Abstract
Background
Artificial intelligence-assisted teaching, as an innovative model that combines intelligent technology and personalized education, is increasingly being emphasized in higher medical education.
Methods
This study included 523 participants, with a valid response rate of 87.2%. An integrated model based on the ARCS motivation model and constructivist theory was developed to explore the factors influencing medical students’ learning outcomes in the context of AI-assisted instruction. Descriptive statistics were conducted using SPSS 23.0, and a structural equation model was constructed and validated using Amos 23.0. Mediation analysis was performed with Process (version 3.3.1).
Results
The study confirmed that teaching quality had a positive effect on learning motivation (β = 0.645, P < 0.001) and learning outcomes (β = 0.128, P = 0.032). Learning motivation positively influenced learning attitude (β = 0.822, P < 0.001) and learning satisfaction (β = 0.350, P < 0.001). Learning attitude had a positive impact on both learning satisfaction (β = 0.530, P < 0.001) and learning outcomes (β = 0.232, P = 0.020). Learning satisfaction was also positively associated with learning outcomes (β = 0.415, P < 0.001). The external environment had a positive effect on learning motivation (β = 0.449, P < 0.001) and learning outcomes (β = 0.101, P = 0.033). Moreover, learning motivation played a significant mediating role in the relationships between teaching quality and learning outcomes (β_inmedia = 0.343, 95% CI [0.273, 0.414]), as well as between the external environment and learning outcomes (β_inmedia = 0.287, 95% CI [0.218, 0.355]).
Conclusion
Teaching quality and external environment indirectly enhance medical learning outcomes by strengthening learning motivation. Learning motivation plays a key role in shaping learning attitude, satisfaction, and outcomes, confirming the positive value of AI-assisted teaching in optimizing learning mechanisms. This study contributes to the application of AI-assisted teaching in medical education and provides empirical support for improving medical students’ learning performance.
Keywords: Medical education, AI-assisted, Learning outcomes, ARCS model, Constructivist theory
Introduction
Background
With the rapid development of Artificial Intelligence (AI) technology, its application in the field of education is becoming increasingly widespread [1]. AI is capable of providing adaptive and personalized educational content through student feedback, helping students identify knowledge gaps and adjust their learning strategies in a timely manner [2]. The education of medical students is highly specialized, requiring both a solid theoretical foundation in the specialty and an emphasis on practical skills training [3]. The integration of AI technologies into medical education presents numerous opportunities to improve students’ knowledge, skills, and competencies, including generating virtual clinical cases and virtual patients, accelerating research outcomes, planning curricula and optimizing course development, providing personalized learning experiences, and enhancing students’ diagnostic and problem-solving skills [2, 4, 5]. These techniques not only help students better grasp theoretical knowledge but also greatly enhance their practical and clinical skills [6]. For instance, the use of a "chatbot utilizing standardized patient" platform that employs dialogue to simulate patient interactions can offer medical students an immersive and personalized learning experience, thereby enhancing their foundational knowledge acquisition and clinical reasoning skills [7]. Consequently, in the face of rapidly evolving knowledge and increasingly diverse clinical needs, AI demonstrates substantial potential as a vital tool and knowledge platform in medical education [8, 9].
Learning outcomes are influenced by a number of factors. Student learning is largely influenced by the teacher [10]. Hanaysha et al. [11] found that teacher competencies positively influence student achievement. Altinay et al. [12] stated in their study on the capacity building of trainee teachers that AI supports and motivates the learning process and can be effective in changing the needs and learning experiences of students. Therefore, teachers should carefully plan for the integration of AI into their lesson plans to enhance personalized learning. Constructivist theory posits that students occupy a central role in the learning process [13]. Research by Darmawan [14] indicates a robust correlation between the intensity of students’ interest in learning content, their propensity to engage actively, and their academic outcomes, with students who demonstrate an active learning disposition showing better performance in knowledge acquisition. In a study conducted by Yusup et al. [15], it was determined that both students’ attitudes and motivation have a significant impact on the learning process. In a study examining the adoption of AI-based academic support systems and their impact on student performance in higher education institutions in Malaysia and Pakistan, Dahri et al. [16]found that student satisfaction had a significant positive effect on academic achievement in both countries. Notably, digital literacy plays an increasingly important role in AI-mediated learning environments [17], as higher digital skills enhance students’ understanding and use of AI tools, thereby influencing their learning efficiency and outcomes [18]. Additionally, the efficacy of learning resources, platforms, and assessment methods has the potential to influence learning outcomes, particularly within the domain of artificial intelligence [19–21]. In their study, Priamono et al. [22]emphasized that the integration of artificial intelligence and mobile learning (m-learning), along with continuous updates to educators’ understanding of technological advancements, can foster a more interactive, personalized, and adaptive learning environment for students. The utilization of AI tools in generating highly unique and coherently structured content has also been demonstrated to provide students with rich resources for autonomous learning [23]. Chiu [24] emphasizes that generative AI can be particularly effective in motivating students to engage in self-regulated learning by offering immediate and personalized feedback. Similarly, Sasikala et al. [25] posit that AI-driven adaptive learning systems can enhance student engagement. They argue that AI tools, including intelligent tutoring systems and virtual simulations, are more responsive to individual learning needs, thereby improving students’ test performance and overall learning outcomes. Therefore, this study summarizes the main factors affecting learning outcomes as comprising teachers, students, and the external environment.
Amid the gradual integration of AI technologies into educational practice, numerous studies have examined their impact on students’ learning processes and outcomes from various theoretical perspectives. For example, Self-Determination Theory (SDT) emphasizes that learners’ intrinsic motivation arises from the fulfillment of needs for autonomy, competence, and relatedness [26–28]. Chiu et al. [29] connected educational AI with the basic psychological needs framework within SDT to explore how satisfying these needs influences students’ intrinsic motivation for learning with AI technologies. However, SDT primarily focuses on the psychological mechanisms underlying motivation generation, revealing key factors in motivation formation but offering limited concrete guidance for instructional practice [30]. Cognitive Load Theory (CLT) posits that human working memory capacity is limited and that excessive cognitive demands impede learning and memory [31, 32]. Thus, CLT highlights optimizing instructional content and presentation to reduce unnecessary cognitive load. Edwards et al. [33] found that AI chatbots can alleviate cognitive load through adaptive content recommendations, thereby enhancing student memory and learning outcomes. Nonetheless, CLT has been criticized for overemphasizing teacher-directed instruction while neglecting the value of exploratory and metacognitive strategies in learning [34]. Additionally, some research suggests that reducing cognitive load is not always desirable, supporting the view that strategically challenging cognition can promote expertise development [35]. In contrast, constructivist learning theory emphasizes students’ active construction of knowledge and meaning through interaction with contexts, tasks, and others during the learning process [36]. This theory aligns well with AI-assisted teaching’s emphasis on personalized, inquiry-based, and feedback-driven learning characteristics. Empirical studies by Do et al. [37] demonstrate that constructivist environments significantly enhance learning motivation and strategy use. Based on constructivism, Adigun [38] proposed the “Triple Loop Engagement” model, advocating the integration of task-driven and contextual support in instructional design to cultivate students’ autonomous learning capabilities and knowledge integration. Furthermore, motivation, as a key psychological variable influencing learning outcomes, is equally crucial in AI-assisted teaching. The ARCS motivation model offers a structured instructional design framework aimed at stimulating and sustaining learner motivation [39]. A meta-analysis by Goksu and Islam [40] revealed that the ARCS model significantly enhances students’ motivation and academic achievement across diverse educational settings and stages, demonstrating strong applicability. Fang et al. [41] noted that the model’s application in educational research has primarily focused on instructional design, theoretical foundations, and measurement tools, suggesting that future work should integrate additional theories to broaden its explanatory power. Therefore, this study is grounded in these two theoretical frameworks to investigate factors influencing medical students’ learning within AI-assisted teaching models.
Conceptual framework
This study integrates constructivist theory and the ARCS model to develop an integrated model (hereafter referred to as the integrated model) that encompasses students, teachers, and the external environment, aiming to investigate the learning outcomes of medical students under the AI-assisted teaching model.
Constructivist theory is an important theory in the field of education. This theory posits that students are the center of education and that learning requires students to take control and construct knowledge independently [13]. It emphasizes that learning is an active process, where students build knowledge through experiences and interactions with their environment, developing their understanding through exploration, reflection, and discussion [42]. The core of this theory lies in learners’ initiative and participation [43]. In teaching, AI products such as chatbots and virtual assistants can provide students with abundant resources and immediate feedback, offering them opportunities to fully exercise their agency, thereby promoting the development of divergent, creative, and critical thinking, and providing broad opportunities for cognitive growth [44].
Motivation is closely related to students’ learning outcomes and is an important topic in educational research [41]. The ARCS model, proposed by Keller, aims to enhance learning motivation [39]. This model focuses on these four elements to create diversified instructional designs that aim to stimulate learners’ interest in knowledge acquisition and boost their learning motivation, making the ARCS model widely applied in the field of education [45]. Related research shows that in AI-assisted educational environments, the ARCS model can effectively help teachers stimulate students’ learning motivation during the teaching process [46]. Moreover, research by Yeol-Eo Chun and colleagues has found that AI-based adaptive learning can offer personalized content based on medical students’ levels, more effectively motivating learning, optimizing the learning process, and improving learning outcomes [47].
The integration of the ARCS motivational model with constructivist learning theory offers theoretical support for AI-assisted teaching. The integration of the ARCS motivational model with constructivist learning theory offers theoretical support for AI-assisted teaching [48, 49]. In this study, the two frameworks are integrated within AI-supported instructional settings. Specifically, educators can draw on the ARCS model to design diverse and personalized instruction using AI technologies, thereby enhancing students’ intrinsic motivation and promoting engagement and learning effectiveness [50]. However, traditional applications of the ARCS model often lack interactivity [51], which is a key factor affecting students’ critical thinking, creativity, and academic performance [40]. In contrast, constructivism emphasizes learners’ active exploration, social interaction, and contextual practice in constructing knowledge, highlighting their central role in learning [52]. In AI-assisted environments, students can develop clinical reasoning through interaction with generative AI, while achieving social validation of knowledge through discussions with teachers and peers. Therefore, the ARCS model provides a systematic pathway for motivating learners, while constructivism plays a complementary role in enhancing interactivity, learner agency, and knowledge construction. The integration of these two theories not only addresses the limitations of each framework but also offers theoretical support and practical guidance for delivering personalized and highly engaging learning experiences in AI-supported educational settings.
Significance of the study
Priamono et al. emphasized in their research that integrating AI and mobile learning, along with updating educators’ understanding of technological advancements, can create a more interactive, personalized, and adaptive learning environment for students [22]. AI tools can generate highly unique and coherent content, providing students with abundant self-learning resources [23]. In the context of AI-assisted instruction, students not only interact with teachers and peers, but also engage deeply with AI technologies—such as chatbots—to obtain immediate feedback and construct personalized knowledge [53, 54]. While many current studies focus primarily on the key factors of teachers and students in relation to learning outcomes, they often lack a comprehensive consideration of the external environment. In addition, artificial intelligence—such as large language models—can play a significant role in medical education by providing personalized learning experiences, generating realistic patient case scenarios, enhancing textbook content, and summarizing medical research [55]. Although numerous studies have shown that AI can improve student learning outcomes [56–58], there is still a lack of research on how AI-assisted instruction specifically influences the learning outcomes of medical students. Therefore, this study integrates the ARCS motivational model with constructivist learning theory by incorporating the “student-external environment” dimension into the interaction pathway. A theoretical framework centered on the “teacher-student-external environment” triad is proposed to uncover the internal mechanisms by which multiple factors work together to enhance learning outcomes in AI-supported teaching environments. This offers a new theoretical perspective for understanding the factors that influence learning effectiveness in medical education.
Research objectives
This study aims to explore the factors influencing medical students’ learning outcomes under an AI-assisted instructional model. Based on constructivist learning theory and the ARCS motivation model, a “teacher-student-external environment” theoretical framework is established to identify key influencing factors and verify their impact pathways. Through empirical research, the study seeks to explore the potential of large language models in facilitating knowledge construction, improving academic performance, and enhancing clinical reasoning skills among medical students, thereby providing a reference for optimizing instructional design and teaching models in medical education.
Method
Research model design
This study conducts an analysis of the factors influencing the learning outcomes of medical students in the context of AI-assisted instruction, focusing on three key dimensions: teachers, students, and the external environment. At the teacher level, it is emphasized that teachers should design teaching strategies based on teaching objectives, enrich curriculum content to improve teaching quality, and use diversified teaching methods to stimulate students’ interest in learning, foster their learning motivation, and promote the comprehensive development of students in the AI-assisted teaching environment [59, 60]. At the student level, it is emphasized that students should be fully aware of the teaching methods, with an emphasis on active exploration and discovery in their learning process. Starting from their motivation to learn, students should correct their attitudes towards learning and reasonably formulate learning plans based on their actual situations, which plays a role in enhancing learning outcomes. Additionally, the influence of external factors, such as learning resources, learning platforms, and assessment methods, is also considered [19]. It can be concluded that the quality of AI-assisted teaching, learning motivation, learning attitudes, learning satisfaction, and the external environment are key determinants of learning outcomes in AI-assisted teaching models.
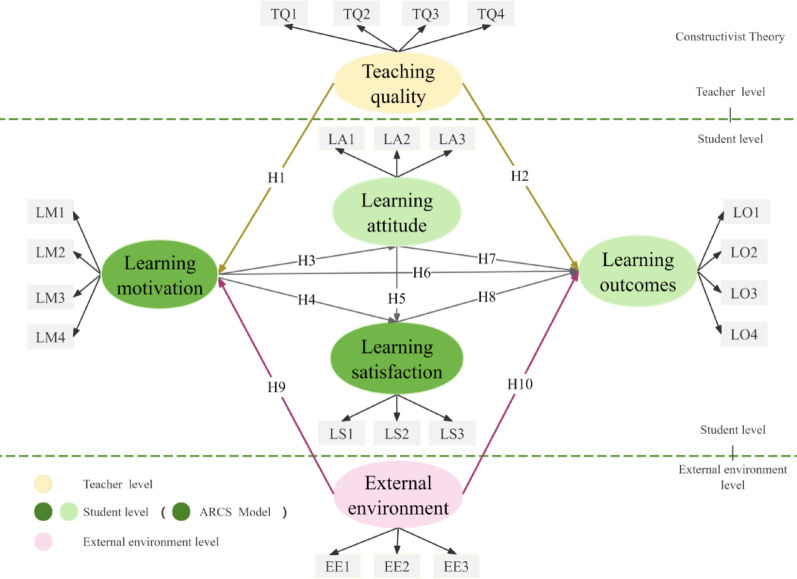
Therefore, based on constructivist theory and the ARCS model, this study developed a theoretical framework to examine the learning outcomes of medical students within a student-centered AI-assisted teaching approach. The framework incorporates the dimensions of student, teacher, and external environment, with learning motivation as a mediating variable, as illustrated in Fig. 1.
Fig. 1.
Integrated modeling framework based on the ARCS model and constructivist theory
Teacher level
Teaching quality refers to the level of instruction and its effectiveness, or the extent to which students’ developmental changes meet certain standards over a specified period of time and under certain conditions, as measured by how well teaching objectives and the educational goals of individual schools are achieved [61]. In this study, teaching quality is quantified through student evaluations, with assessment dimensions encompassing the scientific accuracy and coherence of the instructional content, the clarity of learning objectives, the appropriateness of instructional organization, and the comprehensiveness of assessment methods. These dimensions are rated by students based on their classroom experiences, thereby reflecting their perceived level of teaching quality. In an AI-driven teaching and learning environment, teachers can utilize AI technology to generate and optimize course materials, such as handouts, exercises, and case studies, while quickly updating content based on the latest academic research and real-time industry developments [62]. Studies have shown that AI-assisted teaching can significantly enhance the teaching quality for medical students [6, 63].
Learning motivation refers to the behavioral drives that encourage people to pursue goals, cognitive beliefs, and emotional responses [64]. Learning motivation is primarily driven by two factors: internal and external drivers. In the context of AI, learning motivation is influenced by AI technology, which enhances students’ interest and engagement through personalized learning, instant feedback, and contextually relevant tasks, but AI anxiety can diminish learning motivation and negatively impact students’ perceptions and enjoyment of learning AI [65]. For medical students, learning motivation plays a key role in increasing their interest and drive to learn [66]. Empirical studies have shown that teaching quality can have a significant positive impact on medical students’ motivation to learn [67]. Faculty can use AI tools to modify content, instructional design, and other strategies to improve teaching quality and thereby boost student motivation [68]. Therefore, we propose the following hypothesis:
H1:
Teaching quality has a positive impact on learning motivation.
Learning outcomes are statements of what a learner knows, understands, and is able to do after completion of learning [69]. In this study, learning outcomes specifically denote students’ improvements in academic performance, enhancement of clinical competence, and attainment of learning objectives through AI-assisted learning. These outcomes can be reflected through self-assessments and course grades. Related studies have shown that AI-driven instructional quality has a positive impact on learning outcomes [70]. Therefore, we hypothesize the following:
H2:
Teaching quality has a positive impact on learning outcomes.
Student level
Learning attitude refers to a latent, abstract mental state that learners exhibit during the learning process, encompassing both emotional and cognitive judgments [71]. Jiang et al. explored the relationship between students’ motivation and learning attitude in a study of online language learning within a virtual classroom [72]. Wei et al. found that stronger student motivation leads to better learning attitudes, resulting in higher emotional satisfaction and a greater willingness to learn in a large language model based intelligent collaborative learning model [73]. Therefore, we hypothesize the following:
H3:
Learning motivation has a positive impact on learning attitude.
Learning satisfaction refers to students’ attitudes and feelings toward their own learning activities [74]. It reflects the learning outcomes of medical students. A study on college students’ online learning and academic achievement satisfaction has demonstrated that learning motivation positively impacts learning satisfaction [75]. Research on case-based teaching in nursing education has also demonstrated that learning motivation positively influences learning outcomes [76]. Meanwhile, a study on high school students’ learning outcomes in computer courses found that learners’ attitudes have a positive effect on learning satisfaction [77]. Based on these findings, we hypothesize the following:
H4:
Learning motivation has a positive impact on learning satisfaction.
H5:
Learning attitude has a positive impact on learning satisfaction.
H6:
Learning motivation has a positive impact on learning outcomes.
A study on the learning attitudes of middle school students confirmed that learning attitude has a positive impact on learning outcomes. A positive learning attitude enhances students’ learning outcomes, while a negative learning attitude inhibits them [78]. A study on students’ online video lectures found that learning satisfaction has a significant positive impact on learning outcomes [79]. Based on these findings, we hypothesize the following:
H7:
Learning attitude has a positive impact on learning outcomes.
H8:
Learning satisfaction has a significant positive impact on learning outcomes.
External environment level
In attribution theory, the external environment is one of the key factors influencing outcomes. The learning outcomes of medical students in an intelligent context are not only influenced by the students themselves and their teachers but also by external factors such as learning resources, collaborative environments, and learning support systems. These external factors can have varying degrees of impact on learning motivation. In this study, the external environment refers to the technological tools, learning platforms, and resource support that learners encounter during AI-assisted instruction, as well as their ability to utilize these conditions to effectively engage in the learning context and complete learning tasks. This variable was operationalized through a questionnaire, with specific dimensions including the accessibility of large language models, the ease of use and practicality of the platforms, and the functional completeness and operational stability during use. Research has shown that the external environment in an intelligent context significantly affects learning outcomes [80]. A study on the impact of online learning resource selection on teacher satisfaction found that abundant learning resources are beneficial for improving students’ learning outcomes [81]. Studies evaluating learning outcomes have confirmed that different assessment methods lead to variations in learning outcomes. Based on these findings, the following hypotheses are proposed:
H9:
The external environment has a positive impact on learning motivation.
H10:
The external environment has a significant impact on learning outcomes.
Mediating effects of learning motivation
Through the literature review of the above research variables, it can be seen that learning motivation can serve as a mediating variable [82], whereby the independent variable can indirectly affect the dependent variable through the mediating role of learning motivation. Therefore, the following hypotheses are proposed:
H11:
Learning motivation mediates the relationship between teaching quality and learning outcomes.
H12:
Learning motivation mediates the relationship between the external environment and learning outcomes.
Scale design
The questionnaire is divided into two parts. The first part collects demographic information, including gender, grade, and major. The second part consists of six core constructs: teaching quality, learning motivation, learning attitude, learning satisfaction, learning outcomes, and external environment, with no fewer than three questions for each construct [83].
The survey questionnaire in this study was based on scales from relevant literature: teaching quality (TQ) [84], learning motivation (LM) [85], learning attitude (LA) [86], learning satisfaction (LS) [87], learning outcomes (LO) [88], and external environment (EE) [89, 90]. However, a pre-survey revealed that simply replicating existing questionnaires could not fully adapt to the context and needs of this study. Therefore, the research team conducted multiple revisions to improve the applicability of the questionnaire, optimizing the phrasing of items and structural setup to ensure that the questionnaire accurately reflects the research topic and possesses high validity and reliability.
During the pre-survey phase, we analyzed items with low CIT (Corrected Item-Total Correlation). When an item’s CIT value was less than 0.5, and deleting the item led to an increase in Cronbach’s α coefficient compared to the overall scale, we removed the item to improve the internal consistency of the scale. To ensure the validity of the measurements for each dimension, we redesigned some of the item statements, ensuring that each dimension retained at least three measurement items. All designs used a five-point Likert scale, ranging from "Strongly Disagree" to "Strongly Agree," with a scoring range of 1 to 5. The measurement for each dimension was calculated based on the average score of the items in that dimension. After multiple adjustments and validations, the final questionnaire demonstrated good internal consistency, structural reliability, and convergent validity.
Data collection
Prior to the formal survey, a pilot study was conducted via an online platform involving 80 medical students who had used large language models (such as ERNIE Bot, Doubao, Qwen, SparkDesk, etc.) in their learning. The aim was to assess the applicability of the questionnaire and refine the survey items. Based on the feedback from the pilot, several items were revised to ensure that all questions effectively reflected the research objectives, thereby enhancing the overall quality and reliability of the questionnaire.
In the formal survey, a simple random sampling method was employed. The research team obtained a complete list of students (including non-sensitive information such as names and student ID numbers) from the course selection system managed by the Academic Affairs Office, which served as the sampling frame. Using a computer-based random number generator, students were assigned numbers and randomly selected to ensure that each eligible student had an equal probability of being chosen. The selected students were then invited to participate in the survey through both online (Sojump, email) and offline (paper-based) channels, with a total of 600 questionnaires distributed. An initial batch of 225 questionnaires was distributed online to evaluate data quality, achieving a response rate of over 90%. Upon confirming data quality, the remaining questionnaires were subsequently administered.
During the data collection phase, a total of 540 questionnaires were returned. First, invalid questionnaires—such as those that were incomplete or had a very short response time—were excluded based on the inclusion and exclusion criteria. Then, missing values were examined. To assess the randomness of the missing data, Little’s MCAR test was conducted, and the results showed P > 0.05, indicating that the data were missing completely at random (MCAR). Therefore, for a small amount of missing data (< 5%), mean imputation was applied. Questionnaires with a large proportion of missing data were excluded from the analysis. Ultimately, 523 valid questionnaires were included, resulting in an effective response rate of 87.2%, which meets the minimum sample size requirement for structural equation modeling (SEM) based on the "10-times rule." Informed consent was obtained from all participants and/or their legal guardians.
Data processing and statistical analysis tools
To ensure the rigor and scientific validity of data analysis, this study employed multiple statistical tools. First, Excel was used for preliminary data management. SPSS 23.0 was applied to conduct descriptive analyses of demographic characteristics and to explore correlations among variables. Structural Equation Modeling (SEM) was performed using AMOS 23.0 to quantify the causal relationships among latent variables. During model fit evaluation, fit indices such as CMIN/df and RMSEA were calculated to assess the model’s goodness of fit. AMOS 23.0 was also used to estimate factor loadings between latent constructs and observed variables, and to report path coefficients, composite reliability (CR), and significance levels (P < 0.05). Mediation effect analysis was conducted using the PROCESS macro (version 3.3.1) in SPSS. Through this comprehensive analysis, the key factors influencing medical students’ learning outcomes under AI-assisted instruction were identified.
Result
Demographic characterization
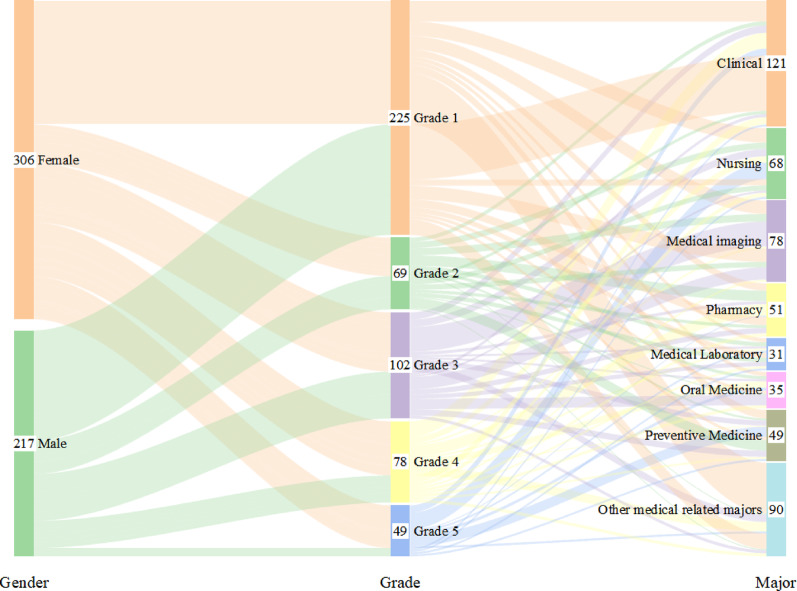
This study was analyzed demographically using SPSS 23.0, and the characteristics of the participants are shown in Fig. 2. In terms of gender, there were 306 female students (58.5%) and 217 male students (41.5%). In terms of specialty distribution, 23.1% were in the five-year clinical medicine program, 13% were in the nursing program, 14.9% were in the medical imaging program, 9.8% were in the pharmacy program, 5.9% were in the medical testing program, 6.7% were in the dentistry program, 9.4% were in the preventive medicine program, and 17.2% were in the other medical-related programs. In terms of grade distribution, there were 225 freshmen, 69 sophomores, 102 juniors, 78 seniors, and 49 seniors. Furthermore, non-parametric tests were performed to examine differences in learning outcomes across gender, academic year, and major. The results indicated no statistically significant differences among these groups—gender (Z = -0.044, p > 0.05), academic year (H = 1.638, p > 0.05), and major (H = 5.039, p > 0.05). Overall, the sample structure of the survey is reasonable and can effectively support the model validation of the impact of AI-assisted teaching on learning outcomes.
Fig. 2.
Demographic characteristics (output from SPSS 23.0)
Model result
Prior to conducting the analysis, it was necessary to verify whether the data conformed to the assumption of normality required for structural equation modeling (SEM). According to Kline [91], skewness values within ± 3 and kurtosis values within ± 10 are considered acceptable indicators of normal distribution. In this study, the skewness values ranged from -1.080 to -0.551, and the kurtosis values ranged from -0.311 to 0.975. Based on Kline’s criteria, the data in this study can be considered to meet the requirements of normal distribution. In addition, to assess potential multicollinearity issues, the variance inflation factor (VIF) was used. Following the recommendations of Kock [92] and Gaskin [93], a VIF value exceeding 3.3 may indicate multicollinearity problems. In this study, all VIF values ranged from 1.541 to 2.462, suggesting that multicollinearity was not a concern.
In this study, all major constructs were measured using validated Likert-scale instruments. To ensure the reliability of the collected data and the robustness of subsequent analyses, internal consistency was assessed through Cronbach’s alpha coefficients. A Cronbach’s alpha value of 0.70 or higher is generally considered acceptable for research purposes. As presented in Table 1, all constructs demonstrated Cronbach’s alpha values ranging from 0.70 to 1.00, indicating that the scales employed in this study demonstrated strong internal consistency and high reliability.
Table 1.
Results of Reliability and Validity Analysis for Each Construct: Factor Loadings, Internal Consistency, and Convergent Validity
| Facet | Item | Parameter significance estimation | Factor loading | Cronbach’s ɑ | Composite reliability | Convergent validity | |||
|---|---|---|---|---|---|---|---|---|---|
| Unstd | S.E | C.R | P | Std | ɑ | CR | AVE | ||
| TQ | TQ1 | 1.000 | 0.691 | 0.801 | 0.804 | 0.507 | |||
| TQ2 | 1.136 | 0.077 | 14.774 | *** | 0.781 | ||||
| TQ3 | 0.978 | 0.070 | 13.896 | *** | 0.716 | ||||
| TQ4 | 0.960 | 0.074 | 12.898 | *** | 0.655 | ||||
| LM | LM1 | 1.000 | 0.683 | 0.805 | 0.818 | 0.530 | |||
| LM2 | 1.067 | 0.081 | 13.182 | *** | 0.775 | ||||
| LM3 | 1.040 | 0.082 | 12.745 | *** | 0.706 | ||||
| LM4 | 1.016 | 0.078 | 13.039 | *** | 0.745 | ||||
| LA | LA1 | 1.000 | 0.685 | 0.784 | 0.764 | 0.519 | |||
| LA2 | 1.103 | 0.075 | 14.782 | *** | 0.761 | ||||
| LA3 | 1.030 | 0.073 | 14.035 | *** | 0.713 | ||||
| LS | LS1 | 1.000 | 0.787 | 0.783 | 0.779 | 0.511 | |||
| LS2 | 0.987 | 0.065 | 15.242 | *** | 0.729 | ||||
| LS3 | 0.833 | 0.057 | 14.607 | *** | 0.688 | ||||
| EE | EE1 | 1.000 | 0.755 | 0.819 | 0.820 | 0.602 | |||
| EE2 | 0.992 | 0.062 | 15.910 | *** | 0.787 | ||||
| EE3 | 1.018 | 0.064 | 15.902 | *** | 0.786 | ||||
| LO | LO1 | 1.000 | 0.700 | 0.810 | 0.808 | 0.513 | |||
| LO2 | 1.018 | 0.069 | 14.754 | *** | 0.696 | ||||
| LO3 | 0.970 | 0.069 | 13.985 | *** | 0.658 | ||||
| LO4 | 0.966 | 0.066 | 14.661 | *** | 0.691 | ||||
TQ, teaching quality; LM learning motivation; LA, learning attitude; LS, learning satisfaction; EE, external environment; LO, learning outcomes
***At the 0.001 level (2 tailed), the correlation was significant
To assess the convergent validity [94]and composite reliability [95]of each construct, standardized factor loadings of the measurement items on their respective latent variables were calculated. These values were then used to compute the Average Variance Extracted (AVE) and Composite Reliability (CR) for each dimension. According to established criteria, an AVE of 0.50 or higher and a CR of at least 0.70 are required to demonstrate acceptable convergent validity and composite reliability [96–98]. As shown in Table 1, all constructs in this study achieved AVE values above 0.50 and CR values exceeding 0.70, indicating satisfactory convergent validity and composite reliability across all dimensions.
Validity refers to the extent to which a comprehensive evaluation system accurately reflects its intended objectives and requirements. It indicates the accuracy with which a measurement tool captures the characteristics it is designed to measure. Higher validity suggests that the results more effectively represent the targeted construct, whereas lower validity implies less accurate measurement. Discriminant validity (DV) is used to quantify the distinctiveness of conceptually unrelated constructs. It aims to demonstrate evidence of differentiation based on the variance among all components. According to standard evaluation criteria for validity, discriminant validity is supported when the square root of the AVE on the diagonal exceeds 0.70 and is greater than the correlation coefficients between constructs. As shown in Table 2, the square root of the AVE for each construct exceeds 0.70 and is greater than the corresponding inter-construct correlations, indicating that the model in this study demonstrates a high level of discriminant validity.
Table 2.
Discriminant validity test results
| Variables | TQ | LM | LA | LS | EE | LO |
|---|---|---|---|---|---|---|
| TQ | 0.712 | |||||
| LM | 0.624** | 0.728 | ||||
| LA | 0.522** | 0.669** | 0.720 | |||
| LS | 0.490** | 0.619** | 0.659** | 0.736 | ||
| EE | 0.449** | 0.520** | 0.446** | 0.525** | 0.776 | |
| LO | 0.615** | 0.727** | 0.718** | 0.730** | 0.557** | 0.716 |
TQ, teaching quality; LM, learning motivation; LA, learning attitude; LS, learning satisfaction; EE, external environment; LO, learning outcomes
**At the 0.01 level (2 tailed), the correlation was significant
Evaluation of structural equation modeling
Model fit was evaluated using several indices, including absolute fit indices such as the relative chi-square (CMIN/df) and the Root Mean Square Error of Approximation (RMSEA), as well as incremental fit indices such as the Incremental Fit Index (IFI), Tucker-Lewis Index (TLI), and Comparative Fit Index (CFI). A lower relative chi-square value indicates better model fit, with values between 1 and 5 generally considered acceptable, as this metric is less sensitive to sample size. IFI, TLI, and CFI range from 0 to 1, with values closer to 1 indicating a better fit. RMSEA assesses the degree of approximation between the model and the observed data; values below 0.08 are indicative of a good fit. According to the model fit results (RMSEA = 0.057, CMIN/df = 2.685, IFI = 0.943, TLI = 0.933, CFI = 0.943), all indices were within acceptable or good ranges. Therefore, it can be concluded that the proposed structural equation model fits the survey data well, and the relationships among variables in the model are well supported by the data.
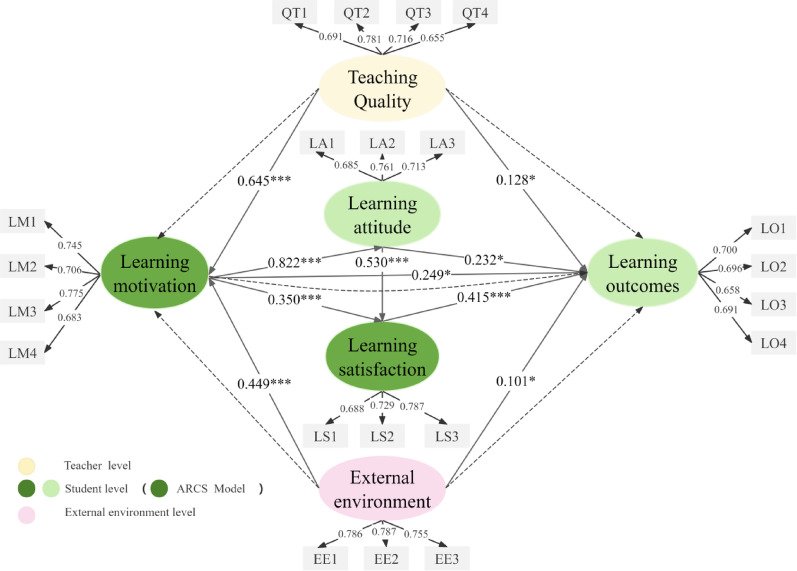
According to the results presented in Table 3 and Fig. 3, the path analysis of the current study revealed several statistically significant relationships. Specifically, teaching quality had a significant positive effect on learning motivation (β = 0.645, P < 0.001), and the external environment also exerted a significant positive influence on learning motivation (β = 0.449, P < 0.001). Learning motivation showed a significant positive association with learning attitude (β = 0.822, P < 0.001), which in turn had a significant positive effect on learning satisfaction (β = 0.530, P < 0.001). Additionally, learning motivation directly and positively influenced learning satisfaction (β = 0.350, P < 0.001). Furthermore, significant positive effects were found between learning motivation and learning outcomes (β = 0.249, P = 0.034), teaching quality and learning outcomes (β = 0.128, P = 0.032), external environment and learning outcomes (β = 0.101, P = 0.033), learning attitude and learning outcomes (β = 0.232, P = 0.020), and learning satisfaction and learning outcomes (β = 0.415, P < 0.001).
Table 3.
Table of path coefficients
| Path | Non-standardized path | Standardized path | S.E | C.R | P | Conclusion | ||
|---|---|---|---|---|---|---|---|---|
| LM | < –- | TQ | 0.544 | 0.645 | 0.052 | 10.410 | *** | Support |
| LM | < –- | EE | 0.349 | 0.449 | 0.039 | 8.874 | *** | Support |
| LA | < –- | LM | 0.895 | 0.822 | 0.078 | 11.459 | *** | Support |
| LS | < –- | LA | 0.584 | 0.530 | 0.120 | 4.884 | *** | Support |
| LS | < –- | LM | 0.420 | 0.350 | 0.125 | 3.363 | *** | Support |
| LE | < –- | LM | 0.272 | 0.249 | 0.128 | 2.124 | 0.034 | Support |
| LO | < –- | TQ | 0.118 | 0.128 | 0.055 | 2.149 | 0.032 | Support |
| LO | < –- | LA | 0.233 | 0.232 | 0.100 | 2.318 | 0.020 | Support |
| LO | < –- | LS | 0.377 | 0.415 | 0.083 | 4.534 | *** | Support |
| LO | < –- | EE | 0.085 | 0.101 | 0.040 | 2.134 | 0.033 | Support |
TQ, teaching quality; LM, learning motivation; LA, learning attitude; LS, learning satisfaction; EE, external environment; LO, learning outcomes
***At the 0.001 level (2 tailed), the correlation was significant
Fig. 3.
Results of integrated model (Indicators of model fit: RMSEA = 0.057, CMIN/df = 2.685, IFI = 0.943, TLI = 0.933, CFI = 0.943). ***. At the 0.001 level (2 tailed), the correlation was significant. *. At the 0.05 level (2 tailed), the correlation was significant
Mediation effect test
The stepwise regression-based mediation analysis was conducted using the PROCESS macro developed by Andrew Hayes. As shown in Table 4, the first step revealed that both teaching quality and external environment had significant positive effects on learning outcomes (β = 0.601, P < 0.001; β = 0.514, P < 0.001), indicating that the total effects were significant. In the second step, teaching quality and external environment were also positively associated with learning motivation (β = 0.592, P < 0.001; β = 0.465, P < 0.001). In the third step, both teaching quality and external environment continued to show significant positive effects on learning outcomes (β = 0.258, P < 0.001; β = 0.227, P < 0.001), and learning motivation had a significant positive impact on learning outcomes as well (β = 0.579, P < 0.001; β = 0.617, P < 0.001). These results indicate that learning motivation plays a partial mediating role in the relationships examined.
Table 4.
Results of the mediation effect test for learning motivation
| Facets | Steps | Implicit variables | Independent variables | R | R-sq | F | β | t | Type of mediation |
|---|---|---|---|---|---|---|---|---|---|
| TQ | initial step | LO | TQ | 0.615 | 0.378 | 316.986*** | 0.601 | 17.804*** | partial mediation |
| second step | LM | TQ | 0.624 | 0.390 | 332.521*** | 0.592 | 18.235*** | ||
| third step | LO | TQ | 0.756 | 0.571 | 346.571*** | 0.258 | 7.184*** | ||
| LM | 0.579 | 15.305*** | |||||||
| EE | initial step | LO | EE | 0.557 | 0.311 | 234.806*** | 0.514 | 15.323*** | partial mediation |
| second step | LM | EE | 0.520 | 0.270 | 192.750*** | 0.465 | 13.883*** | ||
| third step | LO | EE | 0.757 | 0.573 | 348.829*** | 0.227 | 7.330*** | ||
| LM | 0.617 | 17.871*** |
TQ, teaching quality; LM, learning motivation; LA, learning attitude; LS, learning satisfaction; EE, external environment; LO, learning outcomes
***At the 0.001 level (2 tailed), the correlation was significant
The mediating role of learning motivation between teaching quality and learning outcomes, as well as between external environment and learning outcomes, was tested using the Bootstrap method. According to the analysis results in Table 5, the indirect effect values were 0.343 and 0.287, with 95% confidence intervals of [0.273, 0.414] and [0.218, 0.355], respectively. Since the confidence intervals did not include zero, the indirect effects were considered statistically significant, indicating that learning motivation played a significant mediating role in the model [99]. The proportion of the total effect accounted for by learning motivation was 57% and 56%, respectively.
Table 5.
Bootstrap mediation effect test results
| Facet | Relation of effect |
Efficacy value |
LLCI | ULCI | Efficiency ratio |
|---|---|---|---|---|---|
| TQ | Total effect | 0.601 | 0.534 | 0.667 | |
| Direct effect | 0.258 | 0.187 | 0.328 | 43% | |
| Indirect effect | 0.343 | 0.273 | 0.414 | 57% | |
| EE | Total effect | 0.514 | 0.448 | 0.579 | |
| Direct effect | 0.227 | 0.166 | 0.287 | 44% | |
| Indirect effect | 0.287 | 0.218 | 0.355 | 56% |
TQ, teaching quality; LM, learning motivation; LA, learning attitude; LS, learning satisfaction; EE, external environment; LO, learning outcomes
Discussion
The study findings indicate that teaching quality and external environment are key driving factors in enhancing medical students’ learning motivation under AI-assisted teaching models. Increased learning motivation, in turn, facilitates the development of positive learning attitudes and higher levels of learning satisfaction. Moreover, learning attitude has a direct positive effect on satisfaction. Teaching quality, external environment, learning motivation, learning attitude, and learning satisfaction all exert a positive influence on educational outcomes within AI-assisted medical education. Notably, learning motivation plays a significant mediating role between teaching quality, external environment, and learning outcomes. As shown in Fig. 4, instructors can leverage large language models to optimize instructional design, clarify educational objectives, and enhance the professionalism and adaptability of teaching content. By aligning the curriculum with clinical practice, educators can promote students’ active construction of medical knowledge. Thoughtful design of teaching materials and learning environments can enhance learners’ concentration and confidence, while AI-powered interactions may stimulate intrinsic motivation and foster positive learning attitudes. This supports the development of a virtuous cycle of “motivation–attitude–satisfaction.” Furthermore, medical schools, AI development teams, and healthcare institutions should collaborate to build intelligent resource repositories, data-driven assessment tools, virtual collaboration platforms, and real-time support systems. These efforts will deepen the integration of AI into medical education settings, thereby improving educational efficiency, strengthening students’ professional competencies, and cultivating talent for intelligent healthcare systems—ultimately contributing to the development of a high-quality workforce for future smart healthcare.
Fig. 4.
Analysis of Factors Influencing Learning Outcomes
Teacher level
Based on the results of the structural equation model, this study demonstrates that in AI-assisted teaching environments, teaching quality positively influences both learning motivation and learning outcomes, supporting hypotheses H1 and H2. In addition, mediation analysis confirmed that learning motivation mediates the relationship between teaching quality and learning outcomes, thus supporting hypothesis H11.
Teaching quality has a positive impact on both learning motivation and learning outcomes. AI technologies provide educators with instructional design support, enabling them to develop more targeted teaching tasks aligned with educational goals, thereby enhancing teaching quality and stimulating students’ intrinsic motivation [100]. This finding aligns with the study by Sajja [101], which suggested that AI can assist educators in organizing teaching processes more effectively, significantly improving instructional efficiency and student learning outcomes. Moreover, AI can enhance teachers’ digital literacy and computing skills, help them identify students’ learning styles, and encourage the adoption of diversified instructional strategies, thereby improving teaching quality, which plays an important role in enhancing students’ learning motivation [102, 103]. This finding is consistent with the results of the present study. Notably, as AI is increasingly integrated into the classroom, the role of educators is shifting from traditional knowledge transmitters to instructional designers and learning facilitators [104]. However, many medical educators still lack systematic AI training and professional support, which limits the effective integration of AI into curricula [105]. To address this, targeted training programs, teaching workshops, and interdisciplinary collaborations with AI experts are recommended to enhance educators’ competencies in technology implementation, ethical decision-making, clinical integration, and pedagogical strategy [106, 107].
In addition, curriculum integration strategies are critical for the effective implementation of AI-based instruction. At the undergraduate level, the already heavy course load, coupled with resistance from traditional values and accreditation procedures, poses challenges to incorporating new AI-related content. Furthermore, most faculty members lack the necessary technical background, making implementation difficult [108]. To address these challenges, Grunhut et al. [108] suggest adopting a longitudinal integration approach by embedding AI as a thematic thread within existing courses—for example, introducing AI input evaluation in evidence-based medicine modules—to reduce instructional burden while enhancing curricular relevance. Moreover, strengthened collaboration among universities, teaching teams, and technology developers is essential to ensure that AI-related educational content aligns closely with the broader goals of medical training. Pupic [105] further recommends introducing AI education early in undergraduate programs and deepening it at the postgraduate level to establish a progressively structured developmental pathway.
Learning motivation served as a mediating factor between teaching quality and learning outcomes. Boadu et al. [109] further confirmed that student motivation mediates the relationship between teaching quality and academic achievement, which also supports the mediating effect of learning motivation found in our study. Therefore, while improving instructional quality, medical educators should also leverage AI tools to stimulate students’ learning motivation. For example, large language models can be used to facilitate interactive case analysis, terminology training, and clinical reasoning exercises, thereby enhancing student engagement and enthusiasm for learning [110]. For students with a solid foundation in medical knowledge, instructors may also guide them to apply machine learning techniques in data analysis and predictive modeling, thereby strengthening their ability to apply knowledge in practical contexts [111]. The flexible use of AI tools not only supports improvements in teaching quality and student motivation but also helps create a more professionally relevant and personalized learning environment for medical students, ultimately promoting better overall learning outcomes.
Student level
According to the results of the structural equation modeling, in the AI-assisted teaching model, learning motivation has a positive effect on learning attitude; both learning motivation and learning attitude have positive effects on learning satisfaction; and learning motivation, learning attitude, and learning satisfaction all have positive effects on learning outcomes. Therefore, hypotheses H3, H4, H5, H6, H7, and H8 are supported.
Learning motivation has a positive impact on medical students’ learning attitudes. This suggests that students with higher levels of learning motivation tend to exhibit more positive learning attitudes. This finding aligns with the results of Chou et al. [112] in the context of flipped classrooms in language learning, which demonstrated that learning motivation significantly influences the cognitive, affective, and behavioral components of learning attitudes. Similarly, Ait Baha et al. [113]found that chatbot-based learning enhances students’ intrinsic motivation, fosters positive learning attitudes, and facilitates subject-specific knowledge acquisition through interactive and personalized learning experiences. Therefore, when medical students use large language models to access personalized learning plans and receive real-time feedback, their motivation is effectively stimulated, encouraging a more proactive learning attitude toward academic tasks. This attitude, driven by intrinsic motivation, helps them maintain sustained attention and engagement throughout the learning process, laying a solid foundation for subsequent learning satisfaction and improved educational outcomes [114].
Learning motivation and learning attitude positively influence medical students’ learning satisfaction. According to the application value of the ARCS model in instructional design, perceived personalization and interactivity during the learning process can effectively stimulate motivation and enhance students’ learning satisfaction, which is consistent with related findings [1]. In addition, medical students who develop positive learning attitudes tend to experience higher satisfaction with their learning. This is in line with the findings of Santo et al. [115], who reported that both positive and negative emotions are associated with satisfaction in online learning environments. Learning motivation is typically measured through students’ perceptions and motivational tendencies, while learning attitudes reflect their emotional states during participation in the learning process [116]. When medical students engage in AI-assisted learning supported by large language models, their intrinsic motivation not only directly increases their recognition of and satisfaction with the learning process, but their positive attitudes also enhance emotional engagement, leading to greater satisfaction with the course content, learning environment, and instructional methods. Therefore, in AI-supported teaching, educators should focus on motivation as a key factor, leveraging AI’s personalization features and feedback mechanisms to stimulate motivation, transform attitudes, and enhance students’ confidence in the course, ultimately improving their overall learning satisfaction.
Learning motivation, learning attitude, and learning satisfaction in the context of intelligent education all have a positive impact on learning outcomes. Among these, learning satisfaction is the most significant factor influencing learning outcomes. This result indicates that medical students’ satisfaction with course content, teaching methods, and the overall learning experience largely determines their final learning achievements. This finding supports existing research, such as Akhteh et al. [117], who emphasized that positive learning experiences and high levels of satisfaction enhance learners’ autonomy and engagement, ultimately promoting the attainment of learning achievements. Therefore, when medical students feel satisfied with the learning process, they are more likely to develop a sense of recognition and accomplishment, which strengthens their willingness to stay engaged and deepen their understanding, thereby improving learning outcomes. In AI-assisted instructional environments, timely feedback, personalized support, and flexible learning formats contribute to enhanced learning experiences, enabling students to perform better in terms of knowledge acquisition and skill application [118].
In addition, learning motivation and learning attitudes in the context of intelligent education exert a positive impact on learning outcomes. This finding is consistent with the perspective proposed by Zhou &Ahmad [119] from the lens of self-determination theory, which suggests that the stronger the learning motivation, the more likely learners are to achieve higher academic performance. In a study on students’ acceptance of generative AI, Avcı [120] highlighted that fostering a positive attitude to cultivate creative thinking can significantly influence learning outcomes and enhance individual learning capacity. Therefore, under the AI-assisted instructional model, attention should be paid not only to the optimization of teaching technologies but also to the implementation of effective teaching strategies that stimulate intrinsic motivation and foster positive learning attitudes. Such an approach contributes to a student-centered and sustainable learning cycle.
External environment level
In the context of intelligent education, the external environment had a positive impact on both learning motivation and learning outcomes, confirming hypotheses H9 and H10. Meanwhile, learning motivation served as a mediating factor between the external environment and learning outcomes, supporting hypothesis H12.
The external environment exerts a positive influence on both learning motivation and academic outcomes. In AI-assisted instructional contexts, the learning environment for medical students has undergone significant improvements, particularly through the expansion of available learning resources. By utilizing intelligent learning platforms and online tools, students are better equipped to develop their reasoning and comprehension skills, which in turn facilitates deeper engagement with the learning process [121]. This observation is supported by the findings of Pertiwi et al. [122], who reported a positive association between AI-based learning strategies and increased student engagement. AI technologies can stimulate intellectual curiosity and foster greater learner autonomy, thereby activating intrinsic motivation and enhancing both participation and performance. Nevertheless, despite the overall benefits of the external environment, certain limitations remain. Prior studies have highlighted shortcomings in the technological efficiency, semantic clarity, and interactivity of some AI tools, which may hinder students’ learning experiences and reduce motivation [123]. Effective AI integration in educational settings requires reliable digital infrastructure, including high-quality platforms, stable internet connectivity, and strong data privacy safeguards. However, many institutions still face challenges due to insufficient investment and technical support, which constrain the effective implementation and scalability of AI-enhanced teaching practices [124, 125]. To address these gaps, greater financial and technological investment is essential to improve the digital learning environment, enhance user experience, and ensure that educational systems can fully leverage the benefits of AI in teaching and learning [126].
Learning motivation serves as a mediating factor between the external environment and learning outcomes. External elements such as platform stability, resource accessibility, and the user-friendliness of interactive interfaces enhance the overall learning experience, thereby fostering stronger motivation and improving academic performance. This finding aligns with the conclusions of Schrader and Bastiaens [127], who emphasized that perceived environmental support can stimulate learning motivation, which in turn contributes to improved learning achievement—highlighting the mediating role of motivation between environmental support and educational outcomes. Therefore, in AI-assisted instruction, particular attention should be given to the stability of large language model platforms, the usability of their interfaces, and the ease of accessing high-quality resources. Optimizing these critical external factors can help create a more supportive learning environment that effectively enhances medical students’ motivation and learning outcomes.
The findings of this study further confirm the applicability of constructivism and the ARCS motivational model in AI-assisted instructional settings. Constructivism emphasizes student-centered learning, where knowledge is actively constructed through exploration. This study found that, under the intelligent instructional context, teaching quality and the external environment significantly enhanced students’ learning motivation and learning outcomes. This reflects the way AI-assisted teaching creates a more interactive and personalized learning environment, enabling students to actively construct knowledge through authentic, task-based activities. This finding also demonstrates the practical value of the learner-centered constructivist approach in higher medical education.
Moreover, the results also support the theoretical assumptions of the ARCS motivational model. As key factors influencing students’ learning motivation, teaching quality and the external environment can be effectively enhanced by educators through engaging instructional content and interactive learning tools. These strategies help capture students’ attention, provide content relevant to professional medical knowledge to increase perceived relevance, and foster confidence through high-quality teaching and supportive learning environments. These factors ultimately improve students’ motivation and positively influence their learning attitudes and satisfaction. The mediating role of learning motivation between teaching quality and learning outcomes further highlights the important role of motivation in the ARCS model, revealing how instructional design and environmental support can jointly activate learners’ intrinsic drive.
In addition, this study integrates constructivism and the ARCS model to propose a “teacher–student–external environment” framework, which underscores the synergistic path among instructional facilitation, environmental support, and learner construction. This extended framework enhances the practical applicability of existing models and offers a novel theoretical perspective for understanding how AI-assisted instruction can stimulate motivation and optimize learning outcomes in medical education.
In 2018, the Ministry of Education of China issued the National Standards for the teaching quality of undergraduates in ordinary colleges and universities, which include educational quality standards for various medical-related disciplines. Medical schools across the country implement their teaching and training under the framework of these standardized guidelines. Therefore, the findings of this study can still offer valuable insights for relevant practices within the context of medical education. Additionally, Huang et al. [128] conducted a single-center study at a university in Taiwan, investigating the application of an AI-based personalized recommendation system in a flipped classroom setting. Their findings demonstrated that such a system effectively enhanced students’ learning motivation, which in turn increased their engagement and improved learning outcomes. These results align with the findings of the present study and further support the potential of AI-assisted instruction in enhancing students’ academic performance. Therefore, this study provides a useful reference for the application of artificial intelligence in higher education.
Conclusion
This study, based on constructivist learning theory and the ARCS motivational model, proposed an analytical framework to examine the factors influencing medical students’ learning outcomes in an AI-assisted teaching context. Learning motivation was incorporated as a mediating variable to explore the pathways and mechanisms of influence. The framework also integrated the “student–external environment” interaction into the teaching process, underscoring the pivotal roles of teachers, students, and the learning environment, and highlighting the dynamic synergy and feedback among these elements. This integrated approach provides theoretical support for optimizing the design and implementation of AI-assisted teaching in medical education. Furthermore, through mediation analysis, the study further revealed the underlying mechanisms by which AI-assisted teaching impacts learning outcomes, offering a deeper understanding of how learning motivation contributes to academic achievement. These findings have practical implications for designing more effective instructional strategies to enhance students’ learning engagement and academic performance. Ultimately, the study offers a new perspective on the determinants of learning effectiveness in AI-supported education and holds significance for improving the quality of medical training, advancing educational equity, and promoting the digital transformation of medical education.
Limitations and future research directions
This study has several limitations. First, the data were primarily collected through self-reports from the participants, which may be subject to social desirability and subjective biases. For instance, participants might have overestimated their motivation, engagement, or learning outcomes to present themselves in a more favorable light or to align with perceived expectations, resulting in deviations from actual performance. Moreover, reliance on self-reported measures limits the precision of causal inference among variables and may obscure interaction effects or the influence of uncontrolled confounding factors, thereby affecting the internal consistency and external validity of the findings. Future studies could incorporate longitudinal or quasi-experimental designs and include objective measures such as course grades, clinical skills assessments, online learning duration, and task completion rates to improve the credibility of the results and strengthen causal inferences. Second, all participants were recruited from the same university, and the study did not deeply explore the impact of cultural and social backgrounds on the acceptance of AI teaching, which limits the generalizability of the findings. Medical students’ acceptance of AI-based teaching may be influenced by factors such as the educational system, cultural values, and usage habits. Future research could adopt cross-cultural or multi-center designs, incorporating samples from different regions and educational backgrounds to enhance the representativeness and practical implications of the study. In addition, the study did not include potential moderating variables or alternative theoretical explanations, which may have led to the omission of important factors influencing learning outcomes. For instance, students’ digital literacy, learning preferences, or prior exposure to artificial intelligence might impact their learning performance. And the novelty of AI-based teaching could temporarily enhance student motivation and engagement. Future research should consider these variables to deepen the understanding of the mechanisms of AI teaching and enhance the explanatory power of the study.
Appendix
The adapted questionnaire was used to assess the impact of AI-assisted teaching on medical students’ learning outcomes.
| Observed variables | Indicator code | Observed indicator content | Reference |
|---|---|---|---|
| Teaching quality (TQ) | TQ1 | The teaching content is effectively connected | Kassab et al. [84] |
| TQ2 | There are clear teaching objectives and tasks | ||
| TQ3 | A comprehensive teaching evaluation can be conducted | ||
| TQ4 | The course schedule is appropriate and reasonable | ||
| Learning motivation (LM) | LM1 | My interest in course learning has increased | Law et al. [85] |
| LM2 | I want to further improve my abilities | ||
| LM3 | I want to learn more professional knowledge | ||
| LM4 | I want to increase communication with teachers and classmates during learning | ||
| Learning attitude (LA) | LA1 | I believe that AI-assisted teaching helps me stay more focused in class | Afacan and Muhametjanova [86] |
| LA2 | I enjoy courses that use AI-assisted teaching | ||
| LA3 | I think this is a great way of learning | ||
| External environment (EE) | EE1 | I am familiar with and proficient in using learning platforms and tools | Camilleri & Camilleri [87]; Wahyuni et al. [88] |
| EE2 | I can effectively utilize the learning resources provided by AI-assisted teaching | ||
| EE3 | I can adapt to the learning environment of AI-assisted teaching | ||
| Learning satisfaction (LS) | LS1 | I am overall satisfied with AI-assisted teaching | Lin and Wang [89] |
| LS2 | I am satisfied with the way knowledge is presented in AI-assisted teaching | ||
| LS3 | I am satisfied with the learning outcomes of the AI-assisted teaching course | ||
| Learning outcomes(LO) | LO1 | AI-assisted teaching has enriched my learning style | Wang et al. [90] |
| LO2 | I am able to fully understand the content I have learned | ||
| LO3 | I am very familiar with the course content | ||
| LO4 | I am confident in handling exams |
Acknowledgements
The first author conducted the protocol design, completed the survey, and wrote the paper. the corresponding author was responsible for the legal, academic, and ethical aspects of the paper. Other authors were involved in data processing, sample collection, etc. All authors reviewed and approved the final version of the manuscript.
Abbreviations
- AI
Artificial intelligence
- TQ
Teaching quality
- LM
Learning motivation
- LA
Learning attitude
- LS
Learning satisfaction
- EE
External environment
- LO
Learning outcomes
Author contributions
All authors contributed to the conception and design of the study. JYZ and YYZ were responsible for the questionnaire survey and data collection. XPZ, HZ, and FDW handled data organization and analysis. The initial draft of the manuscript was written by XYP, YYL, and XYC. All authors provided feedback on earlier versions of the manuscript, and all authors have read and approved the final manuscript.
Funding
This research was sponsored by the following funds: 2022 Liaoning Adult Education Society Continuing Education Teaching Reform Research Program, Study on the transformation and development of non-academic continuing education in medical university. [General Program, Program Number: LCYJGZXYB22103]. 2021 Research on Undergraduate Teaching Reform in General Higher Education in Liaoning Province, Research on the teaching path of interaction design in SPOC mode under OBE concept. [General Program, Program Number 542]. 2022 Liaoning Province Economic and Social Development Research Topics, Research on the path of improving the competitiveness of medical universities’ discipline culture under the perspective of the three comprehensive education. [LiaoNing Provincial Federation Social Science Circles, Program Number: 2022lslwzzkt-011].
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Dalian Medical University (reference number 2024–027).The procedures used in this study adhere to the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their legal guardians in this study.
Competing interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xinyu Pang, Jinyan Zou and Xiaopeng Zhang contributed equally to this work.
Contributor Information
Yuanyuan Zhang, Email: zhangyuan@dmu.edu.cn.
Xiyi Chen, Email: xychen@dmu.edu.cn.
References
- 1.Chiu TKF, Moorhouse BL, Chai CS, Ismailov M. Teacher support and student motivation to learn with Artificial Intelligence (AI) based chatbot. Interact Learn Environ. 2024;32(7):3240–56. 10.1080/10494820.2023.2172044. [Google Scholar]
- 2.Mir MM, Mir GM, Raina NT, Mir SM, Mir SM, Miskeen E, et al. Application of artificial intelligence in medical education: current scenario and future perspectives. J Adv Med Educ Prof. 2023;11(3):133–40. 10.30476/jamp.2023.98655.1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumari A, Rani S, Bara MP. A study on the perception of medical students using online teaching during covid-19 pandemic. J Family Med Primary Care. 2022;11(6):2552–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abd-alrazaq A, AlSaad R, Alhuwail D, Ahmed A, Healy PM, Latifi S, et al. Large language models in medical education: opportunities, challenges, and future directions. JMIR Med Educ. 2023;9: e48291. 10.2196/48291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karabacak M, Ozkara BB, Margetis K, Wintermark M, Bisdas S. The advent of generative language models in medical education. JMIR Med Educ. 2023;9: e48163. 10.2196/48163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang W, Cai M, Lee HJ, Evans R, Zhu C, Ming C. AI in Medical Education: Global situation, effects and challenges. Edu Inform Technol. 2024;29(4):4611–33. 10.1007/s10639-023-12009-8. [Google Scholar]
- 7.Jiang Y, Fu X, Wang J, Liu Q, Wang X, Liu P, et al. Enhancing medical education with chatbots: a randomized controlled trial on standardized patients for colorectal cancer. BMC Medical Edu. 2024;24(1):1511. 10.1186/s12909-024-06530-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tokuç B, Varol G. Medical education in the era of advancing technology. Balkan Med J. 2023;40(6):395–9. 10.4274/balkanmedj.galenos.2023.2023-7-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sridharan K, Sequeira RP. Artificial intelligence and medical education: application in classroom instruction and student assessment using a pharmacology & therapeutics case study. BMC Medical Edu. 2024;24(1):431. 10.1186/s12909-024-05365-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bardach L, Klassen RM. Smart teachers, successful students? A systematic review of the literature on teachers’ cognitive abilities and teacher effectiveness. Edu Res Rev. 2020;30:100312. 10.1016/j.edurev.2020.100312. [Google Scholar]
- 11.Hanaysha JR, Shriedeh FB, In’airat M. Impact of classroom environment, teacher competency, information and communication technology resources, and university facilities on student engagement and academic performance. Int J Inform Manag Data Insights. 2023;3(2):100188. 10.1016/j.jjimei.2023.100188. [Google Scholar]
- 12.Altinay Z, Altinay F, Sharma RC, Dagli G, Shadiev R, Yikici B, et al. Capacity building for student teachers in learning, teaching artificial intelligence for quality of education. Societies. 2024;14(8): 148. [Google Scholar]
- 13.Karamzadeh A, Mosalanejad L, Bazrafkan L. Effectiveness of ethics case based on blended learning approaches on medical students’ learning: a quasi-experimental study. J Educ Health Promot. 2021. 10.4103/jehp.jehp_59_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Darmawan H. The relationship between students’ interest in learning and mathematics learning outcomes. Afore J Pendidikan Matematika. 2023;2(2):1–11. 10.57094/afore.v2i2.1054. [Google Scholar]
- 15.Yusup M, Marzani M, Lubis T, Anggraeni GS. The influence of learning attitudes and motivation on students’ learning achievement. JMKSP. 2023;8(01/02):1–14. 10.31851/jmksp.v8i1.9844. [Google Scholar]
- 16.Dahri NA, Yahaya N, Al-Rahmi WM, Vighio MS, Alblehai F, Soomro RB, et al. Investigating AI-based academic support acceptance and its impact on students’ performance in Malaysian and Pakistani higher education institutions. Edu Inform Technol. 2024;29(14):18695–744. 10.1007/s10639-024-12599-x. [Google Scholar]
- 17.Yaseen H, Mohammad AS, Ashal N, Abusaimeh H, Ali A, Sharabati A-AA. The impact of adaptive learning technologies, personalized feedback, and interactive AI tools on student engagement: the moderating role of digital literacy. Sustainability. 2025. 10.3390/su17031133. [Google Scholar]
- 18.Joseph GV, Athira P, Thomas MA, Jose D, Roy TV, Prasad M. Impact of digital literacy, use of AI tools and peer collaboration on AI assisted learning: perceptions of the university students. Digit Educ Rev. 2024;45:43–9. [Google Scholar]
- 19.Capone R. Blended learning and student-centered active learning environment: a case study with STEM undergraduate students. Can J Sci Math Technol Educ. 2022;22(1):210–36. [Google Scholar]
- 20.Kapo A, Milutinovic LD, Rakovic L, Maric S. Enhancing e-learning effectiveness: analyzing extrinsic and intrinsic factors influencing students’ use, learning, and performance in higher education. Edu Inform Technol. 2024;29(8):10249–76. 10.1007/s10639-023-12224-3. [Google Scholar]
- 21.Saqr RR, Al-Somali SA, Sarhan MY. Exploring the acceptance and user satisfaction of AI-driven e-learning platforms (blackboard, moodle, edmodo, coursera and edX): An integrated technology model. sustainability [Internet]. 2024; 16(1).
- 22.Priamono GH, Hakim AR, Daryono RW. The influence of artificial intelligence (AI) and mobile learning on learning outcomes in higher education: did the mediation of self-competence matter? J Penelitian dan Pengkajian Ilmu Pendidikan: e-Saintika. 2024;8(2):241–59. 10.36312/esaintika.v8i2.1902. [Google Scholar]
- 23.Boubker O. From chatting to self-educating: Can AI tools boost student learning outcomes? Expert Syst Appl. 2024;238:121820. 10.1016/j.eswa.2023.121820. [Google Scholar]
- 24.Chiu TKF. A classification tool to foster self-regulated learning with generative artificial intelligence by applying self-determination theory: a case of ChatGPT. Educ Technol Res Dev. 2024;72(4):2401–16. 10.1007/s11423-024-10366-w. [Google Scholar]
- 25.Sasikala P, Ravichandran R. Study on the impact of artificial intelligence on student learning outcomes. J Digital Learn Edu. 2024;4(2):145–55. 10.52562/jdle.v4i2.1234. [Google Scholar]
- 26.Deci EL, Ryan RM. The general causality orientations scale: Self-determination in personality. J Res Personality. 1985;19(2):109–34. 10.1016/0092-6566(85)90023-6. [Google Scholar]
- 27.Deci EL, Ryan RM. The “What” and “Why” of goal pursuits: human needs and the self-determination of behavior. Psychol Inquiry. 2000;11(4):227–68. 10.1207/S15327965PLI1104_01. [Google Scholar]
- 28.Ryan RM, Deci EL. Self-determination theory: Basic psychological needs in motivation, development, and wellness: Guilford publications; 2017. ISBN: 1462528767.
- 29.Chiu TKF, Luke MB, Sing CC, Ismailov M. Teacher support and student motivation to learn with Artificial Intelligence (AI) based chatbot. Interact Learn Environ. 2024;32(7):3240–56. 10.1080/10494820.2023.2172044. [Google Scholar]
- 30.Tsai C-Y, Shih W-L, Hsieh F-P, Chen Y-A, Lin C-L, Wu H-J. Using the ARCS model to improve undergraduates’ perceived information security protection motivation and behavior. Comput Educ. 2022;181: 104449. 10.1016/j.compedu.2022.104449. [Google Scholar]
- 31.Sweller J. Cognitive load during problem solving: effects on learning. Cogn Sci. 1988;12(2):257–85. [Google Scholar]
- 32.Schnotz W, Kürschner C. A reconsideration of cognitive load theory. Edu Psychol Rev. 2007;19(4):469–508. 10.1007/s10648-007-9053-4. [Google Scholar]
- 33.Edwards BI, Olugbade D, Ojo OA. Facilitating cognitive load management and improved learning outcomes and attitudes in middle school technology and vocational education through AI chatbot. J Tech Educ Train. 2024;16(3):114–31. [Google Scholar]
- 34.Moreno R. When worked examples don’t work: is cognitive load theory at an impasse? Learn Instr. 2006;16(2):170–81. [Google Scholar]
- 35.Eitel A, Endres T, Renkl A. Self-management as a bridge between cognitive load and self-regulated learning: the illustrative case of seductive details. Edu Psychol Rev. 2020;32(4):1073–87. 10.1007/s10648-020-09559-5. [Google Scholar]
- 36.Renninger EP. Exploring the Impact of Constructivist Learning on Students’ Prob-lem-Solving Abilities in Education. J Ilmu Pendidikan dan Humaniora. 2024;13(2):81–91. [Google Scholar]
- 37.Do H-N, Do BN, Nguyen MH. 3How do constructivism learning environments generate better motivation and learning strategies? Design Sci Approach Heliyon. 2023. 10.1016/j.heliyon.2023.e22862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adigun OT, Mpofu N, Maphalala MC. Fostering self-directed learning in blended learning environments: A constructivist perspective in higher education. High Educ Q. 2025;79(1):e12572. 10.1111/hequ.12572. [Google Scholar]
- 39.Keller JM. Development and use of the ARCS model of instructional design. J Instr Dev. 1987;10(3):2–10. 10.1007/BF02905780. [Google Scholar]
- 40.Goksu I, Islam BY. Does the ARCS motivational model affect students’ achievement and motivation? A meta-analysis Rev Edu. 2021;9(1):27–52. 10.1002/rev3.3231. [Google Scholar]
- 41.Fang X, Ng DTK, Leung JKL, Xu H. The applications of the ARCS model in instructional design, theoretical framework, and measurement tool: a systematic review of empirical studies. Interact Learn Environ. 2023. 10.1080/10494820.2023.2240867. [Google Scholar]
- 42.Halid LI. Constructivist approach to language learning: Linking piaget’s theory to modern educational practice. INTERACTION J Pendidikan Bahasa. 2024;11(2):306–27. [Google Scholar]
- 43.Strachan R, Liyanage L. Active Student Engagement: The Heart of Effective Learning. In: Layne PC, Lake P, editors. Global Innovation of Teaching and Learning in Higher Education: Transgressing Boundaries. Cham: Springer International Publishing; 2015. p. 255–74. [Google Scholar]
- 44.Huang Z, Mao Y, Zhang J. The influence of artificial intelligence technology on college students’ learning effectiveness from the perspective of constructivism — taking ChatGPT as an example. J Edu Human Soc Sci. 2024;30:40–6. 10.54097/y1x3jj43. [Google Scholar]
- 45.Ma L, Lee CS. Evaluating the effectiveness of blended learning using the ARCS model. J Comput Assist Learn. 2021;37(5):1397–408. [Google Scholar]
- 46.Kong SC, Yang Y. A human-centered learning and teaching framework using generative artificial intelligence for self-regulated learning development through domain knowledge learning in K–12 settings. IEEE Trans Learn Technol. 2024;17:1588–99. 10.1109/TLT.2024.3392830. [Google Scholar]
- 47.Chun Y-E, Han JY, Burm E. Mediating effect of learning flow in the relationship between learning motivation and academic achievement of nursing students. African J Biol Sci. 2024. 10.33472/AFJBS.6.9.2024.3830-3840. [Google Scholar]
- 48.Jin S. Optimizing english teaching: ARCS motivation model and task-based language teaching in university. Learn Motivation. 2024;87:102028. 10.1016/j.lmot.2024.102028. [Google Scholar]
- 49.Mohammed S, Kınyo L. Constructivist theory as a foundation for the utilization of digital technology in the lifelong learning process. Turk Online J Distance Educ. 2020;21(4):90–109. [Google Scholar]
- 50.Yang Y, Ouyang T, Zhang L, Wang J. Study on blended teaching mode and its application based on the ARCS motivational model: taking bioinformatics course as an example. Medicine (Baltimore). 2022. 10.1097/MD.0000000000030801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen M-RA. Improving English semantic learning outcomes through AI chatbot-based ARCS approach. Interact Learn Environ. 2025. 10.1080/10494820.2025.2454443. [Google Scholar]
- 52.Mattar J. Constructivism and connectivism in education technology: Active, situated, authentic, experiential, and anchored learning. RIED Rev Iberoam Educ Distancia. 2018. 10.5944/ried.21.2.20055. [Google Scholar]
- 53.Wu D, Zhang S, Ma Z, Yue X-G, Dong RK. Unlocking potential: key factors shaping undergraduate self-directed learning in AI-enhanced educational environments. Systems. 2024. 10.3390/systems12090332. [Google Scholar]
- 54.Ramaul L, Ritala P, Ruokonen M. Creational and conversational AI affordances: How the new breed of chatbots is revolutionizing knowledge industries. Bus Horiz. 2024;67(5):615–27. 10.1016/j.bushor.2024.05.006. [Google Scholar]
- 55.Eysenbach G. The role of ChatGPT, generative language models, and artificial intelligence in medical education: a conversation with ChatGPT and a call for papers. JMIR Med Educ. 2023;9:e46885. 10.2196/46885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.S. T T, I. A SB, editors. Artificial Intelligence Effects on Student Learning Outcomes in Higher Education. 2024 Ninth International Conference on Science Technology Engineering and Mathematics (ICONSTEM); 2024 4–5 April 2024.
- 57.Xie X. Influence of AI-driven inquiry teaching on learning outcomes. Int J Emerg Technol Learn (iJET). 2023;18(23):59–70. [Google Scholar]
- 58.Wu R, Yu Z. Do AI chatbots improve students learning outcomes? Evidence from a meta-analysis. British J Edu Technol. 2024;55(1):10–33. 10.1111/bjet.13334. [Google Scholar]
- 59.Boelens R, Voet M, De Wever B. The design of blended learning in response to student diversity in higher education: instructors’ views and use of differentiated instruction in blended learning. Comput Educ. 2018;120:197–212. [Google Scholar]
- 60.Zheng B, Ward A, Stanulis R. Self-regulated learning in a competency-based and flipped learning environment: learning strategies across achievement levels and years. Med Educ Online. 2020;25(1):1686949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Krammer G, Pflanzl B, Lenske G, Mayr J. Assessing quality of teaching from different perspectives: measurement invariance across teachers and classes. Educ Assess. 2021;26(2):88–103. [Google Scholar]
- 62.Yuan Y. A Study of Artificial Intelligence-Driven Change in Higher Education in the Age of Digital Intelligence. Contemporary Edu Teach Res. 2024;5(3):127–32. 10.61360/BoniCETR242016080306. [Google Scholar]
- 63.Lee H. The rise of ChatGPT: Exploring its potential in medical education. Anatomical Sci Edu. 2024;17(5):926–31. 10.1002/ase.2270. [DOI] [PubMed] [Google Scholar]
- 64.Ford ME. Motivating humans: Goals, emotions, and personal agency beliefs: Sage; 1992. ISBN: 0803945299.
- 65.Wang Y-M, Wei C-L, Lin H-H, Wang S-C, Wang Y-S. What drives students’ AI learning behavior: a perspective of AI anxiety. Interact Learn Environ. 2024;32(6):2584–600. 10.1080/10494820.2022.2153147. [Google Scholar]
- 66.Pelaccia T, Viau R. Motivation in medical education. Med Teach. 2017;39(2):136–40. [DOI] [PubMed] [Google Scholar]
- 67.Ruiz-Alfonso Z, León J, Vega-Santana L, González C. Teaching quality: relationships between students’ motivation, effort regulation, future interest, and connection frequency. Psicología Educativa Revista de los Psicólogos de la Educación. 2021;27(1):67–76. [Google Scholar]
- 68.Shikokoti H, Mutegi R. Influence of artificial intelligence on the quality of education in higher learning: A case study of faculty of education, university of Nairobi. Kenya Journal of Education and Practice. 2024;15:97–114. 10.7176/JEP/15-11-11. [Google Scholar]
- 69.Zawodowego ECRS. The shift to learning outcomes: Conceptual, political and practical developments in Europe: Office for Official Publications of the European Communities; 2008. ISBN: 9289605405.
- 70.Hao M, Wang Y, Peng J. Empirical research on AI technology-supported precision teaching in high school science subjects. Appl Sci. 2024. 10.3390/app14177544. [Google Scholar]
- 71.Koballa TR Jr, Crawley FE. The influence of attitude on science teaching and learning. Sch Sci Math. 1985;85(3):222–32. [Google Scholar]
- 72.Jiang L, Zhou N, Yang Y. Student motivation and engagement in online language learning using virtual classrooms: Interrelationships with support, attitude and learner readiness. Edu Inform Technol. 2024;29(13):17119–43. 10.1007/s10639-024-12514-4. [Google Scholar]
- 73.Wei R, Li K, Lan J, editors. Improving Collaborative Learning Performance Based on LLM Virtual Assistant. 2024 13th International Conference on Educational and Information Technology (ICEIT); 2024 22–24 March 2024.
- 74.Wu J-H, Tennyson RD, Hsia T-L. A study of student satisfaction in a blended e-learning system environment. Comput Educ. 2010;55(1):155–64. [Google Scholar]
- 75.Younas M, Noor U, Zhou X, Menhas R, Qingyu X. COVID-19, students satisfaction about e-learning and academic achievement: mediating analysis of online influencing factors. Front Psychol. 2022;13: 948061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yoo MS, Park HR. Effects of case-based learning on communication skills, problem-solving ability, and learning motivation in nursing students. Nurs Health Sci. 2015;17(2):166–72. [DOI] [PubMed] [Google Scholar]
- 77.Chen R-Y, Tu J-F. The computer course correlation between learning satisfaction and learning effectiveness of vocational college in Taiwan. Symmetry. 2019;11(6):822. [Google Scholar]
- 78.Lee C-H, Yeh D, Kung RJ, Hsu C-S. The influences of learning portfolios and attitudes on learning effects in blended e-learning for mathematics. J Educ Comput Res. 2007;37(4):331–50. [Google Scholar]
- 79.Cook DA, Artino AR Jr. Motivation to learn: an overview of contemporary theories. Med Educ. 2016;50(10):997–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yong SM, Thi LS. Online learning motivation during Covid-19 pandemic: The role of learning environment, student self-efficacy and learner-instructor interaction. Malays J Learn Instr. 2022;19(2):213–49. [Google Scholar]
- 81.Zhu Y, Xu Y, Wang X, Yan S, Zhao L. The selectivity and suitability of online learning resources as predictor of the effects of self-efficacy on teacher satisfaction during the COVID-19 lockdown. Front Psychol. 2022;13: 765832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pan X. Technology acceptance, technological self-efficacy, and attitude toward technology-based self-directed learning: learning motivation as a mediator. Front Psychol. 2020;11: 564294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hair Jr JFH, Sarstedt M, Hopkins L, Kuppelwieser VG. Partial least squares structural equation modeling (PLS-SEM): an emerging tool in business research. Eur Bus Rev. 2014;26(2):106–21. 10.1108/EBR-10-2013-0128. [Google Scholar]
- 84.Kassab SE, Al-Shafei AI, Halim SA, Otoom S. Relationships between the quality of blended learning experience self-regulated learning and academic achievement of medical students: a path analysis. Adv Med Edu Practice. 2015;6(null):27–34. 10.2147/AMEP.S75830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Law KMY, Geng S, Li T. Student enrollment, motivation and learning performance in a blended learning environment: The mediating effects of social, teaching, and cognitive presence. Comput Edu. 2019;136:1–12. 10.1016/j.compedu.2019.02.021. [Google Scholar]
- 86.Afacan Adanır G, Muhametjanova G. University students’ acceptance of mobile learning: A comparative study in Turkey and Kyrgyzstan. Edu Inform Technol. 2021;26(5):6163–81. 10.1007/s10639-021-10620-1. [Google Scholar]
- 87.Camilleri MA, Camilleri AC. Learning from anywhere, anytime: Utilitarian motivations and facilitating conditions for mobile learning. Technol Know Learn. 2023;28(4):1687–705. 10.1007/s10758-022-09608-8. [Google Scholar]
- 88.Wahyuni DS, Ariadi G, Sugihartini N, Mertayasa INE, editors. The Impact of Achievement Motivation on Educational Compatibility mediated by Perceived Ease of Use. Proceedings of the 5th International Conference on Vocational Education and Technology, IConVET; 2022.
- 89.Lin W-S, Wang C-H. Antecedences to continued intentions of adopting e-learning system in blended learning instruction: A contingency framework based on models of information system success and task-technology fit. Comput Edu. 2012;58(1):88–99. 10.1016/j.compedu.2011.07.008. [Google Scholar]
- 90.Wang C-Y, Zhang Y-Y, Chen S-C. The empirical study of college students’ e-learning effectiveness and its antecedents toward the COVID-19 epidemic environment. Front Psychol. 2021. 10.3389/fpsyg.2021.573590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kline RB. 26 convergence of structural equation modeling and multilevel modeling. The SAGE handbook of innovation in social research methods: SAGE Publications Ltd; 2011. p. 562–89.
- 92.Kock N. Common method bias in PLS-SEM: a full collinearity assessment approach. Int J e-Collaboration (ijec). 2015;11(4):1–10. [Google Scholar]
- 93.Gaskin J. Common Method Bias (CMB) in PLS (partial least squares) [Online] Available at: youtube. com/user. Gaskination [Accessed 17 June 2025]. 2017.
- 94.Chen L, Rashidin MS, Song F, Wang Y, Javed S, Wang J. Determinants of consumer’s purchase intention on fresh e-commerce platform: perspective of UTAUT model. SAGE Open. 2021;11(2): 21582440211027875. 10.1177/21582440211027875. [Google Scholar]
- 95.Thackeray R, Crookston BT, West JH. Correlates of health-related social media use among adults. J Med Internet Res. 2013;15(1):e21. 10.2196/jmir.2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sarstedt M, Ringle CM, Hair JF. Partial least squares structural equation modeling. Handbook of market research: Springer; 2021. p. 587–632.
- 97.Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39–50. [Google Scholar]
- 98.Gefen D, Straub D, Boudreau M-C. Structural equation modeling and regression: guidelines for research practice. Commun Assoc Inf Syst. 2000;4(1):7. [Google Scholar]
- 99.Chen S-C, Lin C-P. Understanding the effect of social media marketing activities: The mediation of social identification, perceived value, and satisfaction. Technol Forecast Soc Change. 2019;140:22–32. [Google Scholar]
- 100.Daniel K, Msambwa MM, Antony F, Wan X. Motivate students for better academic achievement: a systematic review of blended innovative teaching and its impact on learning. Comput Appl Eng Educ. 2024;32(4): e22733. [Google Scholar]
- 101.Sajja R, Sermet Y, Cwiertny D, Demir I. Platform-independent and curriculum-oriented intelligent assistant for higher education. Int J Edu Technol Higher Edu. 2023;20(1):42. 10.1186/s41239-023-00412-7. [Google Scholar]
- 102.Zhang J, Zhang Z. AI in teacher education: Unlocking new dimensions in teaching support, inclusive learning, and digital literacy. J Comput Assisted Learn. 2024;40(4):1871–85. 10.1111/jcal.12988. [Google Scholar]
- 103.Latif A, Darmawan D. Examining How School Environment and Teacher Competence Affect Student Learning Motivation at MA Al Fatich Tambak Osowilangun Surabaya. Teach Learn J Mandalika (Teacher). 2024;5(1):69–75. [Google Scholar]
- 104.Zhang C. Artificial Intelligence and the Changing Role of Teachers: the Path from Knowledge Transmitter to Learning Designer. 2024.
- 105.Pupic N, Ghaffari-zadeh A, Hu R, Singla R, Darras K, Karwowska A, et al. An evidence-based approach to artificial intelligence education for medical students: a systematic review. PLoS Digit Health. 2023;2(11): e0000255. 10.1371/journal.pdig.0000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zarei M, Eftekhari Mamaghani H, Abbasi A, Hosseini M-S. Application of artificial intelligence in medical education: A review of benefits, challenges, and solutions. Medicina Clínica Práctica. 2024;7(2):100422. 10.1016/j.mcpsp.2023.100422. [Google Scholar]
- 107.Rincón EHH, Jimenez D, Aguilar LAC, Flórez JMP, Tapia ÁER, Peñuela CLJ. Mapping the use of artificial intelligence in medical education: a scoping review. BMC Med Educ. 2025;25(1):526. 10.1186/s12909-025-07089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Grunhut J, Marques O, Wyatt ATM. Needs, challenges, and applications of artificial intelligence in medical education curriculum. JMIR Med Educ. 2022;8(2): e35587. 10.2196/35587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Boadu SK, Dookurong I, Arthur YD. The effect of teacher quality on perceived students’ mathematics achievement: the mediating role of technology, motivation and student interest. Motivation and Student Interest. 2024.
- 110.Safranek CW, Sidamon-Eristoff AE, Gilson A, Chartash D. The role of large language models in medical education: applications and implications. JMIR Med Educ. 2023;9:e50945. 10.2196/50945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.James CA, Wheelock KM, Woolliscroft JO. Machine learning: the next paradigm shift in medical education. Acad Med. 2021. 10.1097/ACM.0000000000003943. [DOI] [PubMed] [Google Scholar]
- 112.Chou C-P, Chen K-W, Hung C-J. A Study on Flipped Learning Concerning Learning Motivation and Learning Attitude in Language Learning. Frontiers in Psychology. 2021;Volume 12 - 2021. [DOI] [PMC free article] [PubMed]
- 113.Ait Baha T, El Hajji M, Es-Saady Y, Fadili H. The impact of educational chatbot on student learning experience. Educ Inform Technol. 2024;29(8):10153–76. 10.1007/s10639-023-12166-w. [Google Scholar]
- 114.Nagpal DP, Ramesh KM. Investigating the nexus of intrinsic motivation learner engagement and satisfaction in the completion of MOOC courses. SPAST Reports. 2024. 10.69848/sreports.v1i2.4959. [Google Scholar]
- 115.Santo LD, Peña-Jimenez M, Canzan F, Saiani L, Battistelli A. The emotional side of the e-learning among nursing students: the role of the affective correlates on e-learning satisfaction. Nurse Educ Today. 2022;110: 105268. 10.1016/j.nedt.2022.105268. [DOI] [PubMed] [Google Scholar]
- 116.Zhu Y, Zhang JH, Au W, Yates G. University students’ online learning attitudes and continuous intention to undertake online courses: a self-regulated learning perspective. Educ Technol Res Dev. 2020;68:1485–519. [Google Scholar]
- 117.Akhteh MP, Farrokhnia M, Banihashem SK, Noroozi O. The Relationship between Students’ Satisfaction and Motivation and their Perceived Learning Outcome in an Online Peer Feedback Module. Studies on Education, Science, and Technology: ISTES; 2022. p. 297–310.
- 118.Alsaedi AA. AI-Powered Pedagogy: Revolutionizing students’learning experiences through integration of AI technologies. 1257. 2024. https://scholarworks.uaeu.ac.ae/all_theses/1257.
- 119.Zhou F, Ahmad RAHR. The impact of learning motivation on students’ academic performance: a self-determination theory perspective. J Educ Human Soc Res. 2025;2(1):155–63. [Google Scholar]
- 120.Avcı Ü. Students’ GAI Acceptance: Role of demographics, creative mindsets, anxiety, attitudes. J Comput Inform Syst. 2024. 10.1080/08874417.2024.2386545. [Google Scholar]
- 121.Lamti S, El Malhi M, Sekhsoukh R, Kerzazi N, editors. Intelligent Tutoring System for Medical Students: Opportunities and Challenges. Advances in Smart Medical, IoT & Artificial Intelligence; 2024; Cham: Springer Nature Switzerland.
- 122.Pertiwi RWL, Kulsum LU, Hanifah IA. Evaluating the Impact of Artificial Intelligence-Based Learning Methods on Students’ Motivation and Academic Achievement. International Journal of Post Axial: Futuristic Teaching and Learning. 2024:49–58.
- 123.Nguyen VTT, Chen H-L. Examining impacts of information system success and perceived stress on students’ self-regulated learning mediated by intrinsic motivation in online learning environments: second-order structural equation modelling analyses. Educ Inform Technol. 2023;28(10):12945–68. 10.1007/s10639-023-11685-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Guo J, Li H. Optimization and management of communication technology in smart education environments. J Edu Human Soc Res. 2025;2(2):53–64. 10.71222/b93b9d98. [Google Scholar]
- 125.Rehan H. Shaping the future of education with cloud and AI technologies: enhancing personalized learning and securing data integrity in the evolving EdTech landscape. Aust J Mach Learn Res Appl. 2023;3(1):359–95. [Google Scholar]
- 126.Vasou M, Kyprianou G, Amanatiadis A, Chatzichristofis SA, editors. Transforming Education with AI and Robotics: Potential, Perceptions, and Infrastructure Needs. Information Systems; 2025; Cham: Springer Nature Switzerland.
- 127.Schrader C, Bastiaens T. Learning in educational computer games for novices: the impact of support provision types on virtual presence, cognitive load, and learning outcomes. Int Rev Res Open Distrib Learn. 2012;13(3):206–27. 10.19173/irrodl.v13i3.1166. [Google Scholar]
- 128.Huang AYQ, Lu OHT, Yang SJH. Effects of artificial Intelligence-Enabled personalized recommendations on learners’ learning engagement, motivation, and outcomes in a flipped classroom. Comput Edu. 2023;194:104684. 10.1016/j.compedu.2022.104684. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.