Case Reports, Clinical Trial, Comparative Study, Controlled Clinical Trial, Historical Article, Meta-Analysis, Multicenter Study, Observational Study, Observational Study, Veterinary, Preprint, Randomized Controlled Trial, Review, Systematic Review, Technical Report, Validation Study, English, from 2000–2023 | 2,239 |
| ScienceDirect | (stewardship AND “rehabilitation”) NOT antimicrobial - from 2000–2023 | 456 |
| Scopus | TITLE-ABS-KEY (rehabilitation) AND TITLE-ABS-KEY (stewardship OR governance OR governing OR leadership OR policy OR policies OR politics OR “health policy” OR “policy making”) AND NOT “Antimicrobial Stewardship” OR antifung* OR antibio* OR antimicrob* OR pharma* AND (LIMIT-TO (LANGUAGE, “English”) OR LIMIT-TO (LANGUAGE, “Persian”)) AND (LIMIT-TO (PUBSTAGE, “final”)) AND (LIMIT-TO (OA, “all”)), from 2000–2023 | 3,723 |
| Scientific Information Database (SID) | stewardship + rehabilitation | 2 |
| Magiran | stewardship + rehabilitation | 3 |
| Google Scholar |
stewardship “rehabilitation services” – antimicrobial + “stewardship” “rehabilitation” |
2,230 + 11 |
| Final | 8,661 | |
Selection of sources of evidence
After completing the search, the articles were imported into EndNote. Following the removal of duplicates, the remaining articles were screened in three stages: first by title, then by abstract, and finally by full text, in accordance with the established inclusion and exclusion criteria. The titles and abstracts of the articles obtained through the database search were evaluated independently by both researchers, who reached an agreement at this stage of screening.
Data charting process
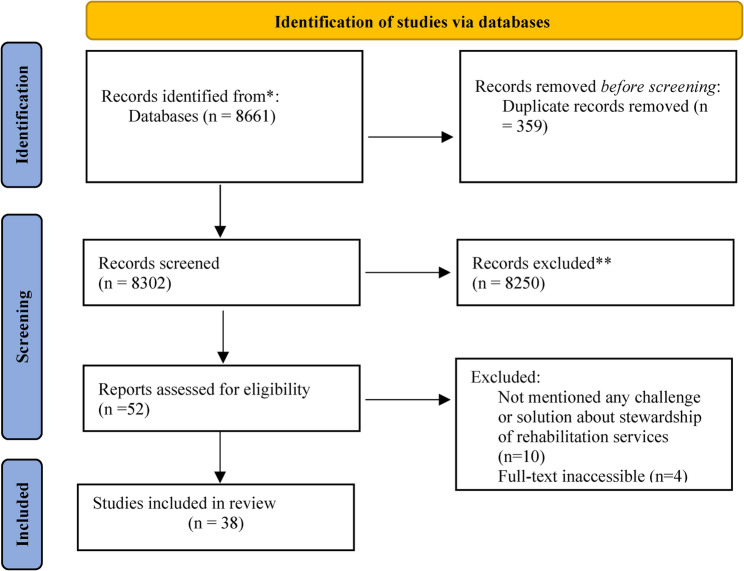
A total of 8,661 articles were extracted from the databases, leaving 8,302 articles after the removal of duplicates. Following the title and abstract screening based on the inclusion and exclusion criteria, 52 articles were selected for full-text review. Additionally, 14 inaccessible articles that did not address any challenges or solutions related to the stewardship of rehabilitation services were excluded. Ultimately, 38 articles were included in the final review. The screening process and search results are illustrated in Fig. 1 as a PRISMA flow diagram [16].
Fig. 1.
PRISMA flow diagram of database search and screening results
Data extraction
A checklist was employed to extract data from the studies identified through database searches. The data extraction tool comprised sections for authors, publication year, setting, purpose, sample size, data collection method, and the six dimensions of the Health System Stewardship Framework. Data from a 10% random sample of the articles were extracted using this checklist to evaluate the reliability of the data collection process.
Synthesis of results
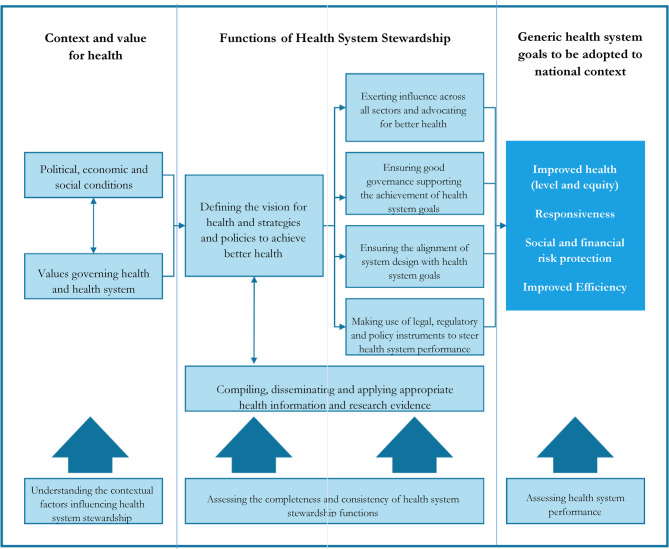
Data were analyzed using qualitative methodology through directed content analysis. Content analysis is an appropriate method for addressing questions regarding the content of the text [17]. For this purpose, the health system stewardship framework developed by Veillard et al. [7] was employed to identify and analyze the challenges and solutions implemented in other countries. This framework connects six functions of stewardship within the national context, values, and the ultimate goals pursued by the health system. These functions include: [1] defining the vision for health and formulating strategies and policies to achieve improved health outcomes; [2] exerting influence across all sectors and advocating for enhanced health; [3] ensuring good governance to support the achievement of health system goals; [4] aligning system design with health system objectives; [5] utilizing legal, regulatory, and policy instruments to guide health system performance; and [6] compiling, disseminating, and applying relevant health information and research evidence [7] (refer to Fig. 2).
Fig. 2.
Conceptual model of health system stewardship (7)
Findings
Between 2009 and 2023, a total of 38 articles were published in the field of rehabilitation services (see Table 2). Approximately 79% of these articles were authored since 2017 (refer to Fig. 3). The majority of the studies employed qualitative methodologies (42.1%), followed by mixed methods (15.8%) and review methodologies (15.8%). In total, six themes, eight sub-themes, 81 challenges, and 74 solutions were identified from the reviewed studies (see Table 3).
Table 2.
Characteristics of studies included in qualitative analysis
| S/N | Title | First Author (year) |
Country/ Region |
Rehabilitation Domain |
Study Type |
|---|---|---|---|---|---|
| 1 | The practice of physical medicine and rehabilitation in sub-Saharan Africa and Antarctica: A white paper or a black mark? [18] | Haig, AJ(2009) | Sub-Saharan Africa and Antarctica | Physical medicine and rehabilitation | Mixed methods |
| 2 | Models for integrating rehabilitation and primary care: a scoping study [19] | McColl, MA (2009) | - | Occupational therapy, physical therapy and physiatry | Scoping review |
| 3 | Exploring barriers of the health system to rehabilitation services for people with disabilities in Iran: A qualitative study [20] | Abdi, K (2015) | Iran | Rehabilitation services | Qualitative |
| 4 | Challenges in implementing the World Health Organization Disability Action Plan [21] | Khan, F (2015) | Madagascar | Rehabilitation services | Qualitative |
| 5 | Beyond physical access: a qualitative analysis into the barriers to policy implementation and service provision experienced by persons with disabilities living in a rural context [22] | Neille, J (2015) | South Africa | Congenital and acquired disabilities | Qualitative |
| 6 | Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis [23] | McVeigh, J (2016) | - | Rehabilitation services | Quantitative |
| 7 | Central intake to improve access to physiotherapy for children with complex needs: a mixed methods case report [24] | Wittmeier, KD (2016) | Canada | Pediatric physiotherapy | Mixed methods |
| 8 | Barriers to the implementation of the health and rehabilitation articles of the United Nations convention on the rights of persons with disabilities in South Africa [25] | Hussey, M (2017) | South Africa | Rehabilitation services | Qualitative |
| 9 | World Health Organisation Global Disability Action Plan 2014–2021: Challenges and perspectives for physical medicine and rehabilitation in Pakistan [26] | Khan, F (2017) | Pakistan | Physiotherapy and rehabilitation | Qualitative |
| 10 | Challenges and barriers for implementation of the World Health Organization Global Disability Action Plan in low-and middle-income countries [27] | Khan, F (2018) | Nigeria compared to similar LMICs, i.e., Madagascar, Pakistan and Mongolia | WHO Global Disability Action Plan | Qualitative |
| 11 | World health organization global disability action plan: The Mongolian perspective [28] | Khan, F (2018) | Mongolia | WHO Global Disability Action Plan | Mixed methods |
| 12 | Responding to the World Health Organization Global Disability Action Plan in Ukraine: developing a national disability, health and rehabilitation plan [29] | Gutenbrunner, Ch (2018) | Ukraine | Rehabilitation services | Qualitative |
| 13 | Strengthening rehabilitation services in Indonesia: A brief situation analysis [30] | Nugraha, B (2018) | Indonesia | Rehabilitation services | Review |
| 14 | Rehabilitation in Malaysia [31] | Naicker, AS (2019) | Malaysia | Rehabilitation services | Analysis and perspectives |
| 15 | Rehabilitation in Nepal [32] | Dhakal, R (2019) | Nepal | Rehabilitation services | Analysis and perspectives |
| 16 | Rehabilitation in Africa [33] | Geberemichael, SG (2019) | Sub-Saharan Africa | Rehabilitation services | Analysis and perspectives |
| 17 | Rehabilitation in low-resource areas [34] | Joshi, M(2019) | LMICs | Rehabilitation services | Analysis and perspectives |
| 18 | Meeting the needs of people with physical disabilities in crisis settings [35] | Barth, CA (2019) | - | Meeting the needs of people with physical disabilities | Editorial |
| 19 | Nationwide implementation of a national policy for evidence-based rehabilitation with focus on facilitating return to work: a survey of perceived use, facilitators, and barriers [36] | Brämberg, EB (2020) | Sweden | National policy for evidence-based rehabilitation | Quantitative |
| 20 | Legal and regulatory approaches to rehabilitation planning: a concise overview of current laws and policies addressing access to rehabilitation in five European countries [37] | Garg, A (2020) | Sweden, Italy, Germany, the Netherlands, and the United Kingdom | Rehabilitation services | Review |
| 21 | A framework for national rehabilitation policy and strategies in Iran: A scoping review of experiences in other countries [38] | Ahmadzadeh, N (2020) | Iran | Rehabilitation services | Scoping review |
| 22 | Challenges of accessing and using rehabilitation services in people with autism spectrum disorder: a systematic review [39] | Aarabi, MA (2020) | - | Autism spectrum disorder | Systematic review |
| 23 | A comparative study of the rehabilitation services systems for people with disabilities [10] | Iravani, M (2020) | Iran, China, Turkey, India, the USA, Mexico, Germany, England, and South Africa | Rehabilitation services for people with disabilities | Qualitative |
| 24 | Situation analysis of rehabilitation services for persons with disabilities in Bangladesh: Identifying service gaps and scopes for improvement [40] | Al Imam, MH (2022) | Bangladesh | Rehabilitation services | Mixed methods |
| 25 | Convention on the rights of persons with disabilities: Qualitative exploration of barriers to the implementation of articles [4] | Najafi, Z (2019) | Iran | Rights of persons with disabilities | Qualitative |
| 26 | Recommendations to improve insurance coverage for physiotherapy services in Iran: a multi criteria decision-making approach [41] | Shahabi, S (2021) | Iran | Physiotherapy services | Mixed methods |
| 27 | Supporting government policies to embed and expand rehabilitation in health systems in Europe: A framework for action [42] | Skempes, D (2021) | Europe | Rehabilitation services | Mixed methods |
| 28 | Stewardship of physiotherapy services in Iran: common pitfalls and policy solutions [43] | Shahabi, S (2022) | Iran | Physiotherapy services | Qualitative |
| 29 | Leadership in rehabilitation teamwork: challenges for developing countries [44] | Uddin, T (2022) | Developing countries | Rehabilitation services | Review |
| 30 | Integrating rehabilitation services into primary health care: policy options for Iran [45] | Shahabi, S (2022) | Iran | Rehabilitation services | Qualitative |
| 31 | How to become a strategic purchaser of rehabilitation services [46] | Chikhradze, T (2022) | The United States | Rehabilitation services | Qualitative |
| 32 | Cross-sectorial collaboration on policy-driven rehabilitation care models for persons with neuromuscular diseases: reflections and behavior of community-based health professionals [47] | Handberg, Ch (2022) | Denmark | Neuromuscular diseases | Qualitative |
| 33 | Coordination of health and rehabilitation services for person with disabilities in Sierra Leone–a stakeholders’ perspective [48] | Victoria Jerwanska, V (2023) | Sierra Leone | Rehabilitation services | Qualitative |
| 34 | Stewardship—the missing loop of rehabilitation in the health system: a policy brief [11] | Najafi, Z (2023) | Iran | Rehabilitation services | Policy brief |
| 35 | Prioritizing rehabilitation in low-and middle-income country national health systems: a qualitative thematic synthesis and development of a policy framework [49] | Neill, R (2023) | LMICs | Rehabilitation services | Qualitative |
| 36 | The intersection of health rehabilitation services with quality of life in Saudi Arabia: current status and future needs [50] | Alanazi, AM (2023) | Saudi Arabia | Rehabilitation services | Qualitative |
| 37 | Legal challenges of rehabilitation services in Iran: The framework of the health system functions model of the World Health Organization [51] | Shahidisadeghi, N (2023) | Iran | Rehabilitation services | Editorial |
| 38 | Impact of the COVID-19 pandemic and governmental policies on rehabilitation services and physical medicine in Jordan: a retrospective study [52] | Almasri, NA (2023) | Jordan | Rehabilitation services | Quantitative |
Table 3.
Challenges and solutions to effective stewardship of rehabilitation services
| Themes | Sub-themes | Challenges | Solutions |
|---|---|---|---|
| (1) Defining the vision for health and strategies and policies to achieve better health | Values governing health and health system |
Entities influencing how values are defined • Ineffectiveness of the disjointed rehabilitation structure and stewardship (4, 20, 39, 43) • Low level of awareness about rehabilitation services among policy-makers (4, 43) High-level policies influencing how values are defined • Higher priority given to acute care and infectious diseases (26, 27) • Apparent divergence among high-level documents (43) • Absence of a comprehensive rehabilitation program (4) • Livelihood support being the dominant discourse instead of empowerment (51) • Overlooking rehabilitation services in health promotion planning strategies (37) • Complexity of rehabilitation governance due to the lack of a common definition for and the multi-sectoral nature of rehabilitation (26, 37) |
Institutional structuring of rehabilitation stewardship • Stewardship of rehabilitation by the health sector (10, 11, 18) • Use of relevant experts in decision-making and policy-making processes (43) • Strengthening the National Council for Persons with Disabilities (10, 11) • Development of rehabilitation services based on an understanding of rehabilitation as a population strategy for health and well-being related to a wide range of health conditions across the continuum of care and throughout life (42) • Strengthening the position of rehabilitation groups in policy-making processes(42) • Designating a focal point to manage and lead the development of national rehabilitation policy (44) Shaping high-level policies • Integrating rehabilitation services into major health policies and programs with a special focus on rehabilitation workforce recruitment and training as well as allocation of resources.(40, 50) • Developing and implementing a long-term policy, strategy, and action plan on disability management (11, 32) • Translation and adaptation of international definitions (such as “functioning”, “disability”) and tools (such as the International Classification of Functioning, Disability and Health) (29) • “Institutionalization” of programs by aligning them with previous Ministry of Health rehabilitation models to support program sustainability (23) • Assessing local rehabilitation needs and identifying priorities for action (42) • Developing an operational, budgeted national rehabilitation program aligned with international and regional normative and programmatic frameworks (42) • Providing comprehensive rehabilitation services along with a special service package for people with disabilities (10, 30, 31, 45) |
| Context |
Special conditions of rehabilitation patients • Severity and instability of patients’ conditions (22) • Duration of disability (22) • Necessity (urgency) of intervention (52) • The number and complexity of services (needs of the patient) (52) Economic-political factors • Unstable political and economic conditions (4, 26, 27) • International sanctions (43) • Unreasonable fees set for rehabilitation services and the very high costs of providing them (43) • Inadequate insurance coverage for rehabilitation services (37, 39, 41, 42, 51) • The expensiveness of rehabilitation services (34, 51) • Lack of financing through subsidies from public revenues and taxes (10, 41, 51) • Low political priority given to rehabilitation services (36, 42, 48) • Lack of dedicated funding for services provided to people with disabilities (25, 40, 42, 48) • Many non-profit service providers are funded by international development agencies and/or private humanitarians, raising concerns about sustainability and fragmentation.(49) Sociocultural factors • Neglecting sociocultural factors in the provision of rehabilitation services (4, 20, 22, 25) Risk factors related to the burden of diseases in the field of rehabilitation • The impact of rising mortality rates and the burden of infectious diseases, violence, poverty, and overall diseases on the increase in disabilities(22) • The burden of road traffic accidents and challenges related to communication routes, access to buildings and roads, and procurement (31) • Occurrence of crises caused by natural disasters, war, economy, and the climate (52) • Lack of proper infrastructure, especially inpatient service infrastructure (25) (49) Technology-related factors • Overlooking new technologies in the provision of rehabilitation services(4) |
• Removal of international sanctions (43) • Taking advantage of funding from insurance companies and taxes (10, 51) • Investing in infrastructure/human resources (11, 27, 31) • Educating the community and building the culture around disability and rehabilitation services (31, 38, 47) • Examining the share of rehabilitation from the country’s insurance credit portfolio (51) • Providing competitive payment mechanisms for primary care workers(45) |
|
| (2) Exerting influence across all sectors and advocating for better health | Intersectoral and intersectoral collaboration |
Multiple entities tasked with the provision of rehabilitation services • Changes to and lack of coordination/communication between ministries governing disability policies and rehabilitation services (48) • Lack of coordination and leadership between ministries and other organizations involved in rehabilitation and disability (26, 48) • Lack of coordination and parallel work among several organizations involved in rehabilitation (including the Ministry of Health, Welfare Organization, Red Crescent, Veteran) (10, 20) Lack of clarity in roles and responsibilities • Lack of clarity in the division of responsibilities (26, 36) • Poor coordination/collaboration between different government departments and health ministries and agencies (27, 29, 30, 51) Lack of coordination and collaboration between different sectors • Limited coordination/collaboration between different sectors including primary health care and hospitals (private/public), charities and community organizations, and NGOs (10, 27, 48) (25, 28) • Failure to do team work in rehabilitation services (34) • Poor interaction between key stakeholders (43) Lack of coordination in providing rehabilitation services • Lack of coordination and cooperation between the departments involved in the financing, purchasing, and provision of rehabilitation services (46) • Lack of a common language between the Welfare Organization and the Health Insurance Organization(51) • Reluctance of insurance companies to cover physiotherapy due to high costs (43) • disconnect between acute and community-based rehabilitation (21) Ignoring influential groups • Low power and influence of therapeutic and educational rehabilitation expert groups (42, 43) • Poor stakeholder participation (43) • Inattention of countries and international organizations to the need for the provision of rehabilitation services to disabled people in disaster and war-torn areas (35) • Lack of adequate training and information about the provision of disability and rehabilitation services to the community(25, 30) |
Clarifying roles and responsibilities • Planning for and developing structures for close coordination and cooperation among key stakeholders (11, 34, 36) Participation of influential groups • Close cooperation with rehabilitation and medical centers and the World Health Organization (21, 35, 36) • Involving people with disabilities in policy processes to improve responsiveness, efficiency, effectiveness, and sustainability of programs and to enhance decision-making and user satisfaction with services (23) • Engaging the workforce, consumers and NGOs to lobby government, improve awareness of disability services, and determine the social and economic impact of disability (21, 26, 28, 35, 42) • Promoting multisectoral and multilateral partnerships for efficient mobilization and utilization of rehabilitation resources (33, 35, 42) • Improving stakeholders’ participation in policy making (42, 43, 45) Promotion of interaction and cooperation • Promoting interdisciplinary cooperation due to the interdisciplinary nature of rehabilitation services (19, 32, 33) • Promoting interaction among stakeholders (43) • Showing the economic value of rehabilitation services (43) • Improving cooperation between involved actors (19, 32, 43) • Strong interdepartmental coordination to create consistent mandates across government departments regarding service delivery (23, 31) |
| (3) Ensuring good governance supporting the achievement of health system goals | Governance and accountability |
Weak governance structure • Unclear accountability structures (43) • Delays in the implementation of health policies as well as recruitment/education/health policies for people with disabilities (26, 27) • Weak political commitment (26–28) • Lack of training/knowledge about disability among policy makers and government officials (26, 36) • Lack of funds for implementing existing policies (26) • Lack of equitable and comprehensive rehabilitation services (4, 29, 33) Decentralization of governance • Lack of strong leadership and a central governing body (27) |
• Establishing a legislative body and central governance for rehabilitation (11, 26, 27) • Creating effective accountability structures (11) • Reducing the divergence between laws and high-level documents (43) • Establishing strong guarantees of enforcement for approved laws (43) • Increasing patients’ involvement in policy making (42, 43) • Education/awareness programs on disability and physical medicine and rehabilitation for policy makers, government officials, hospital administrators (11, 27) • Including physical medicine and rehabilitation staff in policy development (27) • Developing key performance indicators, standards of care and criteria (26, 27) • Active role of physical medicine and rehabilitation departments in facilitating leadership and governance skills (26, 27, 44) • Establishing health care standards/policies, implementation and evaluation (27) • Allocating sufficient resources with international cooperation and support and Promoting the sharing and utilization of knowledge between countries (27) (11) • Decentralizing and separating stewardship from financing and service provision in organizations that provide rehabilitation services (11) |
| (4) Ensuring the alignment of system design with health system goals | Health system resources |
• Inadequate human resources and their improper distribution (18, 21, 25, 28–30, 39, 43, 49) • Inadequate clinical training (43) • Lack of sufficient facilities (21, 43) • Unclear interdisciplinary boundaries (21, 43) |
• Removing interdisciplinary boundaries (37, 43) • Providing required facilities and equipment (43) • Fair distribution of human resources (43, 50) • Using innovative approaches to improve clinical education (29, 43) • Training sufficient rehabilitation workforce according to the needs of each region (10) • Increasing the sustainability of rehabilitation services through capacity building among employees (26, 35, 42, 50) • Upskilling, training, and development of the rehabilitation workforce using innovative, web-based technologies/systems (26, 28, 32, 45, 47) |
| Provision of rehabilitation services within the health system |
• Poor referral system (20, 43) • The lower than expected role of the first level of service delivery in providing rehabilitation services (19) • Lack of coordination between rehabilitation centers, including autism centers (39) • Very little communication between service providers (24) • Long waiting times (24, 25, 39) • Heterogeneity of services provided in different centers (29, 39, 50) • Inefficiency and flaws in the diagnosis and screening of people with disabilities (10, 20, 39) • Inadequate implementation of health care policies for people with disabilities (48) • Lack of access among people with disabilities to basic service packages (10, 21, 22, 39, 49, 51) • Neglecting rehabilitation interventions, including preventive rehabilitation interventions or physiotherapy, in PHC (43) • A large percentage of rehabilitation services are provided by private providers in LMICs (49) |
• Improving the referral system (43, 45) • Developing community-based rehabilitation (19, 34) • Integrating rehabilitation services into structured care pathways, PHC and in other social services (19, 30, 35, 42, 43) • Paying attention to preventive rehabilitation interventions (43) • Developing real fees according to economic and clinical conditions (43) • Expanding the diversity of rehabilitation services (24, 32, 38) • The development of health-related rehabilitation services should be implemented at all levels of health care (primary, secondary, tertiary) and for all phases of health care (acute, post-acute, long-term) (24, 29, 30, 38, 40) • Including rehabilitation services and assistive technology in the free health care plan (48) (49) • Modifying basic rehabilitation services (50) • Development of telerehabilitation (30, 42, 45, 50) |
|
| (5) Making use of legal, regulatory and policy instruments to steer health system performance | Policies, laws and regulations |
• Lack of transparency and balance as well as flaws in laws and policies (10, 20, 28, 29, 37, 43, 51) • Absence of rehabilitation specialists, including physiotherapists, in legislative processes (43) • Failure to provide comprehensive supervision of rehabilitation (10, 40, 48, 51) • Lack of powerful and efficient auditing (43) • Failure to carry out the accreditation process (21, 27, 43) • Corruption (22, 27, 43) • Lack of strong guarantees of enforcement for approved laws (43) |
• Establishing clear and effective laws (43, 50) • Developing efficient auditing systems (43) • Using anti-corruption strategies (43) • Developing key performance indicators and care standards and criteria as well as a comprehensive accreditation system for rehabilitation(26) • Establishing accountability mechanisms for periodic monitoring and review of progress against nationally and internationally agreed goals related to rehabilitation (42) • Strengthening accountability and regulatory frameworks of government at all levels (11) |
| (6) Compiling, disseminating and applying appropriate health information and research evidence |
• Lack of a comprehensive information infrastructure (21, 43) • Inadequate clinical guidance and low-quality studies (43) • The scarcity of economic evaluations (43) • Absence of health technology assessment (HTA) (43) • Lack of a rehabilitation information system for people with disabilities (49) • Lack of full access to comprehensive national data of persons with disabilities (26, 28, 49) • Inaccessible or low quality data needed to implement strategic purchasing decisions for rehabilitation services (46) • Lack of correct and sufficient information to identify real needs and follow service outputs and track service outputs. (46, 49) • Lack of sufficient scientific evidence regarding rehabilitation in environments with limited resources(34) |
• Developing an effective rehabilitation information system (40, 43, 47) • Developing clinical guidelines for rehabilitation services (35, 43) • Conducting high-quality studies (e.g., RCTs and systematic reviews) (43) • Conducting economic evaluations for rehabilitation services (43) • Strengthening investment in research at every level in order to improve understanding, awareness and centrality of issues related to disability (26, 28, 31, 35) • Creating data management platforms for rehabilitation services (10) • Registering existing rehabilitation facilities (including the number of institutions and beds and their quality) as a basis for planning service provision to meet the needs of people with disabilities(30) • Improving web-based access to evidence-based guidelines/protocols for disabilities (26) • Creating a reliable database on the epidemiology of disability (including chronic and mental illnesses) and the need for rehabilitation (29) |
Discussion
This scoping review aimed to identify the challenges and solutions for effective stewardship of rehabilitation services both globally and in Iran, utilizing a health stewardship framework.
This review encompasses 38 studies, providing a comprehensive temporal scope that facilitates the analysis of evolving trends in rehabilitation stewardship over time. The included studies were published between 2009 and 2023. As illustrated in the figure, the number of studies in the early years (2010–2014) was quite limited, with some years yielding no eligible studies for inclusion. This may indicate a lack of research focus on the subject during that period. From 2015 onward, the number of studies began to increase, particularly between 2018 and 2023, demonstrating a consistent upward trend that peaked in 2021. Fluctuations in study volume across the years may be attributed to factors such as policy changes, health crises, or shifting research priorities Fig. 3.
Fig. 3.
Frequency distribution of articles
Data were extracted through six key stewardship functions: establishing a health vision, influencing various sectors, ensuring effective governance, aligning system design with objectives, utilizing legal, regulatory, and policy instruments, and leveraging health information and evidence. Consequently, several factors were identified that contribute to the inefficiency, ineffectiveness, and unsustainability of rehabilitation services, particularly in low- and middle-income countries (LMICs).
First, there is fragmentation and inconsistency in rehabilitation governance, characterized by unclear policies and misaligned objectives. Cross-sector collaboration is essential to address this fragmentation; however, it is often hindered by siloed structures and ambiguous roles. Additionally, weak central leadership and the absence of a lead agency exacerbate coordination and regulatory challenges. In this context, Neill et al. (2023) and a study conducted in Uganda highlight that fragmented governance structures and weak advocacy efforts impede collective action across various levels and among different actors, thereby hindering the effective implementation of rehabilitation policies [49, 53]. For example, limited participation and involvement of patients with disabilities adversely affect responsiveness, satisfaction, productivity, service relevance, sustainability, and diminish ownership over decision-making outcomes [23]. To address this challenge, Shahabi et al. propose integrating rehabilitation services into the primary healthcare (PHC) system. Such integration, combined with a legal framework, intersectoral collaboration, NGO involvement, and robust governance, can enhance the efficiency and effectiveness of rehabilitation services [45]. Similarly, Krug and Cieza underscore the importance of incorporating rehabilitation services into essential service packages to ensure continuity of care [54]. Furthermore, Magaqa’s study identifies the lack of integration into existing health system structures as a significant barrier to scaling up services in South Africa [55].
Second, the study reveals that evidence and data are frequently underutilized in policy decision-making. In fact, in addition to integrated structure, it is crucial to provide comprehensive information on effective rehabilitation services, including both available and necessary resources—such as funding, pharmaceuticals, medical equipment, and human resources—to support evidence-based planning and budgeting [56]. An information management system capable of conducting situational analyses of disability within countries can guide policymakers in service provision and assist healthcare workers in selecting the most appropriate interventions [23].
Thirdly, the study emphasizes the influence of contextual factors, such as crises and demographic shifts, on rehabilitation priorities. However, health systems often struggle to adapt due to inadequate planning and workforce shortages. In Iran, for example, changes in political leadership have affected the prioritization of funding for physical rehabilitation [24]. Similarly, Recent cross-regional studies indicate that economic deprivation and inadequate health infrastructure persist as significant factors influencing the unmet rehabilitation needs in numerous resource-constrained regions, particularly in low- and middle-income countries (LMICs), where there has been a notable increase in rehabilitation-sensitive health conditions in recent years [57]. More broadly, resource limitations and systemic constraints play a critical role in shaping the delivery of rehabilitation service. Persistent financial challenges, workforce shortages, and economic instability frequently hinder service provision and implementation efforts [58]. Furthermore, the COVID-19 pandemic has exacerbated these challenges, exposing inherent systemic weaknesses and underscoring the necessity for adaptive and resilient governance in rehabilitation. Employing a systems thinking framework, Jesus et al. (2020) identified multiple leverage points, such as the expansion of telehealth, workforce adaptability, and crisis preparedness, which can enhance the responsiveness and sustainability of rehabilitation services both during and after emergencies [59]. Therefore, a comprehensive understanding of local contexts and systemic barriers is essential for policymakers to develop effective and sustainable rehabilitation policies [23].
Consequently, several interrelated challenges—including structural deficiencies, disconnected policies, misaligned plans, limited stakeholder participation, and weak information systems that impede evidence-based decision-making—contribute to the fragmented stewardship of rehabilitation services.
Several research gaps persist in the field of rehabilitation stewardship. The role of supervision and accountability mechanisms within stewardship frameworks has not been thoroughly examined, particularly in low- and middle-income countries (LMICs). Furthermore, the cost-effectiveness of various stewardship models remains unclear. Future research should investigate how different governance structures impact the quality, accessibility, and equity of rehabilitation services. Additionally, this review is constrained by the narrow scope and depth of the existing literature. Research on rehabilitation stewardship is relatively scarce, especially in LMICs, which may lead to a biased understanding of global challenges. While integrating findings within a general health stewardship framework offers valuable insights, it may not adequately address the unique complexities of the rehabilitation sector, highlighting the need for a more specialized approach.
Limitation
The present review is constrained by several limitations. Firstly, the focus on studies published in English may have resulted in the exclusion of pertinent research published in other languages or formats, including grey literature. Secondly, despite implementing a comprehensive search strategy, the dynamic and interdisciplinary nature of rehabilitation stewardship may have contributed to the oversight of relevant studies that utilize alternative terminologies. Lastly, the generalizability of the findings is inherently restricted due to context-specific emphasis of many of the included studies. Many of the included studies focus on specific contexts, populations, or settings, which means their findings may not be easily transferable to other environments or groups.
Conclusion
In conclusion, the successful and efficient stewardship of integrated rehabilitation services is contingent upon a variety of interconnected elements. These factors encompass the promotion of service integration throughout a continuum of care, the alignment of pertinent policies and operational strategies to enhance stakeholder collaboration, and the encouragement of engagement via a cohesive policymaking framework. Additionally, the establishment of a robust information system may facilitate evidence-based decision-making and enhance the governance of rehabilitation services.
Acknowledgements
The authors would like to extend their most sincere gratitude and appreciation to the esteemed reviewers of the article.
Authors’ contributions
MA and KA participated in the design of the study. MA, ZN and ZF undertook the literature review process. All authors drafted the manuscript. All authors read and approved the final manuscript.
Funding
Research funding from University of Social Welfare and Rehabilitation Sciences.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval was obtained from the University of Social Welfare and Rehabilitation Sciences (IR.USWR.REC.1402.099).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Rehabilitation [Available from: https://www.who.int/news-room/fact-sheets/detail/rehabilitation
- 2.Gimigliano F, Negrini S. The world health organization rehabilitation 2030: a call for action. Eur J Phys Rehabil Med. 2017;53(2):155–68. [DOI] [PubMed] [Google Scholar]
- 3.Affairs UDoEaS. THE 17 GOALS | Sustainable Development [Available from: https://sdgs.un.org/goals
- 4.Najafi Z, Abdi K, Khanjani MS, Dalvand H, Amiri M. Convention on the rights of persons with disabilities: qualitative exploration of barriers to the implementation of articles 25 (health) and 26 (rehabilitation) in Iran. Med J Islam Repub Iran. 2021;35: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO, Disability. 2023 [Available from: https://www.who.int/news-room/fact-sheets/detail/disability-and-health
- 6.WHO. The world health report 2000 2000 [Available from: https://www.who.int/publications/i/item/924156198X
- 7.Veillard JHM, Brown AD, Barış E, Permanand G, Klazinga NS. Health system stewardship of National health ministries in the WHO European region: concepts, functions and assessment framework. Health Policy. 2011;103(2):191–9. [DOI] [PubMed] [Google Scholar]
- 8.WHO. WHO global disability action plan 2014–2021 [Available from: https://www.who.int/publications/i/item/who-global-disability-action-plan-2014-2021
- 9.abdi k, Najafi Z, Foroughi Z, Afshari M. Health policy analysis for stewardship of rehabilitation services. BMC Health Serv Res. 2024;24(1):1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iravani M, Riahi L, Abdi K, Tabibi SJ. A comparative study of the rehabilitation services systems for people with disabilities. Archives Rehabilitation. 2021;21(4):544–63. [Google Scholar]
- 11.Najafi Z, Abdi K, Soltani S. Stewardship; the missing loop of rehabilitation in the health system: A policy brief. Med J Islamic Repub Iran. 2023;37. [DOI] [PMC free article] [PubMed]
- 12.Jahanbin P, Abdi K, Khanjani MS, Hosseini MA. Exploring barriers of teamwork in providing rehabilitation services: A qualitative content analysis. Archives Rehabilitation. 2019;20(3).
- 13.WHO. Global report on health equity for persons with disabilities [Available from: https://www.who.int/publications/i/item/9789240063600
- 14.Waterworth CJ, Smith F, Kiefel-Johnson F, Pryor W, Marella M. Integration of rehabilitation services in primary, secondary, and tertiary levels of health care systems in low- and middle-income countries: a scoping review. Disabil Rehabil. 2024;46(25):5965–76. [DOI] [PubMed] [Google Scholar]
- 15.Arksey H, O’malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 16.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. [DOI] [PMC free article] [PubMed]
- 17.Downe-Wamboldt B. Content analysis: method, applications, and issues. Health Care Women Int. 1992;13(3):313–21. [DOI] [PubMed] [Google Scholar]
- 18.Haig AJ, Im J, Adewole A, Nelson VS, Krabak B, Africa IRFCP. The practice of physical medicine and rehabilitation in subsaharan Africa and Antarctica: a white paper or a black mark? PM&R. 2009;1(5):421–6. [DOI] [PubMed] [Google Scholar]
- 19.McColl MA, Shortt S, Godwin M, Smith K, Rowe K, O’Brien P, et al. Models for integrating rehabilitation and primary care: a scoping study. Arch Phys Med Rehabil. 2009;90(9):1523–31. [DOI] [PubMed] [Google Scholar]
- 20.Abdi K, Arab M, Rashidian A, Kamali M, Khankeh HR, Farahani FK. Exploring barriers of the health system to rehabilitation services for people with disabilities in Iran: a qualitative study. Electron Physician. 2015;7(7):1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan F, Amatya B, Mannan H, Burkle FM Jr, Galea MP. Rehabilitation in Madagascar: challenges in implementing the World Health Organization disability action plan. J Rehabil Med. 2015;47(8):688–96. [DOI] [PubMed] [Google Scholar]
- 22.Neille J, Penn C. Beyond physical access: a qualitative analysis into the barriers to policy implementation and service provision experienced by persons with disabilities living in a rural context. Rural Remote Health. 2015;15(3):149–62. [PubMed] [Google Scholar]
- 23.McVeigh J, MacLachlan M, Gilmore B, McClean C, Eide AH, Mannan H, et al. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Global Health. 2016;12:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wittmeier KD, Restall G, Mulder K, Dufault B, Paterson M, Thiessen M, et al. Central intake to improve access to physiotherapy for children with complex needs: a mixed methods case report. BMC Health Serv Res. 2016;16:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hussey M, MacLachlan M, Mji G. Barriers to the implementation of the health and rehabilitation articles of the United Nations convention on the rights of persons with disabilities in South Africa. Int J Health Policy Manage. 2016;6(4):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan F, Amatya B, Sayed TM, Butt AW, Jamil K, Iqbal W, et al. World health organization global disability action plan 2014–2021: challenges and perspectives for physical medicine and rehabilitation in Pakistan. J Rehabil Med. 2017;49(1):10–21. [DOI] [PubMed] [Google Scholar]
- 27.Khan F, Owolabi M, Amatya B, Hamzat TK, Ogunniyi A, Oshinowo H, et al. Challenges and barriers for implementation of the World Health Organization global disability action plan in low-and middle-income countries. J Rehabil Med. 2018;50(4):367–76. [DOI] [PubMed] [Google Scholar]
- 28.Khan F, Amatya B, Avirmed B, Yi Y, Shirmen B, Abbott G, et al. World health organization global disability action plan: the Mongolian perspective. J Rehabil Med. 2018;50(4):388–66. [DOI] [PubMed] [Google Scholar]
- 29.Gutenbrunner C, Tederko P, Grabljevec K, Nugraha B, Stiftelsen Rehabiliteringsinformation. Responding to the world health organization global disability action plan in Ukraine: developing a national disability, health and rehabilitation plan. J Rehabil Med. 2018. 10.2340/16501977-2294. [DOI] [PubMed] [Google Scholar]
- 30.Nugraha B, Setyono GR, Defi IR, Gutenbrunner C. Strengthening rehabilitation services in indonesia: A brief situation analysis. J Rehabilitation Med (Stiftelsen Rehabiliteringsinformation). 2018;50(4). [DOI] [PubMed]
- 31.Naicker AS, Engkasan JP, Mazlan M, Yusof YM, Yuliawiratman BS, Hasnan N, et al. Rehabilitation in Malaysia. Phys Med Rehabil Clin N Am. 2019;30(4):807–16. [DOI] [PubMed] [Google Scholar]
- 32.Dhakal R, Groves CC. Rehabilitation in Nepal. Phys Med Rehabil Clin N Am. 2019. 10.1016/j.pmr.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 33.Geberemichael SG, Tannor AY, Asegahegn TB, Christian AB, Vergara-Diaz G, Haig AJ. Rehabilitation in Africa. Phys Med Rehabil Clin N Am. 2019;30(4):757–68. [DOI] [PubMed] [Google Scholar]
- 34.Joshi M. Rehabilitation in low-resource areas. Phys Med Rehabil Clin N Am. 2019;30(4):835–46. [DOI] [PubMed] [Google Scholar]
- 35.Barth CA. Meeting the needs of people with physical disabilities in crisis settings. Bull World Health Organ. 2019;97(12):790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Björk Brämberg E, Jensen I, Kwak L. Nationwide implementation of a national policy for evidence-based rehabilitation with focus on facilitating return to work: a survey of perceived use, facilitators, and barriers. Disabil Rehabil. 2020;42(2):219–27. [DOI] [PubMed] [Google Scholar]
- 37.Garg A, Skempes D, Bickenbach J. Legal and regulatory approaches to rehabilitation planning: a concise overview of current laws and policies addressing access to rehabilitation in five European countries. Int J Environ Res Public Health. 2020;17(12): 4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmadzadeh N, Azar FEF, Baradaran HR, Roghani RS, Shirazikhah M, Joghataei MT, et al. A framework for National rehabilitation policy and strategies in iran: A scoping review of experiences in other countries. Iran J Public Health. 2020;49(9):1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aarabi MA, Abdi K, Khanjani MS. Challenges of accessing and using rehabilitation services in people with autism spectrum disorder: a systematic review. J Rehabil. 2021;22(3):260–77. [Google Scholar]
- 40.Al Imam MH, Jahan I, Das MC, Muhit M, Akbar D, Badawi N, et al. Situation analysis of rehabilitation services for persons with disabilities in Bangladesh: identifying service gaps and scopes for improvement. Disabil Rehabil. 2022;44(19):5571–84. [DOI] [PubMed] [Google Scholar]
- 41.Shahabi S, Skempes D, Behzadifar M, Tabrizi R, Nazari B, Ghanbari MK, et al. Recommendations to improve insurance coverage for physiotherapy services in iran: a multi criteria decision-making approach. Cost Eff Resource Allocation. 2021;19:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Skempes D, Kiekens C, Malmivaara A, Michail X, Bickenbach J, Stucki G. Supporting government policies to embed and expand rehabilitation in health systems in Europe: a framework for action. Health Policy. 2022;126(3):158–72. [DOI] [PubMed] [Google Scholar]
- 43.Shahabi S, Skempes D, Mojgani P, Bagheri Lankarani K, Heydari ST. Stewardship of physiotherapy services in Iran: common pitfalls and policy solutions. Physiother Theory Pract. 2022;38(12):2086–99. [DOI] [PubMed] [Google Scholar]
- 44.Uddin T. Leadership in rehabilitation teamwork: challenges for developing countries. Front Rehabil Sci. 2022;3: 1070416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shahabi S, Kiekens C, Etemadi M, Mojgani P, Teymourlouei AA, Lankarani KB. Integrating rehabilitation services into primary health care: policy options for Iran. BMC Health Serv Res. 2022;22(1): 1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chikhradze T, Brainerd EL, Ishtiaq A, Alperson R. How to become a strategic purchaser of rehabilitation services. Bull World Health Organ. 2022;100(11):709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Handberg C, Werlauff U. Cross-sectorial collaboration on policy-driven rehabilitation care models for persons with neuromuscular diseases: reflections and behavior of community-based health professionals. BMC Health Serv Res. 2022;22(1):1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jerwanska V, Kebbie I, Magnusson L. Coordination of health and rehabilitation services for person with disabilities in Sierra Leone–a stakeholders’ perspective. Disabil Rehabil. 2023;45(11):1796–804. [DOI] [PubMed] [Google Scholar]
- 49.Neill R, Shawar YR, Ashraf L, Das P, Champagne SN, Kautsar H, et al. Prioritizing rehabilitation in low-and middle-income country national health systems: a qualitative thematic synthesis and development of a policy framework. Int J Equity Health. 2023;22(1): 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alanazi AM, Almutairi AM, Aldhahi MI, Alotaibi TF, AbuNurah HY, Olayan LH, et al. editors. The intersection of health rehabilitation services with quality of life in Saudi arabia: current status and future needs. Healthcare: MDPI; 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shahidisadeghi N, Sedighi S, Bakhtiyari M. Legal challenges of rehabilitation services in iran: the framework of the health system functions model of the world health organization. Payesh (Health Monitor). 2023;22(2):233–6. [Google Scholar]
- 52.Almasri NA, Dunst CJ, Hadoush H, Aldaod J, Khader Y, Alrjoub A, et al. Impact of the COVID-19 pandemic and governmental policies on rehabilitation services and physical medicine in Jordan: a retrospective study. Int J Environ Res Public Health. 2023;20(3): 1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Neill R, Rutebemberwa E, Tweheyo R, Ojulo ST, Okello G, Bachani AM, et al. Generating political priority for the health needs of the 21st century: a qualitative policy analysis on the prioritization of rehabilitation services in Uganda. Int J Health Policy Manage. 2024;13:8347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krug E, Cieza A. Strengthening health systems to provide rehabilitation services. Sage Publications Sage CA: Los Angeles, CA; 2017. pp. 72–3. [DOI] [PubMed]
- 55.Magaqa Q. Contributing Factors to Implementation Gaps in Rehabilitation Services in South Africa: Perspectives from health facility-level Rehabilitation Clinician-Managers. 2021.
- 56.Rauch A, Negrini S, Cieza A. Toward strengthening rehabilitation in health systems: methods used to develop a WHO package of rehabilitation interventions. Arch Phys Med Rehabil. 2019;100(11):2205–11. [DOI] [PubMed] [Google Scholar]
- 57.Jesus TS, Carlos A-LJ, Suresh KK, Landry MD. Growing physical rehabilitation needs in resource-poor world regions: secondary, cross-regional analysis with data from the global burden of disease 2017. Disabil Rehabil. 2022;44(19):5429–39. [DOI] [PubMed] [Google Scholar]
- 58.Dorjbal D, Zanini C, Tsegmid N, Stucki G, Rubinelli S. Toward an optimization of rehabilitation services for persons with spinal cord injury in Mongolia: the perspective of medical doctors. Disabil Rehabil. 2021;43(15):2200–12. [DOI] [PubMed] [Google Scholar]
- 59.Jesus TS, Landry MD, Jacobs K. A ‘new normal’ following COVID-19 and the economic crisis: using systems thinking to identify challenges and opportunities in disability, telework, and rehabilitation. WORK. 2020;67(1):37–46. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.