Abstract
Background
Stapes prostheses play a crucial role in improving auditory performance and facilitating the patient's reintegration into social life. However, determining the ideal characteristics of a prosthesis and identifying the best commercially available option remain challenging. This study aims to compare the outcomes of two different types of prostheses: the MatriX Stapes Prosthesis and the new mAXIS Stapes Prosthesis.
Methods
A prospective study was conducted on patients diagnosed with suspected otosclerosis who underwent stapedotomy, receiving either the MatriX or mAXIS prosthesis randomly during surgery. Postoperative follow-ups were conducted for at least one year. Audiometric evaluations were analyzed using statistical tests. Additionally, a systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement.
Results
The prospective study included 84 patients, divided into two groups (G1: MatriX, G2: mAXIS). The auditory results were satisfactory for both prostheses, demonstrating their effectiveness in improving hearing thresholds. We observed a gain for air conduction threshold of 26.2 dB vs 21.2 dB with an ABG closure of 20.7 dB vs and 21.2 dB in G1 and G2 respectively. The literature review encompassed 15 studies, revealing overall positive outcomes with different prosthetic materials.
Conclusions
The study revealed effective auditory improvement with both prostheses, yet no statistically significant differences in air-bone gap closure or average hearing gain. Titanium emerged as the preferred material due to its biocompatibility, lightweight nature, and stability under magnetic resonance imaging. The mAXIS prosthesis is introduced as a cost-effective alternative with favorable intraoperative features.
Keywords: stapedotomy, stapes surgery, stapes prostheses, systematic review
1. Introduction
Otosclerosis is an osteodystrophic disease that affects the bone of the otic capsule. This condition is particularly relevant in the Caucasian population, where it is estimated to affect between 0.3% and 0.4% of individuals [Hall, 1974; Pearson et al., 1974; Deaclu et al., 2001; Dispenza et al., 2013]. The clinical presentation of otosclerosis is characterized by a gradual and slow hearing loss that mainly affects low frequencies. This process can progress for several years without the patient being aware, especially in bilateral cases, which constitute about 80% of otosclerosis cases, although the disease often starts with unilateral involvement [Thomas et al., 2011;Pollarolo et al., 2022]. Vertigo is reported by 10% of patients, manifesting only when the disease progresses to involve the semicircular canals of the inner ear [Ealy and Smith, 2011;Priola et al., 2021]. Tinnitus, on the other hand, afflicts about half of the patients [Rudic et al, 2015]. The treatment of hearing impairment in a patient with otosclerosis can be approached in various ways: follow-up, application of a hearing aid or surgical intervention with the placement of a stapes prosthesis. The decision on the treatment option to adopt depends on a thorough evaluation of various factors, including the severity of hearing loss, patient preference, medical contraindications, and other aspects. Stapes prostheses are effective in improving the patient's auditory performance and allowing a normal reintegration into social life. To date, comparing the various prosthetics available in the market to determine which is the best is very challenging. Differences in auditory outcomes between prostheses are minimal and depend on the material composition of the prosthesis, the type of attachment to the incus, and the piston dimensions [Sevy and Arriaga, 2018]. Today, various materials are used, and often multiple materials are incorporated into the same prosthesis. Materials such as Teflon, stainless steel, tantalum, platinum, and gold constitute the most used prostheses in stapes surgery [Fritsch and Naumann, 2008]. The attachment of the prosthesis to the incus is an extremely delicate surgical step and can influence the auditory outcomes of the surgical procedure, for this reason, over time, specific instruments have been created to adapt to the small dimensions of a prosthesis. The dimensions of a prosthesis also significantly influence the success of the surgical procedure: The length of the piston is chosen by the surgeon based on the distance between the footplate and the medial face of the long crus of the incus, diameter, on the other hand, is the variable that most influences the auditory result of a prosthesis [Sevy and Arriaga, 2018].
The aim of our study is to compare the results obtained using two different types of prostheses, specifically the MatriX Titanium Stapes Prosthesis produced by "Heinz KURZ GmbH Medizintechnik" and the new mAXIS Titanium Stapes Prosthesis produced by "MED-EL Medical Electronics", by reporting our experience and discussing the results of the existing literature review.
2. Material and methods
2.1. Study group
From January 2021 to December 2023, we conducted a prospective study, enrolling patients with a suspected clinical and audiological otosclerosis diagnosis. All recruited patients underwent a detailed collection of medical history (personal data, onset of symptoms, hearing disorders, and any previous medical and/or surgical treatments performed) and a comprehensive otorhinolaryngological examination, including micro-otoscopy and endoscopy of the upper airways. Subsequently, they underwent an audiometric examination, evaluating air conduction (AC), bone conduction (BC), and the air-bone gap (ABG). Patients previously subjected to stapedectomy or surgical revisions were excluded from our study. The recruited patients were randomly divided into two groups by using Stata software (Release 18, StataCorp LLC, College Station, TX): group 1 (G1) received the MatriX Titanium Stapes Prosthesis produced by "Heinz KURZ GmbH Medizintechnik" (Figure 1), while group 2 (G2) received the mAXIS Titanium Stapes Prosthesis produced by "MED-EL Medical Electronics" (Figure 2). The study protocol was then explained to the patients, who, after complete counseling, provided their written consent.
Figure 1.

MatriX Stapes Prosthesis
Figure 2.

mAXIS Stapes Prosthesis
2.2. Prostheses characteristics
Both the MatriX and mAXIS Stapes Prostheses are designed with a variable length, ranging from 3.5 mm to 5.5 mm, and a variable diameter between 0.4 mm and 0.6 mm. Regarding the shape, the main difference between the two prostheses lies in the band loop width: the MatriX features a loop width of 0.5 mm, while the mAXIS is designed with a broader band loop measuring 0.85 mm. Concerning the weight of the prostheses, only the technical data sheet for the mAXIS provides this information, which can vary from 1.0 to 3.5 mg, depending on the length and diameter.
2.3. Surgical treatment
Surgery was performed on all patients by the same otosurgeon by using the reverse steps stapedotomy technique through a transcanal approach to access the middle ear. The choice of technique (classic or reverse stapedotomy) used by the otosurgeon was based on the intraoperative anatomical conformation, as well as the choice of the dimensions of the prosthesis to be placed in the middle ear. The surgical procedure began with infiltration of the skin of the external auditory canal with Mepivacaine hydrochloride 44 mg + Adrenaline 22 µg, incision and elevation of the tympanic-meatum flap. At this point, the stapes and the remaining ossicular chain have been palpated to ensure that the stapes is indeed fixed. Subsequently, the scutum was removed to visualize the niche of the oval window and expose the tympanic portion of the facial nerve. The chorda tympani was then identified and displaced anteriorly, and the platina-incus distance was measured. At this stage, it was possible to identify all landmarks, including the superstructure of the stapes, platina, tendon of the stapedius muscle, and pyramidal eminence. In the classical technique, the procedure continues with the disarticulation of the incudo-stapedial joint. The tendon of the stapedius muscle is then cut, and the superstructure of the stapes is removed. Once the footplate of the stapes is exposed, a stapedotomy is performed using a skeeter drill with a 0.6 mm diamond burr. Subsequently, the prosthesis is positioned and crimped at the level of the long process of the incus, the tympanic meatus flap is repositioned, and the external auditory canal is packed with gelfoam.
In the reverse technique, once all the landmarks were identified, we proceeded first with the stapedotomy using a skeeter drill with a 0.6 mm diamond burr. Subsequently, we performed the placement and crimping of the prosthesis to the long process of the incus. We continued with the disarticulation of the incudostapedial joint and stapedial tendon cut and we removed the superstructure of the stapes removal. The tympanic-meatus flap was then repositioned, and the external auditory canal was packed with gelfoam, as in the classical technique.
2.4. Follow-up
During the first postoperative month, patients underwent weekly follow-ups appointments to assess healing. Additionally, patients underwent audiometric examination to assess hearing recovery and speech audiometry examination to confirm the quality of auditory recovery. Long-term follow-up was conducted for at least one year. The assessment of auditory function was conducted for both the entire patient cohort enrolled in the study and for specific patient subgroups (G1: MatriX Titanium Stapes Prosthesis; G2: mAXIS Titanium Stapes Prosthesis).
The pre- and postoperative audiometric mean values were evaluated [average values obtained from pure-tone audiometry (PTA) at frequencies 0.25-0.5-1-2-4 kHz for bone conduction and average values at frequencies 0.25-0.5-1-2-4-8 kHz for air conduction according to the World Health Organization classification]. Moreover, we evaluated the gain between bone and air conduction (difference between pre- and postoperative audiometric mean values at frequencies 0.5-1-2-4 kHz), the change in pre- and postoperative air-bone gap (ABG) (difference between pre- and postoperative audiometric mean values at frequencies 0.5-1-2-4 kHz for air and bone conduction), and the closure of the ABG (difference between audiometric mean values at frequencies 0.5-1-2-4 kHz for pre- and postoperative ABG).
2.5. Statistical analysis
The statistical data analysis was performed using the Student’s t-test with R software (R-software inc., 2 Shaw Alley, San Francisco CA 94105). Two types of t-tests were employed: a paired t-test for preoperative and postoperative comparisons within each group and an independent t-test to compare the differences between the two groups. The null hypothesis (H0) and the alternative hypothesis (H1) were as follows:
- H0: There are no statistically significant audiometric differences between the two groups.
- H1: There are statistically significant audiometric differences between the two groups.
The significance level (α) was set at 0.05, with a 95% confidence interval.
2.6. Literature review
The literature review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses group (PRISMA) guidelines. Two independent authors conducted a comprehensive search by consulting the main scientific databases on the web, including PubMed, Google Scholar, Medline, EMBASE, Web of Science, and the Cochrane Library.
Specific keyword pairs such as stapedotomy AND prosthesis was used for the search. Titles and abstracts were reviewed to screen out non-relevant articles and the working group reviewed the full text of remaining articles. The results of the studies were then combined, integrated, and analyzed. The criteria for considering studies for the review were based on the population, intervention, comparison, outcome, timing, and settings (PICOTS) framework.
2.6.1. Population and inclusion criteria
Studies in English language on patients of all ages, genders, and ethnicities with a suspected clinical and audiological otosclerosis diagnosis
2.6.2. Intervention
Studies in which patients underwent stapedotomy with prosthesis placement.
2.6.3. Comparison and outcome
Studies comparing two or more prostheses with their respective audiometric outcomes. Prosthesis efficacy in hearing improvement was considered a primary outcome; improvement in air-bone gap (ABG) with the reduction of the threshold of air conduction was considered a secondary outcome.
2.6.4. Timing
Studies published up to April 2023 have been included in this literature review.
2.6.5. Setting
Randomized controlled trials (RCT), non-randomized controlled trials (NRCT), prospective or retrospective cohort studies and case-control studies from community, private and tertiary care university hospitals were included.
3. Results
3.1. Study sample
This prospective study comprised 84 patients, including 64 females and 20 males. The mean age of the patients was 49.1, with an age range of 42 to 71 years. All patients included in the study reported various degrees of hearing loss, confirmed by audiometric examination. None of the patients had undergone previous surgical interventions in the ENT districts, except for one patient who underwent tonsillectomy and septoplasty, and another patient who underwent tonsillectomy. Fibro-endoscopic examination of the nose, paranasal sinuses, and nasopharynx revealed no pathology in the explored anatomical districts. Patients were randomly assigned to two groups, each comprising 42 cases: G1 (MatriX) with 31/42 females (74%) and 11/42 males (26%), G2 (mAXIS), with 33/42 females (78.6%) and 9/42 males (21.4%). Both groups did not differ in mean age (G1: 49.9 ± 6.7; G2: 48.2 ± 6.7). Out of the total sample, 20/84 (23,8%) had a family history of hearing loss, 12/42 belonging to G1 (28.6%) and 8/42 belonging to G2 (19%). Additionally, 25/84 patients (29.7%) had previously undergone stapedotomy in the contralateral ear, 15/42 belonging to G1 (35.7%) and 10/42 belonging to G2 (23,8%). The baseline clinical characteristics of the patients involved in our study are summarized in Table 1.
Table 1. Demographic data and medical history.
| Patients | Male | Female | Mean age (±SD) | Familiarity with Hearing Impairment | Contralateral SPT | |
| SD= standard deviation, SPT= stapedotomy | ||||||
|
G1
(MatriX) |
42 | 11 | 31 | 49,9 (±6,7) | 12 | 15 |
| 50% | 26% | 74% | 28,6% | 35,7% | ||
|
G2
(mAXIS) |
42 | 9 | 33 | 48,2 (±6,7) | 8 | 10 |
| 50% | 21,4% | 78,6% | 19% | 23,8% | ||
| Total | 84 | 20 | 64 | 49,4 (±6,7) | 20 | 25 |
| 100% | 26% | 74% | 23,8% | 29,7% | ||
All patients included in the study reported varying degrees of hearing loss. Other symptoms reported by patients included tinnitus [G1: 64.3% (27/42); G2: 38.1% (16/42)], otalgia [G1: 11.9% (5/42); G2: 9.5% (4/42)], dizziness [G1: 23.8% (10/42); G2: 19% (8/42)], nausea and vomiting [G1: 4.8% (2/42); G2: 2.4% (1/42)], headache [G1: 4.8% (2/42); G2: 2.4% (1/42)], sudden sensorineural hearing loss [G1: 4.8% (1/42); G2: 0% (0/42)]. The data regarding the symptoms reported by patients are presented in Table 2.
Table 2. Symptoms.
| Patients | Hearing loss | Tinnitus | Otalgia | Dizziness | Nausea and vomiting | Headache | Other* | |
| *Sudden hearing loss | ||||||||
|
G1
(MatriX) |
42 | 42 | 27 | 5 | 10 | 2 | 2 | 1 |
| 50% | 100% | 64,3% | 11,9% | 23,8% | 4,8% | 4,8% | 2,4% | |
|
G2
(mAXIS) |
42 | 42 | 16 | 4 | 8 | 1 | 1 | 0 |
| 50% | 100% | 38,1% | 9,5% | 19% | 2,4% | 2,4% | 0% | |
A classic stapedotomy was preferred in 47.9% (20/42) of G1 patients and 50% (21/42) of G2 patients, while the reverse technique was chosen in the remaining 52.1% (22/42) and 50% (21/42), respectively, of G1 and G2 patients. A 4.5mm prosthesis was used in 73.8% of cases (31/42), a 4.25mm prosthesis in 16.7% (7/42), and a 5mm prosthesis in 9.5% (4/42) of cases in the G1 group. In the G2 group, however, a 4.5mm prosthesis was used in 83.3% of cases (35/42), a 4.75mm prosthesis in 9.5% (4/42), and a 4.25mm prosthesis in 7.1% (3/42). In the G1 group, a prosthesis with a diameter of 0.5mm was used in 69% of cases (29/42), while a prosthesis with a diameter of 0.6mm was used in 31% of cases (13/42). In the G2 group, a 0.5mm prosthesis was used in 81% of cases (34/42), and a 0.6mm prosthesis in 19% of cases (8/42).
The stapes footplate was drilled with a skeeter of dimensions comparable to those of the implanted prosthesis in 100% of cases (42/42 in both the G1 and G2 groups). Consequently, any minimal gap between the prosthesis and the footplate hole, where present, was left unfilled and not treated with any material.
No serious complications were observed during or after the surgical intervention; three patients (7.1%) in G1 and two patients (4.8%) in G2 reported a tympanic membrane perforation, four patients (9.5%) in Group G1 and three patients (7.1%) in Group G2 suffered damage to the chorda tympani (Table 3).
Table 3. Complications.
| Patients | Intraoperative complications | Postoperative complications | ||||
| *Skin hives | ||||||
| Tympanic perforation | Chorda Tympani damage | Other | Vertigo | Other | ||
|
G1
(MatriX) |
42 | 3 | 4 | – | 6 | 3* |
| 50% | 7,1% | 9,5% | – | 14,3% | 7,1% | |
|
G2
(mAXIS) |
42 | 2 | 3 | – | 4 | – |
| 50% | 4,8% | 7,1% | – | 9,5% | – | |
The auditory results were satisfactory for both prostheses, demonstrating their effectiveness in improving hearing thresholds. We observed a gain in bone conduction threshold of 5.4 dB (p ≤ 0.05) and 26.2 dB (p ≤ 0.001) for air conduction in G1, with an ABG closure of 20.7 dB (p ≤ 0.001); G2 did not show any improvement in bone conduction, while there was an increase of 21.2 dB (p ≤ 0.001) for air conduction and 21.2 dB (p ≤ 0.001) for ABG (Table 4).
Table 4. G1 (MatriX) vs G2 (mAXIS) mean hearing threshold.
| G1 (MatriX) | G2 (mAXIS) | ||||||
| BC= bone conduction (250-4000 Hz), AC= air conduction (250-8000 Hz), ABG= air-bone gap (250-4000 Hz), NA= not available. | |||||||
| BC | AC | ABG | BC | AC | ABG | ἀ | |
| Preoperative | 26,4 | 59,1 | 32,7 | 18,6 | 53,6 | 35,0 | 0,05 |
| Postoperative | 20,9 | 32,9 | 11,9 | 18,6 | 32,3 | 13,7 | 0,05 |
| Gain | 5,4 | 26,2 | 20,7 | 0 | 21,2 | 21,2 | |
| p-value | 0,04 | 0,0000001 | 0,000001 | 1 | 0,00004 | 0,00001 | |
In the postoperative period, 94.1% of G1 patients achieved an average ABG < 20 dB; the same result was obtained by 100% of G2 patients, moreover 52.9% of G1 patients and 50% of G2 patients reached an average ABG closure in the range of 0-10 dB.
Comparing the auditory data of both prostheses, we did not find any statistically significant differences in terms of ABG and average hearing gain. However, the preoperative mean for bone conduction in G1 was significantly worse than G2 [26.4 dB vs 18.9 dB (p ≤ 0.05)]; G1, on the other hand, recorded better air conduction gain (33.8 dB) than that achieved by Group 2 (21.2 dB) at the frequency of 250 Hz (p ≤ 0.05) (Table 5).
Table 5. G1 (MatriX) vs. G2 (mAXIS) gain and ABG improvement.
| 250 | 500 | 1000 | 2000 | 4000 | ἀ | ||
| BC gain | G1(MatriX) | 2,35 | 4,12 | 6,47 | 4,12 | 7,06 | <0,05 |
| G2 (mAXIS) | –1,88 | –1,88 | 4,38 | –0,63 | –1,88 | <0,05 | |
| p | 0,28 | 0,17 | 0,65 | 0,23 | 0,18 | ||
| AC gain | G1(MatriX) | 33,82 | 32,65 | 30,00 | 20,00 | 22,06 | <0,05 |
| G2 (mAXIS) | 21,25 | 24,38 | 21,88 | 22,50 | 16,25 | <0,05 | |
| p | 0,03 | 0,06 | 0,07 | 0,60 | 0,18 | ||
| ABG improvement | G1(MatriX) | 31,47 | 28,53 | 23,53 | 15,88 | 15,00 | <0,05 |
| G2 (mAXIS) | 23,13 | 26,25 | 17,50 | 23,13 | 18,13 | <0,05 | |
| p | 0,18 | 0,66 | 0,14 | 0,14 | 0,64 |
BC= bone conduction (250-4000 Hz), AC= air conduction (250-8000 Hz), ABG= air-bone gap (250-4000 Hz), NA= not available.
3.2. Literature review
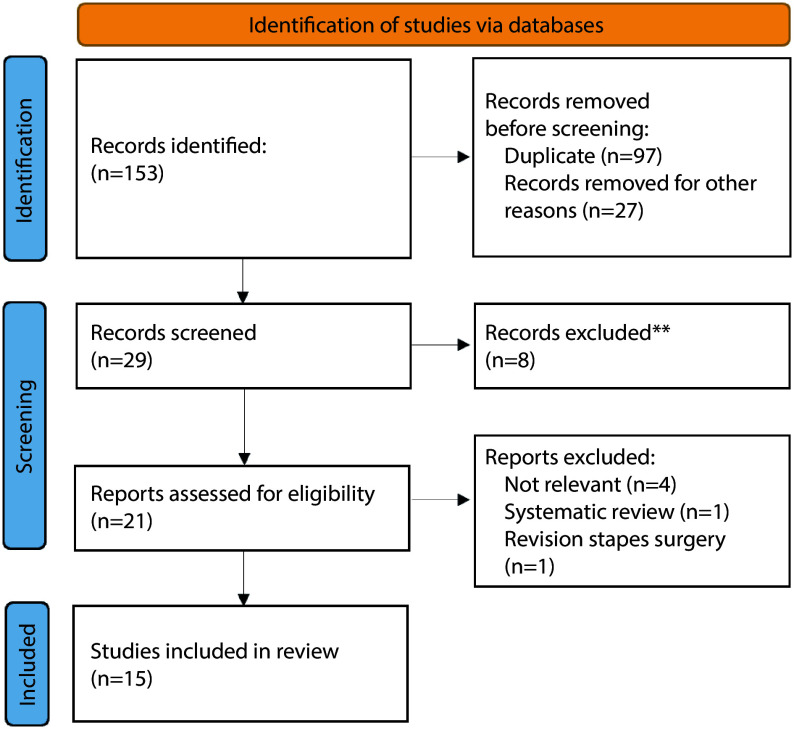
A total of 153 articles were identified. A first screening allowed us to eliminate 97 duplicates, and therefore, to consider the remaining 56 articles. Twenty-seven articles were excluded based on title/abstract screening, allowing us to select 29 articles for full-text screening. Then, the application of inclusion and exclusion criteria allowed us to select only 15 papers for inclusion in the review (Figure 3).
Figure 3.
PRISMA 2020 flow diagram
Table 6 presents the selected manuscripts along with the baseline characteristics of each study group. The studies included in the review evaluated two or more prostheses using pure tone audiometry tests and, based on the results obtained, all demonstrate good efficacy in terms of auditory improvement. Only two authors highlighted statistically significant differences in terms of ABG and average gain between the prostheses examined in their studies. Mangham et al. (2008a) showed a statistically significant difference in the average ABG between the CliP-piston a`Wengen Titanium prosthesis and the Schuknecht Teflon-wire prosthesis in favor of the latter [Mangham CA et al. 2008a]. In another study, the same authors concluded that the average ABG for the 0.6 mm Teflon piston is significantly lower than the 0.6 mm Titanium piston and the 0.5 mm Teflon piston both at 2 months and 1 year postoperatively [Mangham CA, 2008b].Canu et al. (2017) study revealed that the average ABG closure and the percentage of ABGs <15 dB and <10 dB was significantly better for the group that received the Nitinol prosthesis compared to the groups with Fluoroplastic and Titanium prostheses (similar results were obtained when comparing the two groups with titanium prostheses) [Canu et al. 2017] (Table 7).
Table 6. Literature review, hearing thresholds.
| Author | Prosthesis | Study Group | Mean preoperative | Mean postoperative | Gain | ABG | Minimum Follow-up | ||||||||
| Total | Groups | ||||||||||||||
| n | % | n | % | BC | AC | BC | AC | BC | AC | Pre | Post | Gain | |||
| Our case series | MatriX Titanium Stapes Prosthesis | 25 | 100% | 17 | 68% | 26,4 | 59,12 | 20,96 | 32,94 | 5,44 | 26,18 | 32,72 | 11,99 | 20,74 | 12 |
| mAXIS Titanium Stapes Prosthesis | 8 | 32% | 18,59 | 53,59 | 18,59 | 32,34 | 0 | 21,25 | 35 | 13,75 | 21,25 | ||||
| p-value | 0,05 | 0,18 | 0,53 | 0,87 | 0,05 | 0,19 | 0,51 | 0,46 | 0,88 | ||||||
| Faramarzi et al. (2020) | Fluoroplastic Causse Loop Piston | 148 | 100% | 76 | 51,35% | 13,6 | 46,9 | 6,6 | 17,7 | 7 | 29,2 | 33,3 | 11,1 | 22,23 | 6 |
| Big Easy Piston | 72 | 48,65 | 12,8 | 45,2 | 7,9 | 20,2 | 4,9 | 25 | 32,4 | 12,3 | 20,1 | ||||
| p-value | 0,48 | 0,34 | 0,18 | 0,13 | 0,10 | 0,04 | - | - | - | ||||||
| Faramarzi et al. (2021) | Fluoroplastic Causse Loop Piston | 88 | 100% | 44 | 50% | 12,7 | 48,1 | 9,3 | 23,9 | 3,4 | 24,3 | 35,4 | 14,5 | 20,9 | |
| MatriX Stapes Prosthesis Titanium | 44 | 50% | 12,3 | 47,6 | 9,5 | 23,7 | 2,9 | 23,9 | 35,3 | 14,2 | 21,1 | NA | |||
| p-value | 0,74 | 0,78 | 0,90 | 0,91 | 0,67 | 0,86 | 0,93 | 0,76 | 0,91 | ||||||
| Faramarzi et al. (2017) | Fluoroplastic Causse Loop Piston | 120 | 100% | 63 | 52,5% | 15 | 49 | 14,1 | 31,9 | 0,9 | 17,1 | 34,1 | 17,8 | 16,3 | |
| Titanium Soft-clip Piston | 57 | 47,5% | 15,4 | 46,1 | 12,1 | 30,3 | 3,3 | 15,9 | 30,8 | 18,1 | 12,6 | 6 | |||
| p-value | - | - | - | - | - | - | - | - | - | ||||||
| Grolman | K-piston Titanium Prosthesis | 126 | 100% | 63 | 50% | - | 54,3 | - | 34,1 | - | 20,2 | 39,1 | 11,8 | 27,3 | NA |
| CliP-piston a`Wengen Titanium | 63 | 50% | - | 52,3 | - | 32,1 | - | 20,2 | 37,3 | 11,6 | 25,7 | ||||
| p-value | - | - | - | - | - | - | - | - | - | ||||||
| Hornung et al. (2009) | Titanium Soft-clip Piston | 44 | 100% | 21 | 47,73 | 26,7 | - | 27,4 | - | -0,7 | - | 26,5 | 8,9 | 17,6 | 12 |
| CliP-piston a`Wengen Titanium Prosthesis | 23 | 52,27% | 28 | - | 27,9 | - | 0,1 | - | 28,4 | 8,5 | 19,9 | ||||
| p-value | - | - | - | - | - | - | - | - | - | ||||||
| Canu et al. (2017) | NiTiBOND Stapes Prosthesis | 50 | 17,79% | 25 | 48 | 21 | 27 | 3 | 20 | 22 | 6 | 16 | 1 | ||
| Fluoroplastic Piston | 281 | 100% | 50 | 17,79% | 22 | 44 | 20 | 30 | 1 | 14 | 22 | 10 | 12 | ||
| First Titanium Prosthesis | 131 | 72,38% | 24 | 49 | 18 | 28 | 6 | 21 | 25 | 10 | 15 | ||||
| Last Titanium Prosthesis | 50 | 17,79% | 26 | 47 | 23 | 28 | 2 | 19 | 21 | 5 | 16 | ||||
| p-value | - | - | - | - | - | - | - | - | P1: < 0,0001 P2: 0,0001 P3: 0,0001 P4: 0,6 |
||||||
| Odat et al. (2021) | K-piston Titanium prosthesis/Titanium Soft-clip Piston | 58 | 100% | - | - | - | - | - | - | - | - | 27 | 10 | 17 | 12 |
| Fluoroplastic Piston | - | - | - | - | - | - | - | - | 29 | 6 | 23 | ||||
| p-value | - | - | - | - | - | - | 0,37 | 0,12 | 0,05 | ||||||
| Huber et al. (2014) | NiTiBOND Stapes Prosthesis | 116 | 100% | 41 | 35,34% | - | - | - | - | - | - | 8,1 | - | - | |
| SMart Nitinol Piston Prosthesis | 75 | 64,66 | - | - | - | - | - | - | 9,9 | - | - | NA | |||
| p-value | - | - | - | - | - | - | Ptot: < 0,01 | - | - | ||||||
| Tange et al. (1998) | Golden Piston | 106 | 100% | 53 | 50% | - | 52,3 | - | 32,1 | - | 20,2 | 30,0 | 11,6 | - | 7 |
| K-piston Titanium prosthesis | 53 | 50% | - | 54,3 | - | 34,1 | - | 20,2 | 28,2 | 7,6 | - | ||||
| p-value | - | - | - | - | - | - | - | - | - | ||||||
| Mangham CA et al. (2008a) | The Schuknecht Teflon-wire Piston | 311 | 100% | 50 | 16,08% | - | - | - | - | - | - | - | 4,5 | - | 12 |
| De La Cruz Teflon-Platinum Wire Piston | 30 | 9,65% | - | - | - | - | - | - | - | 4,8 | - | ||||
| Mangham Teflon-Platinum Double-fold Piston | 179 | 57,56% | - | - | - | - | - | - | - | 5 | - | ||||
| CliP-piston a`Wengen Titanium Prosthesis | 32 | 10,29 | - | - | - | - | - | - | - | 7,7 | - | ||||
| Teflon Robinson Piston | 20 | 6,43% | - | - | - | - | - | - | - | 7,1 | - | ||||
| p-value | - | - | - | - | - | - | - | - | - | ||||||
| Potena et al.(2015) | Portmann Clip Piston Stainless Steel/Fluoroplastic | 64 | 100% | 32 | 50% | - | - | - | - | - | - | - | - | 16,63 | 2 |
| Titanium Soft-clip Piston | 32 | 50% | - | - | - | - | - | - | - | - | 20,59 | ||||
| p-value | - | - | - | - | < 0,01 | < 0,01 | - | - | < 0,01 | ||||||
| Schrotzlmair | NiTiBOND Stapes Prosthesis | 62 | 100% | 21 | 33,87% | - | - | - | - | - | - | 27,1 | 8,2 | 18,9 | 2 |
| K-piston Titanium Prosthesis | 28 | 45,16% | - | - | - | - | - | - | 26 | 11,2 | 14,8 | ||||
| CliP-piston a`Wengen Titanium Prosthesis | 13 | 20,97% | - | - | - | - | - | - | 30,1 | 17,2 | 12,9 | ||||
| p-value | - | - | - | - | - | - | Ptot: 0,537 | P1: < 0,16 P2: 0,004 P3: 0,03 |
- | ||||||
| Harris and Gong (2007) | SMart Nitinol Piston Prosthesis | 54 | 100% | 26 | 48,15% | - | 50,14 | - | 24,81 | - | 25,33 | 28,61 | 7,07 | 21,54 | 3 |
| Richards-Gyrus Conventional Stainless Steel/ Platinum Ribbon Teflon Piston Prosthesis |
28 | 51,85% | - | 50,04 | - | 27,46 | - | 22,58 | 26,12 | 6,38 | 19,74 | ||||
| p-value | - | 0,97 | - | 0,22 | - | - | 0,19 | 0,52 | - | ||||||
| Mangham CA et al (2008b) | PlatinumTeflon Double-loop Piston (0,5 mm) | 99 | 100% | 13 | 12,15% | - | - | - | - | - | - | - | 8,1 | - | 12 |
| PlatinumTeflon Double-loop Piston (0,6 mm) | 56 | 52,34% | - | - | - | - | - | - | - | 5,4 | - | ||||
| CliP-piston a`Wengen Titanium Prosthesis | 30 | 28,04% | - | - | - | - | - | - | - | 7,7 | - | ||||
| p-value | - | - | - | - | - | - | - | - | - | ||||||
| Rajan et al | Nitinol Stapes Piston Prosthesis | 36 | 100% | 9 | 25% | - | 37,59 | - | 6,48 | - | 31,11 | - | - | - | 3 |
| Titanium Prosthesis | 27 | 75% | - | 36,48 | - | 14,72 | - | 21,76 | - | - | - | ||||
| p-value | - | 0,1 | - | 0,08 | - | - | - | - | |||||||
Table 7. Literature review, conclusions.
| Author | Prosthesis | Conclusions |
| Our case series. | MatriX Titanium Stapes Prosthesis | No statistically significant difference (ABG and average gain) between the prostheses. The gain in VA is better in the group with MatriX prostheses at 250 Hz. |
| mAXIS Titanium Stapes Prosthesis | ||
| Faramarzi et al. (2020) | Fluoroplastic Causse Loop Piston | No statistically significant difference (ABG and average gain) between the prostheses. The gain in VA is better in the group with Teflon prostheses at 250-500-1000 Hz. |
| Big Easy Piston | ||
| Faramarzi et al. (2021) | Fluoroplastic Causse Loop Piston | No statistically significant difference (ABG and average gain) between the prostheses. The closure of ABG is better in the group with titanium prostheses at 250 Hz. |
| MatriX Stapes Prosthesis Titanium | ||
| Faramarzi et al. (2017) | Fluoroplastic Causse Loop Piston | No statistically significant difference (ABG and average gain) between the prostheses. The closure of ABG is better in the group with Teflon prostheses at 250-500 Hz. |
| Titanium Soft-clip Piston | ||
| Tange and Grolman | K-piston Titanium Prosthesis | No statistically significant difference (ABG and average gain) between the prostheses. |
| CliP-piston a`Wengen Titanium | ||
| Hornung et al. (2009) | Titanium Soft-clip Piston | No statistically significant difference (ABG and average gain) between the prostheses. |
| CliP-piston a`Wengen Titanium Prosthesis | ||
| Canu et al. (2017) | NiTiBOND Stapes Prosthesis | The closure of the average ABG and the percentage of ABGs <15 dB and <10 dB was significantly better in the group with Nitinol prostheses compared to the groups with Teflon prostheses and the group with titanium prostheses (first prosthesis). Similar results were obtained when comparing the two groups with titanium prostheses. |
| Fluoroplastic Piston | ||
| First Titanium Prosthesis | ||
| Last Titanium Prosthesis | ||
| Odat et al. (2021) | K-piston Titanium prosthesis/Titanium Soft-clip Piston | No statistically significant difference (ABG and average gain) between the prostheses. The success rate (ABG < 10 dB) was higher for the group with fluoroplastic prostheses. |
| Fluoroplastic Piston | ||
| Huber et al. (2014) | NiTiBOND Stapes Prosthesis | No statistically significant difference (ABG and average gain) between the prostheses. |
| SMart Nitinol Piston Prosthesis | ||
| Tange et al. (1998) | Golden Piston | No statistically significant difference (ABG and average gain) between the prostheses. The gold prosthesis is heavier and provides greater gain in the low and mid-frequency range, while the titanium one is lighter and offers greater gain in the high-frequency range. |
| K-piston Titanium prosthesis | ||
| Mangham CA et al (2008a). | The Schuknecht Teflon-wire Piston | 'The average ABG of the Wengen prosthesis is significantly greater than the average ABG of the Schuknecht prosthesis. The results of both the Wengen and Robinson prostheses are significantly worse compared to those of the Schuknecht prosthesis. Short-term efficacy is lower in the groups with Wengen and Robinson prostheses compared to the other prostheses. |
| De La Cruz Teflon-Platinum Wire Piston | ||
| Mangham Teflon-Platinum Double-fold Piston | ||
| CliP-piston a`Wengen Titanium Prosthesis | ||
| Teflon Robinson Piston | ||
| Potena et al. (2015) | Portmann Clip Piston Stainless Steel/Fluoroplastic | No statistically significant difference (ABG and average gain) between the prostheses. The average gain of the ABG is better in the group with steel and Teflon prostheses. |
| Titanium Soft-clip Piston | ||
| Schrotzlmair et al. | NiTiBOND Stapes Prosthesis | No statistically significant difference (ABG and average gain) between the prostheses. In approximately one-third of the patients in the Wengen prosthesis group, postoperative ABG was better compared to the groups with Nitinol and titanium prostheses (Wengen), where only 5% and 10%, respectively, showed ABG closure but not sufficient. |
| K-piston Titanium Prosthesis | ||
| CliP-piston a`Wengen Titanium Prosthesis | ||
| Harris and Gong (2007) | SMart Nitinol Piston Prosthesis | No statistically significant difference (ABG and average gain) between the prostheses. |
| Richards-Gyrus Conventional Stainless Steel/Platinum Ribbon Teflon Piston Prosthesis | ||
| Mangham CA (2008b) | Platinum Teflon Double-loop Piston (0,5 mm) |
The average ABG for the 0.6 mm Teflon piston is significantly smaller compared to the 0.6 mm Titanium piston and the 0.5 mm Teflon piston at both 2 months and 1 year post-surgery. The ABG for the 0.6 mm Teflon piston is significantly smaller at 500 Hz, with a trend towards a smaller ABG at 4000 Hz. The average ABG for the Titanium piston in a small window is significantly lower than that observed when the window is larger. The Titanium piston appears to provide significantly worse results compared to the Teflon piston at both 2 months and 1 year post-surgery. |
| Platinum Teflon Double-loop Piston (0,6 mm) | ||
| CliP-piston a`Wengen Titanium Prosthesis | ||
| Rajan et al. (2005) | Nitinol Stapes Piston Prosthesis | No statistically significant difference (ABG and average gain) between the prostheses. The average postoperative reduction in conductive hearing loss is better in the Nitinol prosthesis group, but not significant. However, the interindividual variation in postoperative reduction of conductive hearing loss is significantly lower in the Nitinol prosthesis group. |
| Titanium Prosthesis |
4. Discussion
The present study aimed to evaluate the outcomes of stapedotomy procedures using two different prostheses in patients diagnosed with clinical and audiological otosclerosis. The prospective study design allowed for a comprehensive assessment of pre- and postoperative audiometric data, clinical characteristics, and complications. Both prosthetic groups (G1 and G2) showed no significant differences in clinical characteristics, ensuring a balanced comparison. While the majority had no history of previous surgical interventions in the ENT districts, some reported familial hearing loss, and a subset had undergone stapedotomy in the contralateral ear. No significant complications were observed during or after surgery, with a small incidence of tympanic membrane perforations and damage of the chorda tympani.
Postoperative follow-ups demonstrated overall satisfactory auditory results for both prostheses. A significant gain in bone and air conduction thresholds, as well as the closure of the air-bone gap (ABG), indicated the effectiveness of the prostheses in improving hearing thresholds. Notably, both groups achieved a high percentage of patients with an average ABG below 20 dB, reflecting successful outcomes in terms of auditory function restoration.
Comparing the two prostheses, our study did not reveal statistically significant differences in terms of ABG closure and average hearing gain. However, specific frequency analysis demonstrated nuances, such as G1 recording a significantly worse preoperative mean for bone conduction compared to G2. Conversely, G1 exhibited better air conduction gain at the frequency of 250 Hz.
The systematic review demonstrates that the prostheses used in various surgical contexts are all effective in improving the patient's auditory performance and enabling a normal reintroduction into social life. However, none of the authors highlighted significant differences in terms of auditory outcomes among the prostheses under examination. The analysis of comparative studies by various authors indicates the inherent challenge of establishing the ideal prosthesis characteristics, given the multitude of variables involvedGjuric and Rukavina, 2007; Sevy and Arriaga, 2018]. The choice of material is the most crucial factor in selecting a prosthesis.
Today, a variety of materials are utilized, often combining multiple materials within the same prosthesis. Common materials for stapes surgery include Teflon, stainless steel, tantalum, platinum, and gold. The original stapedectomy, devised by Shea (1958), entailed the complete removal of the stapes, followed by the placement of a venous graft and a Teflon (polyethylene) pillar—a novel biocompatible material at the time. Following the initial use of Teflon prostheses, various other types were explored [Shea, 1958].
In 1960, Schuknecht introduced a prosthesis crafted from adipose tissue on a steel wire, which gained widespread acceptance. This prosthesis featured a ring at the end, resting on the fragments of the fractured stapes to reconstruct the sound-conducting mechanism of the middle ear [Schuknecht, 1960]. House later employed a wire to connect the stapes to a Gelfoam fragment or an adipose tissue graft [House, 1962].
With the emergence and popularity of stapedotomy, Teflon and steel began to be combined in the construction of prostheses. Fish's prosthesis, for instance, comprised a Teflon piston and a steel fixation ring on the incus, initially in the form of a wire and later as a band [Fisch, 1994].
For many years, steel was the most widely used material in the construction of prostheses. However, being a ferromagnetic material, a specific type of stainless steel must be utilized when implanting a device in the middle ear. Series 300 steel is preferred over Series 400 because, when exposed to a magnetic field, it does not display any movement, making it suitable for magnetic resonance imaging. This brings us to the present day, with the emergence of titanium, a promising material renowned for its biocompatibility and its lightweight, easily manipulable nature, rendering it the primary component in modern prosthetics [Fritsch, 2007]. The studies included in our review compared prosthetics made from various materials.
It is evident that titanium currently stands as the most widely used material in stapes prostheses. Almost half of the analyzed studies describe the use of prostheses made solely from titanium (46.34%), followed by Teflon (17.07%) and Nitinol (14.64%). The cost-benefit ratio of titanium, along with its lightness, extreme malleability, and the ability to remain stationary in magnetic fields, makes it the ideal material for this type of prosthetics.
The attachment of the prosthesis to the incus is an extremely delicate surgical step, and in some ways, it significantly influences a substantial portion of the auditory outcomes of the surgical procedure. The introduction of titanium-gold prostheses with automatic clips provides a secure fixation to the incus [Wengen, 2000]. This prevents potential damage resulting from manually crimping the prosthesis band. Excessive pressure can lead to incus necrosis due to reduced blood flow. Conversely, too weak crimping can cause abnormal vibrations of the incus generated by the ring, allowing it too much freedom of movement and eventually leading to erosion of the crus longum. Due to these technical challenges, Knox and Reitan (2005) introduced self-crimping prostheses made of Teflon and Nitinol (a nickel-titanium alloy with 45% nickel and 55% titanium) in 2005. This material has the property of conforming to a pre-set configuration when exposed to heat. The use of this new material allows for a more reliable and effective positioning of the prosthesis on the incus [Knox and Reitan, 2005]. However, there remains a risk of causing thermal damage due to heat activation or possible allergic reactions to nickel [Van Rompaey et al., 2015].
The dimensions of a prosthesis significantly influence the success of the surgical intervention. The length of the piston is chosen by the surgeon based on the distance between the platina and the medial face of the crus longum of the incus. A prosthesis that is too long can sink into the vestibule, irreversibly damaging the membranous labyrinth, while one that is too short, besides not efficiently transmitting sound pressure to the internal fluids and not being in its correct position in the oval window, can generate abnormal movements of the incus leading to erosion and the need for revision [Immordino et al., 2023]. The diameter is the variable that most affects the auditory outcome of a prosthesis. There are no significant differences in auditory outcomes during stapedectomy [Michael et al., 1998]. Opinions on auditory outcomes after stapedotomy are, however, contrasting. Wegner et al. (2016) evaluated the speed movement of the stapes and the membrane of the round window on a cadaver in relation to the diameter of the prostheses and platinotomy. The authors concluded that, in the range of mid frequencies (500-4000 Hz), the speed of the round window increased from 2 dB to 3 dB with a 0.6 mm prosthesis compared to a 0.4 mm one [Wegner et al, 2016]. Other studies claim that a 0.4 mm prosthesis might improve gains in frequencies above 4 kHz, while a 0.6 mm one could generate overall better auditory outcomes in all frequencies, even in reducing postoperative ABG and auditory gain [Laske et al., 2011;Bernardeschi et al., 2018]. Others still do not believe that a specific diameter can guarantee a better recovery of auditory capacity [Wegner et al., 2014].
5. Conclusions
In conclusion, our prospective study provides valuable insights into the outcomes of stapedotomy procedures using the MatriX and mAXIS prostheses. Both prostheses demonstrated effectiveness in improving hearing thresholds, with no significant differences in overall auditory outcomes. Instead, it is the surgeon's skills and experience with a specific prosthesis and a precise surgical technique that determine the postoperative auditory success. Modern materials and technical innovations now allow for a safer approach to the pathology for the surgeon and, most importantly, for the patient, who undergoes a quick surgical procedure, standardized in operative times, and almost entirely devoid of severe complications. In our ENT Department, we have chosen to use Titanium prostheses for many years, given the numerous advantages of this material that, in terms of auditory results, justify the cost of this type of prosthesis [Immordino et al., 2022 Immordino et al., 2023]. The choice of the new mAXIS prosthesis is essentially related to its lower cost compared to the one we used previously. The choice of this prosthesis type, in comparison to others available on the market, is also influenced by technical factors that impact intraoperative skill and surgical success. The wider band loop helps reduce pressure on the incus, ensuring a gentler crimping, which may contribute to preventing potential damage to the incus. The wider band loop also provides intraoperative flexibility, thanks to a clear view of the stapes. Furthermore, the flexible shaft, the smooth transition between the piston and the shaft, and the even weight distribution make it stable and extremely easy to handle.
Despite all the promising results obtained, our study has limitations. The relatively small sample size and the absence of long-term data beyond one year may limit the generalizability of our findings. Additionally, further investigations could explore subjective patient-reported outcomes, adding a qualitative dimension to the assessment.
Acknowledgments
Conflicts of Interest
The authors declare no conflict of interest.
Data Availability Statement
Not applicable.
Ethics Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of our University Hospital Policlinico “Paolo Giaccone” of Palermo (11-22042024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Funding Statement
This research received no external funding.
References
- Bernardeschi, D. , De Seta, D. , Canu, G. , et al. , 2018. Does the diameter of the stapes prosthesis really matter? A prospective clinical study. Laryngoscope 128(8), 1922–1926. 10.1002/lary.27021 [DOI] [PubMed] [Google Scholar]
- Canu, G. , Lauretani, F. , Russo, F.Y. , et al. , 2017. Early functional results using the nitibond prosthesis in stapes surgery. Acta Oto-Laryngol. 137(3), 259–264. 10.1080/00016489.2016.1247499 [DOI] [PubMed] [Google Scholar]
- Declau, F. , Van Spaendonck, M. , Timmermans, J.P. , et al. , 2001. Prevalence of otosclerosis in an unselected series of temporal bones. Otol. Neurotol. 22(5), 596–602. 10.1097/00129492-200109000-00006 [DOI] [PubMed] [Google Scholar]
- Dispenza, F. , Cappello, F. , Kulamarva, G. , et al. , 2013. The discovery of stapes. Acta Otorhinolaryngol. Ital. 33(5), 357–359. [PMC free article] [PubMed] [Google Scholar]
- Ealy, M. , Smith, R.J.H. , 2011. Otosclerosis. Adv. Otorhinolaryngol. 70, 122–129. [DOI] [PubMed] [Google Scholar]
- Faramarzi, M. , Gilanifar, N. , Roosta, S. , 2017. Comparison of fluoroplastic Causse loop piston and titanium soft-clip in stapedotomy. Iran. J. Otorhinolaryngol. 29(1), 23–28. [PMC free article] [PubMed] [Google Scholar]
- Faramarzi, M. , Roosta, S. , Daneshian, N. , 2020. Comparison between fluoroplastic and platinum/titanium piston in stapedotomy: A prospective, randomized clinical study. J. Int. Adv. Otol. 16(2), 234–240. 10.5152/iao.2020.5129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faramarzi, M. , Pedramfard, P. , Roosta, S. , et al. , 2021. Evaluating hearing results in stapedotomy: Comparison of fluoroplastic Causse loop piston and matrix prosthesis. Laryngoscope Investig. Otolaryngol. 6(6), 1289–1295. 10.1002/lio2.675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisch, U., Tympanoplasty, Mastoidectomy, and Stapes Surgery. Stuttgart (DE), Thieme Publishing Group, 1994. [Google Scholar]
- Fritsch, M.H. , 2007. MRI scanners and the stapes prosthesis. Otol. Neurotol. 28(6), 733–738. 10.1097/MAO.0b013e318125652a [DOI] [PubMed] [Google Scholar]
- Fritsch, M.H. , Naumann, I.C. , 2008. Phylogeny of the stapes prosthesis. Otol. Neurotol. 29(3), 407–415. 10.1097/MAO.0b013e3181690775 [DOI] [PubMed] [Google Scholar]
- Fucci, M.J. , Lippy, W.H. , Schuring, A.G. , et al. , 1998. Prosthesis size in stapedectomy. Otolaryngol.-Head Neck Surg. 118(1), 1–5. 10.1016/S0194-5998(98)70366-3 [DOI] [PubMed] [Google Scholar]
- Gjuric, M. , Rukavina, L. , 2007. Evolution of stapedectomy prostheses over time. Adv. Otorhinolaryngol. 65, 174–178. [DOI] [PubMed] [Google Scholar]
- Hall, J.G. , 1974. Otosclerosis in Norway, a geographical and genetical study. Acta Otolaryngol. 324, 1–20. [PubMed] [Google Scholar]
- Harris, J.P. , Gong, S.S. , 2007. Comparison of hearing results of nitinol SMART stapes piston prosthesis with conventional piston prostheses: Postoperative results of nitinol stapes prosthesis. Otol. Neurotol. 28(5), 692–695. 10.1097/MAO.0b013e3180340a1d [DOI] [PubMed] [Google Scholar]
- Hornung, J.A. , Brase, C. , Bozzato, A. , et al. , 2009. First experience with a new titanium clip stapes prosthesis and a comparison with the earlier model used in stapes surgery. Laryngoscope 119(12), 2421–2427. 10.1002/lary.20641 [DOI] [PubMed] [Google Scholar]
- House, H.P. , 1962. The prefabricated wire loop-Gelfoam: Stapedectomy. Arch. Otolaryngol. 76(4), 298–302. 10.1001/archotol.1962.00740050308004 [DOI] [PubMed] [Google Scholar]
- Huber, A.M. , Hornung, J. , Plontke, S. , et al. , 2014. NiTiBOND, eine optimierte Steigbügelprothese zur chirurgischen Behandlung der Otosklerose. Laryngorhinootologie 93(3), 178–185. [DOI] [PubMed] [Google Scholar]
- Immordino, A. , Sireci, F. , Lorusso, F. , et al. , 2022. The role of cartilage-perichondrium tympanoplasty in the treatment of tympanic membrane retractions: Systematic review of the literature. Int. Arch. Otorhinolaryngol. 26(3), e499–e504. 10.1055/s-0042-1742349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Immordino, A. , Lorusso, F. , Sireci, F. , et al. , 2023a. Acute pneumolabyrinth: A rare complication after cochlear implantation in a patient with obstructive sleep apnoea on CPAP therapy. BMJ Case Rep. 16(6), e254069. 10.1136/bcr-2022-254069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Immordino, A. , Salvago, P. , Sireci, F. , et al. , 2023b. Mastoidectomy in surgical procedures to treat retraction pockets: A single-center experience and review of the literature. Eur. Arch. Oto-Rhino-Laryngol. 280(3), 1081–1087. 10.1007/s00405-022-07573-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox, G.W. , Reitan, H. , 2005. Shape-memory stapes prosthesis for otosclerosis surgery. Laryngoscope 115(8), 1340–1346. 10.1097/01.mlg.0000172274.73365.11 [DOI] [PubMed] [Google Scholar]
- Laske, R.D. , Roosli, C. , Chatzimichalis, M.V. , et al. , 2011. The influence of prosthesis diameter in stapes surgery: A meta-analysis and systematic review of the literature. Otol. Neurotol. 32(4), 520–528. 10.1097/MAO.0b013e318216795b [DOI] [PubMed] [Google Scholar]
- Mangham, C.A.Jr. , Neel, J. , Mangham, H.F. , 2008a. Success of five stapes prostheses evaluated by Kaplan-Meier product-survival procedure. Otol. Neurotol. 29(7), 900–904. 10.1097/MAO.0b013e318185faf4 [DOI] [PubMed] [Google Scholar]
- Mangham, C.A.Jr. , 2008b. Titanium CliP piston versus platinum-ribbon Teflon piston: Piston and fenestra size affect air-bone gap. Otol. Neurotol. 29(1), 8–12. 10.1097/mao.0b013e31815c2575 [DOI] [PubMed] [Google Scholar]
- Odat, H. , Kanaan, Y. , Alali, M. , et al. , 2021. Hearing results after stapedotomy for otosclerosis: Comparison of prosthesis variables. J. Laryngol. Otol. 135(1), 28–32. 10.1017/S0022215120002595 [DOI] [PubMed] [Google Scholar]
- Pearson, R.D. , Kurland, L.T. , Cody, D.T. , 1974. Incidence of diagnosed clinical otosclerosis. Arch. Otolaryngol. 99(4), 288–291. 10.1001/archotol.1974.00780030298013 [DOI] [PubMed] [Google Scholar]
- Pollarolo, M. , Immordino, A. , Immordino, P. , et al. , 2022. Noise-induced hearing loss in police officers: Systematic review. Iran. J. Otorhinolaryngol. 34(124), 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potena, M. , Portmann, D. , Guindi, S. , 2015. Audiological comparison between two different clips prostheses in stapes surgery. Rev. Laryngol. Otol. Rhinol. 136(1), 33–36. [PubMed] [Google Scholar]
- Priola, R. , Sireci, F. , Lorusso, F. , et al. , 2021. Complex forms of benign paroxysmal positional vertigo. In: Dizziness: Prevalence, Risk Factors and Management. Martines, F., Salvago, P. Eds. New York: Nova Science Publishers, pp. 117–149. [Google Scholar]
- Rajan, G.P. , Eikelboom, R.H. , Anandacoomaraswamy, K.S. , et al. , 2005. In vivo performance of the Nitinol shape-memory stapes prosthesis during hearing restoration surgery in otosclerosis: A first report. J. Biomed. Mater. Res. B: Appl. Biomater. 72(2), 305–309. [DOI] [PubMed] [Google Scholar]
- Rudic, M. , Keogh, I. , Wagner, R. , et al. , 2015. The pathophysiology of otosclerosis: Review of current research. Hear Res. 330, 51–56. 10.1016/j.heares.2015.07.014 [DOI] [PubMed] [Google Scholar]
- Schrötzlmair, F. , Suchan, F. , Kisser, U. , et al. , 2013. Promising clinical results of an innovative self-crimping stapes prosthesis in otosclerosis surgery. Otol Neurotol. 34(9), 1571–1575. 10.1097/MAO.0b013e3182a5d12d [DOI] [PubMed] [Google Scholar]
- Schuknecht, H.F. , 1960. Stapedectomy and graft-prosthesis operation. Acta Otolaryngol. 51(3/4), 241–243. [DOI] [PubMed] [Google Scholar]
- Sevy, A. , Arriaga, M. , 2018. The stapes prosthesis: Past, present, and future. Otolaryngol. Clin. North Am. 51(2), 393–404. 10.1016/j.otc.2017.11.010 [DOI] [PubMed] [Google Scholar]
- Shea, J.J.Jr. , 1958. Fenestration of the oval window. Ann. Otol. Rhinol. Laryngol. 67(4), 932–951. 10.1177/000348945806700403 [DOI] [PubMed] [Google Scholar]
- Tange, R.A. , de Bruijn, A.J. , Grolman, W. , 1998. Experience with a new pure gold piston in stapedotomy for cases of otosclerosis. Auris Nasus Larynx 25(3), 249–253. 10.1016/S0385-8146(98)00008-X [DOI] [PubMed] [Google Scholar]
- Tange, R.A. , Grolman, W. , 2008. An analysis of the air-bone gap closure obtained by a crimping and a non-crimping titanium stapes prosthesis in otosclerosis. Auris Nasus Larynx 35(2), 181–184. 10.1016/j.anl.2007.04.007 [DOI] [PubMed] [Google Scholar]
- Thomas, J.P. , Minovi, A. , Dazert, S. , 2011. Current aspects of etiology, diagnosis and therapy of otosclerosis. Otolaryngol. Pol. 65(3), 162–170. 10.1016/S0030-6657(11)70670-9 [DOI] [PubMed] [Google Scholar]
- Van Rompaey, V. , Claes, G. , Potvin, J. , et al. , 2011. Systematic review of the literature on nitinol prostheses in surgery for otosclerosis: Assessment of the adequacy of statistical power. Otol. Neurotol. 32(3), 357–366. 10.1097/MAO.0b013e31820e7874 [DOI] [PubMed] [Google Scholar]
- Wegner, I. , Kamalski, D.M.A. , Tange, R.A. , et al. , 2014. Laser versus conventional fenestration in stapedotomy for otosclerosis: A systematic review. Laryngoscope 124(7), 1687–1693. 10.1002/lary.24514 [DOI] [PubMed] [Google Scholar]
- Wegner, I. , Eldaebes, M.M.A.S. , Landry, T.G. , et al. , 2016. The effect of piston diameter in stapedotomy for otosclerosis: A temporal bone model. Otol. Neurotol. 37(10), 1497–1502. 10.1097/MAO.0000000000001212 [DOI] [PubMed] [Google Scholar]
- Wengen, D.F. , 2000. Eine neue selbsthaltende Titan-Gold-Stapesprothese. Schweiz Med Wochenschr Suppl 116, 83S–86S. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.