Abstract
Mutations of the conserved residues of influenza virus neuraminidase (NA) that are associated with NA inhibitor (NAI) resistance decrease the sialidase activity and/or stability of the NA, thus compromising viral fitness. In fact, clinically derived NAI-resistant variants with different NA mutations have shown different transmissibilities in ferrets (M. L. Herlocher, R. Truscon, S. Elias, H. Yen, N. A. Roberts, S. E. Ohmit, and A. S. Monto, J. Infect. Dis. 190:1627-1630, 2004). Molecular characterization of mutant viruses that have a homogeneous genetic background is required to determine the effect of single mutations at conserved NA residues. We generated recombinant viruses containing either the wild-type NA (RG WT virus) or a single amino acid change at NA residue 119 (RG E119V-NA virus) or 292 (RG R292K-NA virus) in the A/Wuhan/359/95 (H3N2) influenza virus background by reverse genetics. Both mutants showed decreased sensitivity to oseltamivir carboxylate, and the RG R292K-NA virus showed cross-resistance to zanamivir. We also observed differences between the two mutants in NA enzymatic activity and thermostability. The R292K mutation caused greater reduction of sialidase activity and thermostability than the E119V mutation. The NA defect caused by the R292K mutation was associated with compromised growth and transmissibility, whereas the growth and transmissibility of the RG E119V-NA virus were comparable to those of RG WT virus. Our results suggest that NAI-resistant influenza virus variants may differ substantially in fitness and transmissibility, depending on different levels of NA functional loss.
Antiviral chemotherapy and vaccination are the only options for control of influenza virus infection. Vaccination targets the variable antigenic surface glycoproteins of the circulating strain, whereas antivirals target conserved components of the viral proteins (32, 34). The emergence of resistant variants is a concern with the use of any antiviral drug. Treatment with M2 ion channel blockers (amantadine, rimantadine) can cause emergence of fully pathogenic and transmissible resistant variants in at least 30% of individuals (12, 13). Resistant variants were found in a smaller proportion of patients (approximately 4% to 8% of children and <1% of adults) after treatment with neuraminidase (NA) inhibitors (NAIs) (oseltamivir, zanamivir) (23, 30). However, rigorous detection techniques identified resistant mutants in 9 of 50 (18%) Japanese children during treatment with oseltamivir (21). The fact that NAI-resistant variants often show compromised fitness (impaired growth in vitro and reduced infectivity and transmissibility in animal experiments) (3, 9, 19, 33) is generally considered another advantage of NAI treatment for influenza virus infection.
Two mechanisms of resistance to NAIs have been described, and the molecular determinants of NAI resistance have been mapped not only to NA but also to hemagglutinin (HA) (8, 24). However, mutations at conserved NA residues are reported to be more clinically relevant (25). NA mutations that confer NAI resistance reduce sialidase activity and/or stability (2, 7, 29, 33), but the in vitro replication kinetics of these variants do not always reflect their defective NA enzymatic activity; their replication efficiency may be comparable to that of the wild-type virus (9, 29) or may be compromised (19, 33) in cell culture. The presence of HA mutations that mask the NA defect and the lack of an optimal cell line may limit the characterization of the NAI-resistant variants in vitro (22, 24, 36).
Several studies in animal models have examined the infectivity of NAI-resistant viruses with mutations at the conserved NA residues. These viruses exhibited reduced virulence in mice and ferrets (3, 14, 19, 33). However, A/Wuhan/359/95-like (H3N2) virus with the E119V NA mutation was recently reported to be transmitted as efficiently as the wild-type virus in ferrets (15). This finding contrasted with previous observations that A/Sydney/5/97-like (H3N2) influenza virus with the R292K NA mutation was not transmissible under conditions in which the wild-type virus was efficiently transmitted (14) and that A/New Caledonia/20/99-like (H1N1) virus with the H274Y NA mutation required a challenge dose 100 times higher and was less transmissible than the wild-type virus (14). The possible transmissibility of some NAI-resistant mutants in mammals highlights the need for studies of the fitness of NAI-resistant variants that are not confounded by different virus strains and different infection doses. The use of a plasmid-based reverse genetics (RG) system to generate recombinant viruses with identical genetic backgrounds should allow valid comparisons between resistant viruses that carry different NA mutations.
To determine the effect of NA mutations on the level of NAI resistance, viral replication efficiency in vitro, and transmissibility in vivo, we used plasmid-based RG to generate recombinant viruses, each of which contained a single amino acid change at NA position 119 or 292, in the background of a contemporary human H3N2 influenza virus. We found that NAI-resistant influenza virus variants with different NA mutations may differ substantially in resistance, fitness, and transmissibility.
MATERIALS AND METHODS
Compounds.
The NA inhibitors oseltamivir carboxylate [GS4071; 4-N-acetyl-5-amino-3-(1-ethylpropoxy)-1-cyclohexane-1 carboxylic acid] was provided by Hoffmann-La Roche (Nutley, NJ). Zanamivir (GG167; 4-guanidino-Neu5Ac2en) was provided by the R. W. Johnson Pharmaceutical Research Institute (Raritan, NJ). The compounds were dissolved in distilled water, and aliquots were stored at −20°C until used.
Viruses and cells.
Wild-type A/Wuhan/359/95-like (H3N2) influenza virus (referred to hereafter as A/Wuhan/359/95 virus) and an oseltamivir-resistant variant of A/Wuhan/359/95 were provided by Hoffmann-La Roche. The viruses were isolated from the nasal swabs of a patient before and after treatment with oseltamivir in a clinical trial during the 1997-1998 season. Viruses were isolated in primary rhesus monkey kidney cell culture, followed by plaque purification and were passaged in Madin-Darby canine kidney (MDCK) cells.
MDCK and 293T human embryonic kidney cells were obtained from the American Type Culture Collection (Manassas, VA). Primary rhesus monkey kidney cells were obtained from Cambrex (East Rutherford, NJ). MDCK cells transfected with cDNA encoding human 2,6-sialyltransferase (MDCK-SIAT1 cells) were maintained as described previously (22).
Generation of A/Wuhan/359/95-like viruses by reverse genetics.
The full-length genomes of the wild-type and oseltamivir-resistant A/Wuhan/359/95 viruses passaged in vitro in our laboratory were amplified by reverse transcription-PCR (18), and their sequences were determined by the DNA Sequencing Core at the University of Michigan and by the Hartwell Center at St. Jude Children's Research Hospital. As reported previously, the wild type and the resistant variant differed by one amino acid in the NA (E119V) (4). The wild-type virus was used as the backbone of recombinant viruses generated for this study. Eight plasmids were constructed, each containing the cDNA of one of the eight gene segments of the wild-type virus. A plasmid that contained the cDNA of the NA gene of the oseltamivir-resistant variant was also constructed as previously described (17). The R292K amino acid substitution was introduced into the wild-type NA plasmid as described previously (16). Constructed plasmids were sequenced to ensure that they were identical to the field strain.
Recombinant viruses that were identical, with the exception of the two introduced NA mutations, were generated by transfecting cocultivated 293T and MDCK cells with the wild-type NA plasmid (WT-NA), the oseltamivir-resistant variant NA plasmid that contained the E119V mutation (E119V-NA), or the NA plasmid with the introduced R292K mutation (R292K-NA). The recombinant viruses generated by reverse genetics were designated the RG WT, RG E119V-NA, and RG R292K-NA viruses. Stock viruses were prepared by one passage of the viruses rescued from 293T-MDCK coculture in MDCK cells, in minimal essential medium (MEM) supplemented with 0.3% bovine serum albumin (BSA) and 1 μg/ml l-(tosylamido-2-phenyl)ethyl chloromethyl ketone-treated trypsin (TPCK-trypsin). All eight segments of the stock viruses were sequenced.
Growth of the recombinant viruses.
Fifty percent tissue culture infective doses (TCID50) were determined in MDCK and MDCK-SIAT1 cells. The cells were infected with serial half-log dilutions of the recombinant viruses, incubated for 1 h at 37°C, washed, and overlaid with infection medium (MEM with 0.3% BSA and 1 μg/ml TPCK-trypsin for MDCK cells; Dulbecco's modified Eagle medium with 0.3% BSA and 1 μg/ml TPCK-trypsin for MDCK-SIAT1 cells). TCID50 were determined by hemagglutination assay after incubation for 3 days at 37°C. TCID50 of RG R292K-NA virus were also determined with the addition of 2 mU/ml Clostridium perfringens NA (Sigma, St. Louis, MO) to the infection medium. Fifty percent egg infective doses (EID50) were determined by injecting 100 μl of half-log serial dilutions of virus into the allantoic cavities of 10-day-old embryonated chicken eggs. After 48 h of incubation at 37°C, hemagglutination activity was assayed. TCID50 and EID50 were calculated by the Reed-Muench method (28).
Replication kinetics.
Single-step growth curves were determined for each of the recombinant viruses in both MDCK and MDCK-SIAT1 cells. Confluent cell monolayers were infected with viruses at a multiplicity of infection (MOI) of ∼2.2 PFU/cell. After incubation, the cells were washed with 0.9% aqueous NaCl solution (pH 2.2) to remove any free infectious virus particles and then washed twice with phosphate-buffered saline (PBS) to adjust the pH. Infection medium with or without 2 mU/ml C. perfringens NA was added to the wells. Supernatants were collected 2, 4, 6, 8, and 10 h postinfection and stored at −70°C for titration.
To determine multistep growth curves, MDCK and MDCK-SIAT1 cells were infected with viruses at an MOI of 0.01 PFU/cell. After incubation, the cells were washed and overlaid with infection medium with or without 2 mU/ml C. perfringens NA. Supernatants were collected 12, 24, 36, 48, 60, and 72 h postinfection and stored at −70°C for titration.
Plaque assay in MDCK cells.
Confluent MDCK cells were incubated for 1 h at 37°C with 10-fold serial dilutions of virus in 1 ml infection medium. The cells were then washed and overlaid with freshly prepared MEM containing 0.3% BSA, 0.9% Bacto agar, and 1 μg/ml TPCK-trypsin. The plaques were visualized after incubation at 37°C for 3 days by staining with 0.1% crystal violet solution containing 10% formaldehyde.
Concentration of viruses.
After infection of MDCK cells with recombinant viruses, the culture supernatants were clarified by centrifugation at 450 × g for 30 min. Virus particles were pelleted at 57,000 × g for 1.5 h at 4°C and purified by centrifugation through a continuous 20% to 70% sucrose gradient at 76,000 × g for 2.5 h at 4°C. Fractions containing virus particles were collected and centrifuged at 76,000 × g for 2.5 h at 4°C. Virus pellets were resuspended in STE buffer (0.05 M Tris-HCl, 0.01 M EDTA, 0.1 M NaCl), and aliquots were stored at −70°C.
NA activity and NA inhibition assays.
A modified fluorometric assay was used to determine the NA activity of the virus with the fluorogenic substrate 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA; Sigma) (10, 27). The fluorescence of the released 4-methylumbelliferone was measured in a Fluoroskan II (Labsystems, Helsinki, Finland) spectrophotometer using excitation and emission wavelengths of 355 and 460 nm, respectively. The quantity of NA protein was standardized by the amount of nucleoprotein in 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and staining the gel with SYPRO Ruby protein Gel Stain (Cambrex, Rockland, ME). Enzyme activity was expressed as the quantity of substrate (picomoles) converted during a 30-min incubation at 37°C. NA inhibition was assayed with viruses standardized to equivalent NA enzyme activity and incubated with oseltamivir or zanamivir at concentrations of 0.00005 to 10 μM (11). The drug concentrations required to inhibit 50% of the NA enzymatic activity (IC50) were determined by plotting the percent inhibition of NA activity as a function of the compound concentrations calculated from the dose-response curves.
Cell-based virus reduction assay.
Confluent MDCK and MDCK-SIAT1 cells were preincubated for 1 h with serial 10-fold dilutions of the NAIs (0.001 to 1000 μM), infected with 0.01 PFU/cell of virus, and incubated at 37°C. Virus replication was determined by assaying HA activity 3 days postinfection. The 50% effective concentrations (EC50) of compounds were determined by plotting the percent inhibition of viral replication as a function of the compound concentrations calculated from the dose-response curves.
Transmissibility in the ferret contact model.
The transmissibility of the RG WT, RG E119V-NA, and RG R292K-NA viruses was tested in nine seronegative female ferrets with comparable body weights (mean ± standard deviation [SD], 722.9 ± 27.1 g) that were bred at St. Jude Children's Research Hospital. In groups of three ferrets, one donor ferret and two recipient ferrets were randomly selected. The donor was housed separately from the recipients. Three donor ferrets were anesthetized with isoflurane, and each was inoculated with 1,000 TCID50 of the RG WT, RG E119V-NA, or RG R292K-NA virus in 0.5 ml sterile PBS. After donors were confirmed to shed virus by the Directigen Flu A+B quick test (BD, Franklin Lakes, NJ) of nasal wash fluid on day 2 postinoculation (p.i)., each was housed with two naive recipient ferrets. Clinical signs of infection (weight and temperature changes) were observed for 21 days. Nasal washes were collected daily from donors and recipients for 14 days, and TCID50 were determined in MDCK cells.
RESULTS
NA enzymatic activity and thermostability.
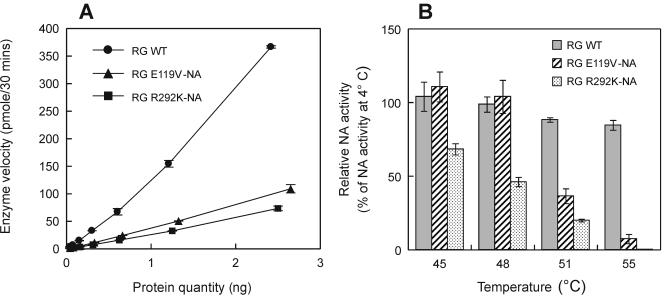
After generating viruses that had a single mutation at conserved NA residue 119 or 292 in a contemporary human influenza virus background, we characterized the effects of the mutations on NA enzymatic activity by comparing NA activities in standardized preparations of RG WT, RG E119V-NA, and RG R292K-NA viruses. Both mutants had significantly lower NA activity than did the RG WT virus (P < 0.01; t test); however, the R292K mutation had a greater effect on NA activity (P < 0.01; t test) (Fig. 1A).
FIG. 1.
NA enzymatic activity (A) and thermostability (B) of RG WT, RG E119V-NA, and RG R292K-NA A/Wuhan/359/95 influenza viruses. MUNANA was used as the substrate at a final concentration of 100 μM. The thermostability of NA in the recombinant viruses was determined after 15 min of incubation at the indicated temperatures. Residual NA enzymatic activity was assayed and is presented as a percentage of the NA activity at 4°C. Datum points represent the mean ± SD from three experiments.
To determine the thermostability of the mutant NAs, we measured the NA activities of the recombinant viruses after 15 min of incubation at different temperatures (Fig. 1B). The NA activity of the RG E119V-NA virus was stable at 4°C, 45°C, and 48°C but decreased dramatically at higher temperatures. By contrast, the NA activity of the RG R292K-NA virus was reduced at 45°C and decreased with increasing temperature above that point. Both mutants showed significantly lowered NA activity at or above 55°C, whereas the NA activity of the RG WT virus decreased only ∼10% between 4°C and 55°C (Fig. 1B). Thus, NA thermostability was greatest in virus with WT-NA, intermediate in virus with E119V-NA, and lowest in virus with R292K-NA.
Susceptibility to NAIs. (i) NA inhibition assays.
To compare the susceptibilities of the RG E119V-NA and RG R292K-NA viruses to NAIs, we performed NA inhibition assays with both oseltamivir carboxylate and zanamivir (Table 1). The concentration of oseltamivir carboxylate required to inhibit 50% of NA enzymatic activity was 209.0 nM for the RG E119V-NA virus, 0.8 nM for the RG WT virus, and ≥30,000 nM for the RG R292K-NA virus. Thus, virus with the R292K mutation was more resistant to oseltamivir carboxylate than virus with the E119V mutation. The IC50 of zanamivir were comparable for the RG WT and RG E119V-NA viruses (2.4 and 2.1 nM, respectively), but the IC50 of zanamivir was ≥13 times as high for the RG R292K-NA virus (31.5 nM). In summary, the RG R292K-NA virus showed resistance to both oseltamivir carboxylate and zanamivir, while the RG E119V-NA virus was resistant only to oseltamivir carboxylate.
TABLE 1.
Sensitivities of recombinant A/Wuhan/359/95 (H3N2) influenza viruses to NAIs
| Virus | NA inhibition assaya (nM, mean IC50 ± SD)
|
Virus reduction assayb (μM, mean EC50 ± SD)
|
||||
|---|---|---|---|---|---|---|
| Oseltamivir carboxylate | Zanamivir | MDCK
|
MDCK-SIATI
|
|||
| Oseltamivir carboxylate | Zanamivir | Oseltamivir carboxylate | Zanamivir | |||
| RG WT | 0.8 ± 0.1 | 2.4 ± 0.1 | 9.5 ± 0.6 | 55.3 ± 2.2 | 0.04 ± 0.01 | 0.06 ± 0.01 |
| RG E119V-NA | 209.0 ± 6.8 | 2.1 ± 0.1 | 93.5 ± 9.2 | 49.6 ± 8.3 | 0.43 ± 0.18 | 0.05 ± 0.02 |
| RG R292K-NA | >30,000 | 31.5 ± 9.3 | 810 ± 88 | 32.7 ± 4.5 | —c | — |
NA inhibition assays were done with MUNANA as the substrate at a final concentration of 100 μM. Values were obtained from three independent determinations.
The assay was performed with MDCK or MDCK-SIAT1 cells infected with virus at an MOI of 0.01 PFU/cell. Values were obtained from triplicate wells in two independent experiments.
—, not applicable. The RG R292K-NA virus showed a severe growth defect in MDCK-SIAT1 cells both in the absence and in the presence of NAIs.
(ii) Virus reduction assay in MDCK and MDCK-SIAT1 cells.
The sensitivities of the RG WT, RG E119V-NA, and RG R292K-NA viruses to NAIs were assayed in both MDCK and MDCK-SIAT1 cells; the latter are more sensitive for assays of NAI resistance (22). In MDCK cells, the sensitivity of the RG E119V-NA virus to oseltamivir carboxylate was approximately 1/10 of that of the RG WT virus while the sensitivity of the RG R292K-NA virus was decreased by a factor of ∼80 (Table 1). The sensitivities of the viruses to zanamivir in MDCK cells were comparable; the RG R292K-NA virus did not show decreased sensitivity to zanamivir as was observed in the NA inhibition assay. In MDCK-SIAT1 cells, the sensitivity of the E119V-NA virus to oseltamivir carboxylate was 1/10 of that of the RG WT virus (EC50, 0.43 and 0.04 μM, respectively). In MDCK-SIAT1 cells, the proportional change in the EC50 was similar to that observed in MDCK cells, but the EC50 were significantly lower, confirming the greater sensitivity of MDCK-SIAT1 cells. The RG WT and RG E119V-NA viruses showed comparable sensitivities to zanamivir in MDCK-SIAT1 cells (Table 1). We were unable to determine the sensitivity of the RG R292K-NA virus in MDCK-SIAT1 cells, possibly because of the impaired growth of the virus in this cell line (Table 1).
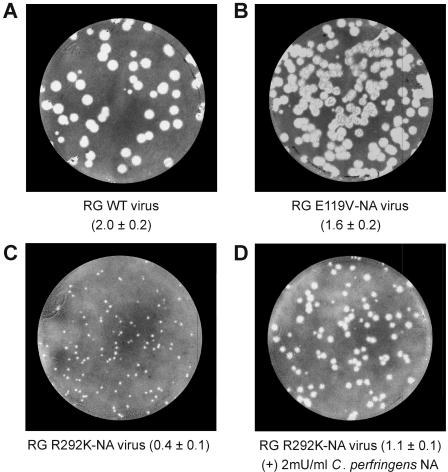
Plaque morphology and growth.
To determine the effects of the E119V and R292K NA mutations on growth in vitro, we first characterized virus plaque morphology in MDCK cells (Fig. 2). The yields of the RG WT, RG E119V-NA, and RG R292K-NA viruses in MDCK cells were comparable (106 to 107 PFU/ml). However, their plaque morphologies differed; the RG WT and RG E119V-NA viruses formed plaques of comparable sizes (Fig. 2A and B), whereas the RG R292K-NA virus formed significantly smaller plaques (P < 0.05, t test) (Fig. 2C). The diameter of the plaques (but not their number) increased by a factor of ∼2 when 2 mU/ml of C. perfringens NA was added to the agar overlay (Fig. 2D).
FIG. 2.
Plaque morphology of recombinant A/Wuhan/359/95 influenza viruses in MDCK cells. MDCK cells infected with the RG WT (A) and RG E119V-NA (B) viruses were incubated in the absence of C. perfringens NA in the agar overlay, while MDCK cells infected with RG R292K-NA virus were incubated in the absence (C) and in the presence (D) of 2 mU/ml C. perfringens NA. After 3 days at 37°C, the cell monolayers were stained and the diameters of 10 randomly selected plaques were measured. Values in parentheses are mean plaque diameters (millimeters) ± SD.
The growth of the recombinant viruses was then assayed in two mammalian cell lines (MDCK, MDCK-SIAT1) and in embryonated chicken eggs (Table 2). All three viruses replicated efficiently in MDCK cells with comparable TCID50 (6.8 to 7.4 log10 TCID50/ml). In MDCK-SIAT1 cells, the TCID50 of the RG WT virus was comparable to that of the RG E119V-NA virus (6.4 and 7.1 log10 TCID50/ml, respectively) but differed from that of the RG R292K-NA virus (4.4 log10 TCID50/ml) by a factor of ∼100. The viral yield of the RG R292K-NA virus in MDCK-SIAT1 cells was rescued in the presence of 2 mU/ml of C. perfringens NA (Table 2). The relative viral yield data also showed the impaired replication of the RG R292K-NA virus in MDCK-SIAT1 cells. In eggs, the RG WT and RG E119V-NA viruses replicated to titers of 4.6 to 4.8 log10 EID50/ml, while the replication of the RG R292K-NA virus was not detectable by the hemagglutination assay (Table 2).
TABLE 2.
Infectivities of recombinant A/Wuhan/359/95 (H3N2) influenza viruses with different NA mutations
| Virus | Viral yield
|
Relative viral yield
|
|||
|---|---|---|---|---|---|
| MDCKa | MDCK-SIAT1a | Eggsb | MDCK-SIAT1/MDCKc | Egg/MDCKd | |
| RG WT | 7.0 ± 0.2 | 6.4 ± 0.3 | 4.6 ± 0.2 | 0.2 | 3.6 × 10−3 |
| RG E119V-NA | 7.4 ± 0.2 | 7.1 ± 0.2 | 4.8 ± 0.2 | 0.5 | 2.5 × 10−3 |
| RG R292K-NA | 6.8 ± 0.4 | 4.4 ± 0.2 (6.7 ± 0.3)e | <f | 4 × 10−3 | <1.6 × 10−7 |
Mean log10 TCID50/ml ± SD from three independent determinations.
Mean log10 EID50/ml ± SD from three independent determinations.
Ratio of mean TCID50/ml in MDCK-SIAT1 and MDCK cells.
Ratio of the mean EID50/ml and the TCID50/ml in MDCK cells.
Values obtained with the addition of 2 mU/ml C. perfringens NA to the infection medium.
<, below level of detection (<0.75 log10 EID50/ml).
Overall, the viral yields of the three recombinant viruses were comparable in MDCK cells but different in MDCK-SIAT1 cells and in eggs. The R292K mutation had a greater impact on viral fitness than the E119V mutation: the growth of RG R292K-NA viruses in MDCK-SIAT1 cells and in eggs was significantly impaired, whereas the growth of RG E119V-NA virus was comparable to that of the RG WT virus.
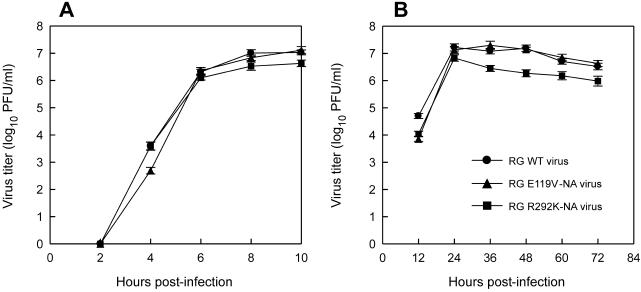
Replication kinetics.
We further assayed the growth of the viruses in single and multiple replication cycles in MDCK and MDCK-SIAT1 cells. In MDCK cells, the three viruses had similar single-step growth curves and all reached comparable viral yields (>106 PFU/ml) at 10 h p.i. (Fig. 3A). The replication efficiencies of the viruses were also similar in multistep growth curves, although the RG R292K-NA virus had a slightly lower titer (<1 log10 PFU/ml difference) after 36 h p.i., possibly because of its heat instability (Fig. 3B). Addition of C. perfringens NA to the medium did not alter the growth curves significantly. Overall, neither the E119V nor the R292K NA mutation significantly affected the viral replication efficiency in MDCK cells.
FIG. 3.
Replication kinetics of recombinant A/Wuhan/359/95 influenza viruses in MDCK cells. (A) Single-step growth curve. Cells were infected with RG WT, RG E119V-NA, or RG R292K-NA virus at an MOI of ∼2.2 PFU/cell. (B) Multistep growth curve. Cells were infected with the recombinant viruses at an MOI of 0.01 PFU/cell. Virus in the supernatant was titrated (log10 PFU/ml) at the indicated times postinfection. Each datum point represents the mean ± SD from three experiments.
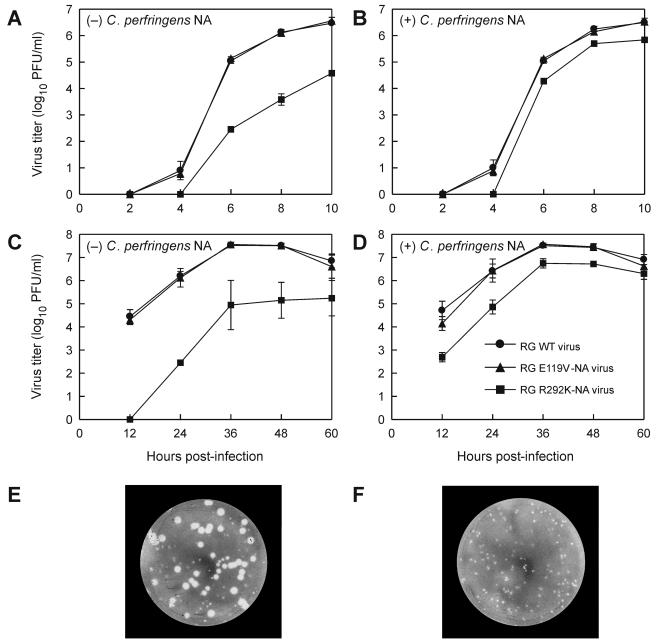
We also compared the replication kinetics of the three recombinant viruses in MDCK-SIAT1 cells, which have increased surface expression of human-like (α2,6-linked terminal SA) cell surface receptors (22). The RG WT and RG E119V-NA viruses showed similar replication kinetics in single-step growth curves in MDCK-SIAT1 cells, whereas the RG R292K-NA virus was not detected in the supernatant until 6 h p.i. (Fig. 4A). The RG R292K-NA virus plaques remained small and homogeneous. The replication defect of the RG R292K-NA virus was rescued in the presence of 2 mU/ml C. perfringens NA (Fig. 4B).
FIG. 4.
Replication kinetics of recombinant A/Wuhan/359/95 influenza viruses in MDCK-SIAT1 cells. (A, B) Single-step growth curves. Cells were infected with RG WT, RG E119V-NA, or RG R292K-NA virus at an MOI of ∼2.2 PFU/cell in the absence (A) or presence (B) of 2 mU/ml of C. perfringens NA in the medium. (C, D) Multistep growth curves. Cells were infected with the recombinant viruses at an MOI of 0.01 PFU/cell in the absence (C) or presence (D) of 2 mU/ml of C. perfringens NA in the medium. Virus in the supernatant was titrated (log10 PFU/ml) at the indicated times postinfection. Each datum point represents the mean ± SD from three experiments. RG R292K-NA virus reverted to WT-NA (R292-NA) during multistep replication in MDCK-SIAT1 cells. Revertant (K292→R) NA was observed in at least one of the three experiments at 36, 48, and 60 h postinfection without supplementary C. perfringens NA (E, 60 h postinfection). This reversion caused the large SD seen for the RG R292K-NA virus in the absence of C. perfringens NA (C). In the presence of C. perfringens NA, plaques were homogeneous in size (F, 60 h postinfection).
Under multicycle growth conditions, the E119V-NA and RG WT viruses replicated to comparable titers while the RG R292K-NA virus showed a profound replication defect (Fig. 4C). The RG R292K-NA virus was not detected until 24 h p.i. Further, at least one of the triplicate supernatants of the RG R292K-NA virus collected 36, 48, and 60 h p.i. grew a mixture of small and large plaques (Fig. 4E). We sequenced the NA genes of viruses in three large and three small plaques. In all large plaques, viruses possessed Arg (R) at NA residue 292 and thus had reverted to wild-type NA. Viruses that produced small plaques retained Lys (K) at residue 292 of NA. These results demonstrated the instability of the R292K mutation during multicycle replication in MDCK-SIAT1 cells. The replication defect of the RG R292K-NA virus was partially compensated by addition of C. perfringens NA to the medium (Fig. 4D); the RG R292K-NA virus produced homogeneous small plaques in MDCK cells in the presence of bacterial NA (Fig. 4F), and sequence analysis showed that K had been retained at position 292 of NA.
Transmissibility in the ferret contact model.
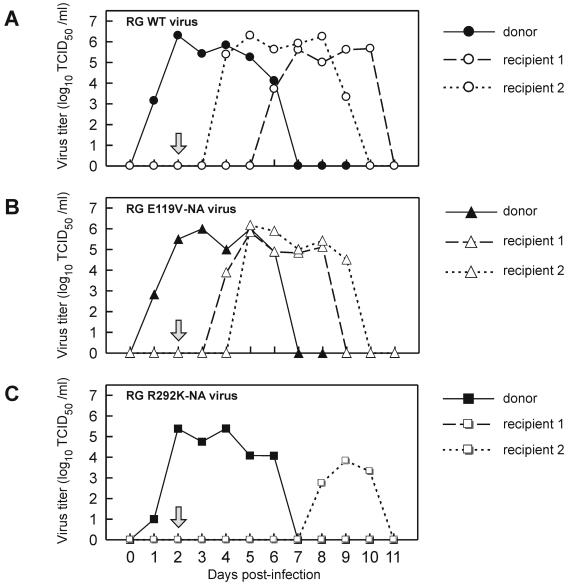
We further compared the transmissibility of the RG WT, RG E119V-NA, and RG R292K-NA viruses by housing two naive contact ferrets with each of three ferrets that had been inoculated with 1,000 TCID50 of the RG WT, RG E119V-NA, or RG R292K-NA virus. The donor ferrets shed virus from day 1 through day 6 p.i. (Fig. 5) and were housed with the naive ferrets on day 2 p.i., when the virus titer in their nasal wash fluid was >105 TCID50/ml. To quantify the amount of virus shed during the course of infection, we calculated the area under the curve (AUC) for the ferret nasal washes that represents the cumulative amount of virus shed by each ferret postinfection (Fig. 5). Ferrets inoculated with the RG WT and RG E119V-NA viruses showed comparable AUCs (30.1 and 30.2, respectively), while the RG R292K-NA donor had an AUC of 24.7.
FIG. 5.
Transmissibility of recombinant A/Wuhan/359/95 influenza viruses in a ferret contact model. Panels show virus titers (log10 TCID50/ml) in the nasal washes of ferrets infected with RG WT virus (A), RG E119V-NA virus (B), or RG R292K-NA virus (C). All donor ferrets (solid lines) were inoculated intranasally with 1,000 TCID50 of recombinant virus in 0.5 ml sterile PBS. At 2 days p.i. (arrow), each donor ferret was moved into housing with two naive recipient ferrets (broken lines). Nasal washes were collected daily for 14 days, and virus was titrated in MDCK cells.
Virus was detected in the nasal washes of the recipient ferrets 2 to 4 days (mean ± SD = 2.8 ± 1.0 days) after they were housed with the RG WT or RG E119V-NA virus donors. In contrast, only one of the two naive ferrets housed with the RG R292K-NA virus donor was infected, and virus was shed significantly later (6 days after the recipient was housed with the donor; P < 0.05). The mean AUCs for the two RG WT recipients and the two RG E119V-NA recipients were comparable (29.2 ± 4.1 and 25.8 ± 1.7, respectively), but the AUC for the RG R292K-NA virus recipient was significantly lower (11.7; P < 0.05). Therefore, although the three donors shed fairly comparable amounts of virus (AUCs, 30.1, 30.2, and 24.7) during the course of infection, the transmission efficiency of the RG R292K-NA virus was significantly lower.
All donor ferrets continued to shed viruses carrying NA mutations identical to those in the viruses used for inoculation, as confirmed by NA sequence analysis of viruses from the nasal washes collected on days 3 and 5 p.i. The two recipients that had direct contact with the RG E119V-NA virus donor shed virus containing the E119V mutation, as verified by the NA sequences of viruses obtained on day 7 p.i. Virus from the nasal wash collected on day 9 p.i. from the recipient exposed to the RG R292K-NA donor had an NA sequence identical to that of the inoculated virus. Hemagglutination inhibition tests confirmed that one of the two recipients housed with the RG R292K-NA donor was not infected (anti-HA antibodies were not detected in the serum). Therefore, all three donors were infected with the inoculated viruses but only the RG E119V-NA virus was transmitted from the donor to two naive recipients as efficiently as the RG WT virus.
DISCUSSION
Influenza virus variants that have NA mutations associated with NAI resistance are not easily selected in vitro or in vivo, and in most previous studies these variants exhibited compromised viral fitness and virulence (3, 14, 19, 24, 36). However, two recent reports suggest that clinically derived NAI-resistant influenza viruses with different NA mutations differ in transmissibility in ferrets (14, 15). We elucidated this possibility by molecular characterization of the resistant variants in a homogeneous genetic background. Our results revealed that the differences between the NAI-resistant variants in fitness and transmissibility may reflect the locations of NA mutations. They also indicate that transmissible NAI-resistant variants may emerge, a finding that underlines the necessity of continuous monitoring for NAI resistance.
The conserved residues in the NA are either catalytic residues that directly contact the substrate and participate in its hydrolysis or framework residues that provide the structure for the catalytic residues (5, 6). Mutations that may confer NAI resistance have been identified at both catalytic and framework residues, and the location of the NA mutation is reportedly associated with the level of NAI resistance (11). Mutations at catalytic residues (R292K, R152K) may confer cross-resistance to zanamivir, oseltamivir carboxylate, and RWJ-270201, while mutations at framework residues (H274Y, E119G/A/D) appear to confer resistance to only zanamivir or oseltamivir carboxylate (11). In our NA inhibition assay, the virus with the R292K mutation was resistant to zanamivir (13-fold) and oseltamivir carboxylate (>30,000-fold), as previously reported (11, 23, 33). Recombinant virus with the E119V mutation, unlike the E119G/A/D mutations that reportedly confer resistance to zanamivir (1, 9, 11, 23), was sensitive to zanamivir but resistant to oseltamivir. E119 and E227 of the NA were reported to form salt bridges with the guanidino group at C-4 of zanamivir (31). While oseltamivir carboxylate has an amino group at C-4 (31), it is possible that direct interaction between either E119 or E227 and the amino group is required. The mechanism by which the E119V mutation confers resistance to oseltamivir carboxylate is unclear, and more-detailed structural analysis may be required.
In the present study, two different in vitro assays were used to evaluate the sensitivity of the viruses to NAIs. When only the NA effect was considered, as in the NA inhibition assay, both the RG E119V-NA and RG R292K-NA viruses demonstrated a high level of resistance to oseltamivir carboxylate (sensitivity decreased >200 and >30,000 times versus that of the WT virus NA, respectively). However, when HA-NA balance and virus replication efficiency were involved, as in the virus reduction assay in MDCK cells, sensitivity to oseltamivir carboxylate decreased only approximately 10-fold in the RG E119V-NA virus and 30-fold in the RG R292K-NA virus. Although the RG R292K-NA virus showed an approximately 13-fold decrease in sensitivity in the NA inhibition assay, the decreased sensitivity was not observed in the virus reduction assay in MDCK cells, possibly because of instability of the virus or a limitation of the assay. Our results suggested that the NA inhibition assay can better identify resistant variants with NA mutations than the virus reduction assay.
Mutations at conserved NA residues that confer NAI resistance may also decrease NA enzymatic activity and further disrupt the HA-NA balance required for efficient viral replication (20, 26, 35). In the present study, we showed that mutations at different conserved residues of NA may lead to different degrees of NA functional loss: mutation of the catalytic residue (R292K) resulted in greater loss of NA activity and thermostability than mutation of the framework residue (E119V). The changes in NA functional activity caused by the R292K and E119V mutations should both disrupt the HA-NA balance. However, we observed that the RG R292K-NA virus had significantly reduced growth in MDCK-SIAT1 cells and impaired transmissibility in ferrets, while the RG E119V-NA virus showed growth and transmissibility comparable to those of the RG WT virus. Despite the fact that both mutations decreased the NA activity, our results showed that only the R292K mutation significantly impaired the HA-NA balance. It is still not clear whether the R292K-NA mutation changed the enzymatic activity and/or substrate specificity of NA or whether the NA expression level differs with different mutations.
MDCK cells are the cell line most commonly used to study influenza viruses. However, MDCK cells were not able to reveal the compromised fitness of the RG R292K virus. We observed that in MDCK cells, the RG R292K-NA virus replication curve for single or multiple cycles was similar to that of the RG WT virus, although the virulence of the RG R292K-NA virus in vivo was significantly impaired. The impaired growth of the virus was detectable in MDCK-SIAT1 cells. The failure of the RG R292K-NA virus to maintain the R292K mutation through multiple cycles of replication in MDCK-SIAT1 cells also suggests greater selection pressure on this virus in MDCK-SIAT1 cells than in MDCK cells; revertants (K→R) were detected in approximately one of three triplicate wells after 36 h postinfection. However, K→R revertants were not identified in the nasal washes collected from the RG R292K-NA virus donor and from the infected recipient ferret, although revertants have been detected in larger groups of ferrets (14).
There are limited reports of characterization of the NAI-resistant variants in vivo, and the different virus strains and infection doses used have made comparisons difficult. The transmissibility of the wild-type A/Sydney/5/97-like (H3N2) influenza virus and a resistant variant with the R292K NA mutation was evaluated in a ferret model with an inoculation dose of 200 TCID50; the resistant variant was not transmissible, while the wild-type virus was transmitted efficiently (14). Conversely, an A/Wuhan/359/95-like (H3N2) virus with the E119V NA mutation was transmitted as efficiently as the wild-type virus with an inoculation dose of <10 TCID50. An A/New Caledonia/20/99-like virus with the H274Y NA mutation was found to require a challenge dose 100 times that of the wild-type virus (∼600 TCID50) and was less transmissible (15). In the present study, the R292K, E119V, and H274Y mutations were introduced into the A/Wuhan/359/95 virus background. However, the H274Y mutation did not confer NAI resistance (data not shown) and thus was not included in further growth and transmissibility evaluations. Although three donor ferrets inoculated with 1,000 TCID50 of the RG WT, RG E119V-NA, or RG R292K-NA virus were efficiently infected and stably shed the virus for 6 days, only the RG E119V-NA virus was transmitted to naive ferrets as efficiently as the RG WT virus.
In conclusion, we used genetically homogeneous recombinant viruses to show that the reported difference in transmissibility of the NAI-resistant variants in ferrets (14, 15) is related to the degree of the NA defect caused by the location of the NA mutation. NAI-resistant influenza virus variants may differ substantially in their fitness and transmissibility, and continuous surveillance for the emergence of transmissible NAI-resistant variants is necessary.
Acknowledgments
This work was supported by grants AI95357 and AI57570 from the National Institute of Allergy and Infectious Diseases; by the VIRGIL European Network of Excellence on Antiviral Drug Resistance in the 6th Framework Programme of the EU; by the American Lebanese Syrian Associated Charities (ALSAC); by a Francis E. Payne Fellowship from the School of Public Health, University of Michigan; and by Hoffmann-La Roche.
We thank Christoph Scholtissek, Richard Webby, Todd Hatchette, and Aleksandr Lipatov for excellent advice; Rachel Truscon and Suzanne Ohmit, University of Michigan, for helpful suggestions; Betsy Williford for illustrations; and Sharon Naron for editorial assistance.
REFERENCES
- 1.Blick, T. J., A. Sahasrabudhe, M. McDonald, I. J. Owens, P. J. Morley, R. J. Fenton, and J. L. McKimm-Breschkin. 1998. The interaction of neuraminidase and hemagglutinin mutations in influenza virus in resistance to 4-guanidino-Neu5Ac2en. Virology 246:95-103. [DOI] [PubMed] [Google Scholar]
- 2.Blick, T. J., T. Tiong, A. Sahasrabudhe, J. N. Varghese, P. M. Colman, G. J. Hart, R. C. Bethell, and J. L. McKimm-Breschkin. 1995. Generation and characterization of an influenza virus neuraminidase variant with decreased sensitivity to the neuraminidase-specific inhibitor 4-guanidino-Neu5Ac2en. Virology 214:475-484. [DOI] [PubMed] [Google Scholar]
- 3.Carr, J., J. Ives, L. Kelly, R. Lambkin, J. Oxford, D. Mendel, L. Tai, and N. Roberts. 2002. Influenza virus carrying neuraminidase with reduced sensitivity to oseltamivir carboxylate has altered properties in vitro and is compromised for infectivity and replicative ability in vivo. Antiviral Res. 54:79-88. [DOI] [PubMed] [Google Scholar]
- 4.Carr, J., J. Ives, N. Roberts, C. Y. Tai, M. Wang, M. Meng, D. Mendel, L. Kelly, R. Lambkin, and J. Oxford. 1999. An oseltamivir-treatment selected influenzaA/Wuhan/359/95 virus with an E119V mutation in the neuraminidase gene has reduced infectivity in vivo. In Second International Symposium for Influenza and Other Respiratory Viruses. The Macrae Group, New York, N.Y.
- 5.Colman, P. M. 1994. Influenza virus neuraminidase: structure, antibodies, and inhibitors. Protein Sci. 3:1687-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colman, P. M., P. A. Hoyne, and M. C. Lawrence. 1993. Sequence and structure alignment of paramyxovirus hemagglutinin-neuraminidase with influenza virus neuraminidase. J. Virol. 67:2972-2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gubareva, L. V., R. Bethell, G. J. Hart, K. G. Murti, C. R. Penn, and R. G. Webster. 1996. Characterization of mutants of influenza A virus selected with the neuraminidase inhibitor 4-guanidino-Neu5Ac2en. J. Virol. 70:1818-1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gubareva, L. V., L. Kaiser, and F. G. Hayden. 2000. Influenza virus neuraminidase inhibitors. Lancet 355:827-835. [DOI] [PubMed] [Google Scholar]
- 9.Gubareva, L. V., M. J. Robinson, R. C. Bethell, and R. G. Webster. 1997. Catalytic and framework mutations in the neuraminidase active site of influenza viruses that are resistant to 4-guanidino-Neu5Ac2en. J. Virol. 71:3385-3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gubareva, L. V., R. G. Webster, and F. G. Hayden. 2002. Detection of influenza virus resistance to neuraminidase inhibitors by an enzyme inhibition assay. Antiviral Res. 53:47-61. [DOI] [PubMed] [Google Scholar]
- 11.Gubareva, L. V., R. G. Webster, and F. G. Hayden. 2001. Comparison of the activities of zanamivir, oseltamivir, and RWJ-270201 against clinical isolates of influenza virus and neuraminidase inhibitor-resistant variants. Antimicrob. Agents Chemother. 45:3403-3408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayden, F. G. 1997. Antivirals for pandemic influenza. J. Infect. Dis. 176(Suppl.)1:S56-S61. [DOI] [PubMed] [Google Scholar]
- 13.Hayden, F. G., R. B. Belshe, R. D. Clover, A. J. Hay, M. G. Oakes, and W. Soo. 1989. Emergence and apparent transmission of rimantadine-resistant influenza A virus in families. N. Engl. J. Med. 321:1696-1702. [DOI] [PubMed] [Google Scholar]
- 14.Herlocher, M. L., J. Carr, J. Ives, S. Elias, R. Truscon, N. Roberts, and A. S. Monto. 2002. Influenza virus carrying an R292K mutation in the neuraminidase gene is not transmitted in ferrets. Antiviral Res. 54:99-111. [DOI] [PubMed] [Google Scholar]
- 15.Herlocher, M. L., R. Truscon, S. Elias, H. L. Yen, N. A. Roberts, S. E. Ohmit, and A. S. Monto. 2004. Influenza viruses resistant to the antiviral drug oseltamivir: transmission studies in ferrets. J. Infect. Dis. 190:1627-1630. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann, E., K. Mahmood, C. F. Yang, R. G. Webster, H. B. Greenberg, and G. Kemble. 2002. Rescue of influenza B virus from eight plasmids. Proc. Natl. Acad. Sci. USA 99:11411-11416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275-2289. [DOI] [PubMed] [Google Scholar]
- 19.Ives, J. A., J. A. Carr, D. B. Mendel, C. Y. Tai, R. Lambkin, L. Kelly, J. S. Oxford, F. G. Hayden, and N. A. Roberts. 2002. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leave virus severely compromised both in vitro and in vivo. Antiviral Res. 55:307-317. [DOI] [PubMed] [Google Scholar]
- 20.Kaverin, N. V., A. S. Gambaryan, N. V. Bovin, I. A. Rudneva, A. A. Shilov, O. M. Khodova, N. L. Varich, B. V. Sinitsin, N. V. Makarova, and E. A. Kropotkina. 1998. Postreassortment changes in influenza A virus hemagglutinin restoring HA-NA functional match. Virology 244:315-321. [DOI] [PubMed] [Google Scholar]
- 21.Kiso, M., K. Mitamura, Y. Sakai-Tagawa, K. Shiraishi, C. Kawakami, K. Kimura, F. G. Hayden, N. Sugaya, and Y. Kawaoka. 2004. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 364:759-765. [DOI] [PubMed] [Google Scholar]
- 22.Matrosovich, M., T. Matrosovich, J. Carr, N. A. Roberts, and H. D. Klenk. 2003. Overexpression of the α-2,6-sialyltransferase in MDCK cells increases influenza virus sensitivity to neuraminidase inhibitors. J. Virol. 77:8418-8425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McKimm-Breschkin, J., T. Trivedi, A. Hampson, A. Hay, A. Klimov, M. Tashiro, F. Hayden, and M. Zambon. 2003. Neuraminidase sequence analysis and susceptibilities of influenza virus clinical isolates to zanamivir and oseltamivir. Antimicrob. Agents Chemother. 47:2264-2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKimm-Breschkin, J. L. 2000. Resistance of influenza viruses to neuraminidase inhibitors—a review. Antiviral Res. 47:1-17. [DOI] [PubMed] [Google Scholar]
- 25.McKimm-Breschkin, J. L. 2002. Neuraminidase inhibitors for the treatment and prevention of influenza. Exp. Opin. Pharmacother. 3:103-112. [DOI] [PubMed] [Google Scholar]
- 26.Mitnaul, L. J., M. N. Matrosovich, M. R. Castrucci, A. B. Tuzikov, N. V. Bovin, D. Kobasa, and Y. Kawaoka. 2000. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. J. Virol. 74:6015-6020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Potier, M., L. Mameli, M. Belisle, L. Dallaire, and S. B. Melancon. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-α-d-N-acetylneuraminate) substrate. Anal. Biochem. 94:287-296. [DOI] [PubMed] [Google Scholar]
- 28.Reed, L. J., and H. Muench. 1938. A simple method for estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 29.Staschke, K. A., J. M. Colacino, A. J. Baxter, G. M. Air, A. Bansal, W. J. Hornback, J. E. Munroe, and W. G. Laver. 1995. Molecular basis for the resistance of influenza viruses to 4-guanidino-Neu5Ac2en. Virology 214:642-646. [DOI] [PubMed] [Google Scholar]
- 30.Stilianakis, N. I., A. S. Perelson, and F. G. Hayden. 2002. Drug resistance and influenza pandemics. Lancet 359:1862-1863. [DOI] [PubMed] [Google Scholar]
- 31.Stoll, V., K. D. Stewart, C. J. Maring, S. Muchmore, V. Giranda, Y. G. Gu, G. Wang, Y. Chen, M. Sun, C. Zhao, A. L. Kennedy, D. L. Madigan, Y. Xu, A. Saldivar, W. Kati, G. Laver, T. Sowin, H. L. Sham, J. Greer, and D. Kempf. 2003. Influenza neuraminidase inhibitors: structure-based design of a novel inhibitor series. Biochemistry 42:718-727. [DOI] [PubMed] [Google Scholar]
- 32.Sugrue, R. J., and A. J. Hay. 1991. Structural characteristics of the M2 protein of influenza A viruses: evidence that it forms a tetrameric channel. Virology 180:617-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tai, C. Y., P. A. Escarpe, R. W. Sidwell, M. A. Williams, W. Lew, H. Wu, C. U. Kim, and D. B. Mendel. 1998. Characterization of human influenza virus variants selected in vitro in the presence of the neuraminidase inhibitor GS 4071. Antimicrob. Agents Chemother. 42:3234-3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Varghese, J. N., J. L. McKimm-Breschkin, J. B. Caldwell, A. A. Kortt, and P. M. Colman. 1992. The structure of the complex between influenza virus neuraminidase and sialic acid, the viral receptor. Proteins 14:327-332. [DOI] [PubMed] [Google Scholar]
- 35.Wagner, R., M. Matrosovich, and H. D. Klenk. 2002. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev. Med. Virol. 12:159-166. [DOI] [PubMed] [Google Scholar]
- 36.Zambon, M., and F. G. Hayden. 2001. Position statement: global neuraminidase inhibitor susceptibility network. Antiviral Res. 49:147-156. [DOI] [PubMed] [Google Scholar]