Abstract
Vertical transmission of Brucella abortus in Sprague-Dawley (SD) rats was verified with microbiologic, serologic, and polymerase chain reaction (PCR) methods. The 38 initially Brucella-free SD rats, weighing 200 to 250 g, were injected subcutaneously with 50 μL of a suspension containing 1 × 109 colony-forming units (cfu) of B. abortus biotype 1 Korean isolate. The rats were allowed to mate with uninfected SD rats. The isolate was detected by culture and by AMOS (abortus, melitensis, ovis, suis) PCR in testis tissue of infected male rats and splenic tissue of infected female rats. By 7 d after inoculation, the results of both the rose bengal test (RBT) and the plate agglutination test (PAT) were positive for antibody against B. abortus; the reciprocal antibody titre ranged from 200 to 400 in the 1-mo-old offspring and 800 in their dams. The infected rats directly transmitted Brucella to their breeding partners and offspring. Fetuses of infected dams were found to be infected at 20 d of gestation. These data are discussed in relation to a model for epizootic and zoonotic cases possibly involving wild animals. Additional rigorous experiments are warranted to explore the value of this model in developing measures to prevent congenital brucellosis.
Résumé
La transmission verticale de Brucella abortus chez des rats Sprague-Dawley (SD) a été vérifiée par méthodes microbiologiques, sérologiques et par réaction d’amplification en chaîne par la polymérase (PCR). Les 38 rats SD exempts de Brucella et pesant 200 à 250 g, ont été injectés par voie sous-cutanée avec 50 μL d’une suspension contenant 1 × 109 unités formatrices de colonie (ufc) d’un isolat coréen de B. abortus biotype 1. Les rats ont pu s’accoupler avec des rats SD non-infectés. Les isolats ont été détectés par culture et par PCR AMOS (abortus, melitensis, ovis, suis) sur le tissu testiculaire des mâles infectés et du tissu splénique des rates infectées. Sept jours après l’inoculation, les résultats du test au rose bengal (RBT) et de l’agglutination sur plaque (PAT) étaient positifs pour la présence d’anticorps anti-B. abortus; les titres réciproques d’anticorps variaient entre 200 et 400 chez les rejetons de 1 mois et 800 chez leur mère. Les rats infectés transmettaient directement B. abortus à leur partenaire d’accouplement et à leurs rejetons. Les fœtus des femelles infectées étaient infectés au jour 20 de gestation. Ces données sont discutées en relation avec un modèle pour une épizootie et des cas zoonotiques impliquant possiblement des animaux de la faune. Des expériences supplémentaires avec plus de rigueur sont requises pour explorer la valeur de ce modèle à développer des mesures pour prévenir la brucellose congénitale.
(Traduit par Docteur Serge Messier)
Brucellosis, a zoonotic disease caused by members of the genus Brucella, affects both humans (1) and animals such as cattle, sheep, goats, swine, and dogs (2). Wildlife are also susceptible and may play a role in transmission to domestic animals and humans (3). Brucella abortus has been isolated from rats (3). Generally, rat infections occur in areas with large numbers of infected cattle (2), which suggests that cattle are an important source of infection for rats through direct or indirect contact. Direct venereal transmission of infection from ewe to ram has been reported as a rare event (4).
The vertical transmission of B. abortus from cow to calf has been well documented in cattle, the calves remaining seronegative for months and even years (5). In sheep, the importance of ewes in the transmission of infection has not been fully clarified, the opinion being that females do not play a significant role in the maintenance of Brucella infection (5). In humans, vertical transmission of brucellosis has recently been demonstrated (6).
The Korean government has undertaken a surveillance program to eradicate bovine brucellosis, but there is still a serious problem in dairy (Holstein) and indigenous Korean beef (Han woo) cattle. Outbreaks affected 4076 head of cattle in 2004 (7). The program mandates that animals testing positive for brucellosis be slaughtered immediately. Measures to control brucellosis in wildlife, including vaccination, need to be addressed. At present, even in the face of the powerful tools of modern molecular technology, there is no known example of eradication of brucellosis from free-ranging wildlife populations without eradication of the infected populations.
No data are available on the vertical transmission of B. abortus in wild animals. We undertook this study to determine whether B. abortus could be transmitted venereally or vertically from experimentally infected rats to uninfected ones as a potential model for studies of bovine brucellosis.
We used a Korean isolate of B. abortus biotype 1 for experimental infection throughout the study. Before inoculation, the strain was grown in Brucella broth (Difco, Kansas City, Missouri, USA) for 48 h at 37°C with 5% CO2. The organisms were washed 3 times and resuspended in physiologic saline. For the preparation of antigens for the rose bengal test (RBT) and the plate agglutination test (PAT), B. abortus 1119-3 was used, according to international standards (8). The master seed was initially propagated on Brucella agar (Difco) and continued in Brucella broth in a shaking incubator at 37°C and 45 × g. After 30 h of culture, the organisms were heat-inactivated at 95°C for 1 h.
We purchased 38 Sprague-Dawley (SD) rats, weighing 200 to 250 g, from a government-licensed commercial breeder. Included within this group of 38 were 12 offspring. The rats were dewormed with piperazine and housed, handled, and fed according to standard humane protocols approved by the guidelines of Chonbuk National University, Jeonju, Republic of Korea, for experimental animal use under the supervision of veterinarians. The animals were screened clinically, microbiologically, parasitologically, and serologically for evidence of disease. Any abnormalities precluded the animal from use in the experiment. Throughout the experiment, the animals were kept in a stringently hygienic, climate-controlled environment and provided with commercial feed and water ad libitum.
Each of 15 female rats and 10 male rats were injected subcutaneously with 50 μL of a suspension containing 1 × 109 colony-forming units (cfu) of the B. abortus biotype 1 Korean isolate in physiologic saline. Another 9 female and 4 male rats received the same volume of saline as a sham inoculation. We allowed 10 infected females and 5 infected males to mate with 6 control females and 2 control males 10 d after inoculation. Two infected females were caged with 1 uninfected male and 1 infected male was housed with 2 uninfected females. A similar pairing protocol was followed in the case of the control rats. Newborn rats remained with their dams until 1 mo of age, when they were euthanized to determine seroconversion and infection status by means of serology, culture, and AMOS (abortus, melitensis, ovis, suis) polymerase chain reaction (AMOS-PCR).
Clinical parameters, such as body temperature, appetite, and thirst, were monitored daily. Appetite and thirst were assessed from the exact quantities of food and water consumed. The rats were also evaluated for pregnancy, abortion, premature birth, and any other adverse reactions.
To isolate bacteria from blood, we obtained 1 mL of heparinized blood by cardiac puncture of live animals anesthetized with ketamine: from the males at 0, 7, and 50 d after inoculation; and from the females at 0 and 7 d after inoculation, at 20 d of gestation, and at 30 d after parturition. Males were euthanized at 0, 7, and 50 d, females at 0, 7, 20, and 50 d after inoculation, and offspring at 1 mo of age. Fetal spleen and testis samples were collected at approximately 20 d of gestation. Testis samples were collected from the euthanized male rats and spleen samples from the euthanized female rats. All tissue samples were stored for 48 h at 4°C before culture and bacteriologic examination; they were also processed as Brucella DNA templates for AMOS-PCR testing according to published protocols (9,10).
Blood was cultured at 37°C with 5% CO2 for 3 d in tryptose soy broth (Difco) containing bovine serum. Subcultures were made on tryptose soy agar (Difco) to assess the colonial and morphologic characteristics of the bacterial growth (8). Isolates were confirmed by PCR (9). In tissue samples, the organism’s identity was bio-chemically confirmed on the basis of CO2 requirements, H2S production, and growth in the presence of thionine and basic fuchsin (8).
For AMOS-PCR profiling (9,10), DNA was extracted from spleen and testis after homogenization with 2 mL of distilled water free of DNase and RNase after extraction with a masticator (Life Technologies, Boone, North Carolina, USA) and using a genomic DNA extraction kit (AccuPrep DNA Extraction Kit; Bioneer, Daejeon, Korea). Initially, AMOS-PCR was carried out on blood and tissue samples. The results with the blood samples were highly variable; therefore, all analyses were carried out on tissue samples.
For serologic monitoring, blood samples were collected by cardiac puncture at the intervals described above. Serum samples were stored at −20°C until screened by means of RBT and PAT (8), with use of inactivated B. abortus strain 1119-3.
All rats inoculated with B. abortus biotype 1 became lethargic, anorexic, and febrile within 24 h. The highest rectal temperature was 38°C (within 72 h). Since the normal temperature of the rat is 37°C to 38.7°C, these temperature changes were not considered significant. No other adverse reactions or clinical signs were observed after inoculation. Anorexia and increased thirst were evident at 3 d and became very severe at 5 d. Consumption normalized at 7 d.
The gestational periods and litter sizes were within the normal range in the infected and control groups. There was no evidence of abortion, premature birth, or stillbirth.
Serum from all the infected rats and their offspring was positive in both the RBT and the PAT (Tables I and II). The mean reciprocal antibody titre was 800 in both sexes 7 d after inoculation. At parturition, the mean RBT titre was 1:1600 in the female rats. The titre among 1-mo-old offspring ranged from 1:200 to 1:400; the mean titre in the dams was 1:800. Results in the control males, females, and offspring were consistently negative.
Table I.
Mean results of the rose Bengal test (RBT) and the plate agglutination test (PAT) in female Sprague-Dawley (SD) rats inoculated with Brucella abortus, their offspring, and control SD rats
| Sample collection time; reciprocal antibody titre (and n)
|
||||
|---|---|---|---|---|
| 30 d after parturition
|
||||
| Animal group n() | 7 d after inoculation | 20 d of gestation | Dam | Offspring |
| Inoculated (22) | 800 (2a) | 1600 (2) | 800 (6) | 200 to 400 (12) |
| Control (8) | — (2) | — (2) | — (2) | — (2) |
Euthanized 7 d after inoculation
Table II.
Mean results of the rose Bengal test (RBT) and plate agglutination test (PAT) in male Sprague-Dawley (SD) rats inoculated with Brucella abortus and control SD rats
| Sample collection time; reciprocal antibody titre (and n)
|
||||
|---|---|---|---|---|
| Animal group n() | Before inoculation | 7 d after inoculation | 50 d after inoculation | |
| Inoculated (10) | — (2) | 800 (2) | 400 to 800 (6) | |
| Control (10) | — (2) | — | — | |
Characteristic colonies of B. abortus biotype 1 were cultured from the blood of infected rats and from the spleen and testis tissue of the inoculated rats and their fetuses. The control rats and fetuses remained culture negative.
The predicted 498-base pair AMOS-PCR amplification profile was obtained with the spleen and testis samples from the infected rats and fetuses (Figure 1). The gels were immediately computer-scanned, photographed, interpreted, and saved. No amplicons were observed in specimens from the control animals, nor were there amplicons of other pathogenic agents commonly isolated from rats.
Figure 1.
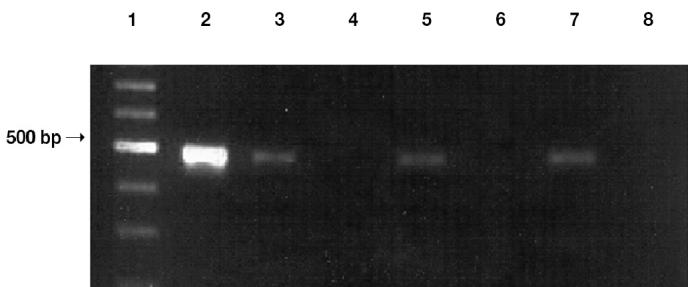
Typical amplification profile in the AMOS (abortus, melitensis, ovis, suis) polymerase chain reaction assay for DNA of Brucella abortus: lane 1 — 1100 base pair (bp) marker; lane 2 — DNA from a bacterial colony (500 bp); lanes 3 and 4 — DNA from an infected and an uninfected fetal rat, respectively; lanes 5 and 6 — DNA from the spleen of an infected and an uninfected female rat, respectively; lanes 7 and 8 — DNA from the testis of an infected and an uninfected rat, respectively.
In Korea and many other countries, schemes for eradicating brucellosis from cattle and sheep are generally based exclusively on serologic testing and slaughter of positive animals, with possible compensation for slaughter. The most successful strategy requires a combination of vaccination, testing, and slaughter (11).
Direct female-to-male venereal transmission has been reported to be rare in Brucella infection (5). We found that both female and male SD rats could play a determining role in maintaining Brucella infection originating from an infected sex partner. All the littermates from infected dams were serologically positive at 1 mo of age. Positive serologic results corresponded to positive AMOS-PCR results for fetuses of infected dams, and the predicted amplicon (498-bp) was consistently demonstrated.
According to the data for the 20-d-old fetuses, this study has established the occurrence of venereal and vertical transmission of B. abortus biotype 1 from infected female rats to uninfected male rats and vice versa. Infected rats could play a role in the maintenance and transmission of the infection among humans and domestic animals. Wild rats are known to harbour Brucella organisms (1,2). The transmission of B. abortus from dam to offspring has been well documented in cattle (5) and is considered to be a major source of latent infection. Carriers are extremely difficult to detect and constitute a major problem in the eradication of brucellosis because they are a potential source of relapse in previously infected herds (10). In bovine brucellosis, infection though neonatal consumption of infected colostrum has been suggested as a mode of transmission (5). It has been postulated that most latent infections of B. melitensis in sheep are acquired through the ingestion of infected colostrum or milk (4). In 1 experiment, Catlin and Sheehan (5) failed to isolate Brucella from aspirated amniotic fluid but found the calf to be serologically positive for brucellosis; they concluded that the calf was not infected in utero, but they did not verify transmission by PCR. In our study, AMOS-PCR and isolation of the organism proved that the fetuses were infected with B. abortus at 20 d of gestation. However, since the infected and uninfected rats were housed together, and the offspring were left with their infected dams, suckling ad libitum, the possibility of milk-derived infection and fecal-oral transmission cannot be precluded.
We believe that our study has demonstrated vertical transmission in rats experimentally infected with B. abortus biotype 1. Transmission was verified by AMOS-PCR and other conventional methods, including concurrent isolation of the organism. More importantly, the potential value of the SD rat model in the epizootiology and pathogenesis of bovine brucellosis has been demonstrated. Additional rigorous experiments are indicated to explore the value of this model in developing intervention measures against congenital brucellosis.
References
- 1.Young JE. An overview of human brucellosis. Clin Infect Dis. 1995;21:283–290. doi: 10.1093/clinids/21.2.283. [DOI] [PubMed] [Google Scholar]
- 2.Moore CG, Schnurrenberger PR. A review of naturally occurring Brucella abortus infections in wild mammals. J Am Vet Med Assoc. 1981;179:1105–1112. [PubMed] [Google Scholar]
- 3.Oliakova NV, Antoniuk VI. The gray rat as a carrier of infectious agents in Siberia and the Far East. Med Parasitol. 1989;3:73–77. [PubMed] [Google Scholar]
- 4.Marco J, Gonzalez L, Cuervo LA, et al. Brucella ovis infection in two flocks of sheep. Vet Rec. 1994;135:254–256. doi: 10.1136/vr.135.11.254. [DOI] [PubMed] [Google Scholar]
- 5.Catlin JE, Sheehan EJ. Transmission of bovine brucellosis from dam to offspring. J Am Vet Med Assoc. 1986;188:867–869. [PubMed] [Google Scholar]
- 6.Giannacopoulos I, Eliopoulou ML, Ziambaras T, Papanastasiou DA. Transplacentally transmitted congenital brucellosis due to Brucella abortus. J Infect. 2002;45:209–210. doi: 10.1016/s0163-4453(02)91043-1. [DOI] [PubMed] [Google Scholar]
- 7.Annual Report, Brucellosis: Ministry of Agriculture and Forestry, Republic of Korea. Available from: http://www.maf.go.kr/english Last accessed September 12, 2005.
- 8.Alton GG, Jones LM, Angus RD, Verger JM. Techniques for the Brucellosis Laboratory. Paris, France: Institut National de la Recherche Agronomique, 1988.
- 9.Ewalt DR, Bricker BJ. Validation of the abbreviated Brucella AMOS PCR as a rapid screening method for differentiation of Brucella abortus field strain isolates and the vaccine strains 19 and RB51. J Clin Microbiol. 2000;38:3085–3086. doi: 10.1128/jcm.38.8.3085-3086.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bricker BJ, Halling SM. Differentiation of Brucella abortus bv. 1, 2, and 4, Brucella melitensis, Brucella ovis, and Brucella suis bv. 1 by PCR. J Clin Microbiol. 1994;32:2660–2666. doi: 10.1128/jcm.32.11.2660-2666.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Animal and Plant Health Inspection Service. Brucellosis Eradication [c1998]. United States Department of Agriculture: Brucellosis. Available from: http://www.aphis.usda.gov/lpa/pubs/bruumr.pdf Last accessed September 12, 2005.


