Abstract
Prostate cancer is the most common invasive malignancy and the second leading cause of cancer-related deaths among U.S. males, with a similar trend in many Western countries. One approach to control this malignancy is its prevention through the use of agents present in diet consumed by humans. Pomegranate from the tree Punica granatum possesses strong antioxidant and antiinflammatory properties. We recently showed that pomegranate fruit extract (PFE) possesses remarkable antitumor-promoting effects in mouse skin. In this study, employing human prostate cancer cells, we evaluated the antiproliferative and proapoptotic properties of PFE. PFE (10-100 μg/ml; 48 h) treatment of highly aggressive human prostate cancer PC3 cells resulted in a dose-dependent inhibition of cell growth/cell viability and induction of apoptosis. Immunoblot analysis revealed that PFE treatment of PC3 cells resulted in (i) induction of Bax and Bak (proapoptotic); (ii) down-regulation of Bcl-XL and Bcl-2 (antiapoptotic); (iii) induction of WAF1/p21 and KIP1/p27; (iv) a decrease in cyclins D1, D2, and E; and (v) a decrease in cyclin-dependent kinase (cdk) 2, cdk4, and cdk6 expression. These data establish the involvement of the cyclin kinase inhibitor-cyclin-cdk network during the antiproliferative effects of PFE. Oral administration of PFE (0.1% and 0.2%, wt/vol) to athymic nude mice implanted with androgen-sensitive CWR22Rν1 cells resulted in a significant inhibition in tumor growth concomitant with a significant decrease in serum prostate-specific antigen levels. We suggest that pomegranate juice may have cancer-chemopreventive as well as cancer-chemotherapeutic effects against prostate cancer in humans.
Keywords: apoptosis, cell cycle, prostate-specific antigen, androgen receptor
Prostate cancer (CaP) is the second leading cause of cancer-related deaths among men in the U.S. and many Western countries (1). For the year 2005, it has been estimated that 232,090 new cases of CaP will be diagnosed and that 30,350 deaths related to CaP will occur in the U.S. alone (1). Although the treatment of localized CaP remains controversial, there are potentially curative options such as radical prostatectomy or radiotherapy. However, once the disease is metastatic, the outlook for the patient is poor. Thus, developing new strategies to combat CaP has become an important mission. Chemoprevention, which refers to the administration of synthetic or naturally occurring agents to suppress, reverse, or delay the process of carcinogenesis, is being increasingly appreciated as an effective approach for the management of neoplasia (2-5). This approach is ideally suited for CaP because it is typically diagnosed in men >50 years of age, and thus even a modest delay in disease progression could significantly impact the quality of life of these patients (6). In this regard, several naturally occurring antioxidants for chemoprevention of CaP are being evaluated in cell culture and in animal model systems (2-6). Some of these agents are showing promise in human CaP patients (3, 6-9).
Pomegranate (Punica granatum, Punicaceae), native to Persia, is an edible fruit cultivated in Mediterranean countries, Afghanistan, India, China, Japan, Russia, and some parts of the United States. In ancient Greek mythology, pomegranates were known as the “fruit of the dead.” Pomegranate has been extensively used as a folk medicine by many cultures (10). Edible parts of pomegranate fruit (≈80% of total fruit weight) are comprised of 80% juice and 20% seed. Pomegranate fruit is a rich source of two types of polyphenolic compounds: anthocyanins (such as delphinidin, cyanidin, and pelargonidin), which give the fruit and juice its red color; and hydrolyzable tannins (such as punicalin, pedunculagin, punicalagin, gallagic, and ellagic acid esters of glucose), which account for 92% of the antioxidant activity of the whole fruit (11). The soluble polyphenol content in pomegranate juice varies between 0.2 and 1.0% (12). It has been shown that the antioxidant activity of pomegranate juice is higher than that of red wine and green tea (11), two dietary substances that are showing promise in preclinical CaP models and in CaP patients (6, 7, 13-19). Pomegranate juice was also found to exert potent antioxidant capacity against lipid peroxidation, which may be a central link for the antiatherogenic effect of pomegranate on lipoprotein, macrophage, and platelets (20, 21). Dietary supplementation of polyphenol-rich pomegranate juice to atherosclerotic mice was recently shown to inhibit significantly the development of atherosclerotic lesions (22). Schubert et al. (23) have shown that pomegranate wine may serve as a potent inhibitor of NF-κB in vascular endothelial cells. It has been shown that pomegranate seed oil and polyphenols in fermented juice retard oxidation and prostaglandin synthesis, inhibit breast cancer cell proliferation and invasion, and promote breast cancer cell apoptosis (24). More recently, we have shown that topical application of pomegranate fruit extract (PFE) prevents phorbol 12-myristate 13-acetate-induced tumor promotion in 7,12-dimethybenz(a)anthracene-initiated CD-1 mouse skin (25).
We hypothesized that PFE may afford chemopreventive as well as cancer-chemotherapeutic effects against CaP. Here, we show that PFE, through modulations in the cyclin kinase inhibitor-cyclin-cyclin-dependent kinase (cdk) machinery, results in inhibition of cell growth followed by apoptosis of highly aggressive human prostate carcinoma PC3 cells. These events were associated with alterations in the levels of Bax and Bcl-2 shifting the Bax:Bcl-2 ratio favoring apoptosis. Furthermore, we show that oral administration of a human acceptable dose of PFE to athymic nude mice implanted with CWR22Rν1 cells resulted in significant inhibition of tumor growth with concomitant reduction in secretion of prostate-specific antigen (PSA) in the serum.
Materials and Methods
Materials. cdk2, cdk4, cdk6, WAF1/p21, KIP1/p27, PSA, and androgen receptor (AR) antibodies were obtained from Santa Cruz Biotechnology. Cyclin D1, D2, and E antibodies were procured from Neomarker (Fremont, CA). Poly (ADP-ribose) polymerase (PARP), Bcl-2, Bax, Bak, and Bcl-XL antibodies were purchased from Upstate Biotechnology (Lake Placid, NY). Anti-mouse or anti-rabbit secondary antibody horseradish peroxidase conjugate was obtained from Amersham Pharmacia Life Sciences. The Bio-Rad DC Protein Assay Kit was purchased from Bio-Rad. Novex precast Tris-Glycine gels were obtained from Invitrogen. The Annexin-V-FLUOS Staining Kit was purchased from Roche.
Preparation of PFE. As described earlier (25), fresh pomegranates were peeled, and the edible portion was squeezed in 70% acetone/30% distilled water (1:20, wt/vol). The red extract was filtered through Whatman no. 1 filter paper, and the filtrate was condensed, freeze-dried, and stored at 4°C. This extract, PFE, was analyzed by MALDI-TOF MS and was found to contain six anthocyanins (pelargonidin 3-glucoside, cyanidin 3-glucoside, delphinidin 3-glucoside, pelargonidin 3,5-diglucoside, cyanidin 3,5-diglucoside, and delphinidin 3,5-diglucoside) and various ellagitannins and hydrolyzable tannins (25).
Treatment of Cells. Human prostate carcinoma cells PC3 and CWR22Rν1, obtained from American Type Culture Collection, were grown in RPMI medium 1640 (GIBCO) and supplemented with 10% FBS/1% penicillin/streptomycin in a 5% CO2 atmosphere at 37°C. PFE dissolved in dimethyl sulfoxide (DMSO) was used for the treatment of cells. Seventy percent to 80% confluent cells were treated with PFE at 10-100 μg/ml for 48 h in complete cell medium. The final concentration of DMSO used was 0.1% (vol/vol) for each treatment.
Cell Viability. The effect of PFE on the viability of cells was determined by 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazoliumbromide assay. The cells were plated at 1 × 104 cells per well in 200 μl of complete culture medium containing 10-100 μg/ml concentrations of PFE in 96-well microtiter plates for 48 h. After incubation for specified times at 37°C in a humidified incubator, 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazoliumbromide (5 mg/ml in PBS) was added to each well and incubated for 2 h, after which the plate was centrifuged at 1,800 × g for 5 min at 4°C. The absorbance was recorded on a microplate reader at the wavelength of 540 nm. The effect of PFE on growth inhibition was assessed as percent cell viability where DMSO-treated cells were taken as 100% viable. DMSO at the concentrations used was without any effect on cell viability.
Protein Extraction and Western Blotting. After treatment with PFE, the cells were incubated in ice-cold lysis buffer (50 mmol/liter Tris-HCl/150 mmol/liter NaCl/1 mmol/liter EGTA/1 mmol/liter EDTA/20 mmol/liter NaF/100 mmol/liter Na3VO4/0.5% Nonidet P-40/1% Triton X-100/1 mmol/liter PMSF, pH 7.4) with freshly added protease inhibitors (Calbiochem) over ice for 20 min. For Western blotting, 40 μg of protein was resolved over 12% polyacrylamide gels, transferred onto a nitrocellulose membrane, probed with appropriate monoclonal primary antibody, incubated with appropriate secondary antibody horseradish peroxidase conjugate, and detected by chemiluminescence and autoradiography. Densitometric measurements of the bands were done with digitalized scientific software program un-scan-it purchased from Silk Scientific Corporation (Orem, UT).
Apoptosis Detection by Fluorescence Microscopy. The Annexin-VFLUOS Staining Kit was used for the detection of apoptotic and necrotic cells according to the manufacturer's protocol. PC3 cells were grown to ≈70% confluence and then treated with 20-100 μg/ml PFE for 48 h. The fluorescence was measured by a Zeiss 410 confocal microscope. In a selected field, the cells stained with annexin V and propidium iodide and unstained cells were counted to ascertain the extent of apoptosis and necrosis.
ELISA for PSA. The human PSA ELISA kit (Anogen, Ontario, Canada) was used for the quantitative determination of PSA levels in the blood serum of athymic nude mice according to the manufacturer's protocol. The kit uses a technique of quantitative sandwich immunoassay for determination of PSA.
In Vivo Tumor Xenograft Model. Athymic (nu/nu) male nude mice were obtained from NxGen Biosciences (San Diego), housed under pathogen-free conditions with a 12-h light/12-h dark schedule, and fed with an autoclaved diet ad libitum. We chose CWR22Rν1 cells for determining the in vivo effects of PFE based on the fact that these cells form rapid and reproducible tumors in nude mice and secrete significant amounts of PSA in the bloodstream of the host. CWR22Rν1 cells were harvested by trypsinization and resuspended in RPMI medium 1640. To establish CWR22Rν1 tumor xenografts in mice, 6- to 8-week-old athymic mice were injected s.c. with 1 × 106 cells mixed with 50 μl of RPMI plus 50 μl of Matrigel (Collaborative Biomedical Products, Bedford, MA). Twenty-four animals were then randomly divided into three groups consisting of eight animals each. The first group of animals received normal drinking water and served as controls. The animals of groups 2 and 3 received the same drinking water supplemented with 0.1% and 0.2% PFE (wt/vol), respectively. Water bottles were changed every other day. The 0.1% and 0.2% doses of PFE selected for feeding mice are based on the assumption that a typical healthy individual (70 kg) may be persuaded to drink 250 or 500 ml of pomegranate juice extracted from one or two fruits, respectively. Body weight, diet, and water consumption were recorded twice weekly throughout the study. Tumor sizes were measured twice weekly, and tumor volume was calculated by the formula 0.5238 × L1 × L2 × H where L1 is the long diameter, L2 is the short diameter, and H is the height of the tumor (26). Every week, blood samples were collected by the “mandibular bleed” and sera were separated from the whole blood and stored at -20°C until assayed for PSA by specific immunoassay.
Statistical Analysis. All statistical analyses were carried out with prism (GraphPad, San Diego), and P values <0.05 were considered significant. The Kaplan-Meier method was used to estimate survival, and differences were analyzed by the log-rank test.
Results
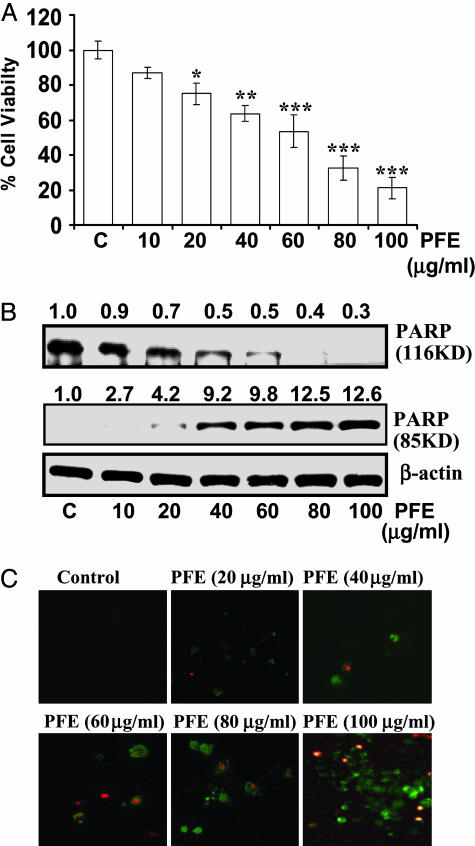
PFE Causes Cell Growth Inhibition and Apoptosis in PC3 Cells. Our first aim was to investigate whether PFE treatment imparts antiproliferative effects against CaP cells. Therefore, using human prostate carcinoma PC3 cells, we first evaluated the effect of PFE on the growth of these cells by 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazoliumbromide assay. As shown in Fig. 1A, PFE treatment (10-100 μg/ml for 48 h) of PC3 cells resulted in a dose-dependent inhibition of cell growth. To assess whether PFE-induced growth inhibition of the cells is mediated through induction of apoptosis, we first evaluated the effect of PFE on cleavage of PARP. As shown in Fig. 1B, employing immunoblot analysis, we found that the full-size PARP protein (116 kDa) was cleaved to yield an 85-kDa fragment after treatment of cells with PFE at 10-100 μg/ml for 48 h. The induction of apoptosis by PFE was also evident from the morphology of cells, as assessed by fluorescence microscopy, after labeling the cells with an apoptosis detection kit containing annexin V and propidium iodide (Fig. 1C). We used this method because it identifies the apoptotic (green fluorescence) as well as necrotic (red fluorescence) cells. As shown by the data in Fig. 1C, PFE treatment resulted in a dose-dependent apoptosis in PC3 cells. These data indicated that PFE treatment also resulted in necrosis of these cells, which may be a secondary event in the apoptotic process.
Fig. 1.
Effect of PFE treatment of PC3 cells on cell growth and apoptosis. (A) Effect on cell growth. The cells were treated with PFE for 48 h, and the viability of cells was determined by 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazoliumbromide assay. Data shown are mean ± SD of three separate experiments in which each treatment was repeated in 10 wells. *, P < 0.05; **, P < 0.01; ***, P < 0.001 vs. control. (B) Effect on cleavage of PARP. The cells were treated with vehicle only or specified concentrations of PFE for 48 h and harvested, and cell lysates were prepared. The data are representative of three independent experiments with similar results. The values above the blots represent the change in the protein expression of the bands normalized to β-actin where vehicle-treated cells are represented as 1.0. (C) Dose-dependent effect of PFE on morphological changes as detected by fluorescence microscopy. Apoptotic cells are stained with annexin V (green fluorescence), and necrotic cells are stained with propidium iodide (red fluorescence). Details are described in Materials and Methods.
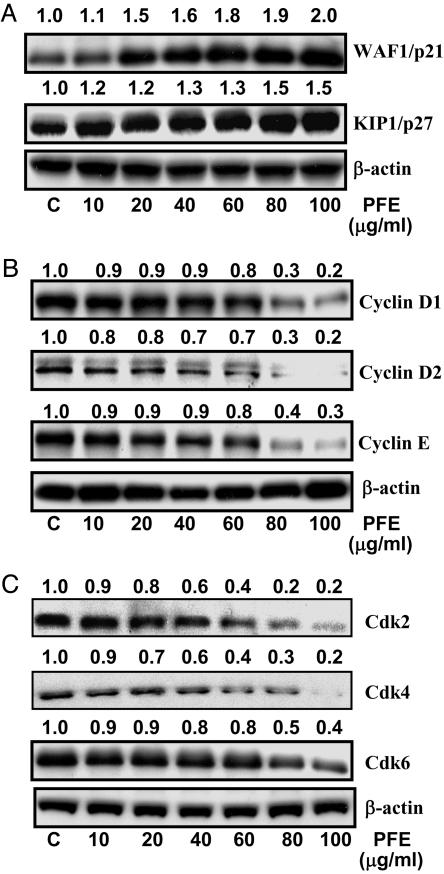
PFE Induces Apoptosis Through an Induction in WAF1/p21/KIP1/p27 with Inhibition in Cyclins and cdks. Because our studies demonstrated that PFE treatment of PC3 cells resulted in apoptosis of PC3 cells, we examined the effect of PFE on cell-cycle-regulatory molecules operative in the G1 phase of the cell cycle. We assessed the effect of PFE on the induction of WAF1/p21 and KIP/p27, which are known to regulate the entry of cells at the G1-S phase transition checkpoint and induce apoptosis. Immunoblot analysis revealed that PFE treatment of the cells resulted in a marked induction of WAF1/p21 and KIP1/p27 in a dose-dependent manner compared with the basal levels (Fig. 2A). Using immunoblot analysis, we also assessed the effect of PFE treatment on the protein expressions of the cyclins and cdks, which are known to be regulated by WAF1/p21. PFE treatment of the cells resulted in a dose-dependent decrease in protein expressions of cyclin D1, cyclin D2, and cyclin E (Fig. 2B), as well as cdk2, cdk4, and cdk6 (Fig. 2C).
Fig. 2.
Effect of PFE treatment of PC3 cells on protein expression of WAF1/p21 and KIP1/p27 (A), cyclins D1, D2, and E (B), and cdk2, cdk4, and cdk6 (C). The cells were treated with vehicle only or specified concentrations of PFE for 48 h and harvested, and cell lysates were prepared. The data are representative of three independent experiments with similar results. The values above the blots represent the change in the protein expression of the bands normalized to β-actin where vehicle-treated cells are represented as 1.0.
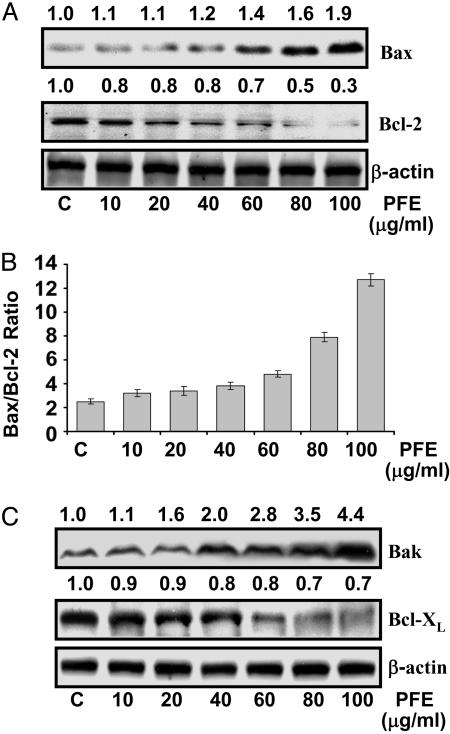
PFE Modulates Bax and Bcl-2 Protein Expression in PC3 Cells. Because Bax and Bcl-2 play crucial roles in apoptosis, we next studied the dose-dependent effects of PFE on the protein levels of Bax and Bcl-2 in PC3 cells. The immunoblot analysis exhibited an increase in the protein expression of Bax (Fig. 3A). In contrast, the protein expression of Bcl-2 was significantly decreased by PFE treatment in a dose-dependent fashion (Fig. 3A). In our study we also found a significant dose-dependent shift in the ratio of Bax to Bcl-2 after PFE treatment, indicating the induction of an apoptotic process (Fig. 3B). Furthermore, we assessed the protein levels of Bak (proapoptotic) and Bcl-XL (antiapoptotic). The immunoblots revealed a significant increase in the protein expression of Bak and a significant decrease in Bcl-XL expression by PFE treatment in a dose-dependent fashion in PC3 cells (Fig. 3C), thus further confirming the induction of apoptotic process.
Fig. 3.
Effect of PFE treatment of PC3 cells on protein expression of Bax and Bcl2 (A), Bax/Bcl2 ratio (B), and protein expression of Bak and Bcl-XL (C). The cells were treated with vehicle only or specified concentrations of PFE for 48 h and harvested, and cell lysates were prepared. The data are representative of three independent experiments with similar results. The values above the blots represent the change in the protein expression of the bands normalized to β-actin where vehicle-treated cells are represented as 1.0.
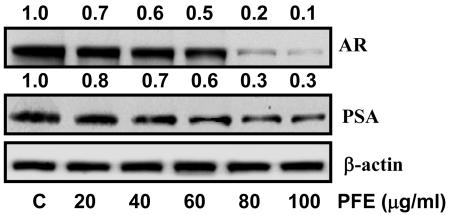
PFE Decreases AR and PSA Expression in CWR22Rν1 Cells. Evidence suggests that androgens are also involved in the development and progression of CaP, where AR is the essential mediator for androgen action (27). In addition, PSA is a clinical diagnostic marker for monitoring the presence and progression of CaP in human patients (28). Because PC3 cells are androgen-independent, are devoid of AR, and do not produce PSA, we selected androgen-responsive CWR22Rν1 cells for these studies, because they express AR and also secrete PSA in the bloodstream of the host. To accomplish this work, we first established that, like PC3 cells, growth of CWR22Rν1 cells is also inhibited by PFE (data not shown). Then we determined the effect of PFE treatment of CWR22Rν1 cells on the AR protein expression and found a significant decrease in its expression in a dose-dependent manner (Fig. 4). At 80 and 100 μg/ml concentrations of PFE, 80% and 90% decreases in AR were observed, respectively (Fig. 4). Recent studies have shown that modulation in AR leads to alteration in androgen-responsive genes (29). One of the androgen-responsive genes is PSA, which is specifically expressed in prostatic tissue and at present is the most sensitive biomarker and screening tool for CaP in humans (29, 30). The CWR22Rν1 cells exhibit high protein levels of intracellular PSA, as evidenced by a 34-kDa band. The dose-dependent effect of PFE on CWR22Rν1 cells exhibited a significant decrease in PSA protein levels by 17%, 28%, 38%, 62%, and 67% at 20, 40, 60, 80, and 100 μg/ml concentrations, respectively (Fig. 4).
Fig. 4.
Effect of treatment of PFE to CWR22Rν1 cells on protein expression of intracellular PSA and AR. The cells were treated with vehicle only or specified concentrations of PFE for 48 h and harvested, and cell lysates were prepared. The data shown are representative of three independent experiments with similar results. The values above the blots represent the change in the protein expression of the bands normalized to β-actin where vehicle-treated cells are represented as 1.0.
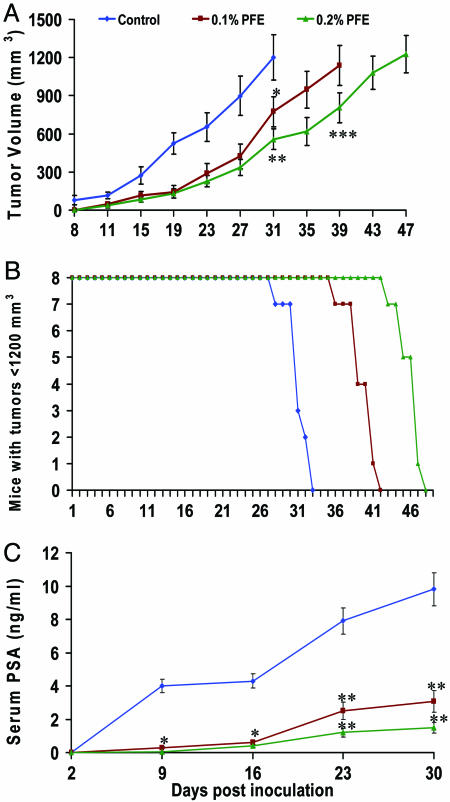
PFE Inhibits Growth of Human Prostate Carcinoma CWR22Rν1 in Nude Mice. PFE given as the sole source of drinking fluid to the nude mice resulted in an inhibition of prostate carcinoma CWR22Rν1 tumor xenograft growth in nude mice. Eight days after cell inoculation, the appearance of small solid tumors was observed in animals receiving water as a drinking fluid. This latency period was prolonged to 11-14 days in animals receiving PFE in drinking fluid. PFE (0.1% and 0.2%) was administered orally ad libitum to these animals day 1 after tumor cell implantation. As shown in Fig. 5 A and B, tumor growth, as inferred by computed tumor volume, was significantly inhibited in mice receiving both 0.1% and 0.2% PFE, with higher inhibitory effects in animals receiving 0.2% PFE than in those receiving 0.1% PFE. In our experimental protocol, we killed the animals when the implanted tumor reached a volume of 1,200 mm3. Thus, as shown in Fig. 5A, in water-fed animals the average tumor volume of 1,200 mm3 was reached in ≈31 ± 3 days after tumor cell inoculation. At this time point, the average tumor volumes of the 0.1% and 0.2% PFE-fed groups were 776 and 558 mm3, respectively. The most effective tumor growth inhibitory response was observed in the 0.2% PFE-fed group, where the targeted average tumor volume of 1,200 mm3 was reached at day 47 ± 4 after tumor cell inoculation. PFE treatment of 0.1% was also found to be significantly effective where the average tumor volume of 1,200 mm3 was achieved in ≈39 ± 3 days after tumor cell inoculation. Tumor data were analyzed for survival probability by Kaplan-Meier analysis, which indicated that continuous PFE infusion to athymic nude mice resulted in increased survival (P < 0.0001, log-rank test), with a median survival of 39 and 47 days (0.1% and 0.2% PFE, respectively), compared with 31 days in water-fed mice (P < 0.0001, log-rank test) (data not shown).
Fig. 5.
Effect of oral administration of PFE on CWR22Rν1 tumor growth and PSA secretion in athymic nude mice. Approximately one million CWR22Rν1 cells were s.c. injected in each flank of the mouse to initiate tumor growth. Twenty-four hours after cell implantation, the control group of animals continued to receive sterilized drinking water whereas animals of group 2 and group 3 received 0.1% and 0.2% PFE, respectively, in the same drinking water ad libitum. Water bottles were changed every other day. Once tumors started to grow, their sizes were measured twice weekly and the tumor volume was calculated. (A) Average tumor volume of water-fed, 0.1% and 0.2% PFE-fed mice plotted over days after tumor cell inoculation. Values represent mean ± SD of eight animals. *, P < 0.01; **, P < 0.001 vs. the water-fed group of mice; ***, P < 0.01 vs. the 0.1% PFE-fed group of mice. (B) Number of mice remaining with tumor volumes ≤1,200 mm3 after they consumed 0.1% and 0.2% PFE for the indicated days. (C) Serum PSA levels were analyzed by ELISA. Values represent mean ± SE of eight animals. *, P < 0.01; **, P < 0.001 vs. the water-fed group of mice. Details are described in Materials and Methods.
PFE Inhibits PSA, a Marker for CaP Progression. During the course of tumor growth in animals at day 2, 9, 16, 23, and 30 after inoculation, blood was collected through the mandibular bleed. Quantitative sandwich ELISA was used to determine PSA levels in mouse serum secreted by CWR22Rν1 tumor xenografts. In PFE-fed animals a significant inhibition of PSA secretion was observed at all time points examined (Fig. 5C). At 23 days after inoculation, secreted PSA levels were 7.9 ± 0.82, 2.5 ± 0.58, and 1.2 ± 0.97 ng/ml in water-fed, 0.1% PFE-fed, and 0.2% PFE-fed animals, respectively. At 30 days after inoculation of tumor cells in 0.1% and 0.2% PFE-fed animals, 70% (P < 0.001) and 85% (P < 0.001) reduced levels of PSA were observed as compared with the water-fed group, respectively (Fig. 5C). Thus, our data clearly demonstrated that PFE feeding to mice resulted in a significant decrease in the serum PSA of animals. Interestingly, the effects of PFE on PSA secretion were found to closely correlate with tumor growth inhibition (Fig. 5 A and C).
Discussion
In recent years, naturally occurring antioxidant compounds present in the diet consumed by humans have gained considerable attention as cancer-chemopreventive and chemotherapeutic agents (2, 4, 5, 7). Recently, we have shown that topical application of PFE prevents 7,12-dimethybenz(a)anthracene-initiated phorbol 12-myristate 13-acetate-induced tumor promotion in CD-1 mouse skin (25). Because pomegranate juice has been shown to possess remarkable antioxidant effect (25) and because some antioxidants are showing promise in prevention and therapy of CaP (6, 13, 31, 32), in this study we investigated whether the pomegranate-juice-derived PFE could be a beneficial agent for CaP in humans. We show that PFE possesses antiproliferative and proapoptotic effects through modulation of cyclin kinase inhibitor-cyclin-cdk machinery in aggressive human CaP PC3 cells. Our data demonstrate that PFE treatment of the PC3 cells resulted in (i) cell growth inhibition, (ii) alterations in the cell cycle regulatory molecules operative in the G1 phase of the cell cycle, and (iii) apoptosis in a dose-dependent fashion. These are important observations because regulation of cell cycle and apoptosis have become appreciated targets for intervention against cancer (33-37).
We and others have shown the involvement of cell cycle regulation-mediated apoptosis as a mechanism of cell growth inhibition by many dietary antioxidants (38-40). Therefore, in the present study we investigated the involvement of the cyclin kinase inhibitor-cyclin-cdk machinery during the induction of cell cycle arrest and apoptosis by PFE in PC3 cells. In eukaryotes, passage through the cell cycle is orchestrated by a family of protein kinase complexes (41). Each complex is composed minimally of a catalytic subunit, the cdk, and its essential activating partner, the cyclin (41). Cyclins D and E are involved during G1-S phase of the cell cycle. In controlled cell growth, association of cyclins D and E with cdk2, cdk4, or cdk6 leads to phosphorylation of Rb and its release from E2F, resulting in progression of the cell cycle and cellular proliferation. Any defect in this machinery results in an altered cell cycle regulation that may result in unwanted cellular proliferation, ultimately culminating in the development of cancer (41). During the progression of the cell cycle, the cdk-cyclin complexes are inhibited via binding to cyclin kinase inhibitors such as the WAF1 and KIP1 families of proteins (42). Thus, we examined the effect of PFE on cell cycle regulatory molecules operative in the G1 phase of the cell cycle. Our data demonstrate a significant up-regulation of the WAF1/p21 and KIP1/p27 during G1 phase arrest and apoptosis of these cells by PFE (Fig. 2 A). In the absence of active p53 in PC3 cells, the observed induction of WAF1/p21 and KIP1/p27 by PFE appears to be independent of p53. It has been shown in many studies that exogenous stimuli may result in a p53-dependent, as well as a p53-independent, induction of WAF1/p21 and KIP1/p27, which may cause a blockade of G1-S phase transition, resulting in a G1 phase cell cycle arrest and apoptosis (38, 43). WAF1/p21 and KIP1/p27 are considered universal inhibitors of cyclin-cdk complexes; therefore, we assessed the effect of PFE treatment on the cyclins and cdks operative in the G1 phase of the cell cycle (i.e., cyclins D1, D2, and E and cdk2, cdk4, and cdk6). We found that PFE treatment of the cells resulted in significant down-modulation of all of these regulatory molecules, although to a different extent (Fig. 2 B and C).
The apoptosis of PC3 cells induced by PFE is important because it is a physiological process that functions as an essential mechanism of tissue homeostasis and is regarded as the preferred way to eliminate unwanted cells (4). This observation was verified by PARP cleavage and fluorescence microscopy (Fig. 1 B and C). Collectively, these results suggest that PFE inhibits the growth of prostate carcinoma cells through cell cycle arrest and induces apoptosis.
Members of the Bcl-2 family of proteins are critical regulators of the apoptotic pathway (44). Bcl-2 is an upstream effector molecule in the apoptotic pathway and is identified as a potent suppressor of apoptosis (44). Bcl-2 is found at inappropriately high levels in more than half of all human tumors (44). Bcl-2 has been shown to form a heterodimer complex with the proapoptotic member Bax, thereby neutralizing its proapoptotic effects. Therefore, the ratio of Bax/Bcl-2 is a decisive factor and plays an important role in determining whether cells will undergo death or survival. In our study, PFE treatment of PC3 cells for 48 h was found to result in a decrease in Bcl-2 protein expression with an increase in the protein expression of Bax (Fig. 3A). Importantly, in PFE-treated cells, the ratio of Bax to Bcl-2 was found to be altered in favor of apoptosis (Fig. 3B). Our results thus suggest that up-regulation of Bax and down-modulation of Bcl-2 may be another molecular mechanism through which PFE induces apoptosis.
To establish the relevance of these in vitro findings to in vivo situation, athymic nude mice were implanted with androgen-responsive CWR22Rν1 cells, which are known to secrete PSA in the bloodstream of the host. Oral feeding of PFE significantly slowed the progression of CWR22Rν1 tumor growth in nude mice (Fig. 5 A and B). Importantly, this tumor growth inhibition followed a significant decrease in the serum levels of PSA, a clinical diagnostic serum marker for monitoring the presence and progression of CaP in human patients (Fig. 5C).
The present study is the first report showing the effect of the fruit pomegranate in inhibiting human prostate carcinoma cell growth in an in vitro and in vivo preclinical model. The reduction in tumor growth with concomitant reduction in PSA levels observed in the xenograft model may have human clinical relevance. The outcome of this study could have a direct practical implication and translational relevance to CaP patients, because it suggests that pomegranate consumption may retard CaP progression, which may prolong the survival and quality of life of the patients. In summary, based on the present findings, it is tempting to suggest that the fruit pomegranate and its associated antioxidants may possess a strong potential for development as a chemopreventive and possibly therapeutic agent against CaP.
Acknowledgments
This work was supported by U.S. Public Health Service Grants R01 CA 78809 and R01 CA 101039.
This paper was submitted directly (Track II) to the PNAS office.
Abbreviations: CaP, prostate cancer; PFE, pomegranate fruit extract; PSA, prostate-specific antigen; PARP, poly (ADP-ribose) polymerase; AR, androgen receptor; cdk, cyclin-dependent kinase.
References
- 1.Jemal, A., Murray, T., Ward, E., Samuels, A., Tiwari, R. C., Ghafoor, A., Feuer, E. J. & Thun, M. J. (2005) CA Cancer J. Clin. 55, 10-30. [DOI] [PubMed] [Google Scholar]
- 2.Hong, W. K. & Sporn, M. B. (1997) Science 278, 1073-1077. [DOI] [PubMed] [Google Scholar]
- 3.Parnes, H. L., Thompson, I. M. & Ford, L. G. (2005) J. Clin. Oncol. 23, 368-377. [DOI] [PubMed] [Google Scholar]
- 4.Mukhtar, H. & Ahmad, N. (1999) Toxicol. Appl. Pharmacol. 158, 207-210. [DOI] [PubMed] [Google Scholar]
- 5.Surh, Y. J. (2003) Nat. Rev. Cancer 3, 768-780. [DOI] [PubMed] [Google Scholar]
- 6.Saleem, M., Adhami, V. M., Siddiqui, I. A. & Mukhtar, H. (2003) Nutr. Cancer 47, 13-23. [DOI] [PubMed] [Google Scholar]
- 7.Greenwald, P. (2005) Recent Res. Cancer Res. 166, 1-15. [DOI] [PubMed] [Google Scholar]
- 8.Klein, E. A. & Thompson, I. M. (2004) Curr. Opin. Urol. 14, 143-149. [DOI] [PubMed] [Google Scholar]
- 9.Parnes, H. L., House, M. G., Kagan, J., Kausal, D. J. & Lieberman, R. (2004) J. Urol. 171, S68-S74. [DOI] [PubMed] [Google Scholar]
- 10.Langley, P. (2000) Br. Med. J. 321, 1153-1154.11061746 [Google Scholar]
- 11.Gil, M. I., Tomas-Barberan, F. A., Hess-Pierce, B., Holcroft, D. M. & Kedar, A. A. (2000) J. Agric. Food Chem. 10, 4581-4589. [DOI] [PubMed] [Google Scholar]
- 12.Narr Ben, C., Ayed, N. & Metche, M. Z. (1996) Lebensm. Unters. Forsch. 203, 374-378. [DOI] [PubMed] [Google Scholar]
- 13.Gupta, S., Hastak, K., Ahmad, N., Lewin, J. S. & Mukhtar, H. (2001) Proc. Natl. Acad. Sci. USA 98, 10350-10355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adhami, V. M., Siddiqui, I. A., Ahmad, N., Gupta, S. & Mukhtar, H. (2004) Cancer Res. 64, 8715-8722. [DOI] [PubMed] [Google Scholar]
- 15.Caporali, A., Davalli, P., Astancolle, S., D'Arca, D., Brausi, M., Bettuzzi, S. & Corti, A. (2004) Carcinogenesis 11, 2217-2224. [DOI] [PubMed] [Google Scholar]
- 16.Jian, L., Xie, L. P., Lee, A. H. & Binns, C. W. (2004) Int. J. Cancer 108, 130-135. [DOI] [PubMed] [Google Scholar]
- 17.Jones, S. B., DePrimo, S. E., Whitfield, M. L. & Brooks, J. D. (2005) Cancer Epidemiol. Biomarkers Prev. 14, 596-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart, J. R., Artime, M. C. & O'Brian, C. A. (2003) J. Nutr. 133, 2440S-2443S. [DOI] [PubMed] [Google Scholar]
- 19.Ratan, H. L., Steward, W. P., Gescher, A. J. & Mellon, J. K. (2002) Urol. Oncol. 7, 223-227. [DOI] [PubMed] [Google Scholar]
- 20.Aviram, M. & Dornfeld, L. (2001) Atherosclerosis 158, 195-198. [DOI] [PubMed] [Google Scholar]
- 21.Aviram, M., Dornfeld, L., Rosenblat, M., Volkova, N., Kalpan, M., Coleman, R., Hayek, T., Presser, D. & Fuhrman, B. (2000) Am. J. Clin. Nutr. 71, 1062-1076. [DOI] [PubMed] [Google Scholar]
- 22.De Nigris, F., Williams-Ignarro, S., Lerman, L. O., Crimi, E., Botti, C., Mansueto, G., D'Armiento, F. P., De Rosa, G., Sica, V., Ignarro, L. J. & Napoli, C. (2005) Proc. Natl. Acad. Sci. USA 102, 4896-4901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schubert, S. Y., Neeman, I. & Resnick, N. (2002) FASEB J. 16, 1931-1933. [DOI] [PubMed] [Google Scholar]
- 24.Kim, N. D., Mehta, R., Yu, W., Neeman, I., Livney, T., Amichay, A., Poirier, D., Nicholls, P., Kirby, A., Jiang, W., et al. (2002) Breast Cancer Res. Treat. 71, 203-217. [DOI] [PubMed] [Google Scholar]
- 25.Afaq, F., Saleem, M., Krueger, C., Reed, J. & Mukhtar, H. (2005) Int. J. Cancer 113, 423-433. [DOI] [PubMed] [Google Scholar]
- 26.Tomayko, M. M. & Reynolds, C. P. (1989) Cancer Chemother. Pharmacol. 24, 148-154. [DOI] [PubMed] [Google Scholar]
- 27.Lamb, D. J., Weigel, N. L. & Marcelli, M. (2001) Vitam. Horm. 62, 199-230. [DOI] [PubMed] [Google Scholar]
- 28.Vicini, F. A., Vargas, C., Abner, A., Kestin, L., Horwitz, E. & Martinez, A. (2005) J. Urol. 173, 1456-1462. [DOI] [PubMed] [Google Scholar]
- 29.Naz, R. K. & Herness, E. A. (2001) Front. Biosci. 6, 1083-1088. [DOI] [PubMed] [Google Scholar]
- 30.Stamey, T. A., Yang, N., Hay, A. R., McNeal, J. E., Freiha, F. S. & Redwine, E. (1987) N. Engl. J. Med. 317, 909-916. [DOI] [PubMed] [Google Scholar]
- 31.Platz, E. A., Pollak, M. N., Leitzmann, M. F., Stampfer, M. J., Willett, W. C. & Giovannucci, E. (2005) Cancer Causes Control 16, 255-262. [DOI] [PubMed] [Google Scholar]
- 32.Fujimoto, N., Chang, C., Nomura, M. & Matsumoto, T. (2005) Urol. Int. 74, 289-297. [DOI] [PubMed] [Google Scholar]
- 33.Ahmad, N., Feyes, D. K., Nieminen, A. L., Agarwal, R. & Mukhtar, H. (1997) J. Natl. Cancer Inst. 89, 1881-1886. [DOI] [PubMed] [Google Scholar]
- 34.Ahmad, N., Gupta, S. & Mukhtar, H. (2000) Arch. Biochem. Biophys. 376, 338-346. [DOI] [PubMed] [Google Scholar]
- 35.Collins, K., Jacks, T. & Pavletich, N. P. (1997) Proc. Natl. Acad. Sci. USA 94, 2776-2778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McDonald, E. R. & El Deiry, W. S. (2000) Int. J. Oncol. 16, 871-886. [PubMed] [Google Scholar]
- 37.Stadler, W. M., Vogelzang, N. J., Amato, R., Sosman, J., Taber, D., Liebowitz, D. & Vokes, E. E. (2000) J. Clin. Oncol. 18, 371-375. [DOI] [PubMed] [Google Scholar]
- 38.Gupta, S., Afaq, F. & Mukhtar, H. (2002) Oncogene 21, 3727-3738. [DOI] [PubMed] [Google Scholar]
- 39.Adhami, V. M., Ahmad, N. & Mukhtar, H. (2003) J. Nutr. 133, 2417S-2424S. [DOI] [PubMed] [Google Scholar]
- 40.Chiao, J. W., Wu, H., Ramaswamy, G., Conaway, C. C., Chung, F. L., Wang, L. & Liu, D. (2004) Carcinogenesis 25, 1403-1408. [DOI] [PubMed] [Google Scholar]
- 41.Sanchez, I. & Dynlacht, B. D. (2005) Semin. Cell Dev. Biol. 16, 311-321. [DOI] [PubMed] [Google Scholar]
- 42.Coqueret, O. (2003) Trends Cell Biol. 13, 65-70. [DOI] [PubMed] [Google Scholar]
- 43.Kim, C. H. & Moon, S. K. (2005) Arch. Biochem. Biophys. 435, 264-272. [DOI] [PubMed] [Google Scholar]
- 44.Oltersdorf, T., Elmore, S. W., Shoemaker, A. R., Armstrong, R. C., Augeri, D. J., Belli, B. A., Bruncko, M., Deckwerth, T. L., Dinges, J., Hajduk, P. J., et al. (2005) Nature 435, 677-681. [DOI] [PubMed] [Google Scholar]