Abstract
Background
Mastering neuroanatomy is a cornerstone of neurosurgical training. Conventional neuroanatomy teaching is conducted with 2-dimensional (2D) images in a lecture format. These 2D methods of teaching neuroanatomy may not be adequate in inculcating a telescopic 3-dimensional (3D) visualisation of neuroanatomy which is necessary in neurosurgery. One such manner of nurturing a 3D understanding of anatomy is with the use of 3D stereoscopic photographs of cadaveric specimens. We conducted a neuroanatomy course comprised of such 3D stereoscopic images, to gauge its effectiveness in neuroanatomical learning amongst neurosurgical trainees of differing seniorities.
Methods
A 10-session neuroanatomy course was conducted over 3 months in our institution. This course was prepared by the senior author and was composed of 3D stereoscopic visualisation (3DSV) of cadaveric dissections based on the 3D Rhoton collection. The course was administered to neurosurgical practitioners of differing experience and seniority, with each session lasting 2 to 3 hours, with audience interaction. Post-course surveys were conducted to assess usefulness - by utilising questions from the extended Kirkpatrick model, comparing 3DSV to 2D delivery and self-ratings of learner satisfaction and self-confidence. Analysis of the results included analysis of medians and proportions.
Results
Twenty-one participants responded to the survey. Learners were medical officers, junior residents, senior residents and consultants, with the median learner being a junior resident. There was strong agreement amongst learners that the course was enjoyable (85.7%) and that it enhanced their understanding of neuroanatomy (90.5%). The majority of learners (59.0%) indicated that the course inspired behavioural change and that it would contribute positively to anatomy examination performance (71.4%). Compared to 2D delivery, all the participants felt that 3DSV facilitated better spatial understanding of complex neuroanatomical structures and that it helped to increase familiarity with digital learning platforms. The course was accorded a mean grade of 9.1/10 (SD: 0.91). The majority of learners strongly agreed with regards to learner satisfaction (62.8%) and learner self-confidence (52.3%).
Conclusions
A structured 3D neuroanatomy course over 10-weeks is highly effective in enhancing spatial understanding, learner satisfaction and self-confidence amongst neurosurgical trainees and practitioners of differing seniorities.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-025-07901-5.
Keywords: 3-Dimensional anatomy, Stereoscopic anatomy, 3D stereoscopic visualisation, Technology enhanced learning, Neuroanatomy, 3D learning, Kirkpatrick model, Learner satisfaction and self-confidence
Introduction
Neuroanatomy is an important pillar of neurosurgical training, and it is considered to be the science most fundamental to Neurosurgery [1]. Mastering neuroanatomy however, is no easy feat - especially for neurosurgical trainees, with busy clinical service needs and the lack of formal postgraduate neuroanatomy education [2]. The gold-standard for anatomy education, and especially neuroanatomical education, is that of cadaveric dissection, which allows for learners to appreciate the complex 3-dimensional (3D) relationship of neural structures and train their psychomotor operative abilities at the same time [3, 4]. Practically though, neuroanatomy is traditionally taught with two-dimensional (2D) illustrations or photographs in textbooks and presentations, which are effective but limited in conveying the complex three-dimensional (3D) structures inherent in neuroanatomy [5–7]. These 2D illustrations often struggle to provide a clear and accurate representation of the complexities of the structures of the brain and skull for the learner [8]. In recent years, the teaching of neuroanatomy has been evolving slowly with the integration of technologies such as 3D stereoscopic visualisation (3DSV), augmented reality (AR) and virtual reality (VR) [9, 10]. Such modalities offer an opportunity to bridge the gap between cadaveric dissection and 2D illustrations, by highlighting the 3D anatomical relationships between neural structures, and providing a realistic anatomical view [7, 11].
Worldwide, and especially after the COVID-19 pandemic, there has been increased adoption of technology-enhanced learning methods such as 3DSV, AR and VR, as well as the use of non-cadaveric plastic-based models to teach anatomy [12]. These non-cadaveric methods of anatomy instruction have been found to have similar learner performance, when compared with cadaveric dissection [13]. The use of 3DSV in particular, was found to have a significant positive effect on the acquisition of anatomical knowledge compared to traditional 2D methods, further emphasizing the importance of stereopsis in enhancing the educational experience in neuroanatomy teaching [14]. The need for technology-enhanced learning is highlighted by the limitations of cadaveric dissection based neuroanatomical learning in Singapore. The main problem is the shortage of cadavers [15] with other challenges being the fixed costs involved in having an anatomical dissection lab environment [16], the inability to access the cadavers at all times [17] and the need for competency before performing dissections.
For neuroanatomy education, 3DSV has been shown to enhance knowledge transfer, engagement, and retention of anatomical information amongst medical students [9, 18]. A similar study conducted with neurosurgical trainees yielded similar results, and showed that both 2D and 3D teaching methods were effective at improving self-rated knowledge and understanding, with the 3D lecture and course being associated with significantly greater gains in confidence for performing specific surgical approaches [19]. Stereoscopic 3D visualisation has also been shown to reduce cognitive load and improve engagement in neuroanatomical teaching, with learners preferring the 3D instruction to traditional 2D instruction [20, 21].
Despite the purported benefits of 3DSV, we found that such instruction was limited to short courses or lectures [9, 19], which were inadequate in imparting the necessary knowledge and inculcating the telescopic vision required for appreciating neuroanatomy relevant to neuroanatomy. Furthermore, we found that the literature was either focused on medical student education, making the course content relatively basic, or involved short courses in evaluating the effectiveness of 3DSV. Hence, we conducted a comprehensive 10-week 3DSV-based neuroanatomy course, to gauge its effectiveness, both quantitatively and qualitatively, in neuroanatomical learning amongst neurosurgical trainees of differing seniorities. We hypothesised that 3DSV based neuroanatomy would be effective in neuroanatomical and neurosurgical education amongst learnings of differing seniorities.
Methods
We conducted a 10-session neuroanatomy course from February to April 2024, in the National Neuroscience Institute, Singapore. The course was conceptualised by and conducted by the senior author using electronic material from the 3D Rhoton collection [22]. It consisted of 3D photographs of cadaveric dissections and diagrams curated to suit the topic. The course was administered to both junior and senior clinicians from the department of Neurosurgery, in face-to-face sessions.
The 3DSV content were prepared by the senior author and were projected onto a screen using a 3D-enabled BenQ projector (BenQ corporation, Taipei, Taiwan). Participants were also each provided a pair of electronic BenQ 3D glasses (BenQ corporation, Taipei, Taiwan). Sessions were conducted in a meeting room with active interaction between the senior author and learners. This setting was chosen deliberately to allow for active participation, allowing for the lesson to be stopped for clarifications and so that the displayed material is close to the learners, to stimulate and promote their visuospatial ability [23].
Ethics approval and consent to participate
This project was exempted from ethics approval since there was no individually-identifiable human medical information in this project and the course material was based on publicly available information. In accordance with the Human Biomedical Research Act 2015 [24] in Singapore, the material used in this study is not considered human tissue and the research conducted is not considered to be human biomedical research, hence exempting it from any ethics review or Institutional Review Board (IRB) review. Ethical norms, such as the Declaration of Helsinki [25], were adhered to, and informed consent was obtained from all human participants.
Course topics
The course schedule was planned in a logical fashion with an initial introduction to cortical surface anatomy followed by more complex topics. During the conduct of each session, a quick recap of the previous weeks topics and important cortical surface anatomy was also included, to aid recall in learners. Each session lasted for approximately 2 to 3 hours. Course topics and session details are depicted in Table 1.
Table 1.
Neuroanatomy course session details
| S/N | Topic | Date |
|---|---|---|
| 1 | Cortical anatomy | 9th February 2024 |
| 2 | White matter, subcortical, supratentorial ventricles | 16th February 2024 |
| 3 | Pineal region and 3rd ventricle | 23rd February 2024 |
| 4 | Temporal lobe and paralimbic structures | 23rd February 2024 |
| 5 | Supratentorial vessels and arteriovenous malformations | 1st March 2024 |
| 6 | Anterior fossa - endoscopic and open approaches | 15th March 2024 |
| 7 | Middle fossa and vasculature | 20th March 2024 |
| 8 | Posterior fossa and infratentorial vessels | 2nd April 2024 |
| 9 | Posterior fossa and approaches | 5th April 2024 |
| 10 | Brainstem | 10th April 2024 |
Post-course survey design
To evaluate the educational impact of the 3DSV neuroanatomy course, a post-course survey was administered electronically to all participants (n = 21) immediately following the final session. The survey consisted of 34 items, grouped into three key domains: (1) a custom-designed set of nine questions based on the extended Kirkpatrick model of training evaluation; (2) a 12-item section assessing learner perceptions of 3D vs. 2D instructional modalities; and (3) the modified National League for Nursing (NLN) Student Satisfaction and Self-Confidence in Learning Scale [26]. The full list of survey questions can be found in Appendix 1.
Extended Kirkpatrick model questions
The extended Kirkpatrick model, including the level for return on investment (ROI) as popularised by Phillips [27], is a popular approach to evaluate training and learning in organisations and has been used effectively for evaluation of teaching tools and methods [28], and in 3DSV based neuroanatomy [9]. We customised 9 questions to assess the five levels of the extended Kirkpatrick model:
Level 1 (Satisfaction/Enjoyment): Learner satisfaction and perceived enjoyment.
Level 2 (Learning): Self-reported knowledge gain and confidence in neuroanatomical understanding.
Level 3 (Behaviour): Anticipated behavioural changes in clinical or surgical practice.
Level 4 (Results): Perceived impact on examination performance.
Level 5 (Return on Investment): Perceived long-term impact on clinical efficiency.
Responses were collected using a 5-point Likert scale (1= strongly disagree, 5 = strongly agree). Where appropriate, item-level results were aggregated and reported descriptively (e.g. frequencies and proportions).
3D vs. 2D evaluation
The next 12 questions assessed differences between the 3D course vs traditional 2D teaching methods. Apart from grading of the course on a numerical scale from 0 to 10, these questions consisted of ‘Yes’ or ‘No’ responses. Learners who had prior exposure to 2D formats were specifically asked were asked to compare the 3DSV teaching approach to prior experiences with conventional 2D neuroanatomy education. Questions explored preferences, clarity of spatial understanding, physical comfort (e.g., eye strain), and perceived added value to clinical and surgical orientation.
Open-ended feedback was also solicited regarding desired future topics for 3D anatomy instruction.
NLN satisfaction and self-confidence in learning scale
We adapted the NLN (National League of Nursing) instrument, Student Satisfaction and Self-confidence in Learning Scale (SSSCLS) to include five questions assessing satisfaction (items 22–26) and eight questions assessing self-confidence (items 27–34). All items were rated using a 5-point Likert scale. The instrument has been previously validated in health education settings [29], and modifications were limited to contextualising terminology for postgraduate learners in neurosurgery.
Data analysis
Descriptive statistics such as median values and interquartile ranges were used to summarise the Likert-scale responses. Categorical data were expressed as frequencies and percentages. Given the small sample size and ordinal nature of the Likert data, formal inferential statistics were not applied. Vertical bar charts were plotted for each of the 5 criteria: satisfaction/enjoyment, learning, behaviour, performance impact, return on investment (ROI). Horizontal bar charts were plotted for 3D vs 2D results. For satisfaction and self-confidence results, vertical bar charts and visual representation of item-level response distributions was generated using stacked bar charts. Graphs were plotted with GraphPad Prism version 10.0.0 for Windows (GraphPad Software, Boston, Massachusetts USA, www.graphpad.com)
Results
Demographics
A total of 21 learners participated in the study. There were 12 junior clinicians, 6 (28.6%) of whom were medical officers and the other 6 (28.6%) were junior residents. Out of the 9 senior clinicians, 4 (19.0%) were senior residents and 5 (23.8%) were consultants. Amongst the junior clinicians, the median number of years of experience in the Neurosurgery department was 4.5 years (IQR 4). Seven (33.0%) learners attended 1 to 3 sessions, 6 (29%) learners attended 4 to 6 sessions, and 8 (38.0%) learners attended 7 to 10 sessions. All participants completed the post-course survey.
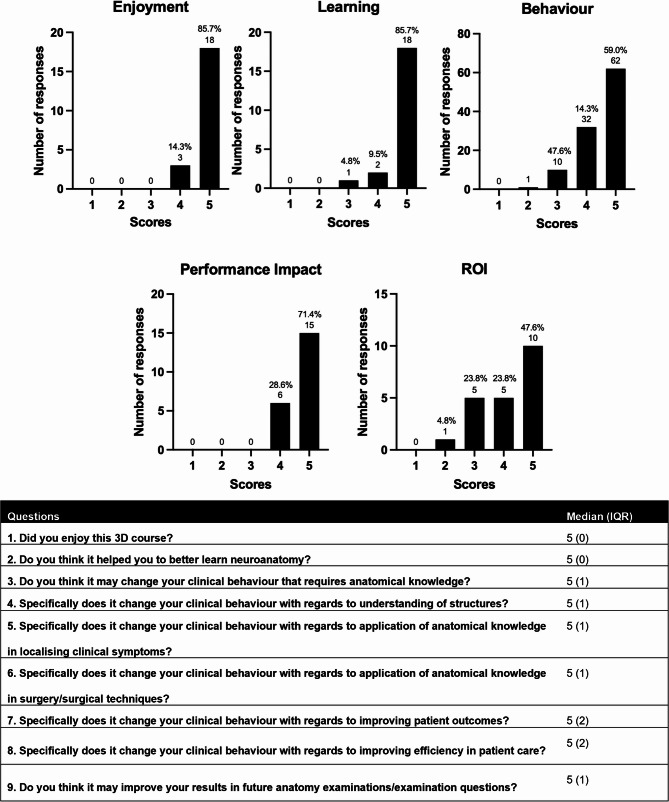
Training evaluation based on the extended Kirkpatrick model
Most learners (85.7%) strongly agreed (5/5) that they enjoyed the 3D course, and 19 learners (90.5%) strongly agreed that it enhanced their understanding of neuroanatomy. Regarding behavioural change, 59.0% (62/105) of the Likert-scale responses across the five relevant questions were rated as 5/5, indicating that the majority perceived potential impact on clinical application, including anatomical localisation, surgical technique, and symptom interpretation. Fifteen learners (71.4%) strongly agreed that the course may contribute positively to future anatomy examination performance, while 10 learners (47.6%) indicated it could enhance efficiency in clinical care. The median score for all the questions were 5, with the interquartile ranges (IQR) being between 0 to 2. The full distribution of responses is illustrated in Figure 1.
Fig. 1.
Responses to extended Kirkpatrick model questions. Question 1 assesses enjoyment, question 2 assesses learning, questions 3–7 assesses behaviour, question 8 assesses ROI, and question 9 assesses performance impact. Abbreviations: IQRInterquartile Range, ROIReturn on Investment
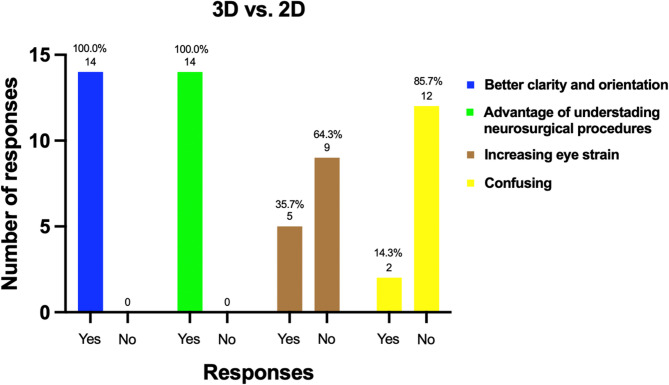
3D Delivery questions and comparison with 2D
All participants rated the overall 3D course experience highly, with a median score of 9/10. Every respondent (100%) agreed that the 3D format facilitated spatial understanding of complex neuroanatomical structures and helped increase familiarity with digital learning platforms.
Fourteen learners (66.7%) had prior exposure to conventional 2D neuroanatomy teaching. Among these, all reported that the 3D approach provided clear additional benefits as shown in Figure 2. Specifically, 12 out of 14 learners (85.7%) did not find the stereoscopic modality more confusing than 2D, and 9 (64.3%) did not report increased eye strain. All learners in this subgroup (100%) perceived improvements in surgical orientation, anatomical clarity, and procedural understanding when using 3D instructional materials.
Fig. 2.
Responses to questions comparing 3D vs. 2D modalities. Abbreviations: 3D 3-Dimensional, 2D 2-Dimensional
For the open-ended feedback question, most learners did not have additional comments. One learner found that the neuroanatomy course was too difficult for beginners. Others provided suggestions for future course topics such as spinal neuroanatomy, cerebrovascular anomalies, and neuroembryology.
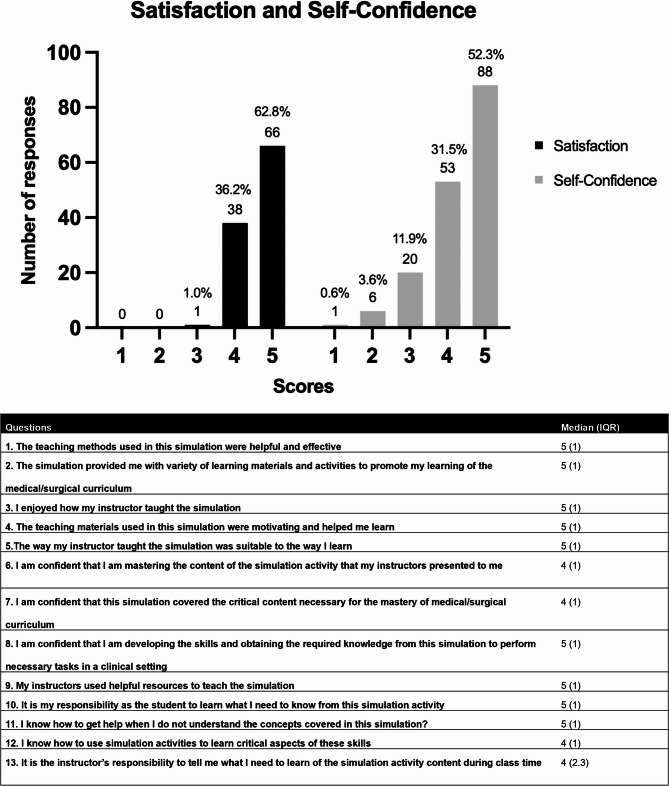
Student satisfaction and self-confidence in learning scale
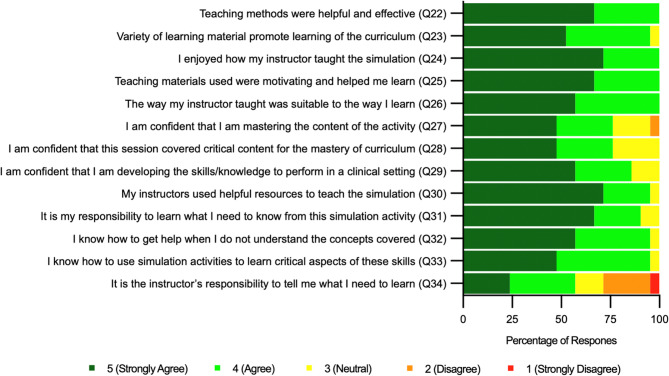
For the 5 questions on satisfaction in the post-course survey (items numbered 22 to 26 in Appendix 1), a total of 66 out of 105 responses (62.8%) gave a score of 5/5. Fourteen (66.7%) learners strongly agreed that the teaching methods used were helpful and effective, 11 (52.4%) learners strongly agreed that the sessions provided them with a variety of learning materials and activities to promote their learning and 15 (71.4%) learners strongly agreed that they enjoyed how the instructor taught. Fourteen (66.7%) learners strongly agreed that the teaching materials used were motivating and helped them to learn, and 12 (57.1%) learners strongly agreed that the way the instructor taught was suitable to the way they learnt. For the next 8 questions on self-confidence (items numbered 27 to 34 in Appendix 1), 88 out of 168 (52.3%) respondents gave a score of 5/5. Ten (47.6%) learners strongly agreed that they were confident that they were mastering the content of the activity, 10 (47.6%) learners strongly agreed that they were confident that the course helped them to master critical content, and 12 (57.1%) learners strongly agreed that they were developing the skills and knowledge necessary to perform tasks in a clinical setting. Fifteen (71.4%) learners strongly agreed that the instructor used helpful resources to teach, 14 (66.7%) learners strongly agreed that it was their responsibility as a student to learn what is needed to be known from the course and 12 (57.1%) learners strongly agreed that they know how to get help when they do not understand the concepts covered in the course. Less than half (10, 47.6%) of the learners strongly agreed that they knew how to use simulation activities to learn critical aspects of neurosurgical skills, and only 5 (23.8%) learners strongly agreed that it is the instructor’s responsibility to tell them what they need to learn during the course. The median values for all the questions ranged between 4 to 5 with IQR from 1 to 2.3. A full distribution of responses is shown in Figure 3 and Figure 4.
Fig. 3.
Responses to the Student Satisfaction and Self-Confidence in Learning Scale. Questions 1–5 assesses student satisfaction, and questions 6–13 assesses student self-confidence. Abbreviations: IQRInterquartile Range
Fig. 4.
Learner’s perceived satisfaction and self-confidence. These correspond to questions 22–34 in Appendix 1. Abbreviations: Q Question
Discussion
Out study demonstrated that a structured 10-week 3D stereoscopic neuroanatomy course is well received amongst learners of differing seniorities and has the ability to enhance learning outcomes for neurosurgical trainees in Singapore, as assessed through extended Kirkpatrick’s evaluation model and a validated learner satisfaction instrument. The overwhelmingly positive response from participants reflects not only strong engagement with the format but also meaningful gains in knowledge, confidence, and anticipated behavioural change. Our findings also align with existing literature, which supports the superiority of 3D stereoscopic education over traditional 2D teaching methods, especially in enhancing learning efficiency and shortening learning curves by facilitating a deeper understanding of key spatial relationships [30].
Our results show that a majority of respondents rated the course to be highly enjoyable. this bodes well for 3DSV as a teaching medium, since the literature suggests that enjoyment in the learning process enhances learner confidence, fosters engagement, and improves recall [31]. There was also strong learner satisfaction and self-confidence, as measured by the adapted NLN scale. High ratings across both subscales reinforce the acceptability of the 3D format and suggest that the course may positively influence motivation and learner autonomy. This positive reception underscores the potential of 3D education and opens avenues for exploring other technology-driven learning modalities, such as augmented reality (AR) and virtual reality (VR), in neurosurgical education.
A particularly notable finding is the marked improvement in spatial understanding reported by the majority of trainees. This suggests that stereoscopic visualisation may address a long-standing challenge in neuroanatomy education: the difficulty of mentally reconstructing three-dimensional relationships from two-dimensional sources such as atlases or CT/MRI slices [32, 33]. Unlike conventional approaches, the immersive format used in this course provided consistent depth cues, which may have facilitated the development of durable internal models of complex anatomical structures for each learner. These internal models are essential for safe and efficient neurosurgical practice, especially when navigating intricate regions such as the brainstem, ventricular system, and skull base [34].
Importantly, the course appeared to exert influence beyond cognitive gains. At level 3 on the extended Kirkpatrick model, trainees indicated behavioural changes, such as increased use of anatomical reasoning during surgical planning. While these behavioural shifts were self-reported and not directly observed, they suggest that the stereoscopic format may promote more anatomically grounded clinical thinking. Furthermore, the anticipation of improved operative outcomes (Level 5) points to the potential long-term value of the course, although this would require further investigation through performance-based assessments or clinical audits. An interesting finding however was the lower scores in these 2 categories compared to other categories. This may be attributed to differences in anatomical knowledge across seniority levels. Junior trainees, in particular, may have less experience with neuroanatomy, making it harder for them to appreciate its clinical relevance.
Some trainees highlighted that the course was not beginner-friendly and that the subject matter was complex for beginners. We expected this feedback when designing this course, and made a deliberate decision not to lower the standard of instruction or of the content matter. We believe that junior learners may not be able to grasp all the concepts that were taught, but instead of lowering the standard of the content, we will bridge this gap with repetition instead. This ensures that learners are taught neuroanatomy at a correct standard which is required for neurosurgical training.
The results also highlight the limitations of traditional 2D instruction. Nearly all participants with prior exposure to 2D neuroanatomy indicated that the stereoscopic approach was superior, particularly in helping them visualise deep structures and understand their spatial orientation. While 3D stereoscopic education may not entirely replace traditional teaching methods, these findings support the integration of immersive visual technologies into surgical training, aligning with broader shifts towards simulation-based and experiential learning in medical education. It should be integrated with existing modalities such as cadaveric dissection, potentially serving as a preparatory tool before attending cadaveric courses. Wilson et al. (2018) similarly advocated for its use as a stepping stone to enhance anatomical learning [13].
Study limitations
Despite these promising findings, the study has several limitations. First, the small cohort size and single-institution setting may limit generalisability. While the 100% response rate strengthens internal validity, larger, multicentre trials would be needed to confirm these outcomes and explore variation across learner levels or cultural contexts. The outcomes at extended Kirkpatrick Levels 3, 4 and 5 were based on self-reporting, which introduces the risk of overestimation due to social desirability bias. Objective assessments, such as pre- and post-course testing on neuroanatomical subject matter, Objective Structured Assessment of Technical Skills (OSATS), or longitudinal follow-up, would provide more definitive evidence of knowledge retention and behavioural impact. Our questionnaire also required participants to fill in their name for logistical purposes of differentiating learners by seniority, but this in turn could have introduced social desirability bias as well, and could have discouraged negative or more critical responses within the small participant pool. Whilst most participants reported minimal adverse effects, one individual experienced transient visual discomfort, underscoring the need for careful ergonomic design in future stereoscopic programmes. Lastly, there was the absence of a control group taught using 2D materials hence preventing direct comparative analysis.
Future directions
This study opens several avenues for future work. There is considerable interest among trainees in expanding the range of anatomical content delivered using 3D stereoscopy — notably, for vascular structures and spinal structures. These are all areas where spatial complexity often hinders learning. Thus, future efforts should focus on developing original 3D photogrammetry images for brain and spine anatomy and expanding 3D neuroanatomy courses. Establishing a dedicated education group to advance neuroanatomy teaching with emerging technologies will be crucial. These initiatives will enhance surgical competence and confidence, ultimately improving the application of knowledge and allowing for the use of 3D stereoscopic tools for surgical planning. One good example of this would be the Dextroscope [35], which can be utilised for preoperative planning in a 3D environment. In the long run, integrating stereoscopic modules with surgical simulation or navigation systems may offer synergistic benefits, bridging the gap between didactic learning and operative performance. This work also is a foray into analysing the effectiveness of 3D stereoscopic visualisation in neuroanatomy education, and we plan to further these efforts with more rigorous pre-course and post-course testing, with questions aimed to assess the subject content, and by introducing anonymity into surveys, to encourage more candid responses. Moreover, we are interested to ascertain if there is an association between surgical experience and the usefulness of 3D neuroanatomy teaching, and to interrogate the specific manner in which surgical experience interacts with neuroanatomy education.
Conclusion
This study demonstrates that a 10-week 3D stereoscopic neuroanatomy course is highly effective in enhancing spatial understanding, learner satisfaction and self-confidence amongst neurosurgical trainees and practitioners. These findings were concordant between both senior and junior learners. Our findings support the integration of immersive visualisation into surgical education and highlight its potential to address the gaps in traditional 2D teaching. Future work should focus on objective assessment of outcomes and broader implementation across training centres.
Supplementary Information
Acknowledgements
Nil.
Abbreviations
- 2D
2-dimensional
- 3D
3-dimensional
- 3DSV
3-dimensional stereoscopic visualisation
- AR
Augmented reality
- VR
Virtual reality
- NLN
National League of Nursing
- SSSCLS
Student satisfaction and self-confidence in learning scale
- IQR
Interquartile range
Authors’ contributions
Conception and design: AAK, LJX, RWK; Acquisition of data: AAK, HLL, LTQ; Analysis and interpretation of data: AAK, SJP, HLL; Drafting the article: AAK, SJP, HLL, LTQ, LJX, RWK; Critically revising the article: AAK, SJP, LJX, RWK; All authors reviewed the submitted version of manuscript and approved the final version of the manuscript.
Funding
The authors do not have any funding to declare for this manuscript.
Data availability
The 3D Rhoton collection is available online and study data is available upon reasonable request.
Declarations
Ethics approval and consent to participate
This study was carried out with adherence to the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rhoton AL Jr. Rhoton’s cranial anatomy and surgical approaches. Oxford University Press; 2019. [Google Scholar]
- 2.Joshi S, Khan M, Jelen MB, Pandit AS. Current attitudes toward neuroanatomy: A comparative Cross-Sectional survey of neurosurgeons from the united Kingdom and worldwide. World Neurosurg. 2022;166:e607–23. [DOI] [PubMed] [Google Scholar]
- 3.Yaşargil MG. A legacy of microneurosurgery: memoirs, lessons, and axioms. Neurosurgery. 1999;45(5):1025. [DOI] [PubMed] [Google Scholar]
- 4.Yadav YR, Parihar V, Ratre S, Kher Y, Iqbal M. Microneurosurgical skills training. J Neurol Surg Part A: Cent Eur Neurosurg. 2016;77(02):146–54. [DOI] [PubMed] [Google Scholar]
- 5.Uruthiralingam U, Rea PM. Augmented and virtual reality in anatomical education - a systematic review. Adv Exp Med Biol. 2020;1235:89–101. [DOI] [PubMed] [Google Scholar]
- 6.Narang P, Raju B, Jumah F, Konar SK, Nagaraj A, Gupta G, et al. The evolution of 3D anatomical models: a brief historical overview. World Neurosurg. 2021;155:135–43. [DOI] [PubMed] [Google Scholar]
- 7.Vezirska D, Milev M, Laleva L, Nakov V, Spiriev T. Three-dimensional printing in neurosurgery: a review of current indications and applications and a basic methodology for creating a three-dimensional printed model for the neurosurgical practice. Cureus. 2022;14(12):e33153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandralegar A, Bernard F, Khatchatourov S, Janssen I, Schaller K, Bijlenga P, et al. Mixed reality compared to the traditional ex cathedra format for neuroanatomy learning: the value of a three-dimensional virtual environment to better understand the real world. Neurosurg Focus. 2024;56(1):E14. [DOI] [PubMed] [Google Scholar]
- 9.Jacquesson T, Simon E, Dauleac C, Margueron L, Robinson P, Mertens P. Stereoscopic three-dimensional visualization: interest for neuroanatomy teaching in medical school. Surg Radiol Anat. 2020;42(6):719–27. [DOI] [PubMed] [Google Scholar]
- 10.Neyem A, Cadile M, Burgos-Martínez SA, Farfán Cabello E, Inzunza O, Alvarado MS, et al. Enhancing medical anatomy education with the integration of virtual reality into traditional lab settings. Clin Anat. 2024. 10.1002/ca.24213. [DOI] [PubMed] [Google Scholar]
- 11.Torregrossa F, Peris-Celda M, Spiriev T, Zoia C, Drosos E, Aldea C, et al. A spotlight on cadaveric dissection in neurosurgical training: the perspective of the EANS young neurosurgeons committee. Brain and Spine. 2024;4:102839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Attardi SM, Harmon DJ, Barremkala M, Bentley DC, Brown KM, Dennis JF, et al. An analysis of anatomy education before and during Covid-19: August-December 2020. Anat Sci Educ. 2022;15(1):5–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson AB, Miller CH, Klein BA, Taylor MA, Goodwin M, Boyle EK, et al. A meta-analysis of anatomy laboratory pedagogies. Clin Anat. 2018;31(1):122–33. [DOI] [PubMed] [Google Scholar]
- 14.Bogomolova K, Hierck BP, Looijen AEM, Pilon JNM, Putter H, Wainman B, et al. Stereoscopic three-dimensional visualisation technology in anatomy learning: a meta-analysis. Med Educ. 2021;55(3):317–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loh N. Anatomical Dissection: Experiences and Education. SMA NEWS [Internet]. 2021 23 March 2025. Available from: https://www.sma.org.sg/news/2021/july/Anatomical-Dissection-Experiences-and-Education
- 16.Takoutsing BD, Wunde UN, Zolo Y, Endalle G, Djaowé DAM, Tatsadjieu LSN, et al. Assessing the impact of neurosurgery and neuroanatomy simulation using 3D non-cadaveric models amongst selected African medical students. Front Med Technol. 2023;5:1190096. [DOI] [PMC free article] [PubMed]
- 17.Veeraraghavan VP. Comparing the benefits and drawbacks of traditional and online anatomy learning in medical education. Med Sci Educ. 2024;34(2):501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evins AI, Rothbaum M, Kim N, Guadix SW, Boyette D, Xia JJ, et al. A novel 3D surgical neuroanatomy course for medical students: outcomes from a pilot 6-week elective. J Clin Neurosci. 2023;107:91–7. [DOI] [PubMed] [Google Scholar]
- 19.Clark AD, Guilfoyle MR, Candy NG, Budohoski KP, Hofmann R, Barone DG, et al. Stereoscopic Three-Dimensional Neuroanatomy Lectures Enhance Neurosurgical Training: Prospective Comparison with Traditional Teaching. World Neurosurg. 2017;108:917–23. [DOI] [PubMed] [Google Scholar]
- 20.Yohannan DG, Oommen AM, Kumar AS, Devanand S, Ut MR, Sajan N, et al. Visualization matters - stereoscopic visualization of 3D graphic neuroanatomic models through AnaVu enhances basic recall and radiologic anatomy learning when compared with monoscopy. BMC Med Educ. 2024;24(1):932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newman HJ, Meyer AJ, Wilkinson TJ, Pather N, Carr SE. Technology enhanced neuroanatomy teaching techniques: a focused BEME systematic review of current evidence: BEME guide 75. Med Teach. 2022;44(10):1069–80. [DOI] [PubMed] [Google Scholar]
- 22.Sorenson J. The rhoton collection. J Neurol Surg B Skull Base. 2016;77(4):294–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hadie SNH, Abdul Manan Sulong H, Hassan A, Mohd Ismail ZI, Talip S, Abdul Rahim AF. Creating an engaging and stimulating anatomy lecture environment using the cognitive load Theory-based lecture model: students’ experiences. J Taibah Univ Med Sci. 2018;13(2):162–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Human Biomedical Research Act. 2015, (2020).
- 25.Association WM. World medical association declaration of helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. [DOI] [PubMed] [Google Scholar]
- 26.Smidt A, Balandin S, Sigafoos J, Reed VA. The kirkpatrick model: a useful tool for evaluating training outcomes. J Intellect Dev Disabil. 2009;34(3):266–74. [DOI] [PubMed] [Google Scholar]
- 27.Phillips JJ. ROI: the search for best practices. Train Dev. 1996;50(2):42–8. [Google Scholar]
- 28.Gillanders SL, McHugh A, Lacy PD, Thornton M. Safe surgical training: evaluation of a national functional endoscopic sinus surgery model simulation course using the Kirkpatrick evaluation model. Ir J Med Sci. 2023;192(6):3039–42 ((1971 -)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franklin AE, Burns P, Lee CS. Psychometric testing on the NLN student satisfaction and self-confidence in learning, simulation design scale, and educational practices questionnaire using a sample of pre-licensure novice nurses. Nurse Educ Today. 2014;34(10):1298–304. [DOI] [PubMed] [Google Scholar]
- 30.Benet A, Tabani H, Griswold D, Zhang X, Kola O, Meybodi AT, et al. Three-dimensional imaging in neurosurgical research and education. World Neurosurg. 2016;91:317–25. [DOI] [PubMed] [Google Scholar]
- 31.de Faria JW, Teixeira MJ, de Moura Sousa Júnior L, Otoch JP, Figueiredo EG. Virtual and stereoscopic anatomy: when virtual reality Meets medical education. J Neurosurg. 2016;125(5):1105–11. [DOI] [PubMed] [Google Scholar]
- 32.Hegarty M, Keehner M, Cohen C, Montello DR, Lippa Y. Applied spatial cognition: From research to cognitive technology. Lawrence Erlbaum Associates; 2007. [Google Scholar]
- 33.Council NR. Learning to Think Spatially. Washington, DC: The National Academies Press; 2006. 332 p. 10.17226/11019.
- 34.Abarca-Olivas J, González-López P, Fernández-Cornejo V, Verdú-Martínez I, Martorell-Llobregat C, Baldoncini M, et al. 3D stereoscopic view in neurosurgical anatomy: compilation of basic methods. World Neurosurg. 2022;163:e593–609. [DOI] [PubMed] [Google Scholar]
- 35.González Sánchez JJ, Enseñat Nora J, Candela Canto S, Rumià Arboix J, Caral Pons LA, Oliver D, et al. New stereoscopic virtual reality system application to cranial nerve microvascular decompression. Acta Neurochir (Wien). 2010;152(2):355–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The 3D Rhoton collection is available online and study data is available upon reasonable request.