Abstract
The management of impaired respiratory gas exchange in patients with nonuniform posttraumatic and septic adult respiratory distress syndrome (ARDS) contains its own therapeutic paradox, since the need for volume-controlled ventilation and PEEP in the lung with the most reduced compliance increases pulmonary barotrauma to the better lung. A computer-based system has been developed by which respiratory pressure-flow-volume relations and gas exchange characteristics can be obtained and respiratory dynamic and static compliance curves computed and displayed for each lung, as a means of evaluating the effectiveness of ventilation therapy in ARDS. Using these techniques, eight patients with asymmetrical posttraumatic or septic ARDS, or both, have been managed using simultaneous independent lung ventilation (SILV). The computer assessment technique allows quantification of the nonuniform ARDS pattern between the two lungs. This enabled SILV to be utilized using two synchronized servo-ventilators at different pressure-flow-volumes, inspiratory/expiratory ratios, and PEEP settings to optimize the ventilatory volumes and gas exchange of each lung, without inducing excess barotrauma in the better lung. In the patients with nonuniform ARDS, conventional ventilation was not effective in reducing shunt (QS/QT) or in permitting a lower FIO2 to be used for maintenance of an acceptable PaO2. SILV reduced per cent v-a shunt and permitted a higher PaO2 at lower FIO2. Also, there was x-ray evidence of ARDS improvement in the poorer lung. While the ultimate outcome was largely dependent on the patient's injury and the adequacy of the septic host defense, by utilizing the SILV technique to match the quantitative aspects of respiratory dysfunction in each lung at specific times in the clinical course, it was possible to optimize gas exchange, to reduce barotrauma, and often to reverse apparently fixed ARDS changes. In some instances, this type of physiologically directed ventilatory therapy appeared to contribute to a successful recovery.
Full text
PDF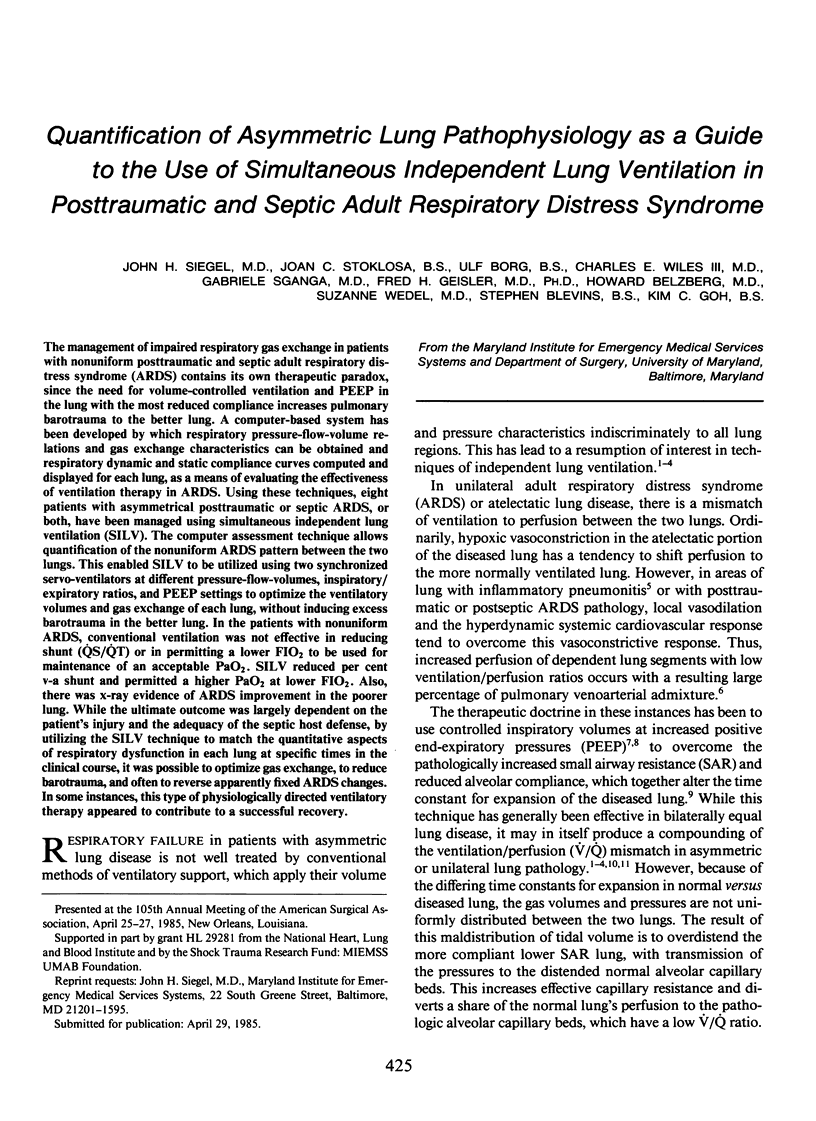
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ashbaugh D. G., Petty T. L., Bigelow D. B., Harris T. M. Continuous positive-pressure breathing (CPPB) in adult respiratory distress syndrome. J Thorac Cardiovasc Surg. 1969 Jan;57(1):31–41. [PubMed] [Google Scholar]
- Baehrendtz S., Bindslev L., Hedenstierna G., Santesson J. Selective PEEP in acute bilateral lung disease. Effect on patients in the lateral posture. Acta Anaesthesiol Scand. 1983 Aug;27(4):311–317. doi: 10.1111/j.1399-6576.1983.tb01958.x. [DOI] [PubMed] [Google Scholar]
- Baehrendtz S., Hedenstierna G. Differential ventilation and selective positive end-expiratory pressure: effects on patients with acute bilateral lung disease. Anesthesiology. 1984 Nov;61(5):511–517. doi: 10.1097/00000542-198411000-00006. [DOI] [PubMed] [Google Scholar]
- Baehrendtz S., Santesson J., Bindslev L., Hedenstierna G., Matell G. Differential ventilation in acute bilateral lung disease. Influence on gas exchange and central haemodynamics. Acta Anaesthesiol Scand. 1983 Jun;27(3):270–277. doi: 10.1111/j.1399-6576.1983.tb01950.x. [DOI] [PubMed] [Google Scholar]
- Carlon G. C., Kahn R., Howland W. S., Baron R., Ramaker J. Acute life-threatening ventilation-perfusion inequality: an indication for independent lung ventilation. Crit Care Med. 1978 Nov-Dec;6(6):380–383. doi: 10.1097/00003246-197811000-00009. [DOI] [PubMed] [Google Scholar]
- Geiger K. Differential lung ventilation. Int Anesthesiol Clin. 1983 Summer;21(2):83–96. doi: 10.1097/00004311-198308000-00007. [DOI] [PubMed] [Google Scholar]
- Glazier J. B., Hughes J. M., Maloney J. E., West J. B. Measurements of capillary dimensions and blood volume in rapidly frozen lungs. J Appl Physiol. 1969 Jan;26(1):65–76. doi: 10.1152/jappl.1969.26.1.65. [DOI] [PubMed] [Google Scholar]
- Hedenstierna G., White F. C., Mazzone R., Wagner P. D. Redistribution of pulmonary blood flow in the dog with PEEP ventilation. J Appl Physiol Respir Environ Exerc Physiol. 1979 Feb;46(2):278–287. doi: 10.1152/jappl.1979.46.2.278. [DOI] [PubMed] [Google Scholar]
- Hillman K. M., Barber J. D. Asynchronous independent lung ventilation (AILV). Crit Care Med. 1980 Jul;8(7):390–395. doi: 10.1097/00003246-198007000-00006. [DOI] [PubMed] [Google Scholar]
- Kumar A., Falke K. J., Geffin B., Aldredge C. F., Laver M. B., Lowenstein E., Pontoppidan H. Continuous positive-pressure ventilation in acute respiratory failure. N Engl J Med. 1970 Dec 24;283(26):1430–1436. doi: 10.1056/NEJM197012242832603. [DOI] [PubMed] [Google Scholar]
- Light R. B., Mink S. N., Wood L. D. Pathophysiology of gas exchange and pulmonary perfusion in pneumococcal lobar pneumonia in dogs. J Appl Physiol Respir Environ Exerc Physiol. 1981 Mar;50(3):524–530. doi: 10.1152/jappl.1981.50.3.524. [DOI] [PubMed] [Google Scholar]
- Light R. B., Mink S. N., Wood L. D. The effect of unilateral PEEP on gas exchange and pulmonary perfusion in canine lobar pneumonia. Anesthesiology. 1981 Sep;55(3):251–255. doi: 10.1097/00000542-198109000-00011. [DOI] [PubMed] [Google Scholar]
- OTIS A. B., MCKERROW C. B., BARTLETT R. A., MEAD J., MCILROY M. B., SELVER-STONE N. J., RADFORD E. P., Jr Mechanical factors in distribution of pulmonary ventilation. J Appl Physiol. 1956 Jan;8(4):427–443. doi: 10.1152/jappl.1956.8.4.427. [DOI] [PubMed] [Google Scholar]
- Oppenheimer L., Craven K. D., Forkert L., Wood L. D. Pathophysiology of pulmonary contusion in dogs. J Appl Physiol Respir Environ Exerc Physiol. 1979 Oct;47(4):718–728. doi: 10.1152/jappl.1979.47.4.718. [DOI] [PubMed] [Google Scholar]
- Powers S. R., Jr, Mannal R., Neclerio M., English M., Marr C., Leather R., Ueda H., Williams G., Custead W., Dutton R. Physiologic consequences of positive end-expiratory pressure (PEEP) ventilation. Ann Surg. 1973 Sep;178(3):265–272. doi: 10.1097/00000658-197309000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powner D. J., Eross B., Grenvik A. Differential lung ventilation with PEEP in the treatment of unilateral pneumonia. Crit Care Med. 1977 Jul-Aug;5(4):170–172. doi: 10.1097/00003246-197707000-00002. [DOI] [PubMed] [Google Scholar]
- Sachdeva S. P. Treatment of post-operative pulmonary atelectasis by active inflation of the atelectatic lobe(s) through an endobronchial tube. Acta Anaesthesiol Scand. 1974;18(2):65–70. doi: 10.1111/j.1399-6576.1974.tb00844.x. [DOI] [PubMed] [Google Scholar]
- Siegel J. H., Farrell E. J., Miller M., Goldwyn R. M., Friedman H. P. Cardiorespiratory interactions as determinants of survival and the need for respiratory support in human shock states. J Trauma. 1973 Jul;13(7):602–619. doi: 10.1097/00005373-197307000-00005. [DOI] [PubMed] [Google Scholar]
- Siegel J. H., Giovannini I., Coleman B. Ventilation:perfusion maldistribution secondary to the hyperdynamic cardiovascular state as the major cause of increased pulmonary shunting in human sepsis. J Trauma. 1979 Jun;19(6):432–460. [PubMed] [Google Scholar]
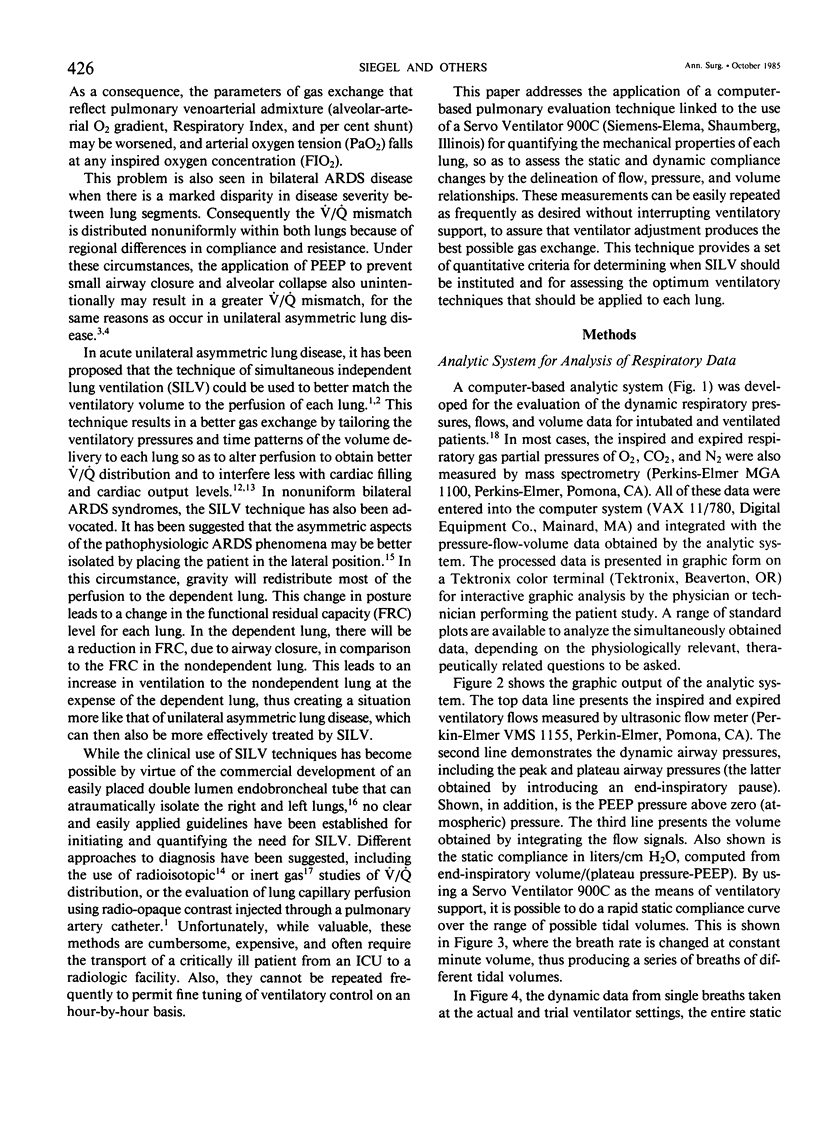
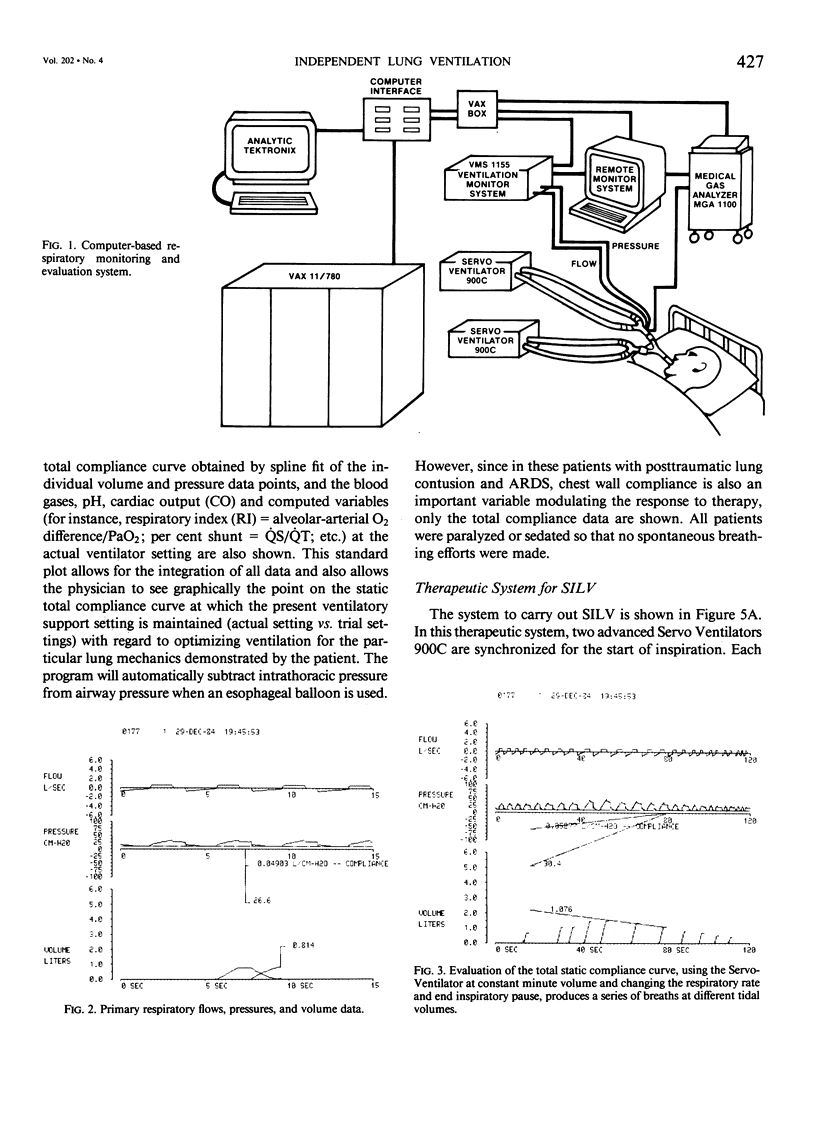
- Siegel J. H., Stoklosa J., Geisler F. H., Borg U., Kung Y., Goh K., Belzberg H., Wedel S., Wiles C. E., 3rd Computer-based evaluation of cardiopulmonary function for the optimization of ventilatory therapy in the adult respiratory distress syndrome. Int J Clin Monit Comput. 1984;1(2):107–126. doi: 10.1007/BF01872749. [DOI] [PubMed] [Google Scholar]
- Suter P. M., Fairley B., Isenberg M. D. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975 Feb 6;292(6):284–289. doi: 10.1056/NEJM197502062920604. [DOI] [PubMed] [Google Scholar]
- Suter P. M., Fairley H. B., Isenberg M. D. Effect of tidal volume and positive end-expiratory pressure on compliance during mechanical ventilation. Chest. 1978 Feb;73(2):158–162. doi: 10.1378/chest.73.2.158. [DOI] [PubMed] [Google Scholar]
- WEST J. B., DOLLERY C. T., HEARD B. E. INCREASED PULMONARY VASCULAR RESISTANCE IN THE DEPENDENT ZONE OF THE ISOLATED DOG LUNG CAUSED BY PERIVASCULAR EDEMA. Circ Res. 1965 Sep;17:191–206. doi: 10.1161/01.res.17.3.191. [DOI] [PubMed] [Google Scholar]
- WEST J. B., DOLLERY C. T., NAIMARK A. DISTRIBUTION OF BLOOD FLOW IN ISOLATED LUNG; RELATION TO VASCULAR AND ALVEOLAR PRESSURES. J Appl Physiol. 1964 Jul;19:713–724. doi: 10.1152/jappl.1964.19.4.713. [DOI] [PubMed] [Google Scholar]