Abstract
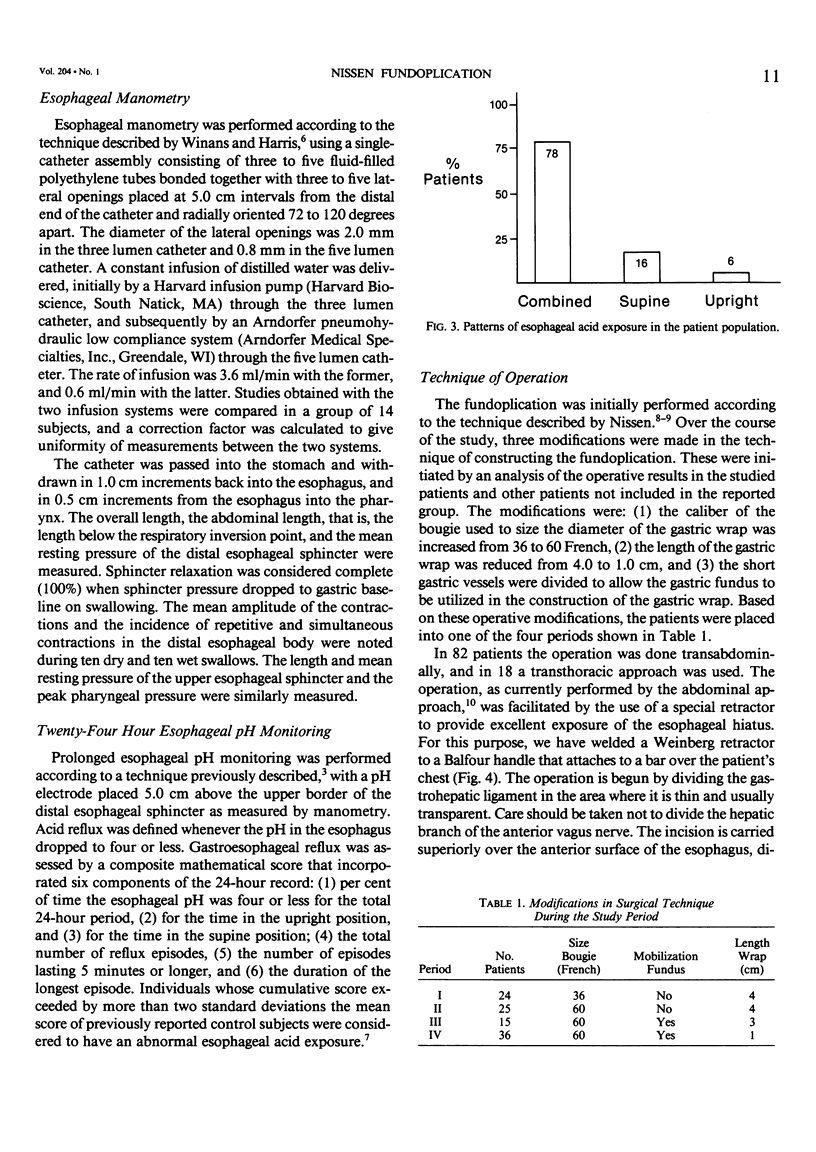
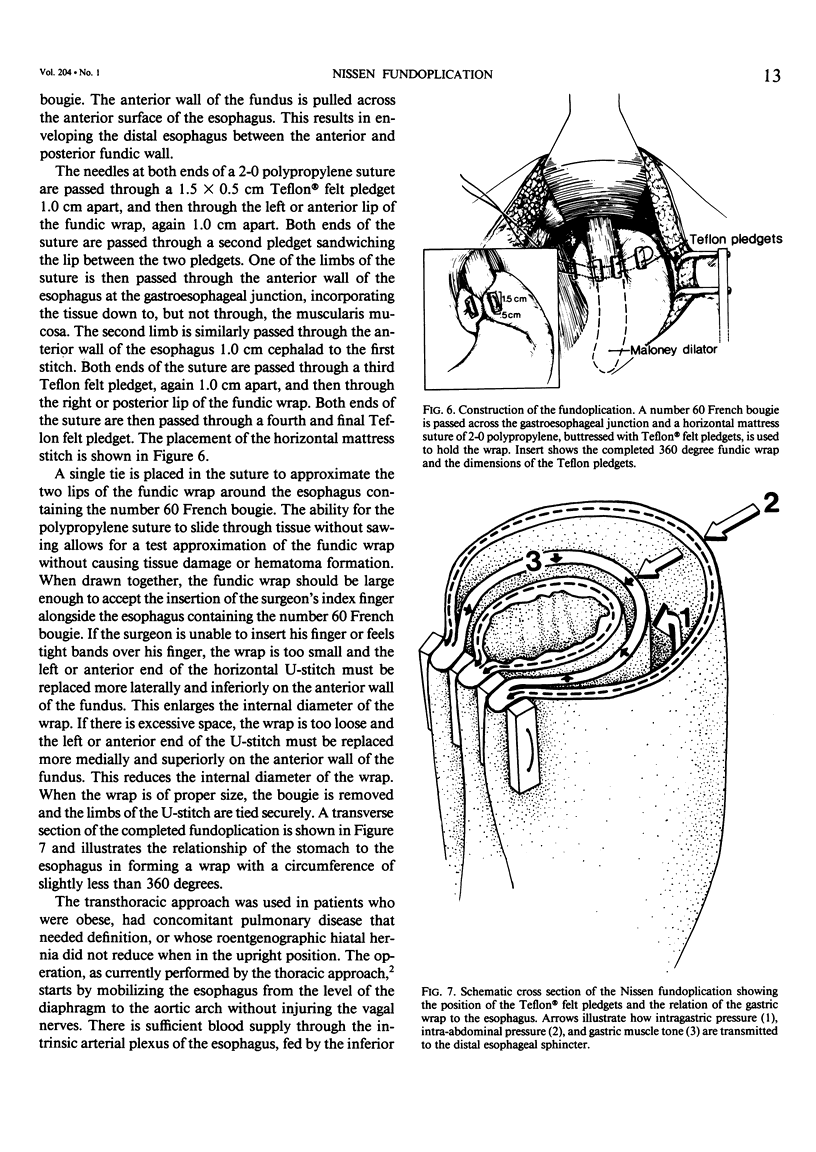
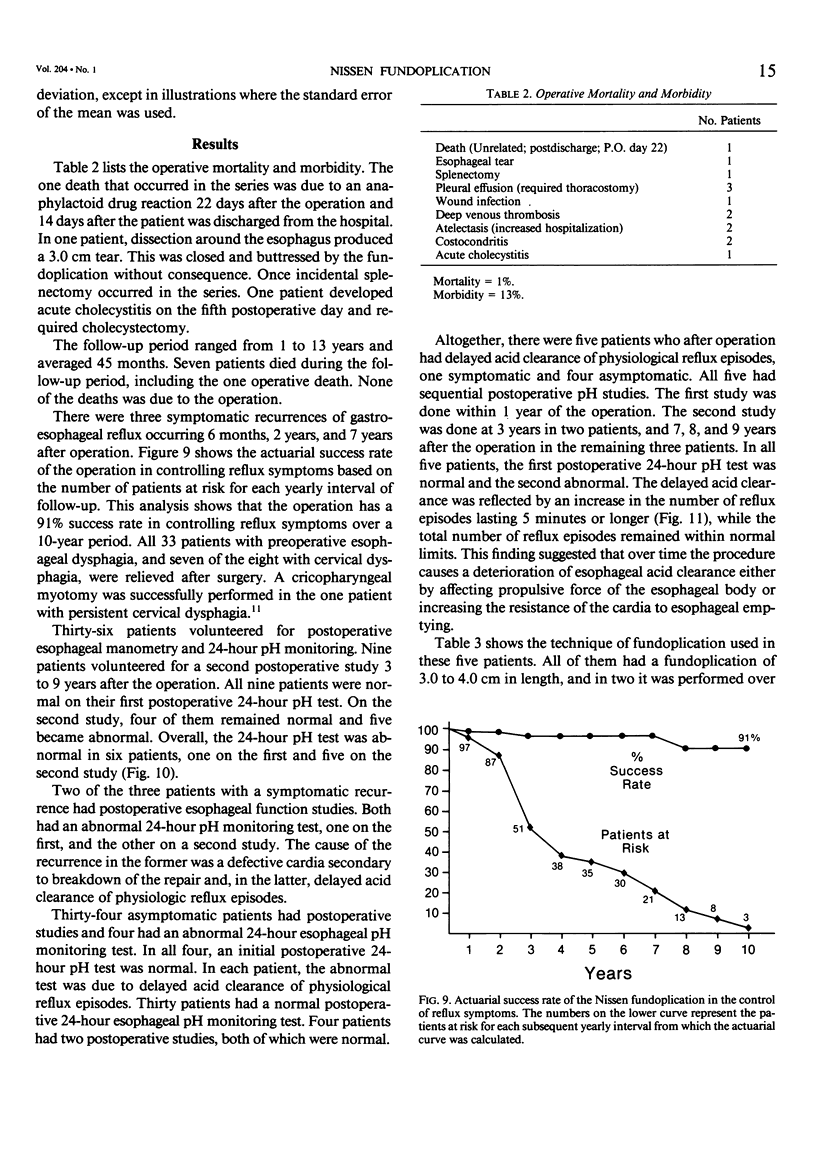
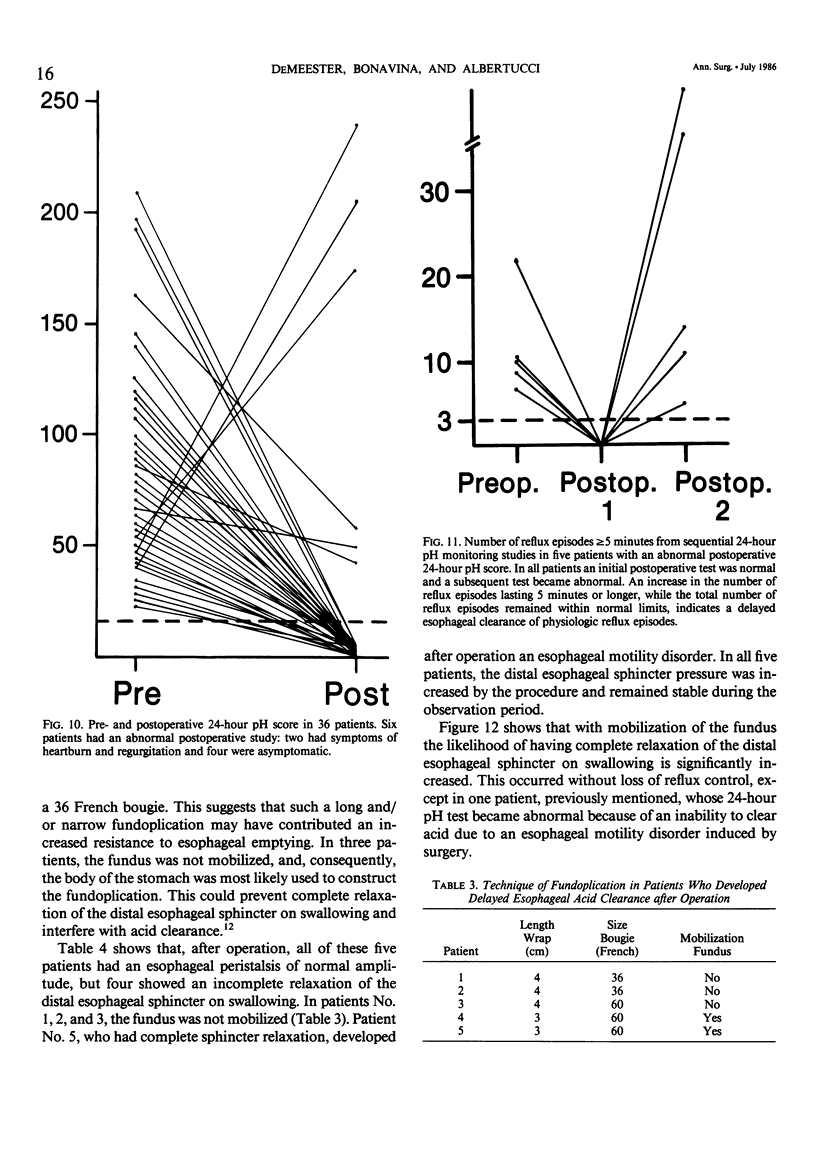
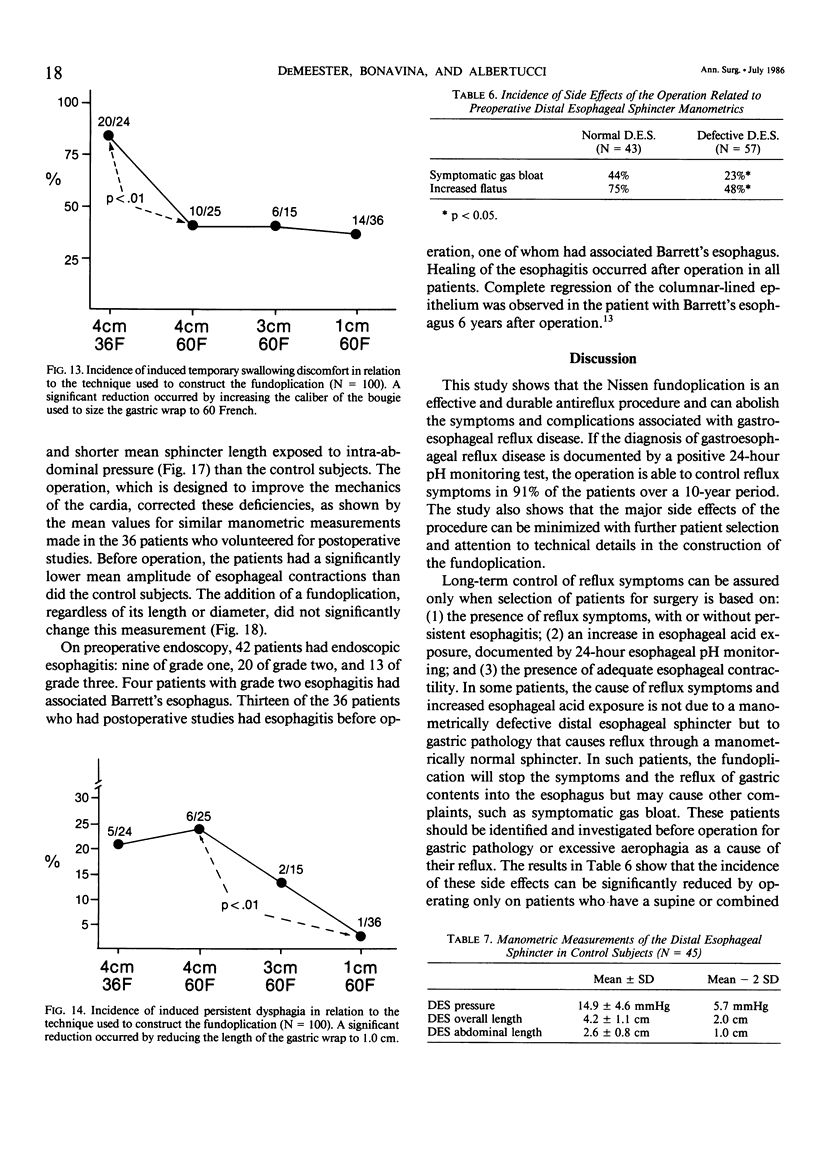
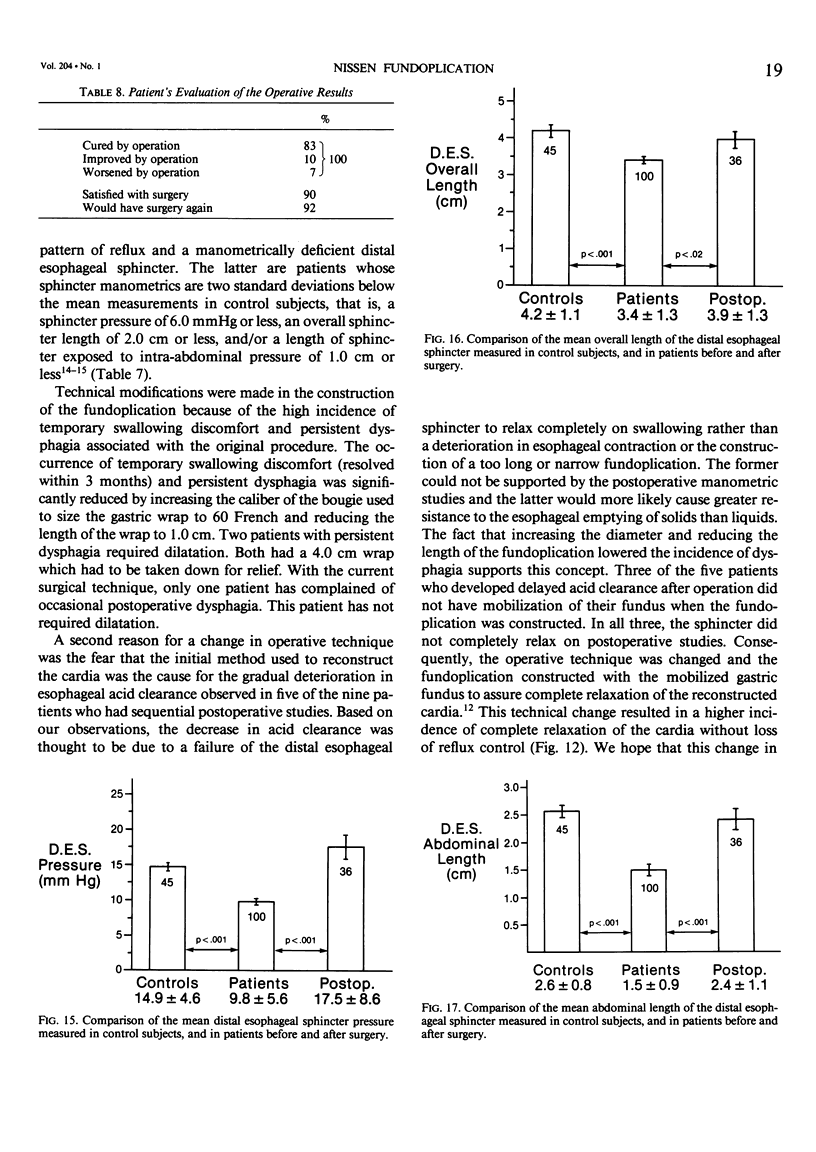
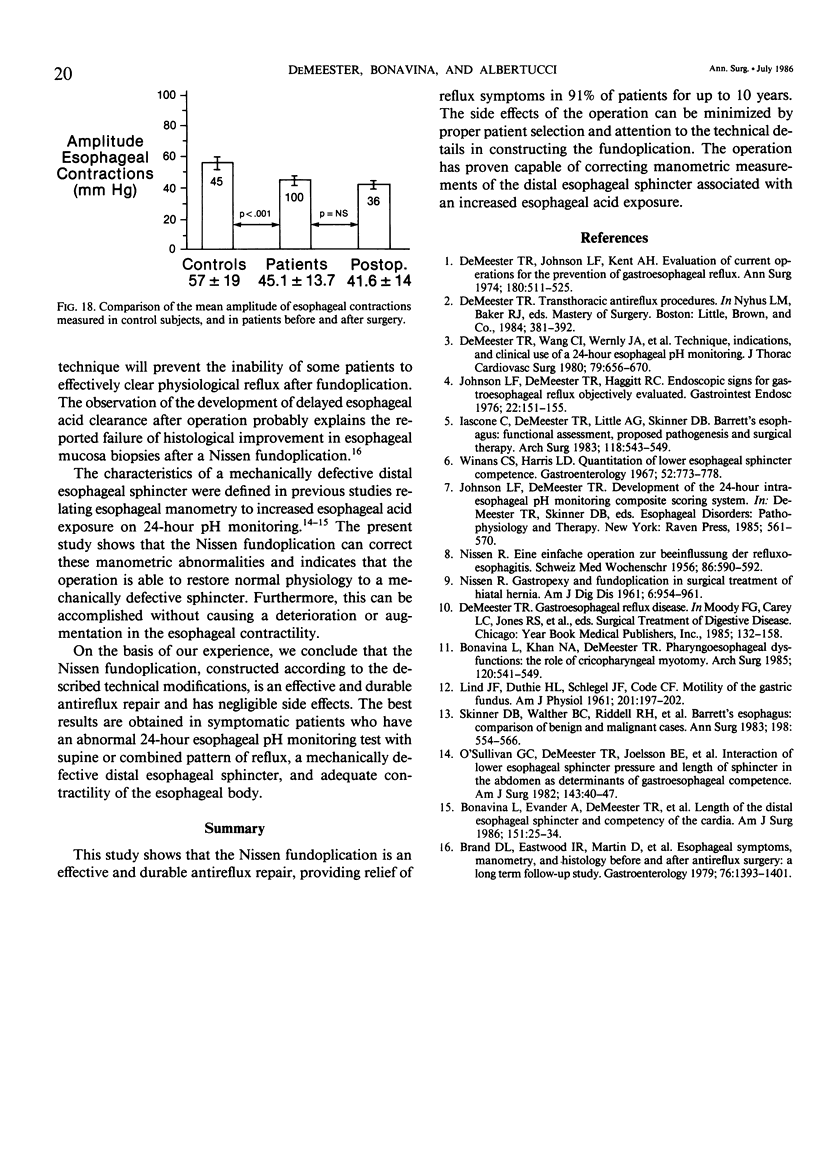
One hundred consecutive patients had a primary Nissen fundoplication for gastroesophageal reflux disease. None of the patients had previous gastric or esophageal surgery or evidence of esophageal stricture or motility disorder. The primary symptom was persistent heartburn in 89 patients and aspiration in 11. An abnormal pattern of esophageal acid exposure was documented in all patients with 24-hour esophageal pH monitoring. By actuarial analysis, the operation was 91% effective in the control of reflux symptoms over a 10-year period. The incidence of postoperative symptomatic gas bloat and increased flatus was lower in patients with preoperative abnormal manometric measurements of the distal esophageal sphincter (p less than 0.05). Three modifications in operative technique were made during the course of the study to minimize the side effects of the operation. First, enlarging the caliber of the bougie to size the fundoplication reduced the incidence of temporary swallowing discomfort from 83 to 39% (p less than 0.01). Second, shortening the length of the fundoplication decreased the incidence of persistent dysphagia from 21 to 3% (p less than 0.01). Third, mobilizing the gastric fundus for construction of the fundoplication increased the incidence of complete distal esophageal sphincter relaxation on swallowing from 31 to 71% (p less than 0.05). This was done to prevent the delayed esophageal acid clearance secondary to incomplete sphincter relaxation observed after operation in five of 36 studied patients. It is concluded that by proper patient selection and the incorporation of the above surgical techniques, the Nissen fundoplication can re-establish a competent cardia and provide relief of reflux symptoms with minimal side effects.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bonavina L., Evander A., DeMeester T. R., Walther B., Cheng S. C., Palazzo L., Concannon J. L. Length of the distal esophageal sphincter and competency of the cardia. Am J Surg. 1986 Jan;151(1):25–34. doi: 10.1016/0002-9610(86)90007-3. [DOI] [PubMed] [Google Scholar]
- Bonavina L., Khan N. A., DeMeester T. R. Pharyngoesophageal dysfunctions. The role of cricopharyngeal myotomy. Arch Surg. 1985 May;120(5):541–549. doi: 10.1001/archsurg.1985.01390290023004. [DOI] [PubMed] [Google Scholar]
- Brand D. L., Eastwood I. R., Martin D., Carter W. B., Pope C. E., 2nd Esophageal symptoms, manometry, and histology before and after antireflux surgery: a long-term follow-up study. Gastroenterology. 1979 Jun;76(6):1393–1401. [PubMed] [Google Scholar]
- DeMeester T. R., Wang C. I., Wernly J. A., Pellegrini C. A., Little A. G., Klementschitsch P., Bermudez G., Johnson L. F., Skinner D. B. Technique, indications, and clinical use of 24 hour esophageal pH monitoring. J Thorac Cardiovasc Surg. 1980 May;79(5):656–670. [PubMed] [Google Scholar]
- Demeester T. R., Johnson L. F., Kent A. H. Evaluation of current operations for the prevention of gastroesophageal reflux. Ann Surg. 1974 Oct;180(4):511–525. doi: 10.1097/00000658-197410000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iascone C., DeMeester T. R., Little A. G., Skinner D. B. Barrett's esophagus. Functional assessment, proposed pathogenesis, and surgical therapy. Arch Surg. 1983 May;118(5):543–549. doi: 10.1001/archsurg.1983.01390050027005. [DOI] [PubMed] [Google Scholar]
- Johnson L. F., DeMeester T. R., Haggitt R. C. Endoscopic signs for gastroesophageal reflux objectively evaluated. Gastrointest Endosc. 1976 Feb;22(3):151–155. doi: 10.1016/s0016-5107(76)73731-3. [DOI] [PubMed] [Google Scholar]
- LIND J. F., DUTHIE H. L., SCHLEGEL J. F., CODE C. F. Motility of the gastric fundus. Am J Physiol. 1961 Jul;201:197–202. doi: 10.1152/ajplegacy.1961.201.1.197. [DOI] [PubMed] [Google Scholar]
- NISSEN R. Eine einfache Operation zur Beeinflussung der Refluxoesophagitis. Schweiz Med Wochenschr. 1956 May 18;86(Suppl 20):590–592. [PubMed] [Google Scholar]
- NISSEN R. Gastropexy and "fundoplication" in surgical treatment of hiatal hernia. Am J Dig Dis. 1961 Oct;6:954–961. doi: 10.1007/BF02231426. [DOI] [PubMed] [Google Scholar]
- O'Sullivan G. C., DeMeester T. R., Joelsson B. E., Smith R. B., Blough R. R., Johnson L. F., Skinner D. B. Interaction of lower esophageal sphincter pressure and length of sphincter in the abdomen as determinants of gastroesophageal competence. Am J Surg. 1982 Jan;143(1):40–47. doi: 10.1016/0002-9610(82)90127-1. [DOI] [PubMed] [Google Scholar]
- Skinner D. B., Walther B. C., Riddell R. H., Schmidt H., Iascone C., DeMeester T. R. Barrett's esophagus. Comparison of benign and malignant cases. Ann Surg. 1983 Oct;198(4):554–565. doi: 10.1097/00000658-198310000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winans C. S., Harris L. D. Quantitation of lower esophageal sphincter competence. Gastroenterology. 1967 May;52(5):773–778. [PubMed] [Google Scholar]


