Abstract
Objective: To evaluate the effect of surgical timing on meniscal healing, knee function recovery, and adverse events in patients undergoing arthroscopic meniscal repair. Methods: A retrospective study of 260 patients treated at Putuo Hospital between February 2020 and August 2024 was conducted. Patients were divided into an early surgery group (≤4 weeks, n=148) and a late surgery group (>4 weeks, n=112). Data from electronic records and follow-up notes included baseline characteristics (age, gender, BMI), surgical indicators (operation time, hospital stay, costs), healing status assessed by 6-month postoperative MRI (complete, partial, or non-healing), functional scores (Lysholm, Tegner, International Knee Documentation Committee (IKDC)), VAS pain levels, adverse events, and prognosis. Statistical analysis included chi-square tests, t-tests, Mann-Whitney U tests, repeated measures ANOVA, and logistic regression, with interaction analysis examining the effects of age, BMI, and surgical timing. Results: The early surgery group showed significantly higher rates of complete healing (66.22% vs. 43.75%, P<0.001) and overall healing (93.92% vs. 85.71%, P=0.026), with lower non-healing rates (6.08% vs. 14.29%) compared to the late surgery group. At 3 and 6 months post-surgery, the early group exhibited better Lysholm, Tegner, and IKDC scores, along with lower Visual Analog Scale (VAS) pain scores (all P<0.001). Logistic regression identified surgical timing (OR=0.054, 95% CI: 0.024-0.111, P<0.001), age (OR=0.22, 95% CI: 0.107-0.429, P<0.001), and BMI (OR=0.266, 95% CI: 0.135-0.507, P<0.001) as risk factors for poor recovery, with interaction analysis revealing significant effects of surgical timing (P<0.001) and age (P=0.006). Conclusion: Early surgery (≤4 weeks) significantly improves healing rates, enhances knee function, and reduces pain, without increasing adverse events. Our findings highlight surgical timing, age, and BMI as key predictors of recovery outcomes, with early intervention resulting in marked functional improvements.
Keywords: Meniscal injury, surgical timing, meniscal healing, knee function
Introduction
Meniscal injuries are among the most common sports-related orthopedic conditions, frequently affecting athletes, young individuals, and elderly patients with degenerative changes [1]. As a crucial cartilaginous structure in the knee, the meniscus plays a vital role in load distribution, joint stability, and motion support. Research by Hanna et al. [2] highlights that meniscal repair, compared to partial meniscectomy, better preserves joint function and reduces the risk of long-term osteoarthritis, emphasizing the importance of preservation strategies in modern treatments. However, these injuries often result in pain, swelling, limited mobility, and secondary osteoarthritis, significantly impacting patients’ quality of life and athletic performance [3]. Arthroscopic meniscal repair has become the preferred treatment due to its minimally invasive nature, rapid recovery, and effective outcomes [4]. Our clinical observations indicate that repair techniques are more effective in preserving meniscal tissue than traditional meniscectomy, reducing long-term complications [5]. Despite these advancements, surgical timing varies, with some patients delaying intervention due to initial conservative management or unrecognized symptom severity [6]. Does early surgery reduce tissue degeneration and secondary damage? Could delayed surgery impair healing due to reduced repair capacity? Current evidence on the impact of surgical timing on patient outcomes is limited, making this investigation clinically important.
Recent studies, both domestic and international, have extensively explored arthroscopic meniscal repair, focusing on surgical techniques, suture materials, and postoperative rehabilitation [7]. Data show that 55.9% of young athletes undergoing acute repair achieved complete healing at 6 months, with significant improvements in functional scores such as the International Knee Documentation Committee Subjective Knee Form (IKDC) and Lysholm [8]. However, the prolonged healing process suggests that early intervention may be crucial for high-demand groups. Nevertheless, studies on the effect of surgical timing on healing, knee function, and complications (e.g., joint effusion, infection, revision surgery) are limited. Existing research lacks standardized timing definitions, large sample sizes, and comprehensive analyses of functional scores (Lysholm, Tegner, IKDC) and pain scores (Visual Analog Scale, VAS). Additionally, the interactions between patient factors such as age and body mass index (BMI) with surgical timing remain underexplored. A systematic review and meta-analysis on anterior cruciate ligament (ACL) and multiligament knee injuries (MLKI) found no significant differences in outcomes with early surgery (within 3-6 weeks) for isolated ACL injuries. However, early intervention in MLKI cases was associated with lower meniscal and cartilage damage. Although not focused on meniscal repair, these findings provide indirect insights. Comprehensive research on surgical timing in meniscal repair remains scarce.
This study aims to systematically evaluate how different surgical timings affect meniscal healing rates, knee function recovery, and adverse events in patients undergoing arthroscopic repair. By analyzing baseline characteristics across groups, we compared postoperative healing rates (complete, partial, non-healing) and surgical indicators (operative time, hospital stay, costs). We also assessed functional recovery at 3 and 6 months using Lysholm, Tegner, IKDC, and VAS scores, as well as the incidence of adverse events (joint effusion, swelling/pain, infection, revision surgery). Additionally, univariate and multivariate logistic regression, along with interaction analysis, will identify risk factors and explore the combined effects of age, BMI, and surgical timing on recovery outcomes.
Methods and materials
Sample size calculation
The sample size was determined based on IKDC scores (mean difference of 2.77, standard deviation ~4) and Lysholm scores (mean difference of 2.61, standard deviation ~4) from Shen et al.’s [10] meta-analysis. Using a two-sided α=0.05, a 1:1 group design, and 90% power, we calculated that each group needed 44 cases (IKDC) or 50 cases (Lysholm) to detect differences between early and delayed anterior cruciate ligament reconstruction.
General information
We retrospectively reviewed arthroscopic meniscal repair cases from Putuo Hospital between February 2020 and August 2024, based on inclusion criteria: confirmed meniscal injury diagnosed via magnetic resonance imaging (MRI) or clinical examination, suitable for arthroscopic repair [1]; patients who underwent the procedure; complete follow-up and clinical data; and precise injury timing from medical records or patient reports. Exclusion criteria included: severe intra-articular injuries (e.g., significant cartilage defects, fractures); prior meniscal or knee surgeries (e.g., ligament reconstruction); severe systemic conditions (e.g., active infection, malignancy, uncontrolled autoimmune diseases) affecting healing or recovery; and pregnant or breastfeeding females.
A total of 260 patients were enrolled, divided into an early group (surgical timing ≤4 weeks, n=148) and a late group (>4 weeks, n=112) based on the injury-to-surgery interval. The study was approved by Putuo Hospital’s medical ethics committee.
Treatment protocol
The arthroscopic repair protocol began with MRI and preoperative blood tests on admission to confirm meniscal tears and concomitant injuries, followed by surgery the next day. Spinal anesthesia (spinal block) was preferred, though general anesthesia was used when necessary. The inside-out suture technique (Figure 1) was employed, with intraoperative management of proliferative synovium, loose bodies, or microfracture procedures, and routine platelet-rich plasma (PRP) injection before closure to enhance healing. Postoperatively, elastic bandaging from ankle to thigh, low-molecular-weight heparin for anticoagulation, and exercises (knee flexion-extension, ankle pump, quadriceps isometric contractions) were initiated on day one. Patients used knee braces and crutches, avoiding full weight-bearing. Follow-up at 6 weeks assessed recovery, guided crutch discontinuation, and further monitoring.
Figure 1.
Arthroscopic images of meniscal repair using inside-out suturing technique. A (Preoperative): Shows the preoperative condition of the meniscus with a visible tear prior to repair. B (Postoperative): Displays the postoperative condition of the meniscus, demonstrating the sutured repair with stitches in place.
Clinical data collection
Data were collected from electronic medical records and outpatient follow-up systems, including baseline characteristics (age ≥45 or <45 years, gender, BMI ≥24 or <24 kg/m2, affected side, tear location, diabetes, hypertension, smoking, alcohol use, concomitant ACL/PCL injuries); surgical indicators (operative time in minutes, hospital stay in days, costs in yuan); healing status (complete, partial, non-healing, overall healing rates); functional scores (preoperative, 3- and 6-month postoperative Lysholm, Tegner, IKDC); pain scores (preoperative, 3- and 6-month postoperative VAS); adverse events (joint effusion, swelling/pain, infection, revision surgery); prognosis (Lysholm ≥90 and IKDC ≥85 for good recovery); and risk factor analysis (univariate/multivariate logistic regression for surgical timing, age, BMI, etc.), including interaction effects of age, BMI, and timing. Data were extracted from admission records and follow-up at 1-2 weeks and 6 weeks to ensure accuracy and completeness.
Functional score definitions
Lysholm knee scoring [11] assesses knee function post-ligament injuries, ranging from 0 to 100, with higher scores indicating better function (95-100 excellent, 84-94 good, 65-83 fair, <65 poor).
Tegner activity scoring [12] measures daily activity and exercise capacity post-sports injury, ranging from 0 to 10 (10 for competitive sports, 0 for bed confinement).
IKDC subjective scoring [13] evaluates knee symptoms and function, scored from 0 to 100, with higher values reflecting better outcomes.
VAS scoring [14] gauges pain intensity, ranging from 0 to 10 (0= no pain, 10= extreme pain).
Meniscal healing definition
Healing status at 6 months was evaluated using MRI, based on Stoller grading criteria [15]: (1) Complete healing: No grade III signals on all planes. (2) Partial healing: Grade III signals on 1-2 planes. (3) Non-healing: Grade III signals on ≥3 planes (Figure 2). (4) Healing rate was calculated as (complete + partial cases)/total cases.
Figure 2.
MRI Evaluation of meniscal healing status. A (Preoperative - Sagittal View): Shows the preoperative sagittal MRI image, highlighting the tear in the medial meniscus. B (Preoperative - Coronal View): Displays the preoperative coronal MRI image, further detailing the meniscal tear. C (Postoperative - Sagittal View): Shows the postoperative sagittal MRI image, indicating the healing status of the meniscus. D (Postoperative - Coronal View): Displays the postoperative coronal MRI image, demonstrating the repaired meniscus condition. Note: MRI: Magnetic Resonance Imaging.
Poor functional recovery definition
Recovery at 6 months was assessed using Lysholm and IKDC scores. Poor recovery was defined as failing to meet both Lysholm ≥90 and IKDC ≥85. Tegner scores were excluded due to their variability, influenced by lifestyle and occupation, while Lysholm and IKDC provide consistent, objective, and subjective insights into recovery.
Outcome measurements
The primary outcomes examined the effects of surgical timing (early ≤4 weeks vs late >4 weeks) on healing rates (complete, partial, non-healing, overall) and knee function recovery (preoperative, 3-month, and 6-month Lysholm, Tegner, and IKDC scores), including proportions of good (Lysholm ≥90, IKDC ≥85) and poor recovery. Secondary outcomes included comparisons of VAS pain scores, operative time, hospital stay, costs, adverse event rates (effusion, swelling/pain, infection, revision surgery), and analysis of risk factors (surgical timing, age, BMI) and interaction effects on recovery via logistic regression.
Statistical analysis
Statistical analyses were performed using SPSS 26.0 and R 4.3.3. Categorical data (e.g., baseline characteristics, healing, events) were compared using chi-square tests (with continuity correction or Fisher’s exact test when needed) and expressed as frequencies and percentages. Normality of continuous data was tested using the Kolmogorov-Smirnov test. Normally distributed data (e.g., operative time, Lysholm, IKDC) were presented as mean ± SD and analyzed using t-tests. Non-normal data (e.g., hospital stay, Tegner, VAS) were presented as median and interquartile range and analyzed using Mann-Whitney U tests. Repeated measures ANOVA assessed functional and VAS scores over time (preoperative, 3-month, and 6-month), with Bonferroni corrections for normal data and Dunnett’s test for non-normal data. Multicollinearity was assessed using the variance inflation factor (VIF) in R’s car package. Logistic regression (using the readr, broom, dplyr, and pROC packages) and interaction analysis (using the rms, cowplot, ggplot2, and visreg packages) were employed to evaluate the effects of surgical timing, age, and BMI on recovery. All tests were two-sided, with P<0.05 considered statistically significant.
Results
Comparison of baseline characteristics
Analysis of baseline characteristics showed no significant differences between the early and late surgery groups in terms of age, gender, BMI, affected side, tear location, history of diabetes, hypertension, smoking, alcohol consumption, and concomitant ACL and PCL injuries (all P>0.05, Table 1).
Table 1.
Comparison of baseline characteristics between the early and late surgery groups
| Variable | Total | Early Group (n=148) | Late Group (n=112) | χ2 | P-value |
|---|---|---|---|---|---|
| Variable | 0.762 | 0.383 | |||
| Age | 145 (55.77%) | 86 (58.11%) | 59 (52.68%) | ||
| ≥45 years | 115 (44.23%) | 62 (41.89%) | 53 (47.32%) | ||
| <45 years | 0.603 | 0.437 | |||
| Gender | 183 (70.38%) | 107 (72.30%) | 76 (67.86%) | ||
| Male | 77 (29.62%) | 41 (27.70%) | 36 (32.14%) | ||
| Female | 0.669 | 0.413 | |||
| BMI | 104 (40.00%) | 56 (37.84%) | 48 (42.86%) | ||
| ≥24 kg/m2 | 156 (60.00%) | 92 (62.16%) | 64 (57.14%) | ||
| <24 kg/m2 | 0.957 | 0.328 | |||
| Affected Side | 98 (37.69%) | 52 (35.14%) | 46 (41.07%) | ||
| Left | 162 (62.31%) | 96 (64.86%) | 66 (58.93%) | ||
| Right | 0.474 | 0.491 | |||
| Tear Location | 141 (54.23%) | 83 (56.08%) | 58 (51.79%) | ||
| Lateral | 119 (45.77%) | 65 (43.92%) | 54 (48.21%) | ||
| Medial | 0.023 | 0.880 | |||
| History of Diabetes | 27 (10.38%) | 15 (10.14%) | 12 (10.71%) | ||
| Yes | 233 (89.62%) | 133 (89.86%) | 100 (89.29%) | ||
| No | 0.210 | 0.647 | |||
| History of Hypertension | 45 (17.31%) | 27 (18.24%) | 18 (16.07%) | ||
| Yes | 215 (82.69%) | 121 (81.76%) | 94 (83.93%) | ||
| No | 1.043 | 0.307 | |||
| Smoking History | 201 (77.31%) | 111 (75.00%) | 90 (80.36%) | ||
| Yes | 59 (22.69%) | 37 (25.00%) | 22 (19.64%) | ||
| No | 0.375 | 0.540 | |||
| Alcohol Consumption | 67 (25.77%) | 36 (24.32%) | 31 (27.68%) | ||
| Yes | 193 (74.23%) | 112 (75.68%) | 81 (72.32%) | ||
| No | 0.055 | 0.814 | |||
| Concomitant ACL Injury | 22 (8.46%) | 12 (8.11%) | 10 (8.93%) | ||
| Yes | 238 (91.54%) | 136 (91.89%) | 102 (91.07%) | ||
| No | 0.053 | 0.818 | |||
| Concomitant PCL Injury | 13 (5.00%) | 7 (4.73%) | 6 (5.36%) | ||
| Yes | 247 (95.00%) | 141 (95.27%) | 106 (94.64%) |
Note: BMI: Body Mass Index, ACL: Anterior Cruciate Ligament, PCL: Posterior Cruciate Ligament.
Comparison of healing rates
The early surgery group exhibited significantly better healing outcomes compared to the late surgery group. Complete healing rates were significantly higher in the early surgery group (P<0.001), and overall healing rates also favored early intervention (P=0.026). Notably, the early surgery group showed lower partial healing rates, while non-healing rates were significantly reduced compared to the late surgery group (P<0.05, Table 2).
Table 2.
Comparison of meniscal healing rates between the early and late surgery groups
| Group | Complete Healing | Partial Healing | Non-healing | Healing Rate |
|---|---|---|---|---|
| Early Group (n=148) | 98 (66.22%) | 41 (27.70%) | 9 (6.08%) | 139 (93.92%) |
| Late Group (n=112) | 49 (43.75%) | 47 (41.96%) | 16 (14.29%) | 96 (85.71%) |
| χ2/Z | 3.732 | 4.938 | ||
| P-value | <0.001 | 0.026 | ||
Comparison of surgery-related indicators
A comparative analysis of surgery-related parameters revealed no significant differences between the groups. Operative time was consistent across both groups (P=0.418), and hospital stay duration showed no significant variation (P=0.757). Treatment costs were slightly higher in the early surgery group compared to the late surgery group, though the difference was not statistically significant (P=0.079) (Table 3).
Table 3.
Comparison of surgery-related indicators between the early and late surgery groups
| Variable | Early Group (n=148) | Late Group (n=112) | t/Z | P-value |
|---|---|---|---|---|
| Surgery Duration (min) | 55.41±18.67 | 57.37±20.14 | 0.810 | 0.418 |
| Length of Hospital Stay (d) | 5.00 [4.00, 6.00] | 5.00 [4.00, 6.00] | 0.310 | 0.757 |
| Treatment Cost (yuan) | 24139.24±1504.92 | 23808.44±1487.92 | -1.764 | 0.079 |
Comparison of functional score outcomes
Preoperative functional assessments showed no significant differences between groups (all P>0.05). At baseline, preoperative Lysholm, Tegner activity, and IKDC subjective scores were comparable between the early and late surgery groups. At 3 and 6 months postoperatively, the early surgery group showed significantly superior functional outcomes. Lysholm scores (P<0.001), Tegner activity scores (P<0.001), and IKDC subjective scores (P<0.001) were all significantly higher in the early surgery group. Both groups showed significant improvement across all time comparisons: preoperative versus 3 months, preoperative versus 6 months, and 3 months versus 6 months (all P<0.001). However, the early surgery group demonstrated a greater magnitude of improvement across all measures (P<0.05, Table 4).
Table 4.
Comparison of functional score changes between the early and late surgery groups
| Variable | Early Group (n=148) | Late Group (n=112) | t/Z | P-value |
|---|---|---|---|---|
| Preoperative Lysholm Score | 54.93±4.70 | 54.96±4.79 | 0.054 | 0.957 |
| 3-month Postoperative Lysholm Score | 81.63±5.42 | 74.50±5.42 | -10.500 | <0.001 |
| 6-month Postoperative Lysholm Score | 92.00 [89.00, 95.00] | 87.00 [83.00, 90.00] | 8.469 | <0.001 |
| t/Z/P-value (Pre vs 3-month Post) | 45.287/<0.001 | 28.572/<0.001 | ||
| t/Z/P-value (Pre vs 6-month Post) | 70.213/<0.001 | 50.648/<0.001 | ||
| t/Z/P-value (3-month vs 6-month Post) | 18.576/<0.001 | 18.211/<0.001 | ||
| Preoperative Tegner Score | 3.00 [2.00, 4.00] | 3.00 [2.00, 5.00] | 0.585 | 0.559 |
| 3-month Postoperative Tegner Score | 7.00 [6.00, 7.25] | 5.00 [5.00, 6.00] | 12.108 | <0.001 |
| 6-month Postoperative Tegner Score | 8.00 [8.00, 9.00] | 7.00 [6.00, 8.00] | 8.842 | <0.001 |
| t/Z/P-value (Pre vs 3-month Post) | 26.163/<0.001 | 10.809/<0.001 | ||
| t/Z/P-value (Pre vs 6-month Post) | 35.997/<0.001 | 20.867/<0.001 | ||
| t/Z/P-value (3-month vs 6-month Post) | 14.204/<0.001 | 15.360/<0.001 | ||
| Preoperative IKDC Score | 59.09±5.00 | 59.69±5.06 | 0.942 | 0.347 |
| 3-month Postoperative IKDC Score | 82.29±5.29 | 74.78±5.25 | -11.369 | <0.001 |
| 6-month Postoperative IKDC Score | 89.72±4.23 | 84.54±4.67 | -9.334 | <0.001 |
| t/Z/P-value (Pre vs 3-month Post) | 58.028/<0.001 | 31.949/<0.001 | ||
| t/Z/P-value (Pre vs 6-month Post) | 76.604/<0.001 | 52.631/<0.001 | ||
| t/Z/P-value (3-month vs 6-month Post) | 18.576/<0.001 | 20.682/<0.001 |
Note: IKDC: International Knee Documentation Committee.
Comparison of VAS score
Preoperative VAS scores showed no significant difference between the groups (P=0.250). At 3 and 6 months postoperatively, the early surgery group reported significantly lower VAS scores compared to the late surgery group (both P<0.001). Both groups showed significant pain reduction across all time intervals: preoperative versus 3 months, preoperative versus 6 months, and 3 months versus 6 months (all P<0.001) (Table 5).
Table 5.
Comparison of VAS score changes between the early and late surgery groups
| Variable | Early Group (n=148) | Late Group (n=112) | t/Z | P-value |
|---|---|---|---|---|
| Preoperative VAS Score | 7.00 [6.00, 8.00] | 7.00 [6.00, 8.00] | 1.150 | 0.250 |
| 3-month Postoperative VAS Score | 4.00 [4.00, 5.00] | 5.00 [5.00, 6.00] | 7.563 | <0.001 |
| 6-month Postoperative VAS Score | 2.00 [2.00, 2.00] | 3.50 [3.00, 4.00] | 10.515 | <0.001 |
| t/Z/P-value (Pre vs 3-month Post) | 21.677/<0.001 | <0.001 | ||
| t/Z/P-value (Pre vs 6-month Post) | 45.074/<0.001 | <0.001 | ||
| t/Z/P-value (3-month vs 6-month Post) | 22.59/<0.001 | <0.001 |
Note: VAS: Visual Analogue Scale.
Comparison of adverse events
Comparative analysis of adverse event incidence revealed no significant differences between the groups. Rates of joint effusion, joint swelling/pain, joint infection, and revision surgery requirements were similar across both groups (all P>0.05). These findings suggest that surgical timing does not significantly influence complication rates (Table 6).
Table 6.
Comparison of adverse events between the early and late surgery groups
| Variable | Early Group (n=148) | Late Group (n=112) | χ2 | P-value |
|---|---|---|---|---|
| Joint Effusion | 7/141 | 8/104 | 0.311 | 0.577 |
| Joint Swelling/Pain | 9/139 | 9/103 | 0.136 | 0.713 |
| Joint Infection | 3/145 | 2/110 | - | >0.999 |
| Revision Surgery | 3/145 | 3/109 | - | >0.999 |
Functional recovery distribution and outcomes
Prognostic evaluation of the 260 patients was based on Lysholm scores ≥90 and IKDC scores ≥85 at 6 months postoperatively. Of these, 109 patients achieved good recovery, while 151 had poor recovery. Distribution analysis based on the Lysholm and IKDC score thresholds revealed that 46 patients (17.69%) did not meet both criteria, indicating suboptimal functional recovery (Figure 3).
Figure 3.
Patient distribution based on Lysholm and IKDC score thresholds and score distributions. A. Patient Distribution Based on Lysholm and IKDC Score Thresholds. B. Lysholm Scores Distribution. C. IKDC Scores Distribution. Note: Lysholm Knee Scoring System (LKSS), and International Knee Documentation Committee (IKDC).
Independent risk factors for poor functional recovery
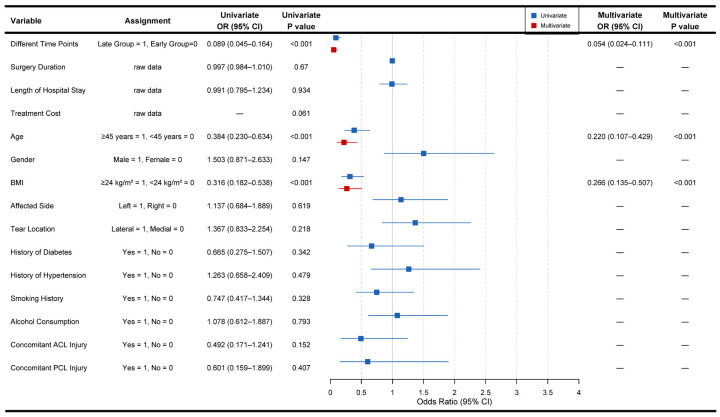
VIF analysis of all variables showed VIF values below 1.3, confirming the absence of multicollinearity among variables (Appendix 1). Univariate logistic regression analysis identified factors significantly associated with postoperative prognosis. Surgical timing strongly correlated with recovery outcomes (OR=0.089, 95% CI: 0.045-0.164, P<0.001). Age also significantly correlated with prognosis (OR=0.384, 95% CI: 0.23-0.634, P<0.001), and BMI was significantly associated with prognosis (OR=0.316, 95% CI: 0.182-0.538, P<0.001). Variables with no significant association with prognosis included operative time (OR=0.997, 95% CI: 0.984-1.01, P=0.670), hospital stay (OR=0.991, 95% CI: 0.795-1.234, P=0.934), treatment costs (OR=1, 95% CI: 1-1, P=0.061), gender (OR=1.503, 95% CI: 0.871-2.633, P=0.147), affected side (OR=1.137, 95% CI: 0.684-1.889, P=0.619), tear location (OR=1.367, 95% CI: 0.833-2.254, P=0.218), diabetes history (OR=0.665, 95% CI: 0.275-1.507, P=0.342), hypertension history (OR=1.263, 95% CI: 0.658-2.409, P=0.479), smoking history (OR=0.747, 95% CI: 0.417-1.344, P=0.328), alcohol consumption history (OR=1.078, 95% CI: 0.612-1.887, P=0.793), concomitant ACL injury (OR=0.492, 95% CI: 0.171-1.241, P=0.152), and concomitant PCL injury (OR=0.601, 95% CI: 0.159-1.899, P=0.407) (all P>0.05) (Figure 4).
Figure 4.
Patient distribution based on risk factors and odds ratios. Note: BMI: Body Mass Index.
Multivariate logistic regression analysis of independent risk factors
Multivariate logistic regression confirmed three independent risk factors for patient prognosis. Surgical timing remained highly significant (OR=0.054, 95% CI: 0.024-0.111, P<0.001). Age maintained its prognostic significance (OR=0.22, 95% CI: 0.107-0.429, P<0.001), and BMI continued to show an independent association with outcomes (OR=0.266, 95% CI: 0.135-0.507, P<0.001) (Figure 4).
Interaction analysis of functional recovery probability
Interaction analysis evaluated the impact of age, BMI, and surgical timing on functional recovery probability. Results showed that age significantly correlated with functional recovery probability (P=0.006). Different time points showed strong association with recovery outcomes (P<0.001), whereas BMI showed no significant association (P=0.124). The interaction effect between age and BMI was not significant (P=0.169) (Table 7). Figure 5 illustrates the interaction relationships between age, BMI, surgical timing, and recovery probability outcomes.
Table 7.
Logistic regression results of interaction analysis for functional recovery probability
| Variable | Estimate | Std. Error | Z | Pr(>|z|) |
|---|---|---|---|---|
| (Intercept) | -1.891 | 0.363 | -5.212 | <0.001 |
| Age | 1.172 | 0.423 | 2.768 | 0.006 |
| BMI | 0.785 | 0.510 | 1.539 | 0.124 |
| Different.Time.Points | 2.920 | 0.378 | 7.733 | <0.001 |
| Age:BMI | 0.932 | 0.677 | 1.377 | 0.169 |
Note: BMI: Body Mass Index.
Figure 5.
Interaction effects on functional recovery probability. A. The image displays the interaction effect of age on the probability of good (green line) versus poor (blue line) recovery. B. The image shows the interaction effect of BMI on the probability of good (green line) versus poor (blue line) recovery. C. The image illustrates the interaction effect of different time points on the probability of good (green line) versus poor (blue line) recovery. Note: BMI: Body Mass Index.
Discussion
Early arthroscopic meniscal repair (≤4 weeks) compared to late surgery (>4 weeks) significantly improved complete and overall healing rates. Additionally, early intervention reduced partial healing and non-healing proportions, demonstrating superior repair outcomes. At 3 and 6 months postoperatively, the early surgery group achieved higher Lysholm, Tegner, and IKDC scores than the late surgery group, resulting in better functional recovery and significantly lower VAS pain scores.
Our analysis revealed no significant differences between the groups in operative time, hospital stay, costs, or adverse event incidence, including effusion, swelling/pain, infection, and revision surgery. These findings suggest that early surgery does not increase complications or medical burden. Regression analysis identified surgical timing, age, and BMI as independent risk factors for poor functional recovery. Surgical timing and age had a greater influence, while BMI and its interaction with age showed a lesser impact.
Our meniscal healing results align with literature on ACL and multiligament injury (MLKI) meta-analyses. Vermeijden et al. [9] found that early surgery significantly reduced meniscal and cartilage damage in MLKI patients, but showed smaller effect differences in isolated ACL injuries. Our study, focusing on meniscal repair, confirms the advantages of early surgery in improving healing rates through MRI assessment based on Stoller grading. This improvement is likely due to early intervention reducing tissue degeneration and fibrosis while preserving the repair potential in the red zone.
van der List et al. [16] found that meniscal repair performed within 3 to 8 weeks significantly decreased failure rates. This finding is highly consistent with our conclusion that early surgery (≤4 weeks) improves healing rates. Their study further clarifies the critical window for surgical timing. Literature reporting indicates [10] that ACL reconstruction shows significant improvement in Lysholm and IKDC scores in early surgery groups, consistent with our findings of significant functional score enhancement in the early surgery group. This suggests that early surgery may optimize functional recovery through accelerated tissue repair.
James et al. [17] found that delayed ACL reconstruction (>12 weeks) significantly increased the risk of meniscal tears and irreparable meniscal damage. This supports our conclusion that early surgery reduces secondary meniscal damage. We also found that surgical timing had minimal impact on adverse events, likely due to advances in minimally invasive techniques, intraoperative PRP injection, and standardized postoperative anticoagulation and rehabilitation protocols, which reduce the risk of complications.
The literature shows [18] that early MLKI surgery improves Lysholm, IKDC, and Tegner scores while reducing cartilage damage, which aligns with our findings of improved functional scores and reduced secondary damage in the early surgery group. Shamrock et al. [19] showed that delayed MLKI reconstruction (>6 weeks) increases the risk of meniscal and cartilage damage, further supporting our conclusions that delayed surgery increases meniscal damage, providing additional evidence for prioritizing early surgery.
Nepple et al. [20] found that the 5-year failure rate for modern meniscal repair reached 19.5%, with medial meniscal repairs showing higher failure rates than lateral ones (23.9% vs. 12.6%, P=0.04). This finding provides an important reference for discussing meniscal healing rates and long-term outcomes of repairs in different locations, which is relevant to our study.
Our research provides valuable clinical evidence for optimizing the surgical timing of meniscal injuries. Early surgery (≤4 weeks) demonstrates significant advantages in improving meniscal healing rates, enhancing knee function, and reducing pain. This suggests that clinical practice should prioritize early surgical intervention following injury to optimize tissue repair capacity and minimize secondary damage risks.
Literature reports indicate [21] that in patients aged ≥40 years, delayed surgery led to preoperative deterioration of isolated meniscal tears. In this population, 48.3% of patients experienced worsening of their meniscal tears, directly supporting our conclusion that delayed surgery accelerates meniscal damage. Sadoghi et al. [22] found that delayed meniscal repair (>12 weeks) reduced functional outcomes in ACL reconstruction (IKDC scores). This further validates the benefits of early meniscal repair for improving functional recovery.
Javid et al. [23] demonstrated that early meniscal repair improved Lysholm scores and reduced medial meniscal extrusion. However, some studies found no significant impact of surgical timing on outcomes, offering a comparative basis for discussing the heterogeneity in isolated repairs in our study.
Age and BMI were identified as independent risk factors for poor functional recovery, highlighting the need for particular attention to elderly patients and those with high BMI during preoperative assessments. This suggests that tailored postoperative rehabilitation plans, such as extended low weight-bearing phases or more intensive functional exercises, could optimize prognosis. Research shows [24] that BHMT repair failure rates reached 14.8%, with higher failure rates observed in isolated and medial meniscal tear repairs. This provides a valuable comparative basis for discussing healing rates and failure risks in our study.
Our finding that operative time, hospital stay, and treatment costs showed no significant differences between the groups suggests that early surgery enhances therapeutic efficacy without increasing the medical resource burden. This is important for guiding medical institutions in optimizing resource allocation. Zsidai et al. [25] demonstrated that delayed PCL reconstruction (>12 weeks) increased cartilage damage and the frequency of medial meniscal surgeries. This is consistent with our conclusion that delayed surgery increases meniscal damage risks, further supporting the advantages of early surgery in reducing secondary damage. Our study provides evidence for developing clinical guidelines on the diagnosis and treatment of meniscal injuries. We recommend early surgery as the preferred strategy, incorporating patient characteristics into management plans to maximize clinical efficacy.
Strengths of our study include a sufficient sample size (260 cases, early group: 148 cases, late group: 112 cases) based on meta-analysis sample size calculations, ensuring high statistical power. We assessed meniscal healing using MRI (Stoller grading) and combined it with functional assessments using Lysholm, Tegner, IKDC, and VAS scores to provide a comprehensive measure of surgical timing efficacy. Our statistical analysis was rigorous, employing VIF analysis to exclude multicollinearity, and we used both univariate and multivariate logistic regression to identify independent risk factors. Interaction analysis further explored the combined effects of age, BMI, and surgical timing, enhancing the scientific validity and credibility of our results.
Data sources from electronic medical records and outpatient follow-up records were systematic and comprehensive, ensuring accuracy and completeness. Although the proportion of patients with concomitant ACL or PCL injuries was relatively low, univariate logistic regression analysis showed no significant association with poor functional recovery. However, the literature indicates [9] that concomitant ligament injuries can influence surgical timing decisions, with early surgery offering greater advantages in reducing secondary damage.
In our study, the early surgery group’s superior healing rates may partially stem from early intervention in patients with concomitant injuries, which helps reduce tissue degeneration. Postoperative management measures, such as PRP injection, low-molecular-weight heparin anticoagulation, and early rehabilitation training, may have reduced adverse event differences by promoting tissue repair and preventing complications like VTE, further supporting the safety and efficacy of early surgery.
Limitations of our study include its retrospective design, which may introduce selection bias due to non-randomized grouping influenced by conservative treatment or delayed surgery. Additionally, the 6-month postoperative follow-up is insufficient to assess long-term outcomes like osteoarthritis, as the literature reports that meniscal injury complications may develop years after surgery. We also used stricter recovery criteria (Lysholm ≥90, IKDC ≥85) compared to common clinical standards (Lysholm ≥80, IKDC ≥70) to enhance rigor, but this may have led to more patients being classified as “poorly recovered” despite adequate clinical recovery. Prior analysis using lower criteria identified only 6 cases of poor recovery, whereas the stricter criteria increased this proportion, highlighting the need to balance rigorous standards with clinical reality. Furthermore, the small number of patients with concomitant ACL or PCL injuries may have slightly affected healing and functional recovery, though univariate analysis showed no significant association. Finally, not subdividing meniscal tear types (e.g., longitudinal or bucket-handle tears) for their specific impact on surgical timing limits the generalizability of our results. Future studies will include longer-term follow-up (2-5 years postoperatively) to assess osteoarthritis and functional recovery. We also plan to conduct randomized controlled trials to eliminate selection bias, perform subgroup analyses on age, BMI, and tear types, and explore the interactions between suture techniques and surgical timing to refine our conclusions.
Conclusion
Our study demonstrates that early surgery (≤4 weeks) for arthroscopic meniscal repair significantly improves healing rates, enhances knee function recovery, and reduces pain scores. Importantly, this does not increase the incidence of adverse events or medical resource burden. We identified surgical timing, age, and BMI as independent risk factors for poor functional recovery, with early surgery showing particularly pronounced benefits for functional restoration. These findings provide scientific evidence for the clinical optimization of surgical timing.
Acknowledgements
This study was supported by the 2024 Putuo District Central Hospital to introduce talent start-up fund (No. 2024-YJRC-03).
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Zhang X, Zhou J, Jin X, Ji Y, Wang K. Diagnostic accuracy of MRI in knee meniscus tear and ACL injury. Altern Ther Health Med. 2024;30:136–139. [PubMed] [Google Scholar]
- 2.Hanna T, Smith NP, Sebastianelli WJ. Treatment, return to play, and performance following meniscus surgery. Curr Rev Musculoskelet Med. 2022;15:157–169. doi: 10.1007/s12178-022-09754-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Roy L, Warnecke D, Hacker SP, Simon U, Dürselen L, Ignatius A, Seitz AM. Meniscus injury and its surgical treatment does not increase initial whole knee joint friction. Front Bioeng Biotechnol. 2021;9:779946. doi: 10.3389/fbioe.2021.779946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hiranaka T, Furumatsu T, Okazaki Y, Kintaka K, Kamatsuki Y, Zhang X, Xue H, Ozaki T. Postoperative external tibial rotation is correlated with inferior meniscal healing following pullout repair of a medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2022;30:1491–1498. doi: 10.1007/s00167-021-06656-y. [DOI] [PubMed] [Google Scholar]
- 5.Saint-Etienne A, Benhenneda R, Vieira TD, Fayard JM, Thaunat M. Clinical outcomes of different management techniques for medial meniscal type 3 ramp lesions in anterior cruciate ligament reconstruction: a comparative analysis between all-inside repair, suture hook repair, and lesions left in situ. Am J Sports Med. 2024;52:1250–1257. doi: 10.1177/03635465241232088. [DOI] [PubMed] [Google Scholar]
- 6.Bierke S, Abdelativ Y, Hees T, Karpinksi K, Häner M, Park H, Petersen W. Risk of arthrofibrosis in anatomical anterior cruciate ligament reconstruction: the role of timing and meniscus suture. Arch Orthop Trauma Surg. 2021;141:743–750. doi: 10.1007/s00402-020-03464-w. [DOI] [PubMed] [Google Scholar]
- 7.Moon HS, Choi CH, Jung M, Chung K, Jung SH, Byun J, Kim JG, Kim SH. Association between insufficient restoration of meniscal tension during surgical repair of medial meniscus root tear and surgical outcomes: clinical implication of curtain-cliff sign. Am J Sports Med. 2025;53:163–171. doi: 10.1177/03635465241293733. [DOI] [PubMed] [Google Scholar]
- 8.Willinger L, Herbst E, Diermeier T, Forkel P, Woertler K, Imhoff AB, Achtnich A. High short-term return to sports rate despite an ongoing healing process after acute meniscus repair in young athletes. Knee Surg Sports Traumatol Arthrosc. 2019;27:215–222. doi: 10.1007/s00167-018-5335-2. [DOI] [PubMed] [Google Scholar]
- 9.Vermeijden HD, Yang XA, Rademakers MV, Kerkhoffs GMMJ, van der List JP, DiFelice GS. Early and delayed surgery for isolated ACL and multiligamentous knee injuries have equivalent results: a systematic review and meta-analysis. Am J Sports Med. 2023;51:1106–1116. doi: 10.1177/03635465211069356. [DOI] [PubMed] [Google Scholar]
- 10.Shen X, Liu T, Xu S, Chen B, Tang X, Xiao J, Qin Y. Optimal timing of anterior cruciate ligament reconstruction in patients with anterior cruciate ligament tear: a systematic review and meta-analysis. JAMA Netw Open. 2022;5:e2242742. doi: 10.1001/jamanetworkopen.2022.42742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deviandri R, van der Veen HC, Lubis AM, Postma MJ, van den Akker-Scheek I. Responsiveness of the indonesian versions of the anterior cruciate ligament-return to sport after injury score, the international knee documentation committee subjective knee form, and the lysholm score in patients with ACL injury. Orthop J Sports Med. 2023;11:23259671231191827. doi: 10.1177/23259671231191827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klasan A, Putnis SE, Grasso S, Kandhari V, Oshima T, Parker DA. Tegner level is predictive for successful return to sport 2 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29:3010–3016. doi: 10.1007/s00167-020-06335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shephard L, Abed V, Nichols M, Kennedy A, Khalily C, Conley C, Jacobs C, Stone AV. International knee documentation committee (IKDC) is the most responsive patient reported outcome measure after meniscal surgery. Arthrosc Sports Med Rehabil. 2023;5:e859–e865. doi: 10.1016/j.asmr.2023.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Todor A, Vermesan D, Haragus H, Patrascu JM Jr, Timar B, Cosma DI. Cross-cultural adaptation and validation of the Romanian International Knee Documentation Committee-subjective knee form. PeerJ. 2020;8:e8448. doi: 10.7717/peerj.8448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee J, Lee DW, Kyeong TH, Lee JW, Kim JG. Single-incision bone bridge lateral meniscus allograft transplantation: preserving neurovascular safety with promising results for posterior horn distortion and graft maturation. Knee Surg Sports Traumatol Arthrosc. 2023;31:5864–5872. doi: 10.1007/s00167-023-07641-3. [DOI] [PubMed] [Google Scholar]
- 16.van der List JP, Daniel S, Blom I, Benner JL. Early meniscal repair leads to higher success rates than delayed meniscal repair: a systematic review and meta-analysis. Am J Sports Med. 2025;53:2761–2770. doi: 10.1177/03635465241298619. [DOI] [PubMed] [Google Scholar]
- 17.James EW, Dawkins BJ, Schachne JM, Ganley TJ, Kocher MS PLUTO Study Group. Anderson CN, Busch MT, Chambers HG, Christino MA, Cordasco FA, Edmonds EW, Green DW, Heyworth BE, Lawrence JTR, Micheli LJ, Milewski MD, Matava MJ, Nepple JJ, Parikh SN, Pennock AT, Perkins CA, Saluan PM, Shea KG, Wall EJ, Willimon SC, Fabricant PD. Early operative versus delayed operative versus nonoperative treatment of pediatric and adolescent anterior cruciate ligament injuries: a systematic review and meta-analysis. Am J Sports Med. 2021;49:4008–4017. doi: 10.1177/0363546521990817. [DOI] [PubMed] [Google Scholar]
- 18.Vaishya R, Patralekh MK, Vaish A, Tollefson LV, LaPrade RF. Effect of timing of surgery on the outcomes and complications in multi-ligament knee injuries: an overview of systematic reviews and a meta-analysis. Indian J Orthop. 2024;58:1175–1187. doi: 10.1007/s43465-024-01224-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shamrock AG, Hall JR, Hajewski CJ, An Q, Duchman KR. Cartilage and meniscus injuries are more common in patients undergoing delayed multiligament reconstruction. J Knee Surg. 2022;35:560–565. doi: 10.1055/s-0040-1716378. [DOI] [PubMed] [Google Scholar]
- 20.Nepple JJ, Block AM, Eisenberg MT, Palumbo NE, Wright RW. Meniscal repair outcomes at greater than 5 years: a systematic review and meta-analysis. J Bone Joint Surg Am. 2022;104:1311–1320. doi: 10.2106/JBJS.21.01303. [DOI] [PubMed] [Google Scholar]
- 21.Yokoe T, Tajima T, Yamaguchi N, Morita Y, Chosa E. A longer duration from injury to surgery is associated with preoperative deterioration of an isolated meniscal tear in patients aged 40 years or older. J Orthop Surg (Hong Kong) 2022;30:10225536221101692. doi: 10.1177/10225536221101692. [DOI] [PubMed] [Google Scholar]
- 22.Sadoghi P, Widhalm HK, Fischmeister MF, Leitner L, Leithner A, Fischerauer SF. Delayed meniscus repair lowers the functional outcome of primary ACL reconstruction. J Clin Med. 2024;13:1325. doi: 10.3390/jcm13051325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Javid K, Akins X, Lemaster NG, Ahmad A, Stone AV. Impact of time between meniscal injury and isolated meniscus repair on post-operative outcomes: a systematic review. World J Clin Cases. 2025;13:95004. doi: 10.12998/wjcc.v13.i7.95004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Costa GG, Grassi A, Zocco G, Graceffa A, Lauria M, Fanzone G, Zaffagnini S, Russo A. What is the failure rate after arthroscopic repair of bucket-handle meniscal tears? A systematic review and meta-analysis. Am J Sports Med. 2022;50:1742–1752. doi: 10.1177/03635465211015425. [DOI] [PubMed] [Google Scholar]
- 25.Zsidai B, Engler ID, Narup E, Lin RT, Nazzal EM, Winkler PW, Samuelsson K, Irrgang JJ, Musahl V. Delayed multiligament PCL reconstruction is associated with a higher prevalence of intraarticular injury and may influence treatment. BMC Musculoskelet Disord. 2023;24:502. doi: 10.1186/s12891-023-06638-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.