Abstract
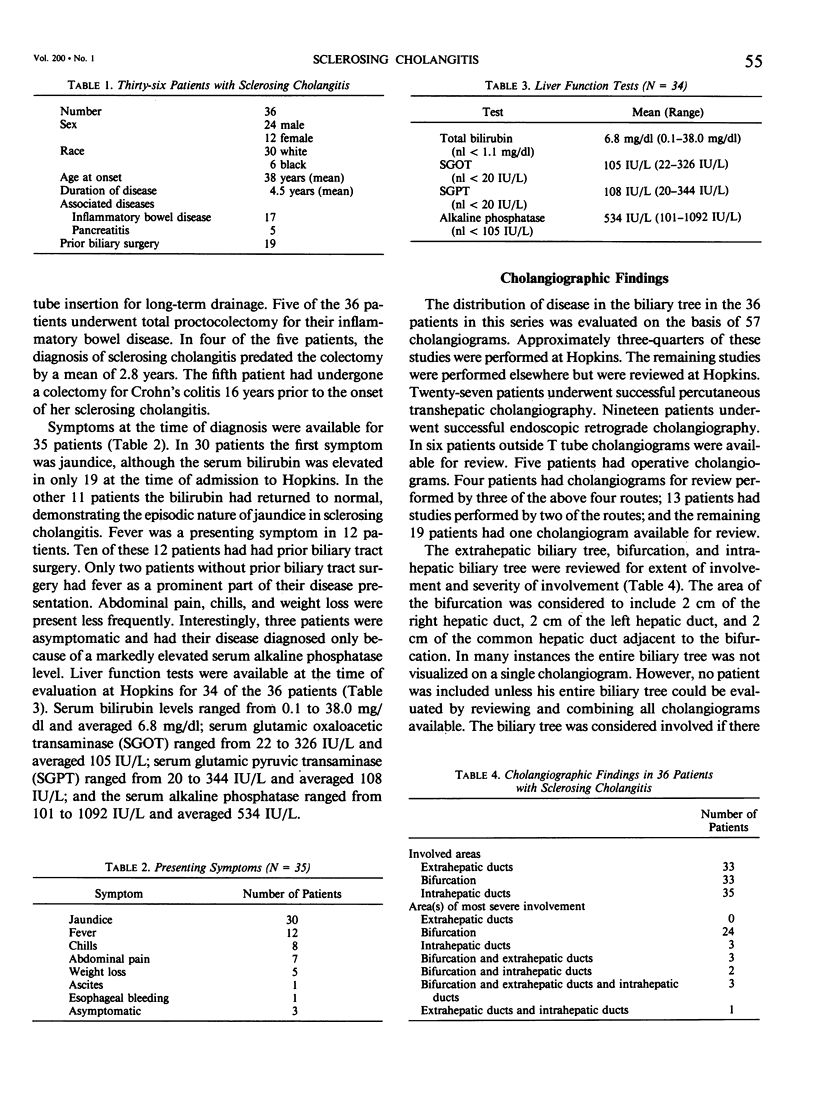
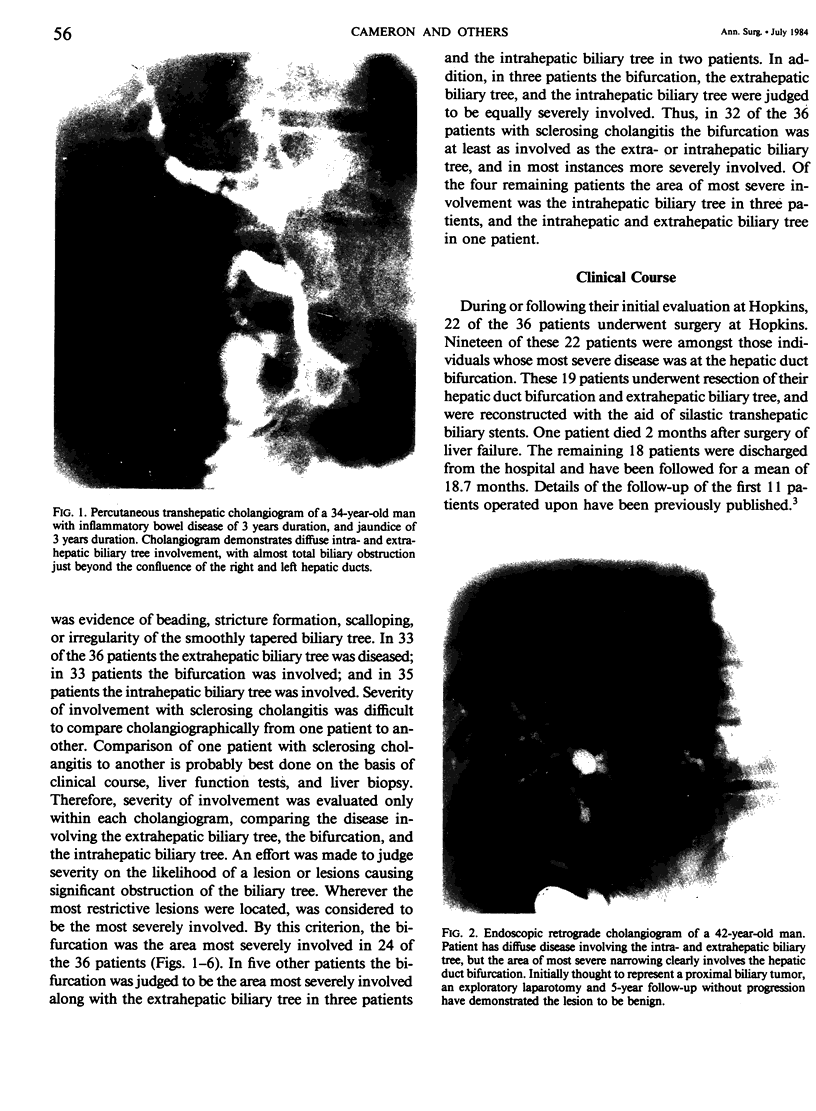
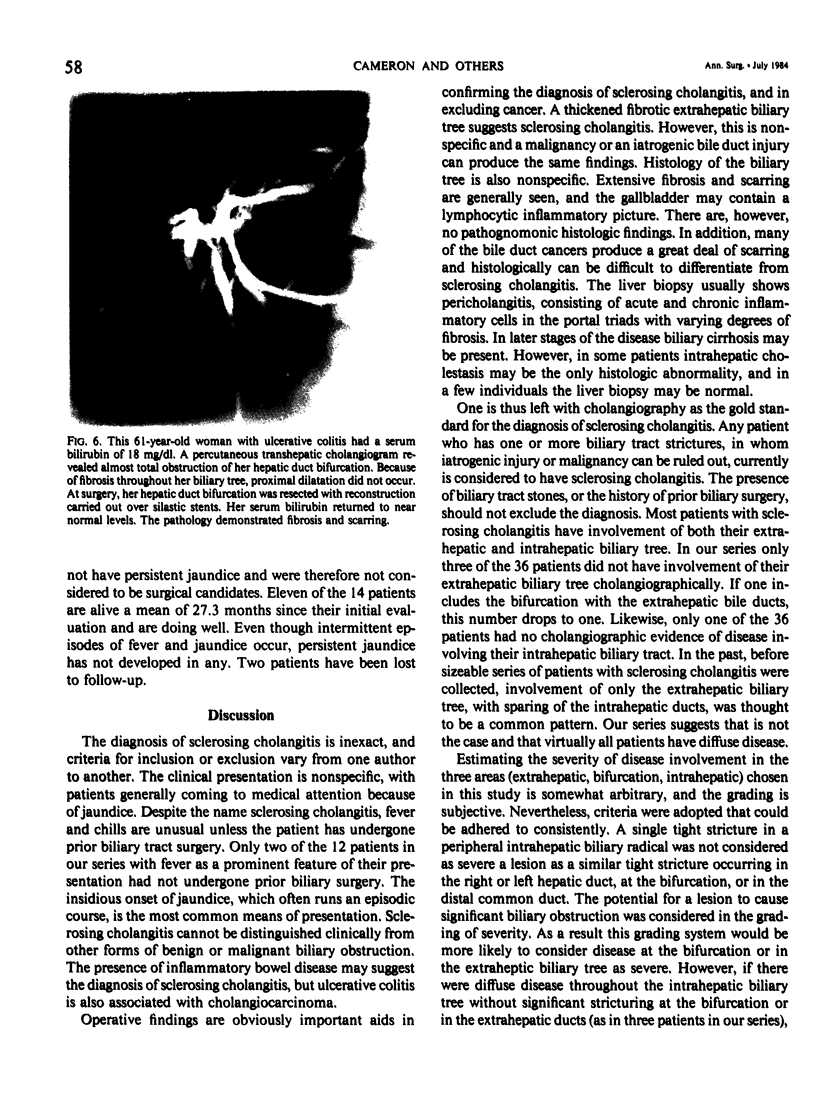
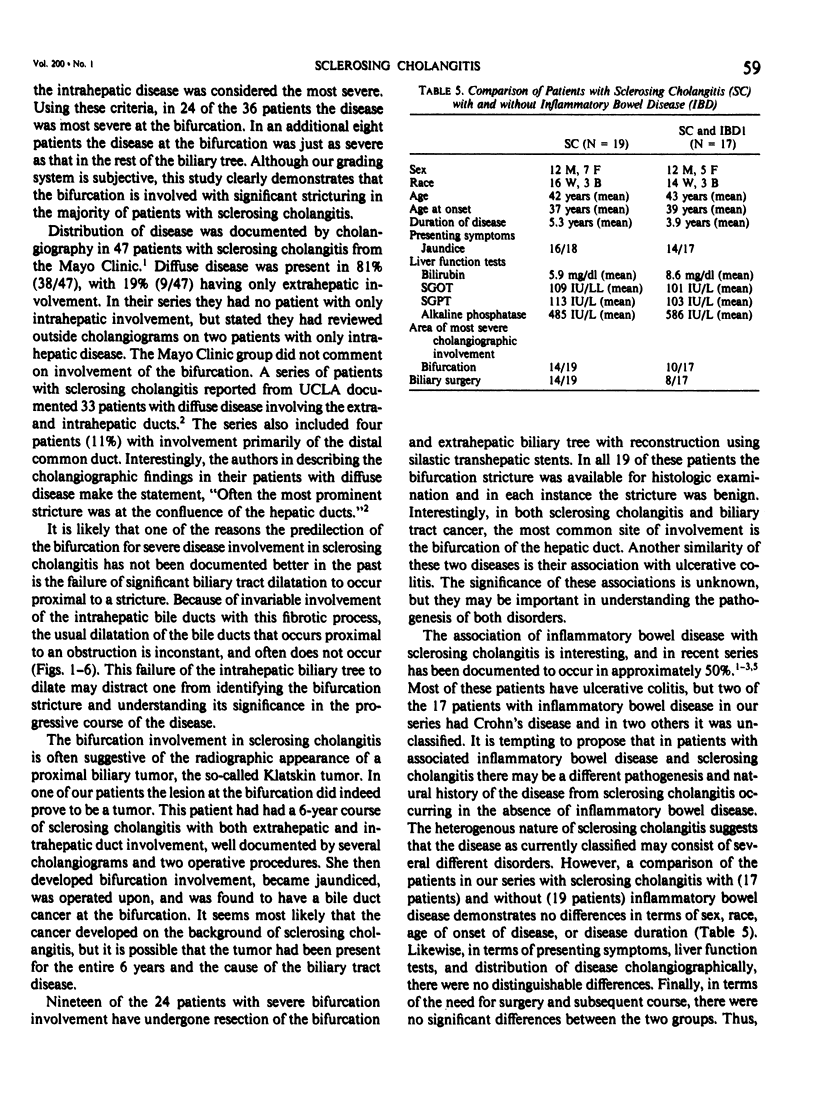
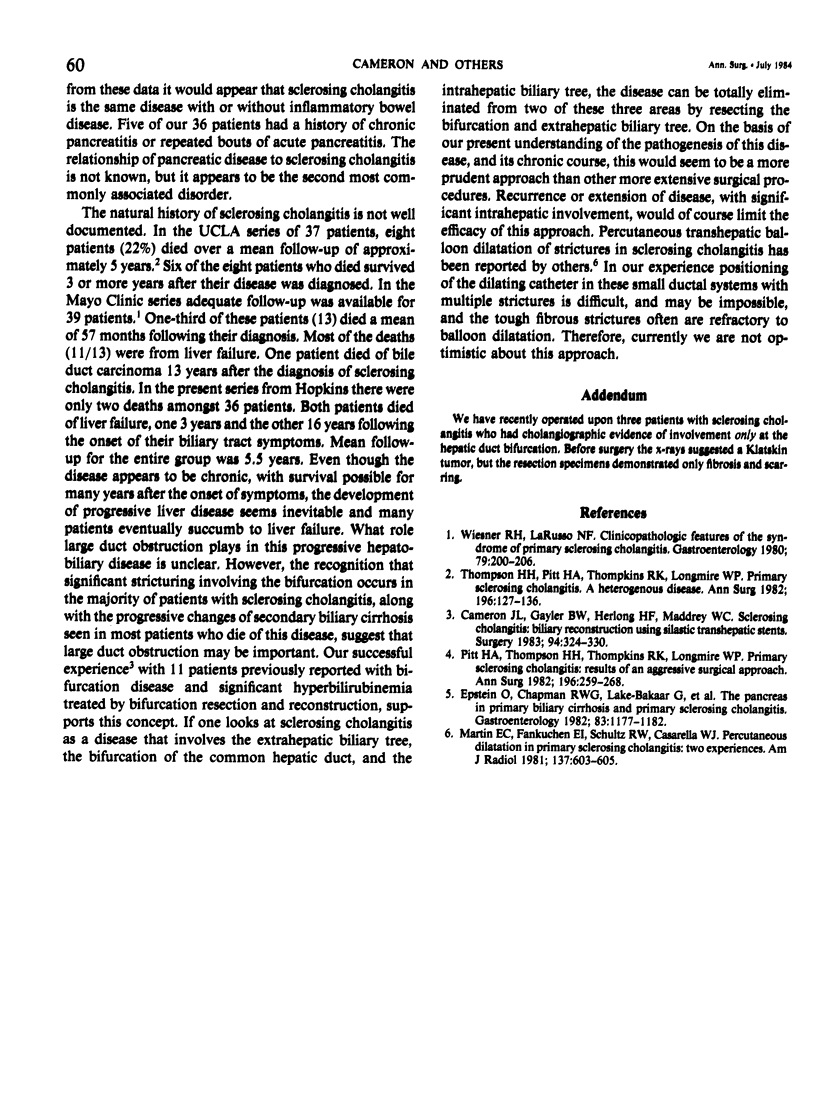
The cholangiograms of 36 patients with sclerosing cholangitis were reviewed. The mean age of the patient group was 43 years, and the mean disease duration was 4.5 years. Seventeen of the patients had associated inflammatory bowel disease. The mean serum bilirubin was 6.8 mg/dl, the mean SGOT was 105 IU/L, the mean SGPT was 108 IU/L, and the mean serum alkaline phosphatase was 534 IU/L. The cholangiograms demonstrated involvement of the extrahepatic bile ducts in 33 patients, involvement of the hepatic duct bifurcation in 33 patients, and involvement of the intrahepatic bile ducts in 35 patients. The cholangiograms were graded as to the areas of the most severe obstructive involvement. In 24 patients the area of most severe involvement was the hepatic duct bifurcation. In eight additional patients the hepatic duct bifurcation, along with the extrahepatic ducts and/or the intrahepatic ducts, were felt to be the areas most severely affected. This predilection for severe obstructive disease at the hepatic duct bifurcation in sclerosing cholangitis held for both patients with and without inflammatory bowel disease. Thus, most patients with sclerosing cholangitis have cholangiographic evidence of diffuse extrahepatic and intrahepatic biliary tract disease, with the hepatic duct bifurcation being the area generally most severely affected.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cameron J. L., Gayler B. W., Herlong H. F., Maddrey W. C. Sclerosing cholangitis: biliary reconstruction with Silastic transhepatic stents. Surgery. 1983 Aug;94(2):324–330. [PubMed] [Google Scholar]
- Epstein O., Chapman R. W., Lake-Bakaar G., Foo A. Y., Rosalki S. B., Sherlock S. The pancreas in primary biliary cirrhosis and primary sclerosing cholangitis. Gastroenterology. 1982 Dec;83(6):1177–1182. [PubMed] [Google Scholar]
- Martin E. C., Fankuchen E. I., Schultz R. W., Casarella W. J. Percutaneous dilatation in primary sclerosing cholangitis: two experiences. AJR Am J Roentgenol. 1981 Sep;137(3):603–605. doi: 10.2214/ajr.137.3.603. [DOI] [PubMed] [Google Scholar]
- Pitt H. A., Thompson H. H., Tompkins R. K., Longmire W. P., Jr Primary sclerosing cholangitis: results of an aggressive surgical approach. Ann Surg. 1982 Sep;196(3):259–268. doi: 10.1097/00000658-198209000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson H. H., Pitt H. A., Tompkins R. K., Longmire W. P., Jr Primary sclerosing cholangitis: a heterogenous disease. Ann Surg. 1982 Aug;196(2):127–136. doi: 10.1097/00000658-198208000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiesner R. H., LaRusso N. F. Clinicopathologic features of the syndrome of primary sclerosing cholangitis. Gastroenterology. 1980 Aug;79(2):200–206. [PubMed] [Google Scholar]