Abstract
Background
The complex interaction of food habits, stress levels, and gut microbiota is instrumental in shaping global human well-being. Lifestyle indicators like diet, stress, and exercise have immense potential to drive gut health but are usually plagued by the divide between knowledge and action.
Methodlogy
This research compared lifestyle variables and awareness of gut health in 51 participants on a standardized questionnaire. It analyzed variables such as frequency of meals, intake of processed foods, intake of dietary fiber and probiotics, history of digestive diseases, perceived influence of stress, and knowledge of the gut–brain axis.
Results
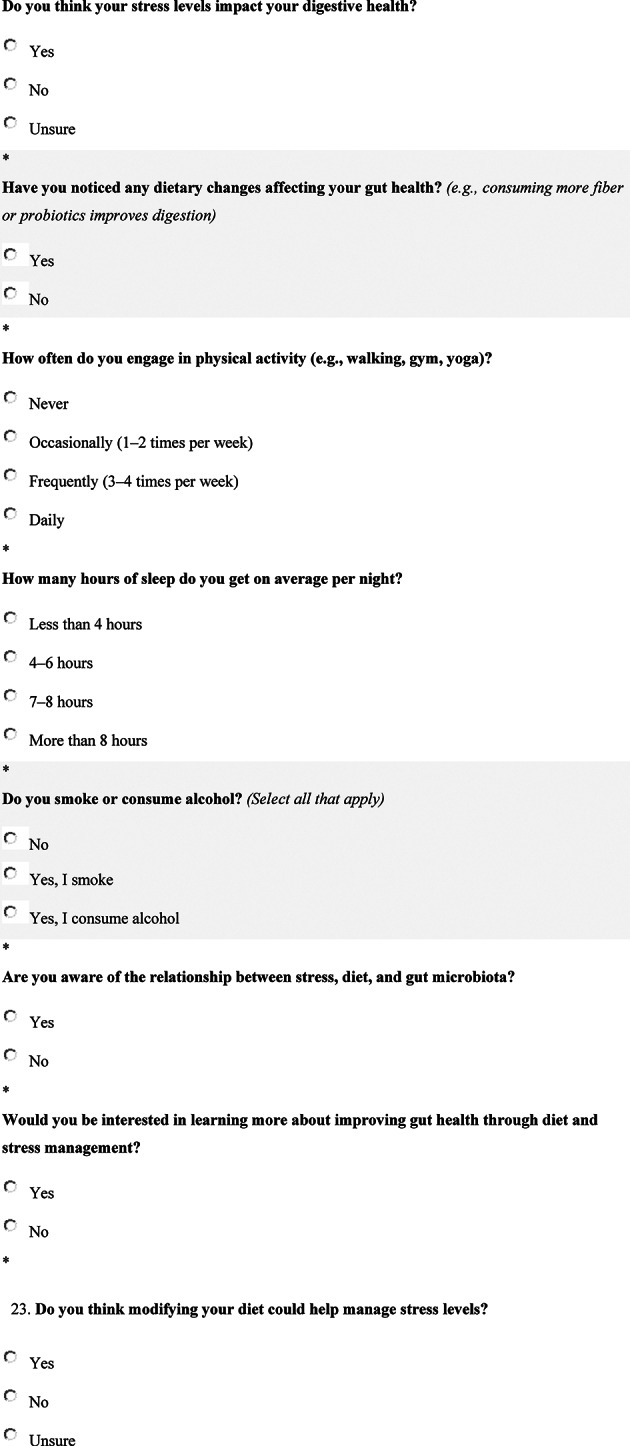
Results indicated that 69.05% of the participants ate only 1-2 meals a day, and 71.43% had moderate consumption (1-2 times per week) of fast or processed foods. A concerning fact is that only 7.14% ate probiotic foods daily, and only 28.57% had high-fiber foods in their daily diet. Gastrointestinal problems were prevalent, with 56.41% having issues and 51.28% having occasional problems (1-2 times per week). In addition, 66.67% thought that stress influences their digestion, and 74.36% experienced changes in diet influencing their gut. Just 13.16% were physically active daily, and 44.74% slept for less than six hours daily, both are known to influence the gut microbiome. While 76.32% understood the diet–stress–microbiota connection, just 57.89% were of the view that dietary modifications can help manage stress.
Conclusion
The research points to an important gap between knowledge and practical behaviors concerning gut health and stress management. There is a need for public health programs to enhance sustainable lifestyle and dietary changes to improve microbial diversity, digestive well-being, and mental health.
Graphical abstract
Keywords: Stress, Diet, Gut microbiota, Cross-Sectional study, Questionnaire-Based study, Perceived stress scale (PSS), Dietary patterns, Gastrointestinal symptoms, Gut–Brain axis, Microbiota imbalance
Introduction
The gut microbiota, a complex community of trillions of microbes living within the human gastrointestinal tract, is crucial for overall health. It is well known to be involved in the metabolism of nutrients, immune modulation, and the preservation of gut integrity [1]. Over the last decade, evidence has increasingly tied the composition of the gut microbiota with psychological state, specifically with stress, in evidence of a bidirectional communications network linking brain and gut, often known as the gut–brain axis [2]. This interactive relationship contains neural, hormonal, and immunologic pathways that, through incessant exchange, ensure a steady passage of messages from the central nervous system to the gut [3]. Chronic stress has been reported to affect both food behavior and gut microbiota [4]. Stress can give rise to emotional eating or dietary avoidance, leading to enhanced intake of high-fat, high-sugar, and low-fiber foods [5]. Such nutritional habits are reported to disrupt the diversity and functionality of gut microbiota, which could amplify gastrointestinal disturbances and emotional distress. This triadic interaction among stress, diet, and gut microbiota is paramount to comprehend the physiological and psychological pathways underlying several health disorders [6].
Physiological and behavioral reactions might account for the relationship between gut microbiota and life stress. By triggering the stress response system, which raises the production of cortisol and inflammatory cytokines, stress can instantly impact on physiology. Chronic, ongoing stress has been linked to gastrointestinal and cardio-metabolic illnesses and disrupts the normal HPA-axis response and immunological function. Few studies have looked at the potential mediating role of chronic cortisol levels, an objective indicator of stress, in the relationships between gut microbiota and subjective stress. Second, it is known that one of the main modifiable factors influencing the variety, quantity, and function of microbiota is food. Regular eating habits are linked to anti/pro-inflammatory properties, mucosal protection, and microbial clusters. Numerous gut microbiota taxa have also been linked to the consumption of micro- and macronutrients, with dietary fiber frequently playing a significant role in preserving bacterial diversity. As a result, some have noted that diet quality plays a mediating and moderating role in the processes that lead to stress-related diseases. Several studies have described the contribution of the gut microbiota to the modulation of mood and behavior via the synthesis of neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA) [7].
Stress has been linked, in return, to changes in gut motility, heightened intestinal permeability (“leaky gut”), and immune activation, all of which have the potential to modify the microbial community [8]. In addition, nutrients in the diet, like dietary fiber, prebiotics, and fermented foods, all have critical roles in sustaining microbial diversity and gastrointestinal health. Diets high in refined sugars, saturated fats, and ultra-processed foods are linked with microbial dysbiosis, a condition of imbalance in gut microbiota correlated with many diseases such as irritable bowel syndrome (IBS), obesity, and mood disorders [9].
Despite previous knowledge, few studies have investigated this interrelationship based on questionnaire data in a cross-sectional design, especially in diverse populations. This study aims to fill the gap in research by investigating perceived stress, dietary habits, and gastrointestinal symptoms reflecting gut dysbiosis.
Significance of the study
Although the gut-brain axis has become an integral pathway through which diet, stress, and mental health are interconnected, much of what has been written in the literature is experimental or in clinical populations and therefore not generalizable to everyday, real-world environments. This cross-sectional study completes an essential gap by evaluating these relationships in a naturalistic, real-world environment, using data from a demographically representative sample of adults to examine real-life food eating habits, self-reported stress levels, and gastrointestinal well-being. In evaluating this triad of factors in concert, the study gives a more ecologically valid account of how diet and stress interact to affect gut health in representative populations. Importantly, this research closes the knowledge gap between what has been identified in terms of gut health and what is truly occurring. Even while the scientific world continues to establish the role that the gut microbiota plays in mental and physical health, a large majority of the population are unaware that their eating and stress management habits are undermining their well-being. The findings of this study can be applied to inform effective public health communications, stress management interventions, and nutrition education to promote gut-friendly lifestyle interventions.
Research problem
While scientific evidence more and more corroborates the bidirectional interaction among stress, diet, and gut microbiota through the gut-brain axis, much of what we know remains confined to controlled experimental or clinical environments. Consequently, we have little insight into how these interactions play out in daily life in community-dwelling adults, a population whose lifestyle behaviors are extremely heterogeneous, less tracked, and underrepresented in existing research. In particular, there is sparse empirical evidence regarding the co-occurrence and interactive effects of diet habits (e.g., nutrition quality, eating styles, and hydration) and subjective stress levels on co-occurring digestive symptoms like bloating, abnormal bowel movements, and overall gastrointestinal discomfort among general populations. The lack of ecologically valid, integrative data poses a challenge to the advancement of comprehensive, behaviorally grounded interventions for enhancing gut-brain health through lifestyle changes.
Objectives
To determine the eating habits of participants, such as frequency of meals, consumption of processed foods, probiotics, and fiber.
To find the perceived association between stress, diet, and gut health.
Hypothesis
Null hypothesis (H₀)
There is no strong association between dietary habits, stress levels, and gut microbiota-related health outcomes in the study population.
Alternate hypothesis (H₁)
There is a strong association between dietary habits, stress levels, and gut microbiota-related health outcomes in the study population.
Methodology
Study design
The research employed a cross-sectional, exploratory, and hypothesis-generating design to identify associations between gastrointestinal symptoms, dietary habits, and perceived stress. It was employed in an attempt to catch a glimpse of the concurrent factors in one neighborhood with minimal regional data regarding the gut-brain axis. It is suitable for investigating plausible associations that could guide further interventional or longitudinal study. The perceived stress was ascertained through a validated self-report measure, GI symptoms were assessed through a symptom checklist for functional digestive disorders, and dietary patterns were assessed through a food frequency questionnaire (FFQ) content-checked by three nutritionists and two psychologists. Data were examined descriptively and with bivariate correlations to investigate variable associations. The results provide a basis for exploring further research into the effects of stress and diet on gut health and mental health.
Study sample size and population
Adults aged 18 years and older formed the study population. Convenience sampling was utilized to choose 51 subjects with different educational and professional levels. The participants were chosen based on their availability during the study period, with voluntary enrollment. Male and female volunteers were enrolled without any socioeconomic or health status restrictions. Excluding serious ulcer patients with GI surgery performed within a month.
Sample Size Formula for Cross-Sectional Study (Proportion-Based Estimation):
 |
where:
n = required sample size.
Z = Z-score for 95% confidence level (1.96).
p = estimated prevalence (proportion of interest).
d = desired margin of error (precision).
Expected prevalence, p = 0.50p = 0.50p = 0.50 (used when no prior estimate is available to give the maximum required sample size).
Confidence level = 95% → Z = 1.96Z = 1.96Z = 1.96.
Desired margin of error, d = 0.14d = 0.14d = 0.14.
Then:
 |
Data collection tool
Three questionnaires that were validated questionnaires were used. Perceived Stress Scale (PSS-5): To measure the degree of stress experienced in the last month, with emphasis on uncertainty, lack of control, and overload. Food Frequency Questionnaire (FFQ) To collect dietary intake habits in the last month, with emphasis on frequency of intake of fiber-containing foods, processed foods, fermented foods, and sugar [10]. Gut Health Questionnaire: A specially formulated self-reporting questionnaire to evaluate gastrointestinal symptoms, such as bloating, constipation, diarrhea, abdominal pain, and regularity of bowel. The questionnaires were filled out either on paper or via the internet. Demographic information such as age, gender, education, and lifestyle behaviors (e.g., smoking, exercise) was also gathered [11]. All participants were administered the same mode of administration to provide consistency within the study. This was standardized via structured, self-completed questionnaires administered under the direction of trained staff. The tools applied in the study were tested by a panel of five experts—three nutritionists and two psychologists—with related academic and clinical expertise. The content validation process entailed pretesting the questionnaire for relevance, clarity, and comprehensiveness. Feedback was collected using a validated checklist and suitably revised to enhance the validity of the instrument and its alignment with the study objectives.
Ethical considerations
The research was done according to the ethical standards of human research. Ethical approval was granted by the Institutional Review Board of Nur International University (IRB Reg. NIU-112-23). Consent of participants were written. Participants were made aware of the subject matter of the study, their right to withdraw at any time, that confidentiality would be maintained about their information, and they would be used for academic purposes only.
Statistical analysis
Statistics were carried out on SPSS. Descriptive statistics were calculated for questionnaires and demographics. Pearson correlation coefficients were applied to examine the associations between gut health markers, dietary patterns, and stress scores [12].
Results
Demographic characteristics
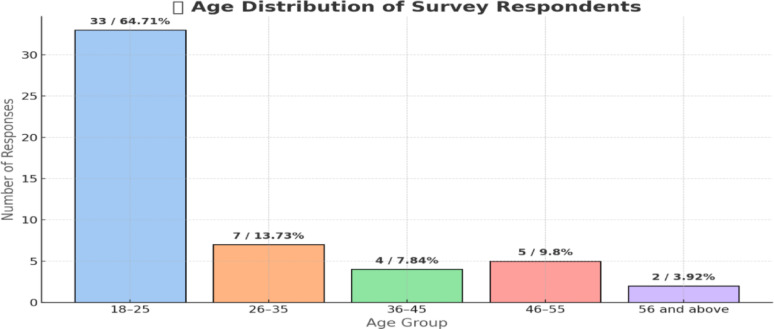
The sample size was 51, with a preponderance of males (72.55%). A higher percentage were graduates with at least a bachelor’s degree, among whom 43.14% had a master’s or more. High school and bachelor’s graduates made up 27.45% each. Students comprised the largest occupation category (56.86%), followed by full-time workers (29.41%). Few were unemployed (7.84%), retired (3.92%), or part-time workers (1.96%). (Fig. 1) (Tables 1 and 2).
Fig. 1.
Age of the Participants.The majority of the survey responders (64.71%) fall within 18–25 years. Lower proportions comprise those in 26–35 years (13.73%), 46–55 years (9.8%), 36–45 years (7.84%), and 56 years and older (3.92%). This is a high presence of youths in the survey
Table 1.
Frionnullequency of age with mean, median, and standard deviation
| Age Range | Midpoint (x) | Frequency (f) | f × x | f × x² |
|---|---|---|---|---|
| 18–25 | 21.5 | 33 | 709.5 | 15,256.25 |
| 26–35 | 30.5 | 7 | 213.5 | 6,511.75 |
| 36–45 | 40.5 | 4 | 162 | 6,561 |
| 46–55 | 50.5 | 5 | 252.5 | 12,750.25 |
| 56 and above | 60 | 2 | 120 | 7,200 |
| Total | — | 51 | 1,457.5 | 48,279.25 |
| Mean (µ) | — | — | 28.6 | — |
| Median | — | — | 21.5 | — |
| Standard Deviation (σ) | — | — | — | ≈ 12.44 |
Table 2.
Characteristics of participating individuals
| Category | Subcategory | No. of Participants | % of Responses | Mean ± SD |
|---|---|---|---|---|
| Gender | Male | 37 | 72.55% | 0.725 ± 0.063 |
| Female | 14 | 27.45% | 0.275 ± 0.063 | |
| Education Level | No formal education | 1 | 1.96% | 0.020 ± 0.020 |
| High school | 14 | 27.45% | 0.275 ± 0.063 | |
| Bachelor’s degree | 14 | 27.45% | 0.275 ± 0.063 | |
| Master’s degree or higher | 22 | 43.14% | 0.431 ± 0.069 | |
| Occupation | Student | 29 | 56.86% | 0.569 ± 0.069 |
| Employed (Full-time) | 15 | 29.41% | 0.294 ± 0.063 | |
| Employed (Part-time) | 1 | 1.96% | 0.020 ± 0.020 | |
| Unemployed | 4 | 7.84% | 0.078 ± 0.038 | |
| Retired | 2 | 3.92% | 0.039 ± 0.027 |
Perceived stress management ability
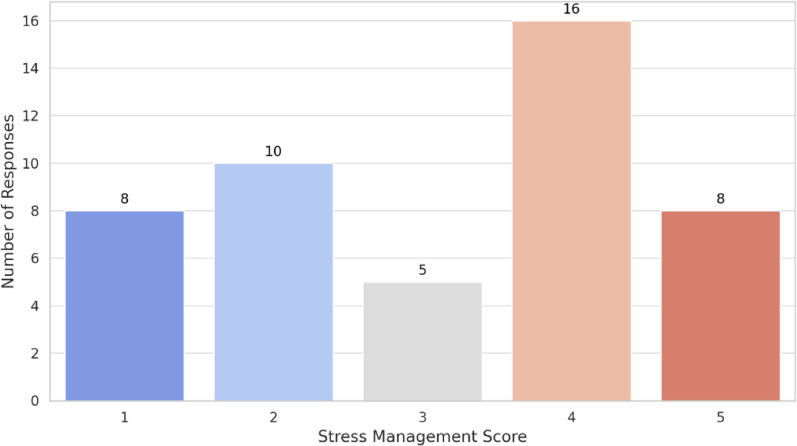
The information indicates that stress is prevalent among the participants, with 43.48% reporting it often or always. The highest sources of stress reported were work/studies (36.17%), family obligations (34.04%), and money (31.91%). Health issues and others were less reported. Exercise (42.55%) and TV/music watching (34.04%) were the most commonly used coping mechanisms for stress, followed by socializing (19.15%). 12.77% perform meditation. A significant 25.53% employed other coping strategies, indicating diverse stress management styles (Table 2). The results are similar to the studies as a whole identifies the intricate link between eating behavior and stress (Table 3) (Fig. 2).
Table 3.
Stress indication parameters in participants
| Category | Response | No. of Participants | % of Responses | Mean ± SD |
|---|---|---|---|---|
| Incidence of Experienced Stress | Rarely | 10 | 21.74% | 0.217 ± 0.061 |
| Sometimes | 17 | 36.96% | 0.370 ± 0.071 | |
| Often | 9 | 19.57% | 0.196 ± 0.058 | |
| Always | 11 | 23.91% | 0.239 ± 0.064 | |
| Common Sources of Stress | Work/Studies | 17 | 36.17% | 0.370 ± 0.071 |
| Financial issues | 15 | 31.91% | 0.326 ± 0.069 | |
| Family responsibilities | 16 | 34.04% | 0.348 ± 0.070 | |
| Health problems | 7 | 14.89% | 0.152 ± 0.051 | |
| Other | 6 | 12.77% | 0.130 ± 0.047 | |
| Ways to Cope with Stress | Exercise | 20 | 42.55% | 0.435 ± 0.073 |
| Meditation/Yoga | 6 | 12.77% | 0.130 ± 0.047 | |
| Socializing | 9 | 19.15 |
Fig. 2.
Stress Management Score 1 = Poorly, 5 = Very Well.The bar chart illustrates scores for stress management ranging from 1 to 5, with the greatest number of responses (16) at score 4, which demonstrates typically good stress management. Scores 1 and 5 both received 8 responses, score 2 received 10, and score 3 had the lowest (5), which infers that most respondents score their stress management as higher than average
Dietary patterns
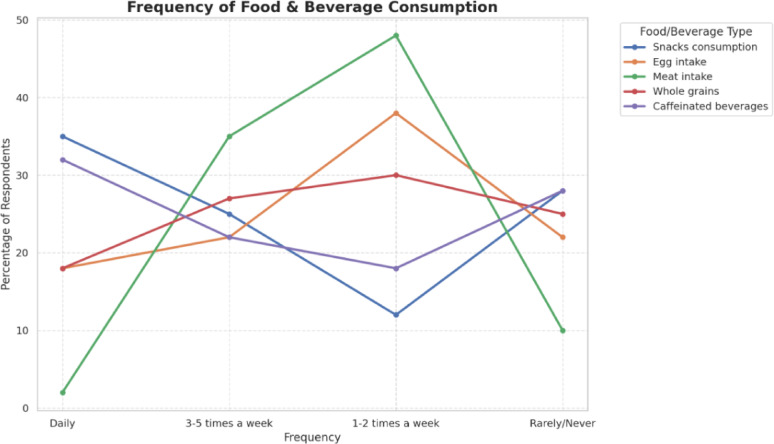
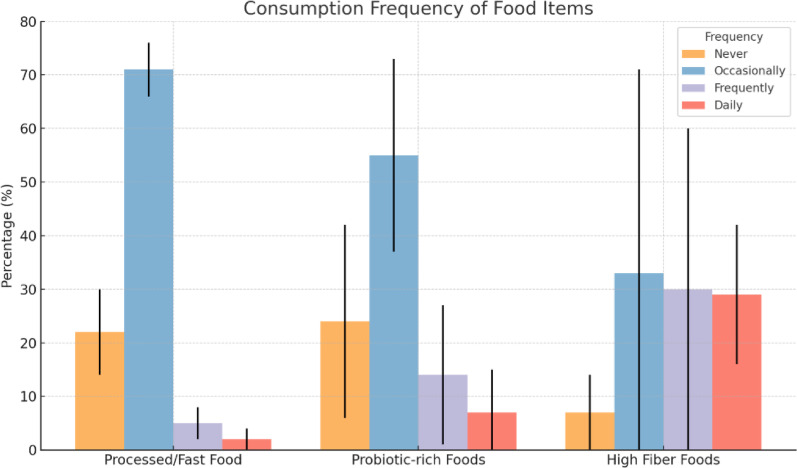
Analysis of the FFQ revealed that participants with high stress levels had significantly higher intake of sugary snacks, fast foods, and caffeinated beverages. In contrast, those with low stress reported more frequent consumption of fiber-rich vegetables, fruits, whole grains, and fermented foods like yogurt and kefir. The majority of participants (69.05%) claimed to eat only 1–2 meals daily, whereas only 9.52% had four or more. Processed or fast foods were usually eaten (71.43%), but few ate it daily (2.38%). Probiotic foods were eaten occasionally by 54.76%, whereas 23.81% never ate them as shown in Fig. 3. More than half of the respondents (59.52%) ate high-fiber foods frequently or every day. Also, 52.38% indicated having used dietary supplements, reflecting relatively moderate concern towards gut health and nutrition among study participants despite narrow daily meal frequencies (Table 3). The findings show diverse eating patterns. The majority of participants eat meat (47.67%) and fast food (41.86%) 1–2 times a week. Egg is eaten regularly by 36.05% 1–2 times a week, and 26.74% eat it 3–5 times. Caffeinated drinks are drunk every day by 36.05%. Whole grains are eaten 1–2 times a week by 30.23%, and in-between-meal snacks are avoided mostly, with 37.21% not eating them rarely or never. In general, moderate frequency patterns predominate in all food groups (Fig. 3). The studies are similar to our findings depict a consistent pattern of association between diet quality and mental health, particularly depression, anxiety, and stress (Table 4) (Fig. 3).
Fig. 3.
Food and Beverage Consumption Frequency.percentage of consumers of different food and drink products in four frequency bands: daily, 3–5 times weekly, 1–2 times weekly, rarely/never. The consumption of snacks peaks on a daily basis at 35%, tapering down to 12% at 1–2 times weekly before mounting to 23% in the rarely/never bracket. Caffeinated drinks are used every day by 32%, fall to 18% for 1–2 times a week, and then increase again to 28% in rarely/never users. Egg consumption rises from 18% daily to the highest frequency of 38% for 1–2 times a week and falls to 22% in rarely/never. Meat consumption indicates very little daily use (3%), spikes very high at 48% for 1–2 times a week, and decreases to 10% in the rarely/never category. Whole grain consumption indicates a constant pattern, going up from 18% daily to 30% for 1–2 times a week and decreasing slightly to 25% in the rarely/never group. These patterns indicate that snacking and caffeine are frequent daily practices, meat and egg consumption is more weekly, and whole grain consumption is relatively stable across frequencies
Table 4.
Dietary patterns of the individual
| Meal Consumption/Food Type | Category | No. of Participants | % of Responses |
|---|---|---|---|
| Meals consumed per day | |||
| 1–2 | 29 | 69.05% | |
| 3 | 9 | 21.43% | |
| 4 or more | 4 | 9.52% | |
| Consume processed or fast food | |||
| Never | 9 | 21.43% | |
| Occasionally (1–2 times/week) | 30 | 71.43% | |
| Frequently (3–4 times/week) | 2 | 4.76% | |
| Daily | 1 | 2.38% | |
| Consume probiotic-rich foods (e.g., yogurt, kefir) | |||
| Never | 10 | 23.81% | |
| Occasionally (1–2 times/week) | 23 | 54.76% | |
| Frequently (3–4 times/week) | 6 | 14.29% | |
| Daily | 3 | 7.14% | |
| Consume high-fiber foods (whole grains, fruits, veg) | |||
| Never | 3 | 7.14% | |
| Occasionally (1–2 times/week) | 14 | 33.33% | |
| Frequently (3–4 times/week) | 13 | 30.95% | |
| Daily | 12 | 28.57% | |
| Dietary supplements (probiotics, prebiotics, vitamins) | |||
| Yes | 22 | 52.38% | |
| No | 20 | 47.62% |
Gut health indicators
More than half of the participants (56.41%) indicated having digestive problems, which occurred frequently in most cases (51.28%). A large majority (66.67%) felt that stress affects the digestive system, and 74.36% observed that food changes influence their gut. The majority participated in some physical activity, although only 13.16% did so every day. Smoking and alcohol consumption were minimal (21.05%). Knowledge of the stress-diet-gut microbiota connection was high (76.32%), and an equal percentage expressed interest in knowing more. Moreover, 57.89% thought that dietary modification could be useful in controlling stress (Table 4). The studies reviewed here collectively examined the intricate interactions among mental health, psychosocial stress, and gut microbiota in human and animal models. These observations suggest that stress can exert a subtle influence on microbial patterns (Fig. 4) (Fig. 5) (Table 5).
Fig. 4.
Consumption frequency of food items. The vertical black lines at the top of each bar represent error bars. These reflect statistical variability or uncertainty in the percentage values
Fig. 5.
Sleeping Duration of the participants. Less than 4 h (Green): Representing 7 participants (18.42%), 4–6 h (Orange): The largest group, comprising 17 participants (44.74%), 7–8 h (Blue): This group includes 12 participants (31.58%), More than 8 h (Pink): A minority of 2 participants (5.26%)
Table 5.
Participant survey summary: gut health, diet, and stress
| Survey Item | Response | No. of Participants | % of Responses | SD (if applicable) |
|---|---|---|---|---|
| Digestive Issues Experienced | Yes | 22 | 56.41% | — |
| No | 17 | 43.59% | — | |
| If Yes, Frequency of Digestive Symptoms (n = 39) | Rarely (1 pt) | 14 | 35.90% | |
| Occasionally (1–2x/week) (2 pt) | 20 | 51.28% | ||
| Frequently (3–4x/week) (3 pt) | 2 | 5.13% | ||
| Daily (4 pt) | 3 | 7.69% | SD = 0.80 | |
| Stress Levels Impact Digestion | Yes | 26 | 66.67% | — |
| No | 8 | 20.51% | — | |
| Unsure | 5 | 12.82% | — | |
| Noticed Dietary Changes Affect Gut Health | Yes | 29 | 74.36% | — |
| No | 10 | 25.64% | — | |
| Physical Activity Frequency (1–4 scale) | Never (1 pt) | 9 | 23.68% | |
| Occasionally (1–2x/week) (2 pt) | 21 | 55.26% | ||
| Frequently (3–4x/week) (3 pt) | 3 | 7.89% | ||
| Daily (4 pt) | 5 | 13.16% | SD = 0.86 | |
| Smoke or Consume Alcohol | No | 30 | 78.95% | — |
| Yes, I smoke | 7 | 18.42% | — | |
| Yes, I consume alcohol | 1 | 2.63% | — | |
| Aware of Diet-Stress-Microbiota Link | Yes | 29 | 76.32% | — |
| No | 9 | 23.68% | — | |
| Interested in Gut Health Education | Yes | 29 | 76.32% | — |
| No | 9 | 23.68% | — | |
| Believes Diet Can Help Manage Stress | Yes | 22 | 57.89% | — |
| No | 9 | 23.68% | — | |
| Unsure | 7 | 18.42% | — |
Discussion
Discussion of participant characteristics
Most of the respondents are aged between 18 and 25, accounting for approximately 64.71% of the sample. This indicates a youth population, possibly because the research is relevant to younger individuals, the sampling method (e.g., online surveys or student sampling), or the focus on university or early-professional populations. The 26–35 years category constitutes a lower percentage at 13.73%, followed by 36–45 (7.84%) and 46–55 (9.80%). An age of 56 and above is only 3.92% of the respondents, indicating limited participation from adults of an older age group. This focus among the younger age groups indicates that the results are likely to significantly represent the views, experiences, or knowledge levels of young adults. If the research is focused on technology use, educational intervention, youth mental health, or social media habits, then age representation is satisfactory to the goals. Of 51 participants, 72.55% were men and 27.45% were women, indicating a significant Gender disparity. The data show that the majority of respondents have attained postsecondary education, where 43.14% hold a Master’s degree or higher and 27.45% have a Bachelor’s degree. This would indicate that 70.59% of the respondents have a Bachelor’s level of education or higher, indicating an extremely educated sample base. The rest of 27.45% comprises those with a high school education only, and a very small percentage (1.96%) had no formal education. More than half of the participants (56.86%) are students, which is in line with the earlier observation of a largely young sample. This largest group, which would most likely be university or college students, can account for the high percentage of respondents holding Bachelor’s and Master’s degrees. 29.41% are working full-time, representing working professionals, whereas merely 1.96% are part-time workers. The low percentage of part-time workers might be indicative of either a cultural bias where part-time work is not prevalent or merely the population being surveyed. 7.84% are unemployed, whereas 3.92% are retired, showing a small but significant subset that can be used to gain insight into economic vulnerability or the experience of post-employment life. The occupational bias towards students means that the survey results will likely reflect the attitudes, behaviors, and priorities of student populations predominantly. The presence of unemployed and retired respondents, while limited, is nevertheless worthwhile. Such respondents are likely to experience special challenges, e.g., economic distress, health risks, or social isolation. Their data can be critical in social welfare research, pension policy evaluation, or health behavior research. The prevalence of students in the 18–25 category implies a natural trend, since this is usually the period of formal schooling. Full-time employed individuals would be more likely to be in the 26–45 category, although the data is not cross-tabulated. Retirees naturally fall in the 56 and above category. Although males make up a greater percentage of the sample, it would be useful to examine whether educational level differs substantially by gender. This could reveal gender differences in access to education or areas of study, which are pertinent to gender mainstreaming in education policy. Higher education equals being a student or working full-time. The education profile implies a talent or semi-skilled group. It is of considerable consequence in studies of the labor market, assessments of digital literacy, or capacity development programs. Younger, better-educated, and male-dominated participants tend to be easier to reach and more likely to respond. While this can generate rich data on some issues, it also calls for caution in generalizing to wider populations. Drawing from the cases and records gathered from interview statements, information based on thorough insight about the target group, which hitherto have gone unreported, is obtained through this work of study.
General Positive Influences of Part-Time Work: Taking both the positive and negative into consideration, the authors conclude that the advantages to low-income older persons of part-time work in general outweigh the disadvantages. Those advantages are increased financial well-being, a feeling of renewed purpose, and improved socialization. Demographic and Work Patterns: The research includes a profile of respondents’ background, such as a summary of their prior work history, motives for requiring part-time employment, and the character of jobs that they obtained. These facts reveal the structural and functional features of part-time employment for the sample. The study investigates levels of job satisfaction among respondents and explores their attitudes towards workplace discrimination. Evidence indicates that although some cases of age discrimination were mentioned, they were not widespread. Nevertheless, the likelihood that some might downplay such incidents because of fear of losing employment is recognized. The contribution of employment placement services in the provision of employment for elderly persons is examined, both where they assist and where there is room for improvement to meet the needs of this group. According to what they have discovered, the authors make recommendations that aim to improve labor conditions and employment opportunities for low-income older adults. They offer these recommendations to guide policymakers, practitioners, and researchers who have an interest in aging and labor issues. This comprehensive study greatly enlightens us of the complexities involved in part-time work among poor older persons, with a call to ensure that they have facilitative policies and practices to enhance their work experiences [13].
Pintelon et al. [14] examines how traditional social class structures continue to influence individuals’ exposure to social risks, despite shifts towards social investment-oriented welfare policies. Persistent Influence of Social Class: The research establishes that origin social class plays an important role in determining the risk of suffering from social risks like unemployment, poor health, jobless household, lone parenthood, and low-paid work. This recognizes that the conventional class-based inequalities continue to dominate the social landscapes of modern societies [14]. Even though social investment policies are designed to ensure equality of opportunity and social mobility, the authors state that these strategies will be unable to properly address the deep-rooted nature of class-based disadvantages. By failing to acknowledge and respond to these persistent inequalities, such policies run the risk of compounding or even intensifying social exclusion. The piece warns that social investment plans, if poorly designed, could lead to ‘Matthew effects,’ whereby resources disproportionately flow to already privileged groups, thereby aggravating existing social inequalities. The writers prefer social policies with definite acknowledgement of the function that social class performs in determining human life chances. They believe that in the absence of such attention, social risk-counteractive policy may not reach the area of true equity. the study indicates the long-term influence of social class on individuals’ susceptibility to social risks and advocates for more subtle, class-sensitive approaches in designing social investment policies [14].
Stress frequency
The information regarding stress frequency offers an important baseline to determine how often people experience being overwhelmed or stressed in their lives. The highest percentage of respondents (36.96%) said that they occasionally feel stressed. These points to a high but significant degree of stress occurrence in the surveyed General population. Those who always feel stressed make up 23.91%, almost a quarter of the population, a significant percentage that reflects chronic stress problems in this subgroup. On the other hand, a lower percentage, 21.74%, indicated that they seldom felt stress, indicating either an extremely efficient coping mechanism or a life that avoids stressors. The category that indicated frequently feeling stress (19.57%) also adds to a larger picture of regular exposure to stress for almost 43.48% of the participants when added to the “always” category. This result emphasizes the critical importance of stress management facilities and health promotion campaigns, most importantly for preventing chronic stress and its sequelae.
subjects listed several sources of stress, and these responses are as follows: Work and academic tension was the single most prevalent reason, influencing 36.17% of individuals. The second most frequent reason was family duty, at a rate of 34.04%. Financial concerns were third, and they closely followed family-related stressors, influencing 31.91% of the participants. In a post-pandemic world economy characterized by inflation, unemployment, uncertainty, and increasing living expenses, financial insecurity is a lasting and overwhelming cause of psychological distress. Though health problems (14.89%) and other sources (12.77%) had lower frequencies, these are not to be underestimated. Chronic disease, pain, or disability may lead to long-term stress, and “other” categories could encompass challenges such as social isolation, study pressure, or environmental factors. Though the existence of stress is unavoidable, people’s coping styles can reduce its effects. The coping mechanisms are summarized as follows: The most common coping style is exercise, and 42.55% of the participants reported using it. Exercise has long been shown to be a highly effective mechanism in fighting stress through the release of endorphins, bettering mood, and enhancing General well-being. Entertainment coping, like TV watching or music listening, follows at 34.04%. Passive relaxation in this manner serves to distract from stressors and provide temporary relief and emotional regulation. Social support, mentioned by 19.15%, demonstrates the significance of social support in managing stress. Talking with friends, family members, or support groups offers emotional reassurance and perspective during stressful times. Interestingly, yoga and meditation are practiced by only 12.77% of the participants.
Emotional eating, typically linked with unhealthy coping, was chosen by merely 1 participant (2.13%). Though the figure is small, it still highlights the existence of maladaptive stress reactions that could have long-term implications on health. The “Other” category was referenced by 25.53%, suggesting that people adopt a broad variety of less typical or individualized stress management strategies. These may be hobbies, creative activities, journaling, prayer, therapy, or solitude. It is a measure of the individuality of each subject’s emotional reaction and their requirement for tailored mental health interventions. Self-perception is very critical in how stress is managed. Respondents were asked to rate their stress management ability on a scale of 1 to 5, where 1 signifies very poor and 5 signifies excellent. The many responses (34.04%) fell at level 4, implying that many people are quite confident that they can handle stress. But only 17.02% were at level 5, which is optimal stress management. This could imply an awareness of where there is still room for improvement. At the opposite extreme, 17.02% of the participants placed themselves at level 1, and 21.28% chose level 2, for a total of 38.3% who perceive themselves as having weak or below-average stress management ability. This is a troubling discovery, as it suggests that over one-third of the participants believe they have serious difficulty with stress regulation. The middle point (level 3) was chosen by only 10.64%, indicating that fewer respondents rated their stress management as average. The three most prevalent stressors—work/studies (36.17%), family duties (34.04%), and financial issues (31.91%)—reflect a society in distress due to performance pressure, household burdens, and economic insecurity. These stressors are mutually reinforcing. Despite the employment of healthy coping mechanisms by most, the percentage of people scoring their stress management skills low (38.3% at level 1 and 2) indicates a gap between perception and behavior. This can be due to internalized pressure, low self-esteem, or absence of external validation. Building psychological resilience and promoting self-awareness may help fill this gap.
Relationship among diet, stress, and gut health
A majority of the participants (69.05%) ate 1–2 meals per day, 21.43% ate three meals, and 9.52% ate four or more meals per day. After examining the consumption of fast or processed food, 71.43% of them had it occasionally (1–2 times a week), while only 2.38% consumed such foods daily. A smaller proportion (4.76%) utilized processed food often (3–4 times a week), and 21.43% never utilized them. Processed foods, which are Generally rich in fats, sugars, and additives, are claimed to damage gut microbiota by promoting the development of pathogenic bacteria at the expense of useful species. Although 54.76% had these foods from time to time, only 14.29% used them regularly and 7.14% on a daily basis. Interestingly, 23.81% of the respondents said they never ate probiotic-rich foods. This indicates a deficiency in dietary intake of gut-friendly bacteria that promote health of the gut, immune system, and the mind. Whole grain, legumes, fruits and vegetables which are rich in fiber were consumed daily by 28.57% of the respondents; frequently, by 30.95%; and occasionally by 33.33%. Only 7.14% did not consume such foods at all. Fiber from food acts as a prebiotic, which feeds beneficial gut bacteria and aids in regular movement of bowels. Proper fiber consumption also helps to control blood sugar levels, lower cholesterol, and assist with weight control. The fairly balanced consumption of high-fiber foods in this sample indicates a moderately favorable dietary pattern, though higher daily consumption would further contribute to digestive and overall well-being. Half of the participants (52.38%) took dietary supplements such as probiotics, prebiotics, or vitamins. Supplementation may supplement nutrition gaps or augment specific health goals.
The study by Roman et al. [15], investigated eating habits in 1,398 adults in Romania to establish the prevalent eating habits and its association with obesity. Increased consumption of red meat and processed meat, fried food, and starchy side dishes. Characterized by high consumption of fast food, processed meats, and added sugars. Pilot in lacking fruits, vegetables, fish, legumes, and soy food. The High Meat/High Fat Pattern was associated with a 20% increased risk of obesity (Odds Ratio [OR] 1.2; 95% Confidence Interval [CI]: 1.1–1.4). The Prudent Pattern was associated with a 20% decreased risk of obesity (OR 0.8; 95% CI: 0.7–0.9). The Western Pattern was not significantly associated with obesity, perhaps because it is prevalent among active, younger people. The High Meat/High Fat Pattern was more prevalent in men, those with lower education, rural dwellers, and smokers. The Western Pattern was more prevalent in younger people, those with higher physical activity, and smokers. The Prudent Pattern was linked to older age, female sex, higher education, non-smoking, and higher physical activity. The research emphasizes targeted nutritional education and intervention, particularly in populations consuming the High Meat/High Fat and Western diets, to counteract obesity risks. The research presents valuable findings concerning the eating habits of Romanians and emphasizes the importance of taking into account cultural and demographic factors in public health interventions designed to prevent obesity [15].
The majority of the interviewees (56.41%) confessed to ever having suffered from either bloating, constipation, or diarrhea issue at some point in time. 51% twenty-eight (51.28%) of them suffered from it on an intermittent basis (1–2 times a week) while fewer still had frequent (5.13%) or daily (7.69%) experiences. Infrequent experiences were experienced in 35.90% of the responses. Sixty-six and two-thirds percent (66.67%) of the subjects who were interviewed confessed that they had been subjected to stress which impacted their gastrointestinal health. Only 20.51% did not hold the view that there was a link between stress and digestion, and 12.82% were not sure, which points towards a lack of information and knowledge regarding this topic. The majority of the sample population (74.36%) had observed differences in their diet affecting their gut health. It reflects that individuals are receptive to the notion that particular food choices impact their digestion, a step towards healthy eating and better results. Additionally, 76.32% also revealed awareness of diet-stress-gut microbiota inter-linkage. It is a welcome sign, as it reflects greater responsiveness towards the gut-brain axis and the inter-disciplinary approach to wellness. A positive 76.32% of the study subjects indicated a desire to know more about how to enhance gut health via diet and stress management. When asked if they believed changing their diet might stabilize stress, 57.89% were in agreement, 23.68% disagreed, and 18.42% had no opinion. The notion that food influences mood and psychological state is finally being accepted by the scientific community. Diet rich in omega-3 fatty acids, magnesium, tryptophan, and antioxidants supports mood, while sugar and ultra-processed diets support elevated anxiety and depression. Only 13.16% of them confessed daily physical exercise, 55.26% confessed occasional exercise, and 7.89% confessed regular exercise. Shockingly, 23.68% never engaged in physical activity. Regular exercise is crucial for gut motility, increasing microbiota diversity, and stress modulation. Low physical activity levels could be contributing to both poor gut and mental health. Stimulating regular movement, even the simplest exercises such as walking or yoga, could take a huge leap forward in improving participants’ welfare. Sleep time was also a significant factor that was studied. A mere 31.58% claimed to have slept for 7–8 h—the amount most adults need. Almost half (44.74%) slept for just 4–6 h, while 18.42% slept less than 4 h, and only 5.26% slept more than 8 h shown in Fig. 5. Poor sleep is a well-known cause of increased stress levels, poor digestion, compromised immunity, and hormonal imbalance. Sleep deprivation interferes with the gut-brain axis, influencing appetite control, microbial diversity, and mood. The majority of participants (78.95%) indicated abstinence from smoking and alcohol, which is a good sign of health-aware behavior. Nevertheless, 18.42% smoked and 2.63% drank alcohol.
Perceived stress management ability
The most frequently cited source of stress was work or school duties, particularly since the majority of student respondents would have been busy with school activities. School stress arises from expectations to perform, workload, fear of failure, and uncertainty regarding future opportunities. In the workplace setting, workplace stress may be motivated by employment insecurity, overtime hours, unrealistically short deadlines, or inadequate management. Surprisingly, family obligations are nearly as large a stressor as study/work responsibilities. These might encompass caregiving, parental expectations, conflicts, or emotional labor. In younger adults, reconciling family expectations and individual aspirations usually proves to be a source of stress. Second only to financial issues, nearly one-third of respondents experience economic insecurity due to student loans, inflation, and uncertainty in the job market. Economic insecurity remains a major concern with these issues. Financial distress is inextricably connected to food insecurity and mental health issues, and could potentially worsen unhealthy dietary habits (e.g., processed, cheap foods) that harm gut microbiota. Even though less common, health problems (14.89%) and “other” unspecified sources (12.77%) remain significant stress generators. Long-term illness, disability, or fears regarding bodily function can cause ongoing stress burdens. The “other” category possibly encompasses relationship stress, social media, or existential fears, which are less measurable but no less pervasive. Meditation and yoga, though viewed by only 12.77%, are increasingly being used to reduce stress, improve concentration, and positively influence brain chemistry and intestinal function via the vagus nerve. Emotional eating is noted by a mere 2.13%, which is surprisingly low given the widely reported correlation of stress with increased craving for high-calorie, high-fat foods. It is possible that this behavior is not being accurately reported due to social desirability bias. Emotional eating can lead to unhealthy gut microbiota profiles and metabolic dysregulation. A significant percentage of participants (25.53%) mentioned employing “other” strategies to deal, possibly writing in a journal, prayer, hobby, sleep, or even unhealthy activities like substance use.
These results indicate that although most feel they are coping with stress moderately to well (levels 3–5), a substantial number (38.3%) perceive their stress management as poor or very poor (levels 1–2). This subjective assessment is important, as inadequate stress management has been linked with a higher risk of psychological disorders, cardiovascular disease, and gastrointestinal distress.
Enns et al. explored the interaction between emotional intelligence (EI), coping, and perceived stress in 203 university students in helping fields. The results identified that greater EI was linked to lower perceived stress, a relationship partly mediated through coping. That is, students with higher EI employed more adaptive and fewer maladaptive coping strategies, which impacted their stress levels. These findings suggest that the development of EI can be an effective way to reduce students’ stress levels in helping professions. The authors recommend incorporating the development of EI into training in education to facilitate the coping skills of students [16].
Dietary patterns and gut microbiota
Each category’s frequency (Daily, 3–5 times/week, 1–2 times/week, Rarely/Never) represents different levels of dietary dependence and preference, thus contributing to a better picture of overall diet quality and possible health consequences. The statistics indicate that snacking between meals is fairly moderate among the population, with the highest percentage (37.21%) reporting that they never or seldom snack, and a significant 56.98% occasionally snack (1–5 times a week). A mere 5.81% snack every day. Snacking is usually linked with excessive calorie consumption and inappropriate dietary selection, provided the snacks are processed food, high in sugar, salt, and fat content. Controlled and cautious snacking on fruits, nuts, or yogurt, however, can contribute towards maintaining blood sugar levels and averting excess intake in course meals. The comparatively low rate of daily snacking indicates controlled practice but translates into some doubts regarding the appropriateness of the frequency of snacks consumed by habitual snackers. Consume of eggs seems quite prevalent, with 81.40% of the population consuming eggs in some measure. The biggest segment consumes eggs 1–2 times a week (36.05%), followed by 3–5 times a week (26.74%). Daily consumers contribute a considerable share of 18.60% shown in Fig. 4. Eggs are a food high in quality protein, essential fatty acids, vitamins (notably B12 and D), and minerals such as choline and selenium. Only a small portion (3.49%) eats meat daily, while 12.79% rarely or never consume it. Meat is an important source of intact proteins, iron, B vitamins (particularly B12), and zinc. Red meat consumption in excess, however, especially processed, has been associated with greater cardiovascular disease, colorectal cancer, and metabolic disorder risks. The evidence supports a balanced meat intake, and most individuals eat it in moderation. The lower daily consumption may lower related chronic disease risks without compromising protein intake when combined with plant sources. Whole grain intake is still restricted. Only 17.44% eat whole grains every day, and yet another 55.81% consume them once a week. A whopping 26.74% hardly ever or never eat whole grains. Caffeinated drinks are drunk on a daily basis by more than one third of respondents, and over 59% drink them once a week or more. Fast food eating is fairly widespread, with 62.79% consuming it 1–5 times weekly. Only 2.33% eat it every day, and roughly one-third (34.88%) hardly ever or never eat fast food. Fast foods are usually high in saturated fats, salt, added sugars, and calories, and low in fiber and nutrients. Regular eating is linked to obesity, cardiovascular disease, and metabolic syndrome. The evidence exhibits a moderate trend, where fast food is kept to once or twice a week by the majority of consumers. Although better than daily intake, public health promotion should be encouraged to reduce consumption frequencies further and promote alternatives such as home preparation or healthy meal-preparation dishes.
Most of the population has a high consumption of 1–2 meals a day, while others eat three or more meals a day. Eating frequency can influence metabolic functions and gut microbiota. Normal eating habits may enhance a rich microbial environment, while irregular eating might interfere with microbial balance. Diet contributes to the modulation of stress levels. Some dietary patterns, especially those high in fiber and fermented foods, have been linked with lower perceived stress. The inclusion of a variety of nutrient-dense foods can contribute to mental health and alleviate stress-related gastrointestinal symptoms. Physical activity is different for different people, with some exercising regularly and others less frequently. Physical activity has been demonstrated to have a positive effect on gut microbiota diversity and function. Exercise can increase microbial diversity, enhance gut barrier function, and decrease inflammation. Sleep quality and duration are essential for gut health. Sufficient sleep helps maintain a healthy gut microbiome, whereas sleep deprivation can harm microbial balance. Encouraging good sleep hygiene could be useful in preserving gut health. The Knight et al., 2024 study, examines the relationship between psychosocial stress and diet to gut microbiota composition and diversity in young adult Black and White women. African American (AA) women had significantly reduced alpha diversity (as indicated by amplicon sequence variant [ASV] count) and lower abundance of the genus Blautia than European American (EA) women. AA women further had increased perceived stress, lifetime discrimination, and higher hair cortisol levels. There were positive correlations between discrimination experience reports and the richness of the genus. Negative correlation was between discrimination and richness of genus Blautia. There were negative correlations between perceived stress and overall microbial richness and richness of the genus. Increased consumption of trans fats and sweet foods was linked with reduced microbial diversity. Fiber consumption was positively correlated with the relative abundance of Lachnospiraceae NK4A136 but negatively correlated with Eubacterium coprostanoligenes. The research failed to identify that dietary components or cortisol status mediated the association between psychosocial stress and diversity of gut microbiota or targeted abundances of specific bacteria [17].Kim et al. (2018) found that adult personality traits are predictive of gut microbiota diversity, and this affirms the gut-brain axis in behavior. Those with higher neuroticism and lower conscientiousness had more Gammaproteobacteria and Proteobacteria—microbes commonly linked with inflammation. Higher conscientiousness, however, was positively correlated with butyrate-producing Lachnospiraceae, health-promoting bacteria linked to gut health. Although these observed correlations were small, they were statistically significant and suggest that personality may affect, or be affected by, the gut microbiome. They contribute to growing evidence that psychological and behavioral traits have biological correlates in the gut microbial community [18]. Fahad and Bukhari (2024) explored the role of the gut-brain axis in psychiatry in the special nutritional and social environment of Pakistan. They highlighted the interdependent relationship between the gut microbiota and the brain, with regard to how an imbalance of microbes influences mood disorders such as anxiety and depression. They observed that diet, stress, and culture heavily influence gut microbiota composition and, consequently, mental health. The authors promoted the incorporation of microbiota-targeted interventions, including diet changes and probiotics, in mental health measures. This study highlights the significance of considering local dietary and cultural practices when treating mental health through the gut-brain axis [19].
Strength and weakness
The research highlights the importance of gut well-being and stress management in preventing various mental and physical conditions. It offers useful pointers to preventive medicine and public health policy, with early intervention through dietary and lifestyle changes. Use of validated instruments such as Food Frequency Questionnaires (FFQs) and dietary recalls enhances the precision and consistency of nutrient intake data.
Cross-sectional design restricts the causal effect and long-term influence of stress or food on gut microbiota. Social desirability, recollection bias, and cultural factors make self-report measures of stress and diet intake challenging. Insufficient longitudinal follow-up prevents us from ascertaining the effects of dietary intervention or stress on long-term gastrointestinal and mental health. For facilitating replicability worldwide, future studies must facilitate cooperation between disciplines and use publicly available food and microbiome data.
Future research directions
Here the association of gut microbiota, diet, and stress is accentuated; however, the methodological approach is needed to be developed by future research to quantify and look into causal processes and prioritize real-life applications. To validate their impacts on the gut-brain axis, interventional trials with dietary change, probiotic/prebiotic treatment, and stress management need to be performed. To measure the functional impact of microbiota, for instance, the significant metabolites such as SCFAs, neurotransmitters, and bile acids, several ‘omics’ approaches such as metabolomics are required. As their characteristic microbiome signs and response to treatments, vulnerable populations (adolescents, pregnant women, elderly, and mentally ill) must be the first to be targeted in the initial research. Research on the biologic mechanisms through which gut microbiota affect brain activity—using brain imaging, vagus nerve stimulation, neuro-inflammatory markers, and levels of hormones are imperative. Interpreting these findings into dietary advice, mental health interventions, and population campaigns can facilitate the promotion of gut health and stress resilience and consequent decrease in the burden of chronic disease.
Conclusion
The subjects were emphatically stating that stress was affecting their digestive health, pointing towards the direct connection of mental anguish and gut health. Stress has been shown to impair the mucous layer, alter the motility of the gut, and induce intestinal inflammation, resulting in symptoms of irritable bowel syndrome (IBS), bloating, and altered bowel habits. Gastrointestinal symptoms further appear widespread and ubiquitous among the studied population, suggesting a chronic pattern most likely resulted from both stress and poor dietary patterns. Remarkably, although most individuals believe that stress-releasing eating is possible, extremely few regularly practice eating patterns consistent with such belief—awareness vs. behavior gap. Frequent consumption of dietary supplements such as probiotics and vitamins indicates increased concern with measures of gut health. Though supplementation can respond to deficiency, it cannot substitute the long-term advantages of a balanced whole-food diet and lifestyle.
Acknowledgements
The Authors are thankful to Nur International University, Lahore, Pakistan for providing the research facilities for this study. We confirm the final authorship for this manuscript and ensure that anyone else who contributed to the manuscript but does not qualify for authorship has been acknowledged with their permission. We acknowledge that all listed authors have made a significant scientific contribution to the research in the manuscript approved its claims and agreed to be an author.
Appendix
Author contributions
Faiyaz Ahmed1, Fahad Saad Alhodieb1, Saleh A. Alsanie1, Musarrat Rasheed2, Catherine Tamale Ndagire-all the authors take part equally.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability
Data Availability Even though adequate data has been given in the form of tables and figures, however, all authors declare that if more data required then the data will be provided on a request basis from corresponding author Catherine Tamale Ndagire.
Declarations
Ethics approval and consent to participate
This study involved human participants and was conducted with ethical approval from the Institutional Review Board of Nur International University (IRB Reg. NIU-112-23) by following all the guidelines of National Biosafety Rules 2005, Punjab Biosafety Rules 2014, Punjab Animal Health Act 2019, and in compliance with the Helsinki Declaration. Informed consent was obtained from all participants prior to their inclusion in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Álvarez J, et al. Gut microbes and health. Gastroenterología y Hepatología. (English Edition). 2021;44(7):519–35. [DOI] [PubMed] [Google Scholar]
- 2.Ge L, et al. Psychological stress in inflammatory bowel disease: psychoneuroimmunological insights into bidirectional gut–brain communications. Front Immunol. 2022;13:1016578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drela N. Neuro-Endocrine-Immune interactions in maintaining the integrity of the Body, in PsychoNeuroImmunology: volume 1: integration of psychology, neurology, and immunology. Springer; 2025. pp. 17–57.
- 4.Dubinski P, Czarzasta K, Cudnoch-Jedrzejewska A. The influence of gut microbiota on the cardiovascular system under conditions of obesity and chronic stress. Curr Hypertens Rep. 2021;23(5):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qin L, Lv W. Dietary content and eating behavior in ulcerative colitis: a narrative review and future perspective. Nutr J. 2025;24(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kodidala S, et al. Unraveling the intricacies of the gut-brain axis: from physiology to psychology and obesity. Сибирский научный медицинский журнал. 2024;44(5):19–23. [Google Scholar]
- 7.Samaripour H. Neurotransmitters and mental health: understanding the chemical underpinnings of psychological disorders. Int J New Chem. 2025;12(4):825–41. [Google Scholar]
- 8.Madison AA, Bailey MT. Stressed to the core: inflammation and intestinal permeability link stress-related gut microbiota shifts to mental health outcomes. Biol Psychiatry. 2024;95(4):339–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitrea L, et al. Guts imbalance imbalances the brain: a review of gut microbiota association with neurological and psychiatric disorders. Front Med. 2022;9:813204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cade JE, et al. Food-frequency questionnaires: a review of their design, validation and utilisation. Nutr Res Rev. 2004;17(1):5–22. [DOI] [PubMed] [Google Scholar]
- 11.Reis RS, Hino A, Añez C. Perceived stress scale. J Health Psychol. 2010;15(1):107–14. [DOI] [PubMed] [Google Scholar]
- 12.Huizingh EK. Applied statistics with SPSS. 2007.
- 13.Alexander LB, Kaye LW. Part-time employment for the Low-income elderly: experiences from the field. Routledge; 2021.
- 14.Pintelon O, et al. The social stratification of social risks: the relevance of class for social investment strategies. J Eur Soc Policy. 2013;23(1):52–67. [Google Scholar]
- 15.Roman G. Dietary patterns and their association with obesity: a cross-sectional study. Acta Endocrinologica (Bucharest). 2019;15(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Enns A, et al. Perceived stress, coping strategies, and emotional intelligence: a cross-sectional study of university students in helping disciplines. Nurse Educ Today. 2018;68:226–31. [DOI] [PubMed] [Google Scholar]
- 17.Knight RO, et al. A cross-sectional study observing the association of psychosocial stress and dietary intake with gut microbiota genera and alpha diversity among a young adult cohort of black and white women in Birmingham, Alabama. BMC Womens Health. 2024;24(1):142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim Han-Na, Yeojun Yun, Seungho Ryu, Yoosoo Chang, Min-Jung Kwon, Juhee Cho, Hocheol Shin, and Hyung-Lae Kim. Correlation between gut microbiota and personality in adults: A cross-sectional study. Brain Behav Immun.2015;69: 374-385. 10.1016/j.bbi.2017.12.012 [DOI] [PubMed]
- 19.Fahad M, Bukhari B. The gut-brain axis: exploring the relationship between microbiota and mental health. Am Int J Biology Life Sci. 2024;6(1):1–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data Availability Even though adequate data has been given in the form of tables and figures, however, all authors declare that if more data required then the data will be provided on a request basis from corresponding author Catherine Tamale Ndagire.