Structured Abstract
Objective:
To assess the distribution of National Institutes of Health (NIH)-funded surgeon-scientists by residency training institution and to examine whether training at institutions with higher NIH funding is associated with greater individual NIH funding.
Summary Background Data:
Surgeon-scientists face challenges securing NIH funding, with surgical research funding lagging behind other fields. Training in resource-rich environments may enhance research engagement and funding success.
Methods:
Blue Ridge Institute for Medical Research (BRIMR) rankings were used to identify NIH-funded principal investigators (NIH-PIs) among surgeons in Departments of Surgery from 2013–2023. Residency program NIH-funding quartiles, and top-ten programs, were determined by averaging institutional funding from BRIMR spreadsheets. Chi-square or Fisher’s exact tests, nonparametric tests, Z-tests, and linear regression were performed.
Results:
Among 559 NIH-funded surgeon-scientists, 394 (70.5%) trained at first-quartile institutions, representing 75–82% of NIH-PIs annually and receiving 79–85% of total funding each year. Total annual funding was significantly higher among first-quartile trained NIH-PIs ($117.9 vs. $24.8 million; p<0.0001), though median funding per NIH-PI did not differ ($354,544 vs. $328,179; p=0.358). In subgroup analysis, top-ten trained NIH-PIs had higher median funding per PI ($379,407 vs. $322,666; p=0.013) and experienced faster annual growth in funding per PI ($61,920/year vs. $38,666/year, p=0.009) even when adjusted for current affiliated institution funding quartile. Additionally, top-ten trained PIs exhibited greater scientific influence measured by the NIH iCite tool’s weighted relative citation ratio (119 vs. 100; p=0.034).
Conclusion:
Surgeon-scientists who trained at first-quartile institutions represent the majority of NIH-funded investigators, highlighting the potential influence of training in well-funded environments.
Keywords: Residency training, NIH funding, surgeon-scientists, Blue Ridge Institute for Medical Research
Introduction
Surgeons have historically made significant contributions to scientific discovery and the advancement of surgical practice and medicine.1 Research remains a cornerstone of academic surgery, and preserving this legacy depends on the engagement and development of new generations of surgeon-scientists. However, the existence of the surgeon-scientist role is increasingly challenged by clinical workloads, growing administrative responsibilities, and difficulties in securing extramural funding.2–4
Funding from the National Institutes of Health (NIH) is not only the most common funding source for scientific research but is also a well-recognized achievement for an individual’s professional career. Surgeon-scientists have traditionally submitted fewer grant applications and had lower success rates than their non-surgeon counterparts, which has been reflected by an increasing reliance on PhD principal investigators (PIs) in departments of surgery.5,6 Compounding this, NIH funding for surgeon-scientists decreased 27% from 2007 to 2014 compared to total NIH funding, and total NIH awards increased 79.2% compared to just 41.4% for surgical awards.3,5
With the increasing clinical demands and declining NIH funding for surgeon-scientists, it is critical to understand factors associated with funding success. Prior research has identified mentorship, research experience during training, research-focused degrees, and institutional support as important predictors of success.2–4,7,8 A roadmap for the aspiring surgeon-scientist emphasizes training experiences and institutional support as key contributors to sustained research productivity.4 Given the critical role of training in shaping future surgeon-scientists, institutions with higher NIH funding may offer a more robust environment with enhanced infrastructure for mentorship, resources, and research development, ultimately supporting greater success in securing funding.
To our knowledge, no previous studies have examined the relationship between surgeon-scientists’ residency training institutions and their representation among NIH-funded investigators. Motivated by the need to identify ways to support and to sustain the surgeon-scientist pipeline, we sought to understand whether NIH-funded surgeon-scientists disproportionately trained at institutions with higher levels of NIH funding. We hypothesized that surgeon-scientists who trained at residency programs in the highest quartile of NIH funding would constitute the majority of NIH-funded surgeon-scientists and would receive greater overall funding.
Methods
Database Creation
The Blue Ridge Institute for Medical Research (BRIMR) publishes annual rankings of institutions, departments, and PIs based on NIH funding. Principal investigators were identified from BRIMR’s “Department of Surgery” PI spreadsheets for the years 2013–2023. Surgeon-scientists were defined as NIH-funded physicians with a medical degree (MD, DO, or MBBS) practicing within a general surgery subspecialty, regardless of research type. Degree and specialty data were collected from institutional webpages. Individuals without a medical degree or whose specialty was in medicine or non-general surgery subspecialties, including orthopedics, otolaryngology, neurosurgery, and obstetrics and gynecology, were excluded. For those meeting the inclusion criteria, additional demographic and professional data including sex, international medical graduate (IMG) status, and residency training program were gathered from institutional and departmental webpages. When information was unavailable from these sources, publicly accessible platforms such as LinkedIn, Doximity, and ResearchGate were used. As all data were obtained from publicly available sources, this study was exempt from Institutional Review Board (IRB) approval.
Marker of Scientific Influence
The NIH iCite tool was used to obtain the weighted relative citation ratio (RCR) from 2013 to 2023 for each PI. The RCR is a citation-based metric that measures the scientific influence of a publication, calculated as citations per year normalized to NIH-funded papers in the same field.9,10 The weighted RCR, defined as the sum of all RCRs for a given PI, was used as an indicator of scientific productivity and impact.
Grant Data
NIH RePORTER (Research Portfolio Online Reporting Tools Expenditures and Results) was searched for each PI to obtain grant funding information. Only PIs who received at least one K-series, R-series, P-series, U-series, or T-series award during the study period were included in the analysis. When analyzed, R01 and K08 awards were evaluated separately from other R awards (including R03, R21, R23, R25, R33, R34) and other K awards (including K07, K23, K24), respectively. The total number of each award type per year was recorded for each PI.
Calculating Residency NIH Funding Quartile
The BRIMR “Schools of Medicine” and “Hospitals” spreadsheets were queried from years 2013–2023. Institutional NIH funding was averaged over this period to generate a composite NIH funding list. BRIMR methodology notes that the NIH sometimes credits grants to affiliated teaching hospitals rather than to their parent medical schools, which can understate the funding and rankings of those schools.11 This limitation applies to BRIMR’s “Department of Surgery” rankings, which can also underrepresent schools of medicine with multiple affiliated hospitals. For example, Harvard Medical School is listed on the BRIMR “Schools of Medicine” spreadsheet, whereas its affiliated hospitals, including Brigham & Women’s Hospital, Massachusetts General Hospital, and Beth Israel Deaconess Medical Center, are not independently included. To address this, Harvard was removed from the list, and the institutional funding for these hospitals was extracted separately from the “Hospitals” spreadsheets. Institution-level funding rather than Department of Surgery funding was used, particularly given the noted limitations and because surgical residents often benefit from institution-wide resources and may collaborate across departments or receive support from NIH grants awarded outside their home department. Institutions were ranked and grouped into quartiles based on their average NIH funding levels over the designated time period, and the top ten institutions were separately designated for subgroup analyses. If a PI’s residency program was not listed in BRIMR, their quartile classification was marked as “Not Applicable,” and they were excluded from quartile-based comparative analyses.
Statistical Analysis
PIs who trained at first-quartile residency programs or at top ten institutions were compared to those from all other quartiles (second, third, and fourth) using standard univariate statistical methods. Categorical variables were analyzed using chi-square tests or Fisher’s exact tests, as appropriate, and continuous variables were compared using the Mann-Whitney U test. The proportion of PIs, total funding, and grant type distributions between groups were compared using two-proportion Z-tests. Linear regression or mixed-effects linear regression were used, as appropriate, to assess differences in the rate of increase in total funding per group per year and changes in average funding per PI per year. All statistical analyses were conducted using R Studio (version 4.4.1). Two-tailed tests were performed, with p <0.05 considered statistically significant.
Results
A total of 559 NIH-funded surgeon-scientists in Departments of Surgery from 2013 to 2023 were identified, collectively holding 983 awards. Among them, 421 (75.3%) were male, while only 138 (24.7%) were female. Most PIs did not hold an advanced degree beyond their medical degree, though 104 (18.6%) had PhDs, 113 (20.2%) had Master’s degrees, and 9 (1.6%) held both a PhD and a Master’s. The most common surgical specialties among funded PIs were cardiothoracic surgery (18.8%) and surgical oncology (16.8%). Of all grants awarded, 392 (39.9%) were R01 awards, while 114 (11.6%) were K08 awards. Additional cohort characteristics are detailed in Table 1.
Table 1:
Summary of representation in the BRIMR rankings of unique surgeon-scientists from 2013 to 2023.
| Representation in Blue Ridge Rankings | |
|---|---|
| Residency Training NIH Funding Quartile | |
| First | 394 (70.5%) |
| Second | 91 (16.3%) |
| Third | 27 (4.8%) |
| Fourth | 6 (1.1%) |
| Not on BRIMR Institution Sheets | 41 (7.3%) |
| Gender | |
| Male | 421 (75.3%) |
| Female | 138 (24.7%) |
| Graduate Degree(s) | |
| PhD | 104 (18.6%) |
| Master’s | 113 (20.2%) |
| PhD/Master’s | 9 (1.6%) |
| None | 333 (59.6%) |
| IMG | |
| Yes | 57 (10.2%) |
| No | 502 (89.8%) |
| Specialty | |
| Bariatric | 1 (0.2%) |
| Breast | 12 (2.1%) |
| Cardiothoracic | 105 (18.8%) |
| Colorectal | 17 (3.0%) |
| Endocrine | 16 (2.9%) |
| General | 22 (3.9%) |
| Pediatric Surgery | 43 (7.7%) |
| Plastics | 35 (6.3%) |
| Surgical Oncology | 94 (16.8%) |
| Transplant | 74 (13.2%) |
| Trauma/Acute Care/Critical Care/Bum | 77 (13.8%) |
| Vascular | 63 (11.3%) |
| Multiple Grants | |
| Yes | 227 (40.6%) |
| No | 332 (59.4%) |
| Grant Types | |
| R01 Awards | 392 (39.9%) |
| Other R Awards | 203 (20.7%) |
| K08 Awards | 114 (11.6%) |
| Other K Awards | 57 (5.8%) |
| P Awards | 25 (2.5%) |
| U Awards | 102 (10.4%) |
| T Awards | 90 (9.1%) |
Abbreviations: Blue Ridge Institute for Medical Research (BRIMR), National Institutes of Health (NIH), International Medical Graduate (IMG)
First Quartile NIH-Funded Institution Trained PIs versus All Others
Of the 559 surgeon-scientists, 394 (76.1%) trained at one of the 38 residency programs in the first quartile of NIH funding (first quartile trained PIs), while 124 (23.9%) trained at institutions in the second, third, or fourth quartile (all other quartile trained PIs). The distribution of sex was similar between groups (Table 2), with males comprising 288 (73.1%) of first quartile trained PIs and 100 (80.6%) of all other quartile-trained PIs (p=0.116). The proportion of PIs holding additional degrees was also comparable (p=0.454). However, all other quartile trained PIs were significantly more likely to be IMGs compared to first quartile trained PIs (18.5% vs. 5.1%, p<0.0001). First quartile trained PIs showed a trend towards greater scientific influence, with a median weighted RCR of 109 vs. 94.4 (p=0.118). In terms of total annual funding, first quartile trained PIs received significantly more total funding than all other quartile trained PIs, with a median of $117.9M (IQR $44.0M) vs. $24.8M (IQR $12.2M; p<0.0001). However, there was no significant difference in average funding per PI per year ($354,555 vs. $328,179; p=0.358). On linear regression, the first quartile trained PI group experienced a significantly greater rate of increase in total funding per year, receiving $6.26 million more annually compared to all other quartile trained PIs ($8.8M/year vs. $2.5M/year; p<0.001; Figure 1A). In a mixed-effects linear regression adjusting for year, current institutional affiliation, whether the PI remained at their training institution, and PI characteristics, the rate of increase in funding did not differ between first quartile trained and other quartile trained PIs ($49,217/year vs. $46,779/year, p=0.816; Figure 1B). Current affiliation with a first quartile funded institution was also not associated with higher annual funding per PI (p=0.437). Unsurprisingly, holding multiple NIH grants was most strongly associated with greater annual funding (p<0.001). Sex was also significantly associated with NIH funding, with male PIs receiving an average of $148,500 more in annual funding compared to female PIs (p=0.048). Other factors such as specialty, IMG status, graduate degree, and remaining at the same institution where one trained were not independently associated with annual NIH funding per PI (p>0.05 for all). Although PIs trained at first quartile programs received greater aggregate NIH funding, they did not hold a disproportionately greater share of total funding relative to their representation among funded PIs in most years. However, this difference reached statistical significance in 2016 (p=0.021) and 2017 (p=0.043); Figure 2A). They also did not receive a disproportionate number of R01s (p=0.896), K08s (p=0.275), other K awards (p=0.980), P awards (p=0.179), U awards (p=0.735), or T awards (p=0.909). However, they were awarded a significantly greater proportion of other R-series awards than would be expected based on their representation among funded PIs (p=0.012; Figure 2B).
Table 2.
Demographic and grant characteristics of unique principal investigators who trained at residency programs in the first quartile of NIH funding compared to those who trained at a residency program in any other quartile of NIH funding, excluding those not listed on the BRIMR sheets.
| First Quartile-Trained PIs (n=394) | All Other Quartile-Trained PIs (n=124) | P-value | |
|---|---|---|---|
| Gender | 0.116 | ||
| Male | 288 (73.1%) | 100 (80.6%) | |
| Female | 106 (26.9%) | 24 (19.4%) | |
| Graduate Degree(s) | 0.454 | ||
| PhD | 80 (20.3%) | 20 (16.1%) | |
| Master’s | 76 (19.3%) | 19 (15.3%) | |
| PhD/Master’s | 6 (1.5%) | 2 (1.6%) | |
| None | 232 (58.9%) | 83 (66.9%) | |
| IMG | <0.0001 | ||
| Yes | 20 (5.1%) | 23 (18.5%) | |
| No | 374 (94.9%) | 101 (81.5%) | |
| Remained at the Same Institution | <0.001 | ||
| Yes | 118 (29.9%) | 17 (13.7%) | |
| No | 276 (70.1%) | 107 (86.3%) | |
| Specialty | <0.001 | ||
| Bariatric | 0 (0.0%) | 1 (0.8%) | |
| Breast | 8 (2.0%) | 4 (3.2%) | |
| Cardiothoracic | 85 (21.6%) | 10 (8.1%) | |
| Colorectal | 12 (3.0%) | 4 (3.2%) | |
| Endocrine | 11 (2.7%) | 4 (3.2%) | |
| General | 14 (3.5%) | 5 (4.0%) | |
| Pediatric Surgery | 29 (7.4%) | 12 (9.7%) | |
| Plastics | 27 (6.9%) | 5 (4.0%) | |
| Surgical Oncology | 67 (17.0%) | 25 (20.2%) | |
| Transplant | 57 (14.5%) | 8 (6.5%) | |
| Trauma/Acute Care/Critical Care/Bum | 42 (10.7%) | 28 (22.6%) | |
| Vascular | 42 (10.7%) | 18 (14.5%) | |
| Weighted RCR | 109 [49.3 – 238.8] | 94.4 [37.9 – 219.7] | 0.118 |
| Average Funding Per PI/Year | $354,555 [$194,826 – $627,210] | $328,179 [$199,484 – $527,576] | 0.358 |
| Total Funding Per Year * | $117.9 [$99.7 – $143.7] | $24.8 [$20.0 – $32.2] | <0.0001 |
| Multiple Grants | 0.588 | ||
| Yes | 54 (13.7%) | 14 (11.3%) | |
| No | 340 (86.3%) | 110 (88.7%) |
Abbreviations: National Institutes of Health (NIH), Principal Investigators (PIs), International Medical Graduate (IMG), Relative Citation Ratio (RCR)
in millions
Figure 1.
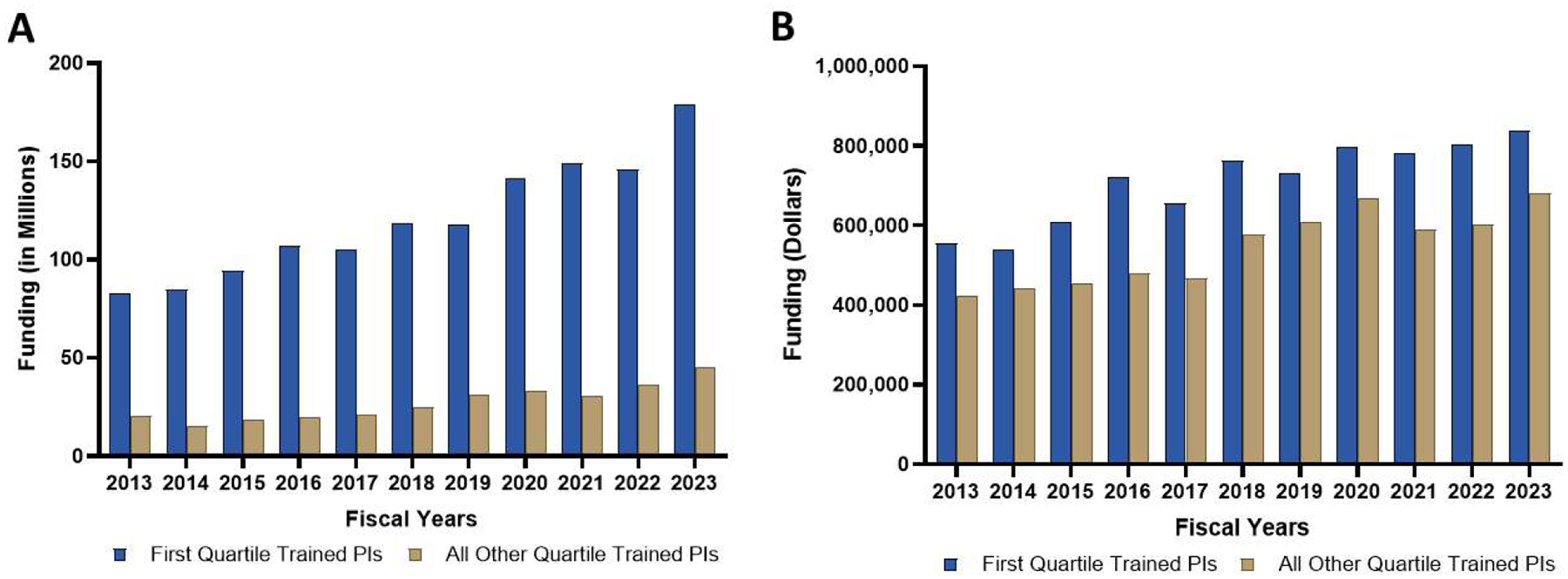
(A) Annual trend in total NIH funding for PIs trained at NIH funded institutions in the first quartile compared to those trained in all other quartiles. (B) Yearly trend in average funding per PI, comparing PIs from first quartile NIH funded institutions to those from all other quartiles.
Figure 2.
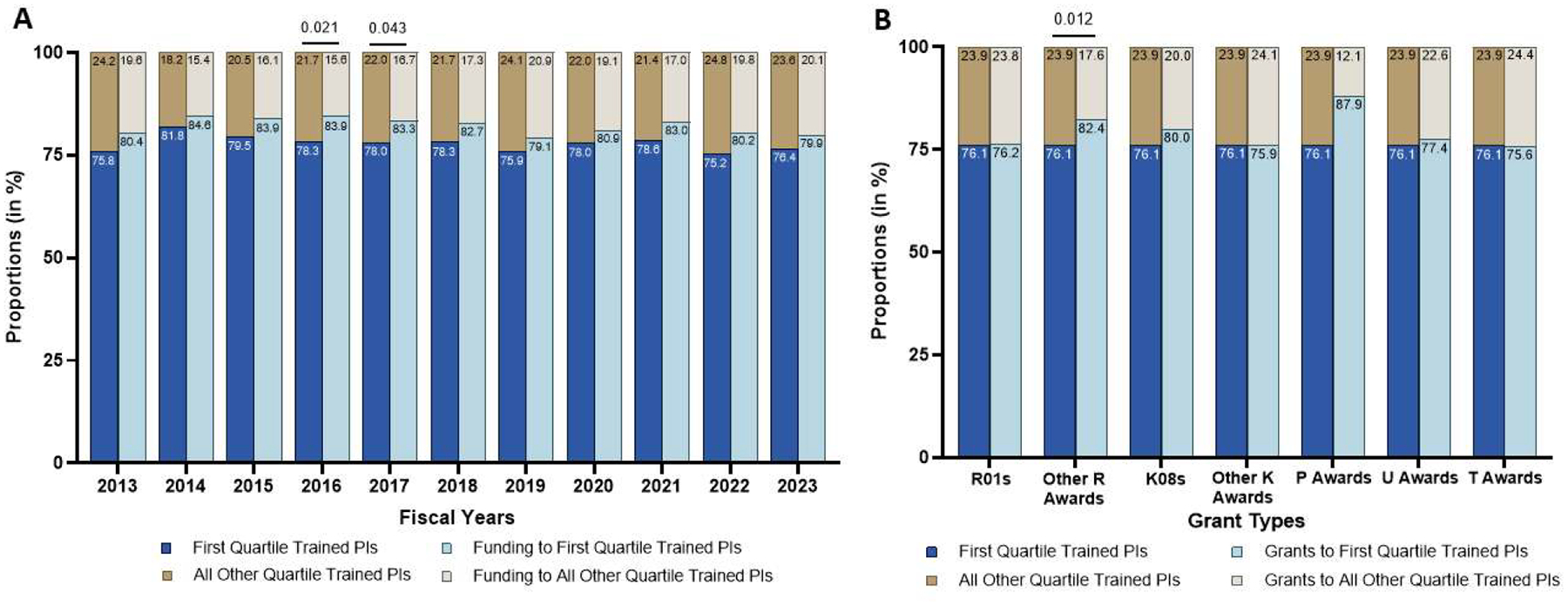
(A) Proportion of NIH funded PIs by quartile of residency training funding (first quartile versus all other quartiles) relative to proportion of funding received. (B) Proportion of NIH funded PIs relative to distribution of award type.
Top Ten NIH-Funded Institution Trained PIs versus All Others
A subgroup analysis comparing PIs who trained at institutions in the top ten of NIH funding (top ten trained PIs) to all other PIs was performed. There were 200 (38.6%) top ten trained PIs and 318 (61.4%) PIs in the all other quartile group (Table 3). The sex distribution remained similar between groups, with 146 (73.0%) of top ten trained PIs and 242 (76.1%) of all other trained PIs being male (p=0.491). The proportion of IMGs was again significantly higher in the all other quartile trained group (10.7% vs. 4.5%, p=0.020). Top ten trained PIs exhibited significantly greater scientific influence as measured by the weighted RCR (119 vs. 100, p=0.034).
Table 3.
Demographic and grant characteristics of unique principal investigators who trained at residency programs in the top ten of NIH funding compared to those who trained at a residency program in the rest of the first quartile and all other quartiles of NIH funding, excluding those not listed on the BRIMR sheets.
| Top Ten-Trained PIs (n=200) | All Other Quartile-Trained PIs (n=318) | P-value | |
|---|---|---|---|
| Gender | 0.491 | ||
| Male | 146 (73.0%) | 242 (76.1%) | |
| Female | 54 (27.0%) | 76 (23.9%) | |
| Graduate Degree(s) | 0.158 | ||
| PhD | 41 (20.5%) | 59 (18.6%) | |
| Master’s | 38 (19.0%) | 57 (17.9%) | |
| PhD/Master’s | 6 (3.0%) | 2 (0.6%) | |
| None | 115 (57.5%) | 200 (62.9%) | |
| IMG | 0.020 | ||
| Yes | 9 (4.5%) | 34 (10.7%) | |
| No | 191 (95.5%) | 284 (89.3%) | |
| Remained at the Same Institution | 0.129 | ||
| Yes | 60 (30.0%) | 75 (23.6%) | |
| No | 140 (70.0%) | 243 (76.4%) | |
| Specialty | |||
| Bariatric | 0 (0.0%) | 1 (0.3%) | |
| Breast | 3 (1.5%) | 9 (2.8%) | |
| Cardiothoracic | 54 (27.0%) | 41 (12.9%) | |
| Colorectal | 7 (3.5%) | 9 (2.8%) | |
| Endocrine | 8 (4.0%) | 7 (2.2%) | |
| General | 8 (4.0%) | 11 (3.5%) | |
| Pediatric Surgery | 16 (8.0%) | 25 (7.9%) | |
| Plastics | 9 (4.5%) | 23 (7.2%) | |
| Surgical Oncology | 35 (17.5%) | 57 (17.9%) | |
| Transplant | 28 (14.0%) | 37 (11.6%) | |
| Trauma/Acute Care/Critical Care/Bum | 16 (8.0%) | 54 (17.0%) | |
| Vascular | 16 (8.0%) | 44 (13.8%) | |
| Weighted RCR | 119 [60.0 – 250] | 100 [41.6 – 223] | 0.034 |
| Average Funding Per PI/Year | $379,407 [$222,964 – 659,574] | $322,666 [$191,148 – $568,228] | 0.013 |
| Total Funding Per Year * | $62.9 [$49.6 – $84.0] | $84.2 [$64.6 – $91.1] | 0.076 |
| Multiple Grants | 0.840 | ||
| Yes | 25 (12.5%) | 43 (13.5%) | |
| No | 175 (87.5%) | 275 (86.5%) |
Abbreviations: National Institutes of Health (NIH), Principal Investigators (PIs), International Medical Graduate (IMG), Relative Citation Ratio (RCR)
in millions
In contrast to the first quartile analysis, total annual funding trended lower for the top ten group compared to all other quartiles ($62.9M vs. $84.2M; p=0.076), reflecting the smaller size of the top ten group. However, top ten trained PIs received significantly greater funding per PI per year on average ($379,407 vs. $322,666; p=0.013). On linear regression, increase in total funding per year trended higher among the top ten trained PI group, with an annual increase of $247,216 more than the all other trained PI group ($5.9M/year vs. $5.5M/year; p=0.700; Figure 3A). In an adjusted linear mixed-effects model, surgeon-scientists trained at top ten NIH-funded residency programs experienced a significantly greater annual increase in funding per PI per year compared to their peers from non–top ten programs ($61,920/year vs. $38,666/year; p=0.009; Figure 3B). Notably, current affiliation with a top ten institution was not significantly associated with funding increase (p=0.277). Holding multiple NIH grants was again associated with greater annual funding (p<0.001), and male PIs received significantly more funding than female PIs (p=0.046). Remaining at the same institution where training occurred was not independently associated with funding (p=0.377). Top ten trained PIs received a disproportionately greater share of total funding in 2016 (p=0.031), 2020 (p=0.038), 2021 (p=0.015), 2022 (p=0.035), and 2023 (p=0.012) relative to their representation among funded PIs (Figure 4A). While the distribution of most grant types did not differ significantly (p>0.05), R01 grants were disproportionately awarded to top ten trained PIs (p=0.009); Figure 4B).
Figure 3.

(A) Annual trend in total NIH funding for PIs trained at top ten NIH funded institutions compared to those trained in all other quartiles. (B) Yearly trend in average funding per PI, comparing PIs from top ten NIH funded institutions to those from all other quartiles.
Figure 4.

(A) Proportion of NIH funded PIs by quartile of residency training funding (top ten versus all other quartiles) relative to proportion of funding received. (B) Proportion of NIH funded PIs relative to distribution of award type.
Isolating Training Environment and Current Affiliated Environment
Of the 200 top ten trained PIs, 98 (49%) are no longer affiliated with a top ten funded institution. Among surgeon-scientists no longer affiliated with top ten funded institutions, those who trained at a top ten funded institution received significantly higher average annual R01 funding than those who were not trained at a top ten funded program ($544,030 vs. $469,482; p=0.039). While this may reflect a lasting advantage from training in resource-rich settings, these differences should be interpreted in the context of the heterogeneity across institutional environments outside of the top ten. Of all top ten trained PIs, there was not a significant difference in average annual R01 funding between those who remained at top ten funded institutions and those who have transitioned to other institutions ($629,510 vs. $544,030; p=0.775). There was a trend toward higher R01 funding among surgeon-scientists who trained at a top ten funded institution but are no longer affiliated with one compared to those who did not train at a top ten program but are currently at a top ten funded institution ($544,030 vs. $510,521; p= 0.169). These findings suggest that training at a top ten-funded institution confers a sustained advantage in R01 funding, while also highlighting that transitioning to one may also provide meaningful benefits.
Discussion
The NIH is the leading funder of health-related research in the United States.12 Over the past decade, surgeon-scientists have experienced significantly lower grant success rates compared to the overall NIH applicant pool (16.4% vs 19.2%), underscoring both a highly competitive funding landscape and notable disparities for surgeons.13 Despite some encouraging trends14,15, there are ongoing obstacles for surgeon-scientists, making it critical to identify strategies to strengthen the surgeon-scientist pipeline and improve funding success. Residency, particularly structured research experiences, is essential for developing future surgeon-scientists.8 Institutional research environment, one factor in NIH funding evaluation, highlights the importance of resources and infrastructure in supporting investigators.16 In this context, we evaluated whether NIH-funded surgeon-scientists disproportionately trained at residency programs affiliated with institutions receiving higher NIH funding. We found that the majority of NIH-funded surgeon-scientists (75–82% annually) trained at first quartile NIH-funded programs and collectively secured 79–85% of total NIH funding awarded to surgeon-scientists each year. These findings suggest a strong concentration of NIH-funded investigators emerging from resource-rich training environments.
Our findings complement prior work showing that 51.5% of new NIH awards from 2008–2018 were concentrated among the top 14 institutions.17 Mesquita-Neto et al. observed comparable median grant amounts across institutions, aligning with our finding that funding per PI did not significantly differ between surgeon-scientists trained at first quartile NIH-funded residency programs and those trained elsewhere.17 Interestingly, however, we found significantly higher funding per PI among those trained at top ten NIH-funded residency programs compared to their peers. While Mesquita-Neto et al. focused on institutions where surgeon-scientists are currently employed, our study uniquely investigated their residency training backgrounds. We found that first quartile trained surgeon-scientists experienced significantly greater annual growth in total funding compared to peers from lower-funded institutions. Subgroup analysis highlighted more pronounced disparities with PIs trained at top ten institutions holding disproportionately greater shares of total funding in recent years (2016, 2020–2023), higher average funding per investigator, and a greater rate of annual increase in funding per PI. One potential explanation for this distinction is the increasing reliance on multiple PI grants – often R-series awards – which rose to 35.4% by 2020 and are more commonly awarded to well-resourced institutions.18 In our study, top ten trained PIs held a significantly greater proportion of R01 awards. Although not all remained at top ten institutions, their training may have provided enhanced preparation for independent research careers and the ability to build collaborative networks. These findings suggest a convergence of NIH resources toward PIs who trained at institutions with the highest levels of funding, even after accounting for current institutional affiliation. For example, PIs who trained at top ten institutions received significantly higher average R0l funding than those without top ten training, even when both groups were currently based at similarly resourced institutions.
In light of increasing clinical demands and a competitive NIH funding landscape, departments of surgery have increasingly relied on PhD PIs, leading to a 2.8-fold funding gap between surgeon-scientists and PhD PIs despite an overall increase in surgical departmental funding.18 While the value of advanced research-oriented degrees for surgeon-scientists remains debated, some studies have found MD/PhD graduates are significantly more likely to obtain NIH funding compared to MD-only graduates8 or MD/Master’s individuals,2 whereas one survey suggests such degrees are not essential for academic success.7 Such degrees may offer critical skills in research methodology and grantsmanship that are not routinely emphasized during medical school, thereby supporting a successful career as an independent investigator. Mesquita-Neto et al. found a greater prevalence of MD/PhD investigators at the top 14 institutions compared to others.19 Interestingly, our analysis did not detect significant differences in advanced degree attainment between first quartile-trained surgeon-scientists and their counterparts, indicating that opportunities for pursuing such degrees may be broadly accessible regardless of training program. Maintaining these educational opportunities remains important for those interested in research-intensive careers.
Mentorship is an important component in the development and long-term success of surgeon-scientists.2–4,17,20,21 The American Surgical Association Research Sustainability Task Force emphasizes the importance of mentor-mentee relationships, regular meetings, and accountability to foster successful surgeon-scientists.22 Mentorship has also been shown to significantly enhance research productivity and satisfaction. A nationwide survey by Marincola et al. found that having a formal research mentor was associated with more grant applications and higher satisfaction in research.2 While most studies focus on current PIs, Barker et al. emphasized the importance of building a team of mentors during dedicated research periods.23 Experienced mentors with established research funding can help mentees acquire essential skills, navigate early career challenges, and provide support during the transition from residency to fellowship and eventual independence. In our study, remaining at the same institution where one trained, potentially retaining access to previous mentors, was not associated with differences in funding amount. However, without data on unfunded applicants, we cannot determine the effect of institutional continuity on funding success. Nonetheless, mentorship remains a key factor in research career development, and institutions with higher NIH funding may offer more structured mentorship programs and access to experienced, well-funded faculty, potentially better preparing trainees for future success.
Training has consistently been identified as a pivotal phase in shaping the future success of surgeon-scientists as noted in the roadmap presented by the Society of University Surgeons.4 Dedicated research experiences during residency are associated with increased pursuit of academic careers, higher publication output, more grant submissions, and greater extramural funding.20,24–26 However, research opportunities and experiences vary between programs and among different trainee groups. Although IMGs contribute meaningfully to academic productivity, they have historically faced disparities in NIH funding27 and were significantly underrepresented among first quartile and top ten trained surgeon-scientists in our study, potentially contributing to funding inequities. First quartile trained PIs showed trends toward higher weighted RCRs, while those who trained at top ten institutions had significantly higher weighted RCRs, consistent with previous findings linking top-funded institutions to greater scientific impact.17 Recent efforts by groups such as the Blue Ribbon Committee II have sought to reform training paradigms by promoting standardized, competency-based research engagement across programs.28,29 Recommendations include defining a surgeon-scientist track and equipping trainees with core skills. Fundamental skills integral to building a foundation for future academic success have been suggested to include laboratory techniques, grant and manuscript writing, oral presentation skills, budgeting, and team management.4,22,28–30 Higher funded institutions may place greater importance on research and be better equipped to provide these fundamental skills and offer mechanisms to financially support trainees through research, addressing a previously recognized barrier.24 In support of this, surgeon-scientists trained at first quartile programs held more T awards than those from other quartiles. Although individual access to T32 programs during training is unclear, highly funded institutions are likely better positioned to offer structured support and greater access to such mechanisms. Moreover, institutions may offer T32 awards outside of the department of surgery, making it difficult to capture the full extent of support available to trainees.31 Together, these findings underscore that resource-rich training environments likely provide more opportunities for financial support of trainees, ultimately facilitating long-term success as surgeon-scientists.
We have demonstrated NIH-funded surgeon-scientists are disproportionately trained at institutions with the highest levels of NIH funding, suggesting that the training environment plays a meaningful role in shaping future funding success. While direct causality cannot be established without applicant-level data, the consistent representation and greater funding among first quartile and top ten trained PIs imply that these environments may provide key advantages such as stronger mentorship, structured research training, and institutional resources that support the development and sustainability of surgeon-scientist careers. As we look for ways to enhance the surgeon-scientist pipeline, it may be beneficial to examine the specific practices and resources of these highly funded programs and consider integrating their most effective elements into standardized training paradigms. While this study provides an initial framework, future work incorporating qualitative data, such as surveys of NIH-funded surgeon-scientists, could clarify which resources and mentorship structures during their training contributed most to their success, helping identify elements that should be integrated into programs to strengthen the surgeon-scientist pipeline. Our study has several limitations. It includes only surgeon-scientists funded through departments of surgery, potentially excluding those funded through other departments. Additionally, the analysis is limited to PIs with funded grants, as data on unfunded grant applications are not publicly available which limits our ability to determine whether training at a first quartile NIH-funded residency program increases the likelihood of securing NIH funding. The focus on NIH grants also does not account for internal funding, societal grants, or other extramural funding sources such as Department of Veteran Affairs or Department of Defense awards. PI demographics were obtained from institutional webpages which depend on the accuracy and completeness of publicly available information. While data collection was based on the most current records at the time of review, details may change over time.
Conclusions
Surgeon-scientists who trained at first quartile institutions represent the majority of NIH-funded investigators, and those trained in the top ten of NIH-funded institutions have greater funding per PI, even when no longer affiliated with a top ten institution, highlighting the influence of training in well-funded environments. This raises important considerations for equity and sustainability within the surgeon-scientist workforce and suggests efforts to expand access to robust research environments during training could play a key role in broadening future funding success. The direct impact of training location on NIH funding success remains uncertain, however, without applicant-level data which should be assessed in future studies.
Acknowledgements
We would like to acknowledge that Dr. Russell Witt is supported by the National Cancer Institute (NCI) Early Surgeon Scientist Program (CCSG P30CA044579-32). He is also an iTHRIV Scholar which is supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR003015 and KL2TR003016). Dr. Mackenzie Mayhew also received support from the NCI T32 training grant (CA163177). The funding sources had no role in the study design, data collection, analysis, manuscript preparation, or publication decision.
Footnotes
Disclosures: The authors have no disclosures or conflicts of interest.
References
- 1.Toledo-Pereyra LH. Nobel Laureate surgeons. J Invest Surg. 2006;19(4):211–218. [DOI] [PubMed] [Google Scholar]
- 2.Marincola Smith P, Martinez A, Irlmeier R, et al. Factors impacting academic productivity and satisfaction of surgeon-scientists: A nationwide survey: A nationwide survey. Ann Surg. 2025;281(3):445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keswani SG, Moles CM, Morowitz M, et al. The future of basic science in Academic Surgery: Identifying barriers to success for surgeon-scientists. Ann Surg. 2017;265(6):1053–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldstein AM, Blair AB, Keswani SG, et al. A roadmap for aspiring surgeon-scientists in today’s healthcare environment. Ann Surg. 2019;269(1):66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mann M, Tendulkar A, Birger N, Howard C, Ratcliffe MB. National institutes of health funding for surgical research. Ann Surg. 2008;247(2):217–221. [DOI] [PubMed] [Google Scholar]
- 6.Hu Y, Edwards BL, Hu K, Brooks KD, Slingluff CL Jr. Surgery investigators funded through the National Institutes of Health: A rebirth. Surgery. 2017;161(6):1482–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kodadek LM, Kapadia MR, Changoor NR, et al. Educating the surgeon-scientist: A qualitative study evaluating challenges and barriers toward becoming an academically successful surgeon. Surgery. 2016;160(6):1456–1465. [DOI] [PubMed] [Google Scholar]
- 8.Andriole DA, Klingensmith ME, Fields RC, Jeffe DB. Is dedicated research time during surgery residency associated with surgeons’ future career paths?: A national study: A national study. Ann Surg. 2020;271(3):590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hutchins BI, Yuan X, Anderson JM, Santangelo GM. Relative citation ratio (RCR): A new metric that uses citation rates to measure influence at the article level. PLoS Biol. 2016;14(9):e1002541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hutchins BI, Hoppe TA, Meseroll RA, Anderson JM, Santangelo GM. Additional support for RCR: A validated article-level measure of scientific influence. PLoS Biol. 2017;15(10):e2003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.2023 methodology. Blue Ridge Institute for Medical Research | an independent non-profit organization founded in 2006. February 6, 2024. Accessed July 4, 2025. https://brimr.org/notes-on-methodology-2023/
- 12.Viergever RF, Hendriks TCC. The 10 largest public and philanthropic funders of health research in the world: what they fund and how they distribute their funds. Health Res Policy Syst. 2016;14(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Narahari AK, Mehaffey JH, Hawkins RB, et al. Surgeon scientists are disproportionately affected by declining NIH funding rates. J Am Coll Surg. 2018;226(4):474–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demblowski LA, Steinberg SM, Meseroll RA, Santangelo GM, Zeiger MA. National Institutes of Health funding for surgeon-scientists in the US-an update and an expanded landscape. JAMA Surg. 2024;159(3):323–330. [DOI] [PubMed] [Google Scholar]
- 15.Demblowski LA, Busse B, Santangelo G, et al. NIH funding for surgeon-scientists in the US: What is the current status? J Am Coll Surg. 2021;232(3):265–274.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simplified peer review framework. Accessed March 20, 2025. https://grants.nih.gov/policy-and-compliance/policy-topics/peer-review/simplifying-review/framework
- 17.Mesquita-Neto JW, Dailey W, Macedo FI, Merchant NB. Patterns of national institutes of health grant funding to surgical research and scholarly productivity in the United States. Ann Surg. 2020;272(4):539–546. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen M, Gonzalez L, Newman A, et al. Rates of National Institutes of Health funding for surgeon-scientists, 1995–2020. JAMA Surg. 2023;158(7):756–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mesquita-Neto JW, Dailey W, Macedo FI, Merchant NB. Patterns of National Institutes of Health grant funding to surgical research and scholarly productivity in the United States. Ann Surg. 2020;272(4):539–546. [DOI] [PubMed] [Google Scholar]
- 20.Juprasert JM, Marshall TE, Blood AG, Obeid L, Yeo HL. How to support a surgeon scientist: Lessons from national institutes of health K-award recipients. J Surg Res. 2021;260:163–168. [DOI] [PubMed] [Google Scholar]
- 21.Schwartz PB, Krecko LK, Park KY, O’Rourke AP, Greenberg J, Jung S. Our thoughts: Improving general surgery resident preparedness for dedicated research time. Am J Surg. 2022;223(6):1217–1219. [DOI] [PubMed] [Google Scholar]
- 22.Ladner DP, Goldstein AM, Billiar TR, et al. Transforming the future of surgeon-scientists. Ann Surg. 2024;279(2):231–239. [DOI] [PubMed] [Google Scholar]
- 23.Barker JC, Jalilvand A, Onuma A, et al. Facilitating success of the early stage surgeon scientist trainee: Growing the surgeon scientist pipeline. Ann Surg. 2022;275(2):e334–e344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McElroy KE, Chen H, Hardiman K, Corey B, Gillis A. Funding a general surgery residency academic development time program. Am J Surg. 2024;228:222–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhattacharya SD, Williams JB, De La Fuente SG, Kuo PC, Seigler HF. does protected research time during general surgery training contribute to graduates’ career choice?. Am Surg. 2011;77(7):907–910. [PMC free article] [PubMed] [Google Scholar]
- 26.Papasavas P, Filippa D, Reilly P, Chandawarkar R, Kirton O. Effect of a mandatory research requirement on categorical resident academic productivity in a university-based general surgery residency. J Surg Educ. 2013;70(6):715–719. [DOI] [PubMed] [Google Scholar]
- 27.Alnahhal KI, Lingutla R, Penukonda S, et al. Comparison of academic productivity and funding support between United States and international medical graduate vascular surgeons. J Vase Surg. 2023;77(5):1513–1521.el. [DOI] [PubMed] [Google Scholar]
- 28.Stain SC, Ellison EC, Farmer DL, et al. The Blue Ribbon Committee II report and recommendations on surgical education and training in the United States: 2024. Ann Surg. 2024;280(4):535–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hawn MT, Matthews JB, Bumgardner GL, et al. Roadmap for research and scholarship in general surgery residency training: Report of the research subcommittee of Blue Ribbon Committee II on surgical education and training: Report of the research subcommittee of Blue Ribbon Committee II on surgical education and training. Ann Surg. Published online July 22, 2024. doi: 10.1097/SLA.0000000000006453 [DOI] [PubMed] [Google Scholar]
- 30.Moore HB, Moore EE, Nehler MR, et al. Bridging the gap from T to K: integrated surgical research fellowship for the next generation of surgical scientists. J Am Coll Surg. 2014;218(2):279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bellomo TR, Lee J, Kochis MA. Trainee perspective on “roadmap for research and scholarship in general surgery residency training.” Ann Surg. 2025;282(1):172–173. [DOI] [PubMed] [Google Scholar]


