Although age-related macular degeneration and cataracts are leading causes of blindness, how they themselves are caused is unclear. These diseases are thought to result from damage caused, photochemically and nonphotochemically, to various cell types in the eye by oxidative stress. Because its protective fibre cells do not renew themselves, the lens is the ocular structure most susceptible to oxidative damage. When the underlying epithelial cells are exposed to the action of exogenous and endogenous reactive oxygen species, the crystallin proteins in the lens cross-link and aggregate, and cataracts are produced.
The retina, which uses more oxygen than any other tissue in the body, is also susceptible to damage. Long-term exposure to radiation can damage photoreceptor outer segments, inhibit mitosis in the retinal pigment epithelium and choroids and has been associated with photoreceptor degeneration and lipid peroxidation.
Polyunsaturated fatty acids found in the lens and in the photoreceptor membranes of the rods and cones of the retina are particularly susceptible to damage. Their many double bonds predispose them to oxidation, which in turn causes lipid radicals to form. This initiates a cytotoxic cascade that makes these fatty acids unavailable to the lens and photoreceptor membranes and results in losses in function and structural integrity.
The carotenoid pigment lutein (found in egg yolk, corn, and various yellow and green fruits and vegetables) also occurs in certain ocular tissues, specifically the macular pigment of the retina and the epithelium and cortex of the lens (Fig. 1). Lutein may play a role in slowing the age-related degeneration of these tissues, both directly as an antioxidant and indirectly by absorbing blue light. There is a biochemical rationale and some in vitro evidence for this effect.
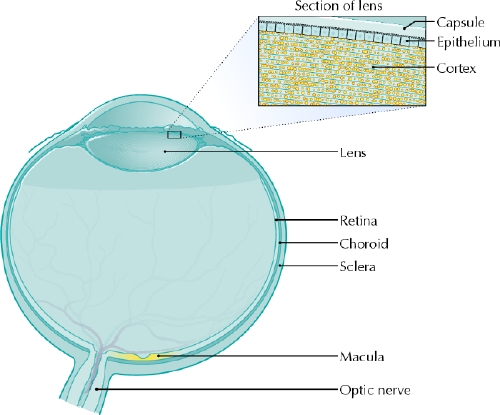
Fig. 1: Cross-section of the eye. Lutein, which is indicated with yellow, is found in the epithelium and cortex of the lens and the macula of the retina. Photo: Lianne Friesen and Nicholas Woolridge
The OH functional group on the lutein molecule's ε-ionone ring makes it susceptible to oxidation. The results of in vitro studies indicate that lutein directly protects against oxidative stress by reducing photosensitizers and singlet oxygen, reacting with free radicals and retarding the peroxidation of membrane phospholipids. Additionally, the double bonds on the polyene chain can readily be oxidized by reactive oxygen species, thus preventing the oxidation of valuable cells.
One of the limiting factors in demonstrating the effects of lutein on oxidation lies in the difficulty of measuring the oxidative stress of the retina. There is evidence to support the antioxidative properties of lutein in vitro, where its oxidative capacity is determined by examining its effect on low-density lipoprotein oxidation or on the oxidative damage of DNA in lymphocytes. However, measuring the oxidative role of lutein in vivo is challenging because markers of oxidation, such as the oxidation products of lutein, are unstable and may reflect oxidative stress in tissue. The few studies that measure biomarkers of oxidation have not found that lutein mediates oxidative stress.
Lutein may also prevent oxidative stress indirectly by absorbing blue light. Exposure to blue light results in the formation of free radicals that contribute to oxidative stress in the retina. Epidemiologic evidence suggests that lutein may reduce blue light intensity by 40%– 90%.1 It is thought that, by absorbing short-wave blue light before it is processed, lutein may reduce photochemical damage of the retina and increase visual acuity, thus reducing the development of age- related macular degeneration.
No randomized trials have been performed to study the effects of lutein on age-related macular degeneration or cataracts. The existing epidemiologic evidence is mixed. The Beaver Dam Eye Study prospectively examined nutrient intake in relation to the incidence of nuclear cataracts.2 Overall, 246 of the 1354 participants reported cataracts.2 Higher intakes of lutein and its isomer zeaxanthin were associated with a decreased incidence of cataracts.2 More specifically, the odds ratio for cataracts in the quintile with the highest intake of lutein (mean intake 1245 g lutein/4.18 MJ) compared with the lowest intake quintile (mean intake 298 g lutein/4.18 MJ) ranged from 0.4 (95% confidence interval [CI] 0.2– 0.8) for people younger than 65 years of age to 0.8 (95% CI 0.4– 1.7) for people older than 65 years.2 Similar outcomes were also observed in 2 larger studies. The results of the Nurse's Health Study and the U.S. Male Health Professionals Study showed that, after controlling for risk factors, people with higher lutein and zeaxanthin intakes were at decreased risk of cataract extraction.3,4 In the Nurse's Health Study, those in quintile 5, with a mean lutein and zeaxanthin intake of 11 685 μg, had a relative risk of cataracts of 0.88 (95% CI 0.75– 1.03) compared with those in quintile 1, whose mean lutein and zeaxanthin intake was 1172 μg.3 Similarly, in the U.S. Male Health Professionals Study, those in quintile 5, with a mean lutein and zeaxanthin intake of 6871 μg, had a relative risk of cataracts of 0.81 (95% CI 0.65–1.01) compared with those in quintile 1, whose mean lutein and zeaxanthin intake was 1300 μg.4
In contrast, Mares-Perlman and colleagues conducted one of the largest epidemiologic studies in this area, using data from the third National Health and Nutrition Examination Survey; among 8222 participants over 40 years of age, no inverse relation was found between dietary lutein and zeaxanthin intake and photographic evidence of early or late macular degeneration.5 However, no randomized clinical trials have been performed that examine the preventive effect of lutein against cataract formation.
Oxidative stress is a likely cause of age-related macular degeneration and cataract formation. Because lutein occurs natually in these tissues, the potentially protective effects of its antioxidative and photochemical properties are intriguing. Additional trials that confirm a prophylactic role for lutein against age-related degenerative processes are worth pursuing as a potential avenue for preventing ocular disease.
Sylvia Santosa Peter J.H. Jones School of Dietetics and Human Nutrition McGill University Ste. Anne-de-Bellevue, Qué.
Footnotes
This article has been peer reviewed.
Competing interests: None declared for Sylvia Santosa. Peter Jones is part owner of Nutritional Fundamentals for Health, a company that sells lutein as one of its products. This article was accepted for publication before CMAJ's conflict of interest policy regarding authors of commentaries and review articles was established (Conflicts of interests and investments. CMAJ 2004;171[11]:1313).
References
- 1.Krinsky NI, Landrum JT, Bone RA. Biologic mechanisms of the protective role of lutein and zeaxanthin in the eye. Ann Rev Nutr 2003;23:171-201. [DOI] [PubMed]
- 2.Lyle BJ, Mares-Perlman JA, Klein BE, Klein R, Greger JL. Antioxidant intake and risk of incident age-related nuclear cataracts in the Beaver Dam Eye Study. Am J Epidemiol 1999;149:801-9. [DOI] [PubMed]
- 3.Chasan-Taber L, Willett WC, Seddon JM, Stampfer MJ, Rosner B, Colditz GA, et al. A prospective study of carotenoid and vitamin A intakes and risk of cataract extraction in US women. Am J Clin Nutr 1999;70:509-16. [DOI] [PubMed]
- 4.Brown L, Rimm EB, Seddon JM, Giovannucci EL, Chasan-Taber L, Spiegelman D, et al. A prospective study of carotenoid intake and risk of cataract extraction in US men. Am J Clin Nutr 1999;70:517-24. [DOI] [PubMed]
- 5.Mares-Perlman JA, Fisher AI, Klein R, Palta M, Block G, Millen AE, el al. Lutein and zeaxanthin in the diet and serum and their relation to age-related maculopathy in the third national health and nutrition examination survey. Am J Epidemiol 2001;153:424-32. [DOI] [PubMed]


