Abstract
Introduction
In this prospective, randomized controlled study, we aimed to evaluate the effect of IgM-enriched immunoglobulin treatment on progression of organ failure and septic shock in patients with severe sepsis.
Materials and methods
Forty-two patients with severe sepsis were enrolled in the study. Patients in the study group (n = 21) received an intravenous immunoglobulin preparation (Pentaglobin®) in addition to standard therapy. Pentaglobin® therapy was commenced on the day of diagnosis of severe sepsis: 5 ml/kg per day Pentaglobin® (38 g/l IgG, 6 g/l IgM, and 6 g/l IgA) was infused over 6 hours and repeated for 3 consecutive days. Patients in the control group (n = 18) received standard sepsis therapy, but no immunoglobulin administration. Blood samples for procalcitonin (PCT) measurements were taken daily for 8 days. Severity of critical illness and development of organ failure were assessed by obtaining daily acute physiological and chronic health evaluation (APACHE) II and sequential organ failure assessment (SOFA) scores.
Results and discussion
Procalcitonin levels showed a statistically significant decrease in the Pentaglobin® group (P < 0.001); however, an improvement in SOFA scores could not be demonstrated. Procalcitonin levels and SOFA scores did not change significantly in the control group. Septic shock incidence (38% versus 57%) and 28-day mortality rate (23.8% versus 33.3%) were found to be similar between the Pentaglobin® and control groups. The evaluation of serial APACHE II scores did not demonstrate a difference between Pentaglobin® and control groups either.
Conclusion
Present data could not demonstrate any beneficial effects of polyclonal immunoglobulin preparation Pentaglobin® on organ morbidity, septic shock incidence and mortality rate in patients with severe sepsis.
Keywords: APACHE II score, Pentaglobin®, procalcitonin, severe sepsis, SOFA score
Introduction
Despite developing therapeutic strategies and new antibiotic regimens, mortality of sepsis and septic shock has actually remained at a level of about 35–50%. Novel anti-inflammatory treatment regimens such as anti-tumor necrosis factor, anti-platelet-activating factor, anti-interleukin-1, anti-endotoxin, anti-bradykinin, inhibitors of nitric oxide synthase and steroids have also yielded disappointing results until now [1,2].
Systemic inflammatory response syndrome and sepsis are diseases of the immune system rather than simple effects of a causative agent. An immunotherapeutic approach that acts through neutralization of endotoxin and various bacterial products by passive administration of intravenous immunoglobulin (ivIg) seems to be promising in clinical practice, rather than target one mediator of the inflammatory cascade. Besides the effect of immunoglobulin substitution in a case of deficiency, several other mechanisms, such as neutralizing endotoxins and exotoxins, scavenging active complement components, as well as lipopolysaccharides, stimulating opsonic and bactericidal activity in serum, reducing pro-inflammatory mediators, and increasing anti-inflammatory mediators, have been postulated for the possible beneficial effects of ivIg in septic patients.
It has been previously shown that commercial ivIgG products contained antibodies against Gram-negative and Gram-positive bacteria, often encountered in the intensive care unit [3]. In a recent study, Trautmann et al. [4] showed that antibodies against lipopolysaccharides of Escherichia coli, Pseudomonas aeruginosa and Klebsiella spp. are much more concentrated in human IgM fraction.
In this prospective, randomized controlled study, we aimed to evaluate the effect of IgM-enriched immunoglobulin treatment on progression of organ failure and septic shock in patients with severe sepsis.
Materials and methods
Patients
After approval by the faculty ethics committee, patients with severe sepsis (temperature >38°C or <36°C, heart rate >90 beats/min, respiratory rate >20/min or PaCO2 < 32 mmHg, white blood cell count >12,000/mm3 or <4000/mm3, documented infection and dysfunction of an organ or hypotension) were enrolled in the study.
Study design
Patients were randomly allocated to the study groups according to the numerical order of a computer-generated randomization list. Patients in the study group (n = 21) received ivIg preparation in addition to standard sepsis therapy. Polyclonal ivIg treatment (Pentaglobin®, Biotest Pharma GmbH, Dreieich, Germany) was started on the day of diagnosis of severe sepsis: 5 ml/kg per day Pentaglobin® (38 g/l IgG, 6 g/l IgM and 6 g/l IgA) was infused intravenously over a period of 6 hours and repeated for 3 consecutive days. Patients in the control group (n = 18) received standard sepsis therapy, but no immunoglobulin administration.
Electrocardiogram, invasive arterial blood pressure and central venous pressure were monitored continuously (Horizon XL; Mennen Medical, Rehovot, Israel). The aim was to achieve a central venous pressure of 8–12 mmHg. Dopamine, dobutamine, epinephrine and/or norepinephrine were used to treat hypoperfusion that was unresponsive to volume resuscitation. Oliguria and fluid overload were treated by hemofiltration, if adequate urine flow could not be obtained by medical therapy. Steroids were not used in any of the patients. Septic shock was diagnosed when severe sepsis was associated with hypotension (systolic blood pressure <90 mmHg or a reduction of >40 mmHg from baseline, in the absence of other cause for hypotension) despite adequate fluid resuscitation. Pulmonary artery catheterization was performed following the diagnosis of septic shock.
Measurements
Blood samples for procalcitonin (PCT) measurements were taken daily for 8 days following study admission. Samples were obtained from an arterial catheter every morning and the samples were processed by the same person in the laboratory of the Medical Biology Department. PCT was determined with an immunoluminometric assay, allowing quantitative measurement of a wide range of PCT concentrations (B.R.A.H.M.S. Diagnostica GmbH, Berlin, Germany).
Severity of critical illness was assessed by obtaining daily acute physiological and chronic health evaluation score (APACHE II). Sequential organ failure assessment (SOFA) score was used to assess the development of organ failure, and in an attempt to describe the degree of organ failure over time in individual septic patients. Duration of mechanical ventilation, length of stay in the intensive care unit, septic shock incidence and 28-day mortality rate were also recorded.
Appropriate microbial samples were obtained before prescribing any prophylactic and pre-emptive medication, and if this was not possible then the probable causative agents were considered and therapy was administered accordingly. All isolated bacteria were identified and antimicrobial susceptibilities of isolates were determined by the disk diffusion method described in NCCLS M2-A6 and M100-S8 [5,6]. In these patients with sepsis, all samples, especially blood cultures, should be obtained as soon as possible and before any changes are made in antimicrobial therapy.
Statistical analysis
Data are presented as mean ± SD or median (range) for data that were not normally distributed. Admission data are assessed using an unpaired t-test. Demographic and outcome data were examined on the basis of intention-to-treat analysis. Mortality rate, septic shock incidence and gender were compared using Fisher's exact test. The Mann–Whitney U-test was used for comparison of quantitative variables between the groups. PCT values, SOFA and APACHE II scores were not normally distributed; these were analyzed with Friedman analysis of variance on ranks. In case of statistical significance, intragroup analyses were performed using the Wilcoxon test. A P value less than 0.05 was considered significant. Data analyses and statistics were performed using SPSS for Windows v. 10.0.1.
Results
Forty-two patients were randomly allocated into two groups. Three patients from the control group were excluded because of technical problems during laboratory analysis. Demographic data and clinical characteristics of the patients are presented in Table 1. Both groups were comparable with respect to their admission APACHE II and SOFA scores. Infection sources and causative organisms obtained are shown in Table 2.
Table 1.
Clinical characteristics of patients on admission
| Characteristic | Pentaglobin® group (n = 21) | Control group (n = 21) | P |
| Age (range) | 42.0 ± 18 (10–72) | 49.3 ± 20.6 (20–76) | 0.23 |
| Gender (F/M) | 9/12 | 11/10 | 0.75 |
| APACHE II | 10.5 ± 4.6 | 14.0 ± 8.5 | 0.10 |
| SOFA | 5.0 ± 2.7 | 5.7 ± 4.0 | 0.50 |
| GCS | 14.2 ± 2.1 | 12.9 ± 4.0 | 0.20 |
Values are expressed as mean ± SD. APACHE II, acute physiological and chronic health evaluation; F/M, female/male; GCS, Glasgow Coma Scale; SOFA, sequential organ failure assessment.
Table 2.
Sources of infection and causative organisms
| Criterion | Pentaglobin® group | Control group |
| Sources of infection | Abdominal sepsis 11 (52.4) | Abdominal sepsis 9 (42.8) |
| Urosepsis 1 (4.8) | Urosepsis 2 (9.5) | |
| Pneumonia 5 (23.8) | Pneumonia 9 (42.8) | |
| CNS infection 3 (14) | Pericarditis 1 (4.7) | |
| Endocarditis 1 (4.8) | ||
| Causative organisms | P. aeruginosa 5 (23.8) | P. aeruginosa 5 (23.8) |
| MRSA 9 (42.8) | MRSA 5 (23.8) | |
| Acinetobacter sp. 1 (4.8) | Acinetobacter sp. 4 (19) | |
| K. pneumoniae 1 (4.8) | K. pneumoniae 1 (4.7) | |
| Enterobacter sp. 1 (4.8) | E. coli 1 (4.7) | |
| S. maltophilia 1 (4.8) | Undetermined 5 (23.8) | |
| Undetermined 3 (14) |
Values are expresed as n (%). Pentaglobin® group (n = 21); control group (n = 21). CNS, central nervous system; MRSA, methicillin-resistant Staphylococcus aureus; E. coli, Escherichia coli; K. pneumoniae, Klebsiella pneumoniae; P. aeruginosa, Pseudomonas aeruginosa; S. maltophilia, Stenotrophomonas maltophilia.
Thirteen patients (72%) in the control group and 14 patients (67%) in the Pentaglobin® group had sepsis resulting from infection with Gram-negative microorganisms. Mortality rates of those sub-groups of patients were 23% in the control group and 14% in the Pentaglobin® group (P = 0.6).
PCT levels showed a statistically significant decrease in the Pentaglobin® group (P < 0.001); however, an improvement in SOFA scores could not be demonstrated. PCT levels and SOFA scores did not change significantly in the control group (Table 3). Daily PCT levels and SOFA scores of both groups are shown in Figs 1 and 2.
Table 3.
Procalcitonin levels, SOFA and APACHE II scores
| Measurement | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 | ANOVA |
| PCT (ng/mL) | |||||||||
| Pentaglobin® | 5.5 (0.9–72.0) | 3.5* (0.9–65.0) | 3.5** (0.9–39.0) | 3.05* (0.9–23.0) | 2.6* (0.8–11.0) | 2.45 (0.6–11.0) | 2.0* (0.6–11.0) | 1.45** (0.6–14.3) | <0.001 |
| Control | 4.0 (0.4–194.0) | 3.14 (0.4–72.0) | 3.2 (0.2–34.0) | 2.65 (0.6–18.0) | 3.15 (0.5–14.0) | 4.0 (0.6–21.6) | 4.0 (0.3–117.0) | 4.0 (0.5–185.0) | 0.8 |
| SOFA | |||||||||
| Pentaglobin® | 5.0 (1.0–10.0) | 6.0 (1.0–11.0) | 6.0 (0–12) | 5.0 (0–16) | 4.0 (0.0–16.0) | 4.0 (0–16) | 3.5 (0.0–15.0) | 4.0 (0–14) | 0.2 |
| Control | 4.5 (1.0–12.0) | 5.5 (1.0–15.0) | 5.0 (2–15) | 5.0 (2–12) | 4.5 (1.0–10.0) | 5.0 (1–11) | 4.0 (1.0–11.0) | 6.0 (0–10) | 0.3 |
| APACHE II | |||||||||
| Pentaglobin® | 15.0 (9–24) | 14.0 (8.0–28.0) | 14.0 (7–24) | 13.0 (7–30) | 11.0 (5.0–30.0) | 11.5* (5.0–30.0) | 12.5 (5.0–30.0) | 8.0** (5–30) | < 0.001 |
| Control | 16.0 (3–27) | 15.5 (5.0–27.0) | 16.0 (5–24) | 15.0 (4–22) | 11.5** (3.0–21.0) | 11.0** (1.0–27.0) | 11.0** (1.0–21.0) | 11.0** (1–16) | < 0.001 |
Values are expressed as median (range). ANOVA, analysis of variance; APACHE II, acute physiological and chronic health evaluation; PCT, procalcitonin; SOFA, sequential organ failure assessment. *P < 0.05, **P < 0.01 when compared to Day 1.
Figure 1.
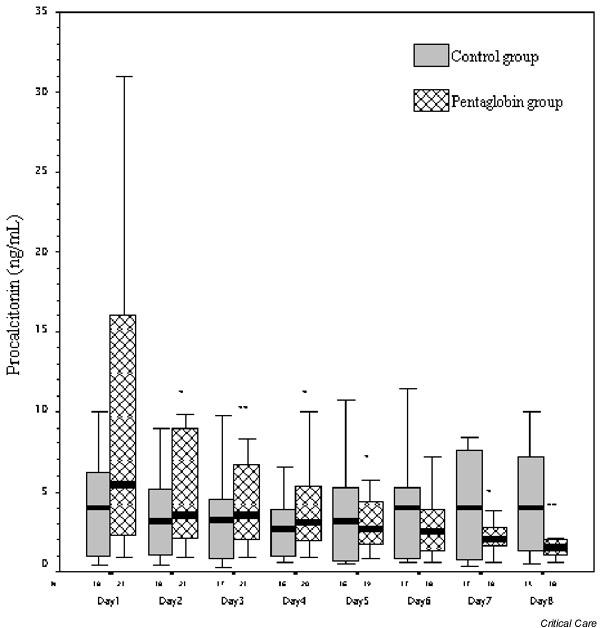
Procalcitonin plasma concentrations of patients in Pentaglobin® and control groups. Indicated are median (inner line), 25/75 percentiles (box) and 10/90 percentiles (whisker) obtained during an 8-day observation period. *P < 0.05, **P < 0.01 when compared to Day 1.
Figure 2.
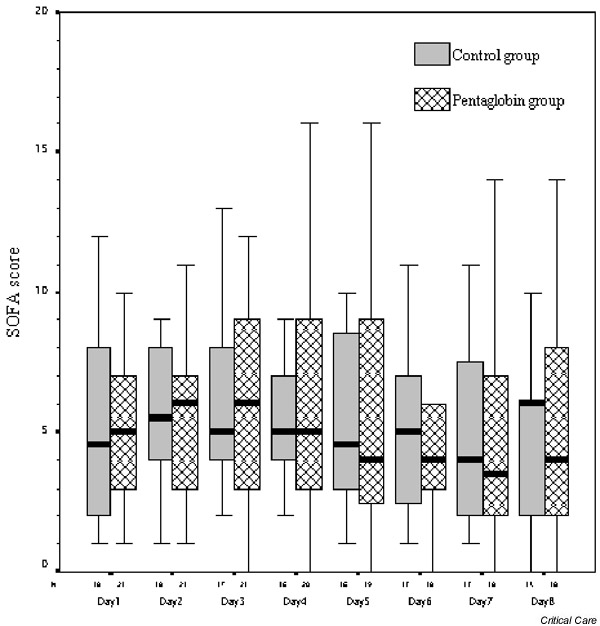
Sequential organ failure assessment (SOFA) scores of patients in Pentaglobin® and control groups. Indicated are median (inner line), 25/75 percentiles (box) and 10/90 percentiles (whisker) obtained during an 8-day observation period.
APACHE II scores showed a statistically significant decrease in the Pentaglobin® and control groups (P < 0.001 in both groups). PCT levels, SOFA and APACHE II scores did not demonstrate statistically significant differences between the groups on each evaluation day.
Duration of mechanical ventilation, length of intensive care stay, septic shock incidence and 28-day mortality rate were found to be similar between the groups (Table 4).
Table 4.
Clinical outcome of patients
| Criterion | Pentaglobin® group | Control group | P |
| Septic shock incidence (%) | 8/21 (38) | 12/21 (57) | 0.35 |
| Duration of mechanical ventilation (days) | 20 (2–58) | 19 (2–76) | 0.60 |
| ICU length of stay (days) | 29 (3–89) | 22 (3–85) | 0.35 |
| 28-day mortality (%) | 5/21 (23.8) | 7/21 (33.3) | 0.70 |
Values are expresed as median (range). Pentaglobin® group (n = 21); control group (n = 21). ICU, intensive care unit.
Discussion
In the present study, the use of IgM-enriched and IgA-enriched IgG preparation in addition to standard sepsis therapy could not produce an improvement in any of the outcome measures of patients with severe sepsis. The only encouraging observation was the reduction in PCT levels obtained with Pentaglobin® administration.
In the previous studies [4,7] specific IgM and IgG antibodies against lipopolysaccharides of Escherichia coli strains, Klebsiella pneumoniae, Pseudomonas aeruginosa, α-haemolysin of Staphylococcus aureus, and against surface proteins of oxacillin-resistant S. aureus and vancomycin-resistant streptococci were detected in Pentaglobin® solution. When using in vitro cell cultures, Pentaglobin® preparation produced the highest inhibition of tumor necrosis factor α release when added to the medium with lipopolysaccharide [8]. Rieben et al. [9] showed that IgM enrichment of ivIg preparations leads to an enhanced complement-inhibitory capacity both in vitro and in vivo as compared with pure ivIgG.
Monoclonal (IgG) and polyclonal (IgGMA) immunoglobulin solutions have previously been applied to different groups of intensive care patients. Both IgG and IgGMA have been used prophylactically in high-risk patients after cardiac surgery and resulted in an improvement in infectious morbidity and in a reduction in mortality rate [10,11,12]. However, consistent reductions in mortality could not be demonstrated in placebo-controlled trials performed in sepsis or septic shock. IgG was applied to 653 sepsis patients having an APACHE II score higher than 20; a moderate improvement was obtained in severity of sepsis, but the mortality rate could not be reduced [13]. De Simone et al. [14] used IgG solution in patients with severe sepsis and obtained reductions in hospitalization and number of days on antibiotics, as well as in the number of positive cultures; however, the mortality rate (75% control versus 58% ivIgG) was unchanged. Similarly, Just et al. [15] (41% control versus 44% ivIgGMA), Jesdinsky et al. [16] (41% control versus 46% ivIgG, ivIgGMA) and Vogel [17] (44% control versus 24% ivIgGMA) were also not able to demonstrate reductions in mortality rate by IgGMA application to different intensive care patients with sepsis.
On the other hand, impressive improvement in outcome for septic patients was reported in certain investigations using ivIg preparations [18,19]. In a study performed by Dominioni et al. [18], the mortality rate was reduced by administration of the IgG solution from 67% to 38% in postoperative septic patients having a sepsis score higher than 20. Schedel et al. [19] reported a statistically significant decrease in the APACHE II score beyond the fifth day after inclusion, as well as a decrease in the 6-week mortality rate (1/27 in the Pentaglobin® group versus 9/28 in the control group) in septic shock patients receiving Pentaglobin® treatment. Serum concentrations of endotoxin-equivalent were also found to be decreased significantly within 24 hours after inclusion of the patients in the study in patients treated with Pentaglobin®. The Cochrane group analyzed 23 controlled clinical studies published between 1966 and 1999 and found that sepsis-related mortality was significantly reduced only in patients who received polyclonal ivIg in contrast to treatment with monoclonal antibodies and anti-cytokines in sepsis and septic shock [20].
Our results could not make a clear-cut contribution to the conflicting data obtained from trials studying the effects of the different types of immunoglobulin preparations in septic patients. As well as the use of different antibiotics, other treatment strategies, such as the use of catecholamines, corticosteroids or hemofiltration have the potential to interact with the immune system and, therefore, with the response of the patients. If we examine possible explanations for inconsistency of the literature, the dosage and application schedule as well as the timing of immunomodulatory therapy should also be taken into consideration. Almost all investigators applied a total amount of approximately 1 l Pentaglobin® 5% during 3 consecutive days in previous studies. The stage of the disease at which immunoglobulin substitution was performed might be an important determinant of the response of the patients. The most striking data about the beneficial effects of polyclonal immunoglobulin were presented by Schedel et al. [19] in septic shock patients. Dominioni et al. [18], also reported impressive mortality reduction with the IgG preparation in septic patients with a sepsis score higher than 20.
It is now well known that systemic inflammatory response syndrome is the result of the imbalance between proinflammatory and anti-inflammatory forces. The compensatory anti-inflammatory response is assumed to lead to an increased susceptibility to infection or anergy, whereas systemic overflow of the proinflammatory system may lead to apoptosis, organ dysfunction, and thus septic shock. The anti-inflammatory potential of Pentaglobin® may not show clear benefits, or may even be harmful, in cases or at disease stages in which proinflammatory forces are not dominant. According to this paradigm, a more precise understanding of the laboratory and clinical information of the immune status of patients will help with administering the right drug at the right time for the right patient.
It was suggested that a single therapeutic method of immunoglobulin substitution in the therapy of this complex syndrome might accomplish the goal of improvement in morbidity, instead of expecting a magic approach to reducing the mortality rate in sepsis. In this study, the SOFA score was used to describe the damage to the different organ systems, as well as the impact of the therapy on the progression of organ dysfunction. With regard to the SOFA scores, which did not demonstrate an improvement in organ morbidity throughout the 8-day follow-up period, this proposal was not supported by our findings.
PCT is a pro-hormone that shows elevated plasma levels in severe bacterial, fungal and parasitic infections, as well as in sepsis and multiorgan failure. It has been used not only in the diagnosis of sepsis but also in treatment of the clinical course of the disease [21,22]. In contrast to the control group, this marker demonstrated a consistent decline in patients treated with Pentaglobin® preparation. However, the decline in PCT levels did not correspond with the clinical course of severe sepsis, which was reflected in unchanged SOFA scores throughout the study. The evaluation of serial APACHE II scores also did not demonstrate a difference between the Pentaglobin® and control groups.
In our study there are some limitations that should be noted. Restricting the investigation period to only 8 days might have hampered the detection of an improvement in SOFA scores of the patients. We suggest that extending the duration of data collection might allow the change in PCT levels to be accompanied by an improvement of the severity of organ dysfunction. The increase in PCT levels on days 6–8 could possibly reflect a septic relapse in some of the patients in the control group. Because cytokine levels were not measured in the present study, we could not comment on the possible role of Pentaglobin® in the prevention of a similar relapse in the treatment group. Our study was performed in a relatively small group of patients with severe sepsis. Increasing the number of patients could confirm a change in the severity of organ dysfunction, the incidence of septic shock and mortality rate as a result of using Pentaglobin®.
Conclusion
In conclusion, our data could not demonstrate any beneficial effects of the polyclonal immunoglobulin preparation Pentaglobin® on organ morbidity, septic shock incidence and mortality rate in patients with severe sepsis. We believe that further investigations should focus on laboratory and clinical measures to identify and monitor patients who might benefit from specific immunomodulatory therapies.
Key messages
· The aim of this prospective study is to evaluate the effect of IgM-enriched immunoglobulin treatment on progression of organ failure and septic shock in patients with severe sepsis.
· Reduction in PCT levels observed with PentaglobinR administration was a striking observation of the study.
· Serial SOFA and APACHE II scores did not reveal significant differences between the groups.
· The decline in PCT levels did not correspond with the clinical course of severe sepsis in the PentaglobinR group.
· Present data could not demonstrate any beneficial effects of polyclonal immunoglobulin preparation on organ morbidity, septic shock incidence and mortality rate in patients with severe sepsis.
Competing interests
None declared.
Abbreviations
APACHE II = acute physiological and chronic health evaluation II; ivIg = intravenous immunoglobulin; PCT = procalcitonin; SOFA = sequential organ failure assessment.
This article is based on a presentation at the Lactate Satellite Meeting held during the 8th Indonesian-International Symposium on Shock and Critical Care, Bali, Indonesia, 24 August 2001.
References
- Calandra T, Baumgartner JD. Anti-endotoxin therapy. In: Edited by Sibbald WJ, Vincent JL, editor. Clinical Trials for the Treatment of Sepsis (Update in Intensive Care and Emergency Medicine 19) Berlin, Heidelberg: Springer-Verlag; 1995. pp. 237–250. [Google Scholar]
- Werdan K, Pilz G. Supplemental immunoglobulins in sepsis: a critical appraisal. Clin Exp Immunol. 1996;104(suppl):S83–S90. [PubMed] [Google Scholar]
- Lamari F, Anastassiou ED, Tsegenidis T, Dimitracopoulos G, Karamanos NK. An enzyme immunoassay to determine the levels of specific antibodies toward bacterial surface antigens in human immunoglobulin preparations and blood serum. J Pharm Biomed Anal. 1999;20:913–920. doi: 10.1016/s0731-7085(99)00087-4. [DOI] [PubMed] [Google Scholar]
- Trautmann M, Held TK, Susa M, Karajan MA, Wulf A, Cross AS, Marre R. Bacterial lipopolysaccharide-specific antibodies in commercial human immunoglobulin preparations: superior antibody content of an IgM-enriched product. Clin Exp Immunol. 1998;111:81–90. doi: 10.1046/j.1365-2249.1998.00445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Committee for Clinical Laboratory Standards Performance Standards for Antimicrobial Susceptibility Tests, 6th edition. Approved Standards NCCLS Document M2-A6. Villanova, PA: NCCLS; 1997.
- National Committee for Clinical Laboratory Standards Performance Standards for Antimicrobial Susceptibility Testing, 10th Informational Supplement. NCCLS Document M100-S10. Villanova, PA: NCCLS; 2000.
- Lissner R, Struff WG, Autenrieth IB, Woodcock BG, Karch H. Efficacy and potential clinical applications of Pentaglobin, an IgM-enriched immunoglobulin concentrate suitable for intravenous infusion. Eur J Surg. 1999;584(suppl):S17–S25. doi: 10.1080/11024159950188493. [DOI] [PubMed] [Google Scholar]
- Trautmann M, Karajan MA, Susa M. Intravenous immunoglobulins inhibit LPS-induced TNF alpha release from human monocytic cells. In: Faist E, editor. Congress Proceedings, 4th International Symposium on the Immune Consequences of Trauma, Shock and Sepsis. Bologna, Italy: Monduzzi Editore; 1997. pp. 775–779. [Google Scholar]
- Rieben R, Roos A, Muizert CT, Tinguely C, Gerritson AF, Daha MR. Immunoglobulin M-enriched human intravenous immunoglobulin prevents complement activation in vitro and in vivo in a rat model of acute inflammation. Blood. 1999;93:942–951. [PubMed] [Google Scholar]
- Pilz G, Kreuzer E, Kaab S, Appel R, Werdan K. Early sepsis treatment with immunoglobulins after cardiac surgery in score-identified post-cardiac patients at high risk for sepsis. Chest. 1994;105:76–82. doi: 10.1378/chest.105.1.76. [DOI] [PubMed] [Google Scholar]
- Pilz G, Appel R, Kreuzer E, Werdan K. Comparison of early IgM-enriched immunoglobulin versus polyvalent IgG administration in score-identified post-cardiac surgical patients at high risk for sepsis. Chest. 1997;111:419–426. doi: 10.1378/chest.111.2.419. [DOI] [PubMed] [Google Scholar]
- Kress HG, Scheidewig C, Schmitt H, Silber RE. Reduced incidence of postoperative infections following intravenous application of an IgA and IgM-enriched immunoglobulin preparation in anergic patients undergoing cardiac surgery. Crit Care Med. 1999;27:1281–1287. doi: 10.1097/00003246-199907000-00011. [DOI] [PubMed] [Google Scholar]
- Werdan K, Pilz G, the SBITS Study Group Polyvalent immune globulins. Shock. 1997;7(suppl):A5/1918. [Google Scholar]
- De Simone C, Delogu G, Corbetta G. Intravenous immunoglo-bulins in association with antibiotics: a therapeutic trial in septic intensive care unit patients. Crit Care Med. 1988;16:23–26. doi: 10.1097/00003246-198801000-00005. [DOI] [PubMed] [Google Scholar]
- Just HM, Metzger M, Vogel W, Pelka RB. Einfluss einer adjuvanten Immunoglobulin-Therapie auf Infektionen bei Patienten einer operativen Intensiv-Therapie-Station: Ergebnisse einer randomisierten kontrollierten Studie. Klin Wochenschr. 1986;64:245–256. doi: 10.1007/BF01711930. [DOI] [PubMed] [Google Scholar]
- Jesdinsky HJ, Tempel G, Castrup HJ, Seifert J. Cooperative group of additional immunoglobulin therapy in severe bacterial infections: results of a multicenter randomized controlled trial in cases of diffuse fibrinopurulent peritonitis. Klin Wochenschr. 1987;65:1132–1138. doi: 10.1007/BF01734833. [DOI] [PubMed] [Google Scholar]
- Vogel F. Bewertung der intravenösen IgM-Therapie bei schweren nosokomialen Infektionen (Ergebnis einer kontrollierten randomisierten Studie). In: Deicher H, Schoppe W, editor. In Klinisch angewandte Immunologie-Sepsis Therapie mit IgM-angereichertem Immunoglobulin. Berlin: Springer-Verlag; 1988. pp. 30–41. [Google Scholar]
- Dominioni L, Dionigi R, Zanello M, Chiaranda M, Dionigi R, Acquarolo A, Ballbio A, Sguotti Cl. Effects of high dose IgG on survival of surgical patients with sepsis scores of 20 or greater. Arch Surg. 1991;126:236–240. doi: 10.1001/archsurg.1991.01410260126018. [DOI] [PubMed] [Google Scholar]
- Schedel I, Dreikhausen U, Nentwig B, Hockenschnieder M, Rauthmann D, Balikcioglu S, Coldewey R, Deicher H. Treatment of gram-negative septic shock with an immunoglobulin preparation: A prospective, randomized clinical trial. Crit Care Med. 1991;19:1104–1113. doi: 10.1097/00003246-199109000-00003. [DOI] [PubMed] [Google Scholar]
- Alejandria MM, Lansang MA, Dans LF, Mantaring JBV. Intravenous immunoglobulin for treating sepsis and septic shock (Cochrane Review). In The Cochrane Library. Issue 2. Oxford: Update Software Ltd; 2002, 4. [DOI] [PubMed]
- Volk HD, Reinke P, Döcke WD. Immunologic monitoring of the inflammatory process: Which variables? When to assess? Eur J Surg. 1999;584(suppl):S70–S72. doi: 10.1080/11024159950188600. [DOI] [PubMed] [Google Scholar]
- Reith HB, Mittelkötter U, Debus ES, Kussner C, Thiede A. Procalcitonin in early detection of postoperative complications. Dig Surg. 1998;15:260–265. doi: 10.1159/000018625. [DOI] [PubMed] [Google Scholar]


